Indeterminate Subcutaneous Lesion of the Nasal Dorsum in an Adolescent: A Multidisciplinary Approach to a Rare Case of Spindle Cell Lipoma
Abstract
1. Introduction
2. Case Report
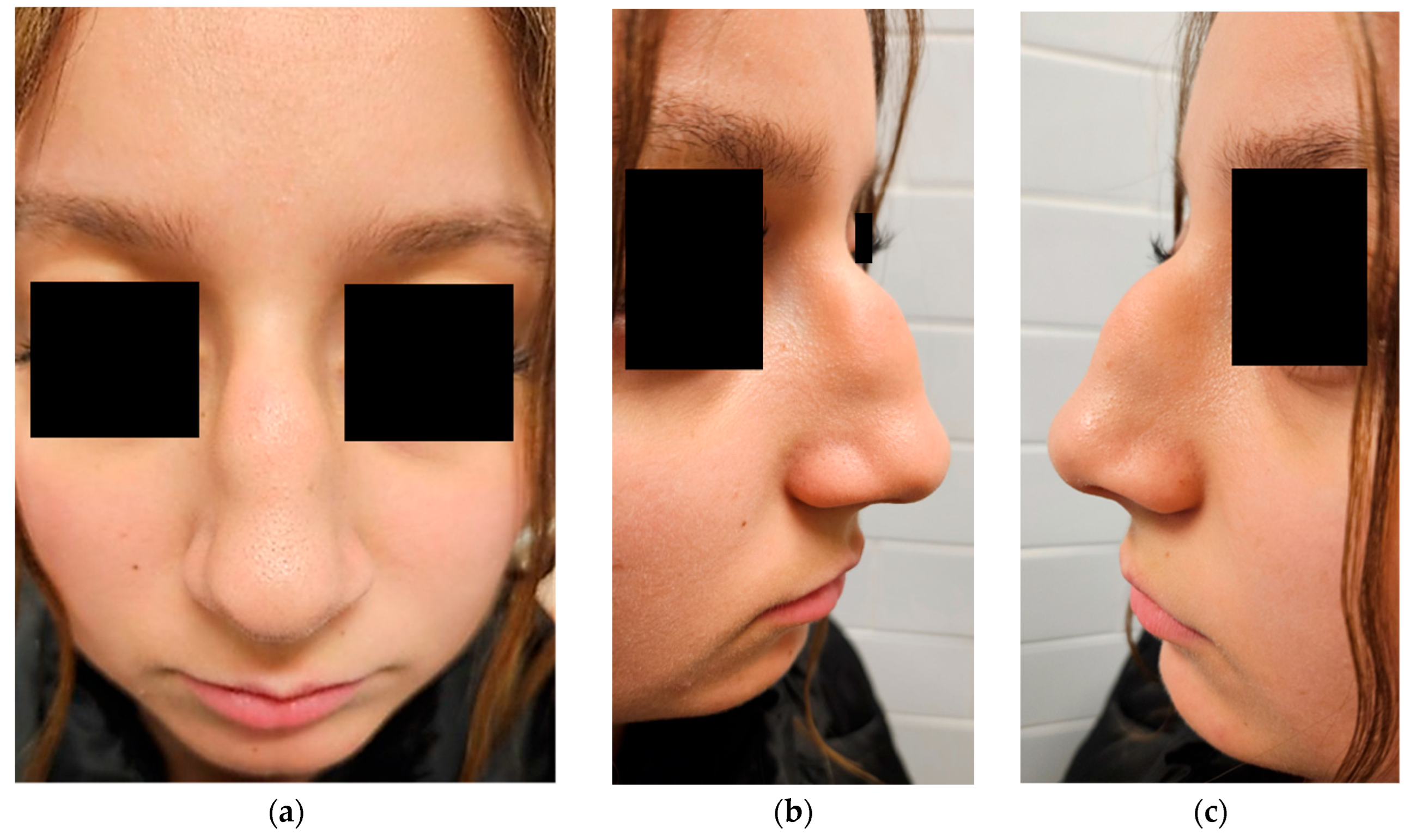
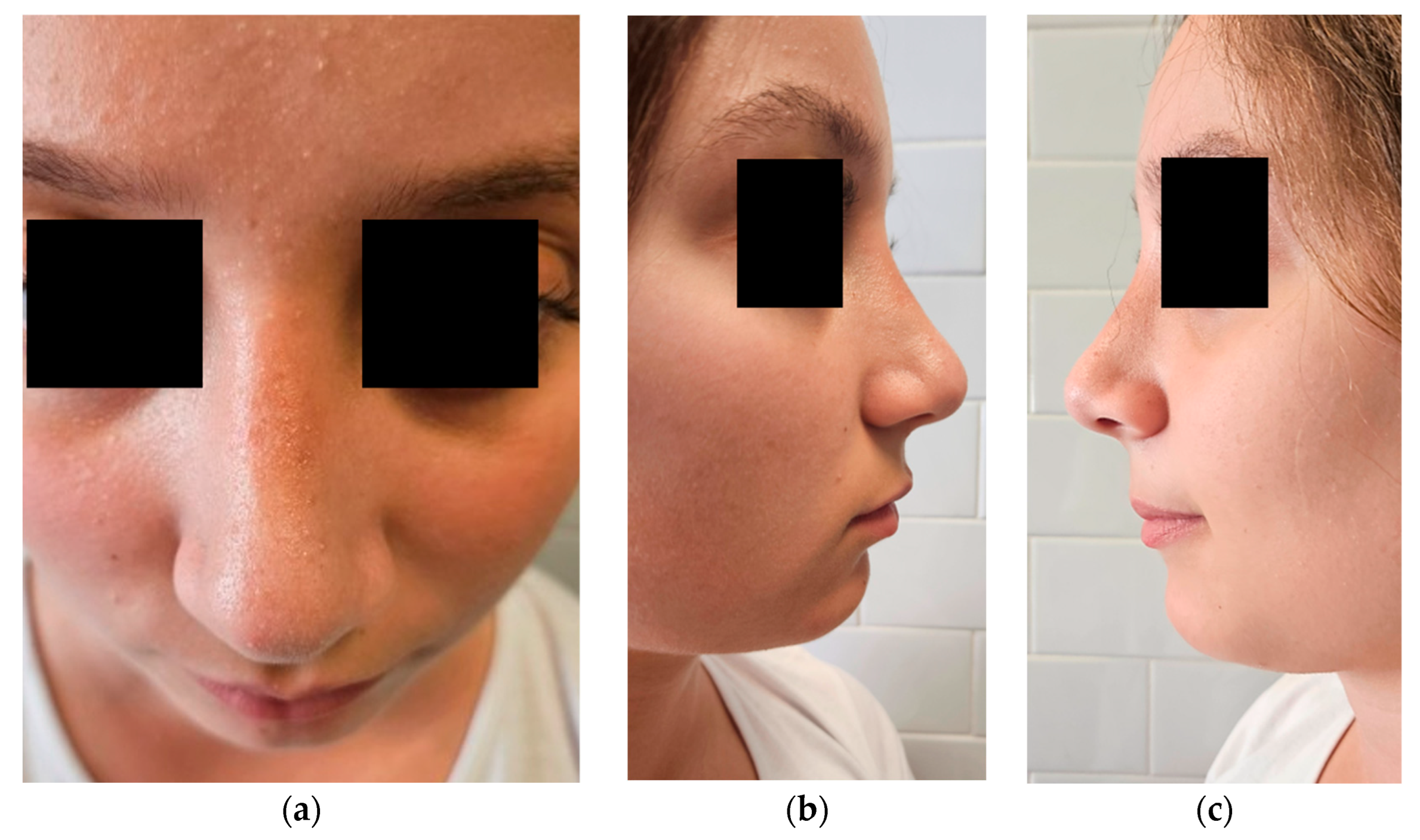
