Deeply Pigmented Reticulated Acanthoma with Sebaceous Differentiation Mimicking Cutaneous Malignancy: A Case Report and Review of the Literature
Simple Summary
Abstract
1. Introduction
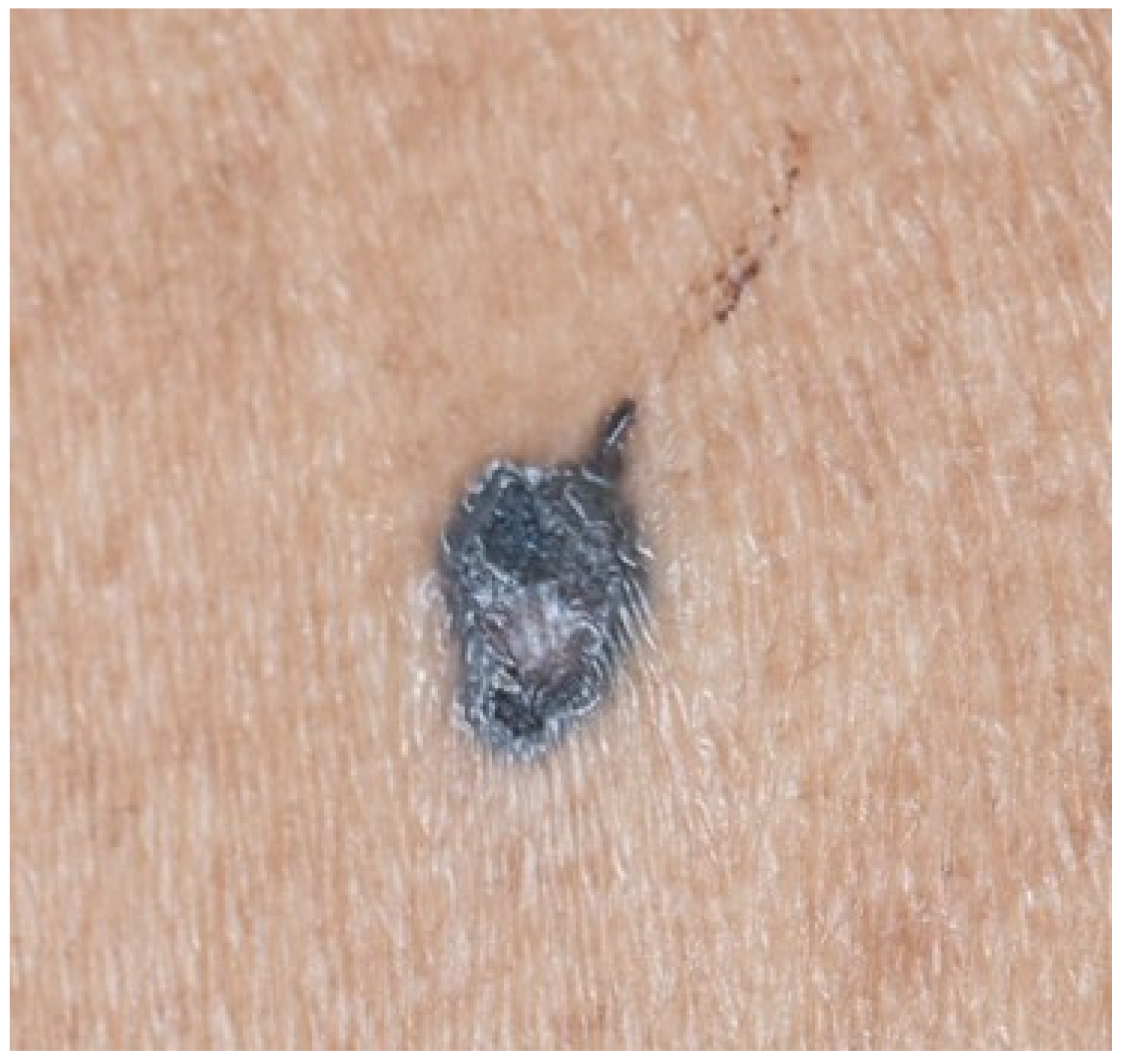
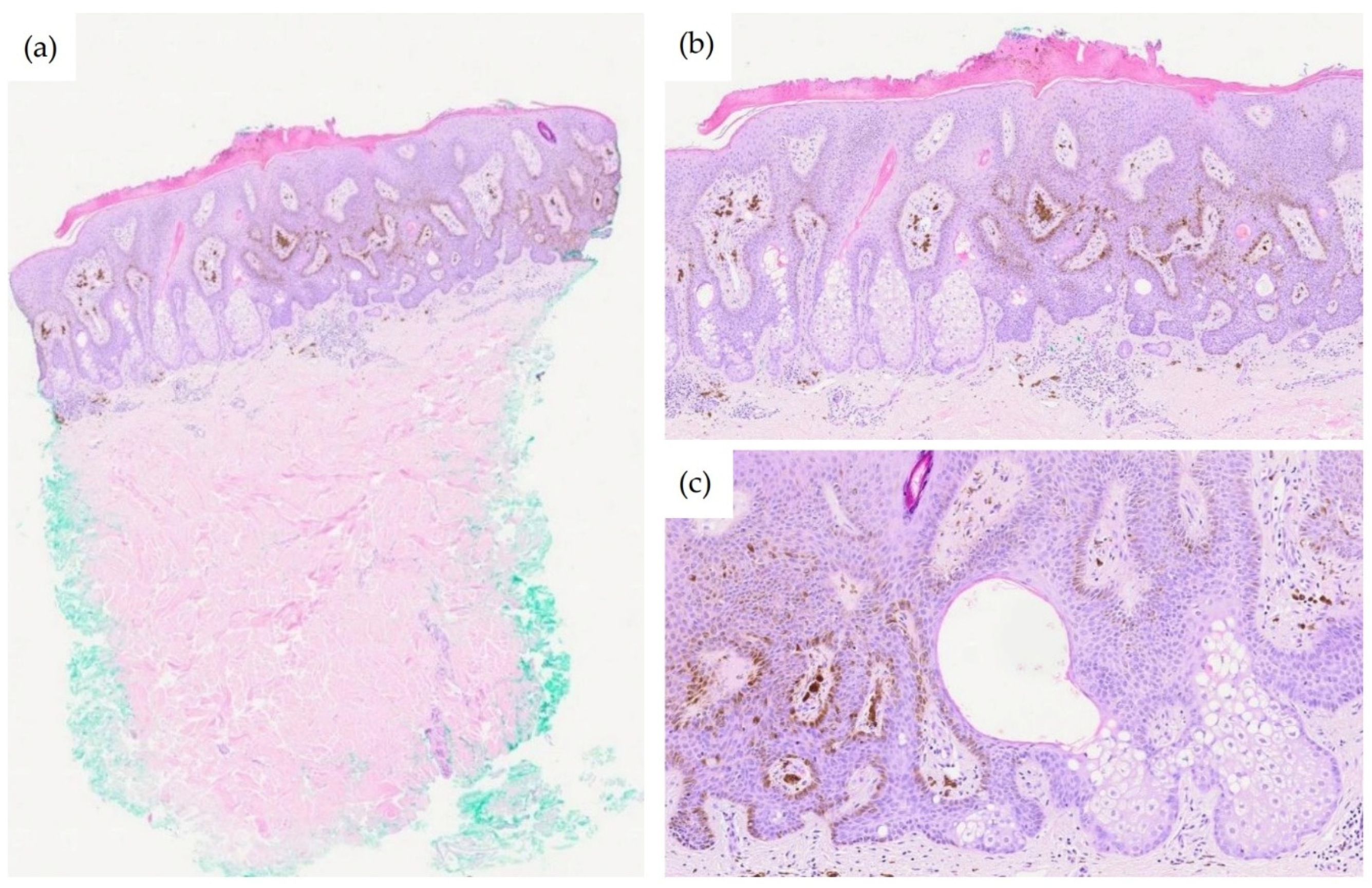
2. Case Description
3. Discussion
3.1. Clinical and Dermoscopic Considerations
3.2. Histopathological Differential Diagnosis
3.3. Muir–Torre Syndrome Considerations
3.4. Management Considerations
3.5. Potential for Malignant Transformation
4. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Steffen, C.; Ackerman, A.B. Reticulated acanthoma with sebaceous differentiation. In Neoplasms with Sebaceous Differentiation; Lea & Febiger: Philadelphia, PA, USA, 1994; pp. 449–467. [Google Scholar]
- Fukai, K.; Sowa, J.; Ishii, M. Reticulated acanthoma with sebaceous differentiation. Am. J. Dermatopathol. 2006, 28, 158–161. [Google Scholar] [CrossRef]
- Valencia, V.G.; Pérez, H.C.; Manrique, M.J.V. Reticulated Acanthoma with Sebaceous Differentiation. Actas Dermo-Sifiliogr. 2022, 113, TS5–TS7. [Google Scholar] [CrossRef]
- Haake, D.L.; Minni, J.P.; Nowak, M.; Abenoza, P.; Nousari, C.H. Reticulated acanthoma with sebaceous differentiation. Lack of association with Muir-Torre syndrome. Am. J. Dermatopathol. 2009, 31, 391–392. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, F.; Leocadia, E.; Macarenco, R.S.; Lapins, J.; Huet, P.; Akay, B.N.; Steiner, D. Reticulated acanthoma with sebaceous differentiation mimicking melanoma. Dermatol. Pract. Concept. 2017, 7, 35–37. [Google Scholar] [CrossRef] [PubMed]
- Molinelli, E.; D’Agostino, G.M.; Sapigni, C.; Simonetti, O.; Brisigotti, V.; Radi, G.; Diotallevi, F.; Legrenzi, L.; Offidani, A. Reticulated acanthoma with sebaceous differentiation. JAAD Case Rep. 2021, 11, 54–56. [Google Scholar] [CrossRef] [PubMed]
