Scar Endometriosis: A Rare Cause of Abdominal Pain
Abstract
:1. Introduction
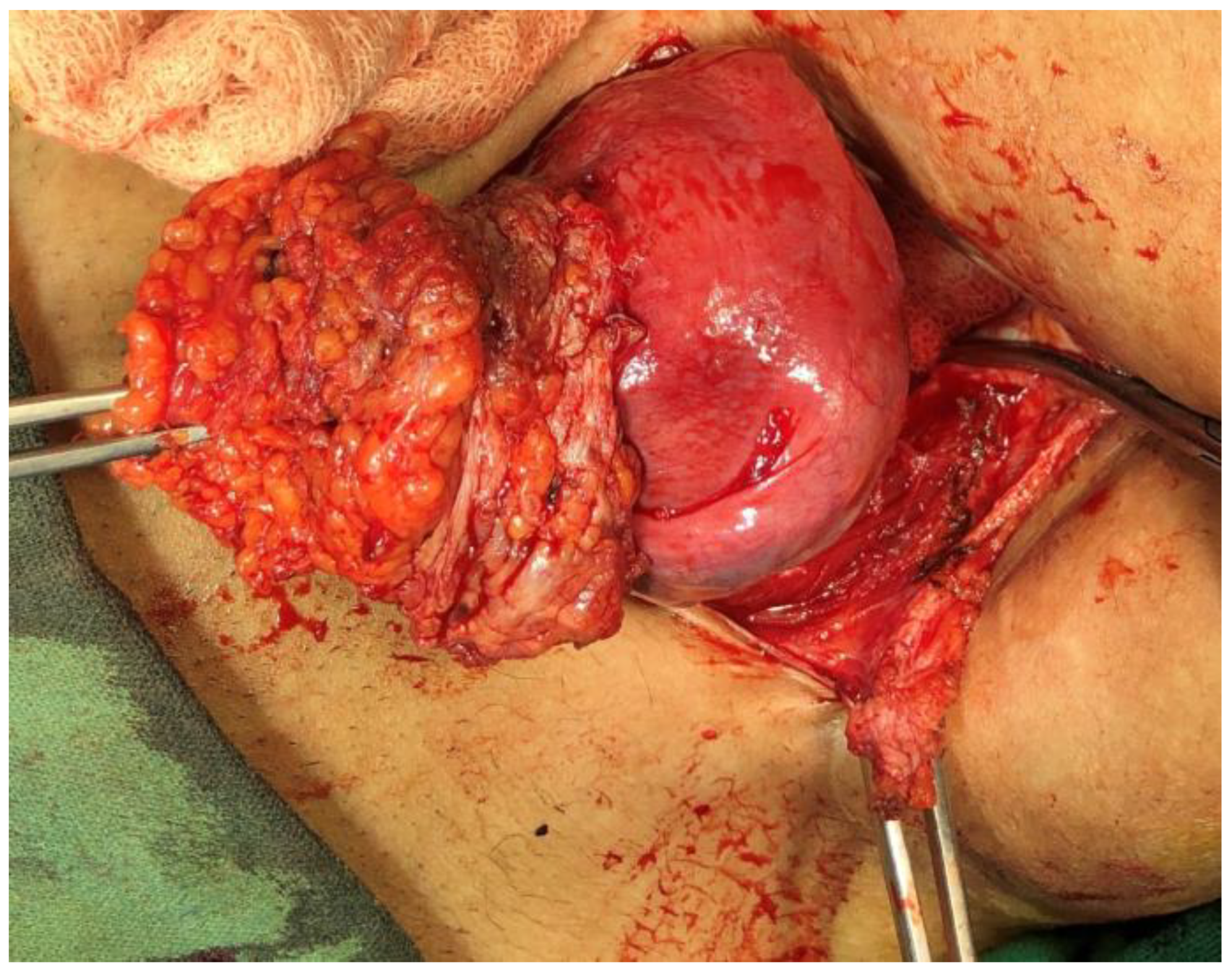
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- New NICE Guideline on Endometriosis Published. Available online: https://www.rcog.org.uk/en/about-us/nga/nga-news/nice-guideline-endometriosis/ (accessed on 30 March 2022).