- Coelho, A.; Luzar, B. Superficial epithelioma with sebaceous differentiation: A case report with literature review. Acta Dermatovenerol. Alp. Pannonica Adriat. 2017, 26, 63–66. [Google Scholar] [CrossRef] [PubMed]
- Shon, W.; Wolz, M.M.; Newman, C.C.; Bridges, A.G. Reticulated acanthoma with sebaceous differentiation: Another sebaceous neoplasm associated with Muir-Torre syndrome? Australas. J. Dermatol. 2014, 55, e71–e73. [Google Scholar] [CrossRef] [PubMed]
- Nakazato, S.; Yanagi, T.; Inamura, Y.; Kitamura, S.; Hata, H.; Fujita, Y.; Anan, T.; Honma, M.; Shimizu, H. Reticulated acanthoma with sebaceous differentiation. Eur. J. Dermatol. 2017, 27, 318–320. [Google Scholar] [CrossRef] [PubMed]
- Ito, T.; Yoshida, Y.; Furue, M.; Yamamoto, O. Dermoscopic features of reticulated acanthoma (superficial epithelioma) with sebaceous differentiation. Eur. J. Dermatol. 2012, 22, 704–706. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, K.; Sugano, Y.; Kaku, Y.; Hatakeyama, K.; Fukumoto, T.; Asada, H. Case of reticulated acanthoma with sebaceous differentiation with clinicopathological surveillance. J. Dermatol. 2017, 44, e204–e205. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.T.; Zhang, Q.; Shen, H.; Liu, Z.H. Reticulated acanthoma with sebaceous differentiation: A case report. Medicine 2025, 104, e46426. [Google Scholar] [CrossRef]
- Yoshida, A.; Yoshida, Y.; Goto, H.; Yamamoto, O. Bowen’s disease occurring on a reticulated acanthoma with sebaceous differentiation: Possible malignant transformation. Eur. J. Dermatol. 2021, 31, 562–564. [Google Scholar] [CrossRef]
| Feature | Published Cases | Present Case | Concordance |
|---|---|---|---|
| Age | 52–93 years (Mean 68 years) | 78 years | Concordant |
| Sex | Male 8, Female 4 | Male | Concordant |