- Nominato, N.S.; Prates, L.F.V.S.; Lauar, I.; Morais, J.; Maia, L.; Geber, S. Caesarean section greatly increases risk of scar endometriosis. Eur. J. Obs. Gynecol. Reprod. Biol. 2010, 152, 83–85. [Google Scholar] [CrossRef] [PubMed]
- Slaiki, S.; Jamor, J. Endometriosis of the rectus abdominis muscles: A rare case of dual location. J. Surg. Case Rep. 2020, 2020, rjaa360. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Sun, Y.; Zhang, C.; Yang, Y.; Zhang, L.; Wang, N.; Xu, H. Cesarean scar endometriosis: Presentation of 198 cases and literature review. BMC Womens Health 2019, 19, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Yıldırım, D.; Tatar, C.; Doğan, O.; Hut, A.; Dönmez, T.; Akıncı, M.; Toptas, M.; Bayik, R.N. Post-Cesarean scar endometriosis. Turkish J. Obstet. Gynecol. 2018, 15, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Tangri, M.K.; Lele, P.; Bal, H.; Tewari, R.; Majhi, D. Scar endometriosis: A series of 3 cases. Med. J. Armed Forces India 2016, 72, S185–S188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Durand, X.; Daligand, H.; Aubert, P.; Baranger, B. Abdominal wall endometriosis. J. Chir. Visc. 2010, 147, 354–359. [Google Scholar]
- Khan, Z.; Zanfagnin, V.; El-Nashar, S.A.; Famuyide, A.O.; Daftary, G.S.; Hopkins, M.R. Risk Factors, Clinical Presentation, and Outcomes for Abdominal Wall Endometriosis. J. Minim. Invasive Gynecol. 2017, 24, 478–484. [Google Scholar] [CrossRef] [PubMed]
- Danielpour, P.J.; Layke, J.C.; Durie, N.; Glickman, L.T. Scar endometriosis—A rare cause for a painful scar: A case report and review of the literature. Can. J. Plast. Surg. 2010, 18, 19–20. [Google Scholar] [CrossRef] [PubMed]
- Alnafisah, F.; Dawa, S.K.; Alalfy, S. Skin Endometriosis at the Caesarean Section Scar: A Case Report and Review of the Literature. Cureus 2018, 10, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uzuncakmak, C. Scar Endometriosis; A Case Report of this Uncommon Entity and Review of the Literature. J. Clin. Case Rep. 2013, 2013, 386783. [Google Scholar] [CrossRef]
- Kocher, M.; Hardie, A.; Schaefer, A.; McLaren, T.; Kovacs, M. Cesarean-section scar endometrioma: A case report and review of the literature. J. Radiol. Case Rep. 2017, 11, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Laxmi, T.; Goma, D.N.S.; Kumariniraula, H.; Roshnitui, T.; Binod, A. Rising Cesarean Section Rates in Nepal: Question of safety and Integrity on Obstetric Emergency Practice. J. Gynecol. Womens Health 2017, 7, 17–20. [Google Scholar]
- Bektaş, H.; Bilsel, Y.; Sar, Y.S.; Ersöz, F.; Koç, O.; Deniz, M.; Boran, B.; Huq, G.E. Abdominal wall endometrioma; A 10-year experience and brief review of the literature. J. Surg. Res. 2010, 164, e77–e81. [Google Scholar] [CrossRef] [PubMed]
- Uçar, M.G.; Şanlıkan, F.; Göçmen, A. Surgical Treatment of Scar Endometriosis Following Cesarean Section, a Series of 12 Cases. Indian J. Surg. 2015, 77, 682–686. [Google Scholar] [CrossRef] [PubMed] [Green Version]





Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nepali, R.; Upadhyaya Kafle, S.; Pradhan, T.; Dhamala, J.N. Scar Endometriosis: A Rare Cause of Abdominal Pain. Dermatopathology 2022, 9, 158-163. https://doi.org/10.3390/dermatopathology9020020
Nepali R, Upadhyaya Kafle S, Pradhan T, Dhamala JN. Scar Endometriosis: A Rare Cause of Abdominal Pain. Dermatopathology. 2022; 9(2):158-163. https://doi.org/10.3390/dermatopathology9020020
Chicago/Turabian StyleNepali, Rohit, Santosh Upadhyaya Kafle, Tarun Pradhan, and Jiba Nath Dhamala. 2022. "Scar Endometriosis: A Rare Cause of Abdominal Pain" Dermatopathology 9, no. 2: 158-163. https://doi.org/10.3390/dermatopathology9020020
APA StyleNepali, R., Upadhyaya Kafle, S., Pradhan, T., & Dhamala, J. N. (2022). Scar Endometriosis: A Rare Cause of Abdominal Pain. Dermatopathology, 9(2), 158-163. https://doi.org/10.3390/dermatopathology9020020