| Number of lesions | Solitary in all cases | Solitary | Concordant |
| Location | Back, trunk, lower body (buttocks, hip), forearm, chest | Upper back | Concordant |
| Size | 6 mm–50 mm | 8 × 5 mm | Concordant |
| Duration | 2 months to 30 years | ~5 years | Concordant |
| Symptoms | Asymptomatic or pruritic | Mild pruritus | Concordant |
| Clinical color | Yellow, brown, red, white, variegated | Dark gray to black | Atypical |
| Clinical differential | Seborrheic keratosis, Bowen disease, Basal cell carcinoma, Melanoma | Melanoma | Concordant |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the European Society of Dermatopathology. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Chamninawakul, P.; Wu, X.; Lee, J.S.S. Deeply Pigmented Reticulated Acanthoma with Sebaceous Differentiation Mimicking Cutaneous Malignancy: A Case Report and Review of the Literature. Dermatopathology 2026, 13, 4. https://doi.org/10.3390/dermatopathology13010004
Chamninawakul P, Wu X, Lee JSS. Deeply Pigmented Reticulated Acanthoma with Sebaceous Differentiation Mimicking Cutaneous Malignancy: A Case Report and Review of the Literature. Dermatopathology. 2026; 13(1):4. https://doi.org/10.3390/dermatopathology13010004
Chicago/Turabian StyleChamninawakul, Padol, Xiaotian Wu, and Joyce S. S. Lee. 2026. "Deeply Pigmented Reticulated Acanthoma with Sebaceous Differentiation Mimicking Cutaneous Malignancy: A Case Report and Review of the Literature" Dermatopathology 13, no. 1: 4. https://doi.org/10.3390/dermatopathology13010004
APA StyleChamninawakul, P., Wu, X., & Lee, J. S. S. (2026). Deeply Pigmented Reticulated Acanthoma with Sebaceous Differentiation Mimicking Cutaneous Malignancy: A Case Report and Review of the Literature. Dermatopathology, 13(1), 4. https://doi.org/10.3390/dermatopathology13010004