2.1. Clinical Presentation
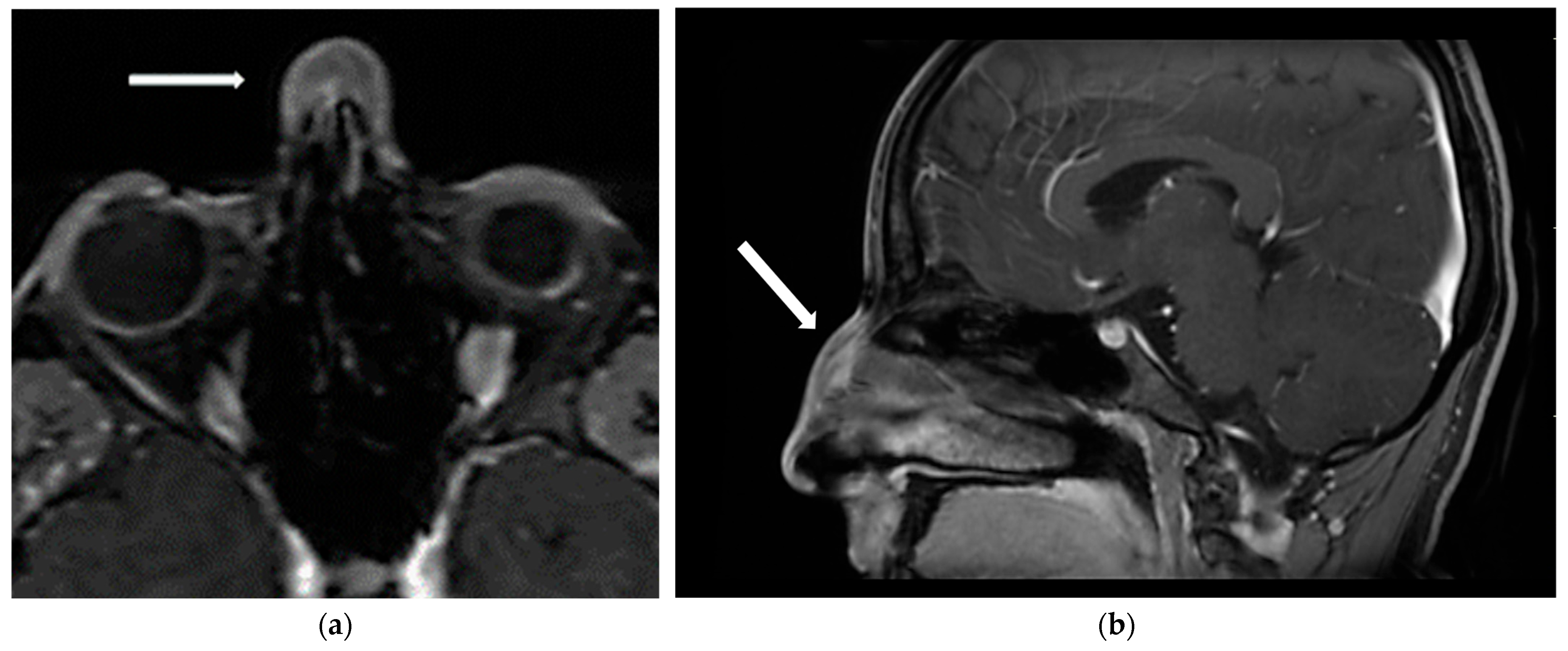
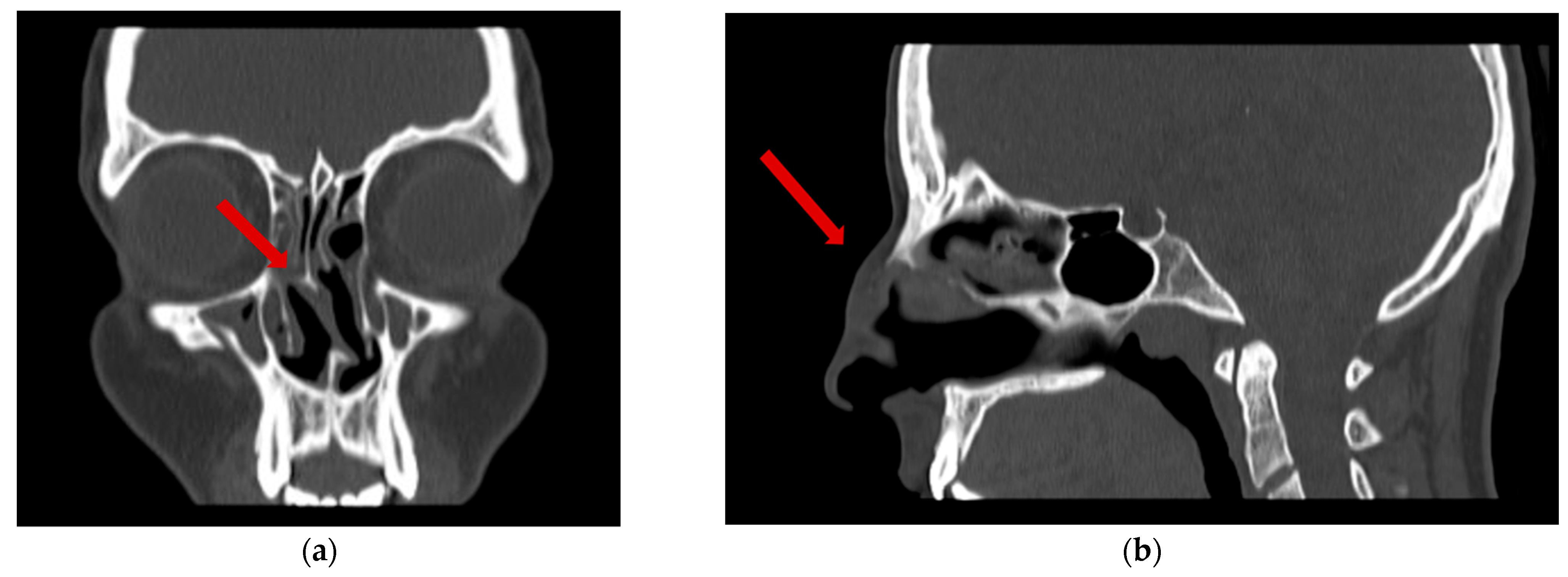
2.2. Investigations
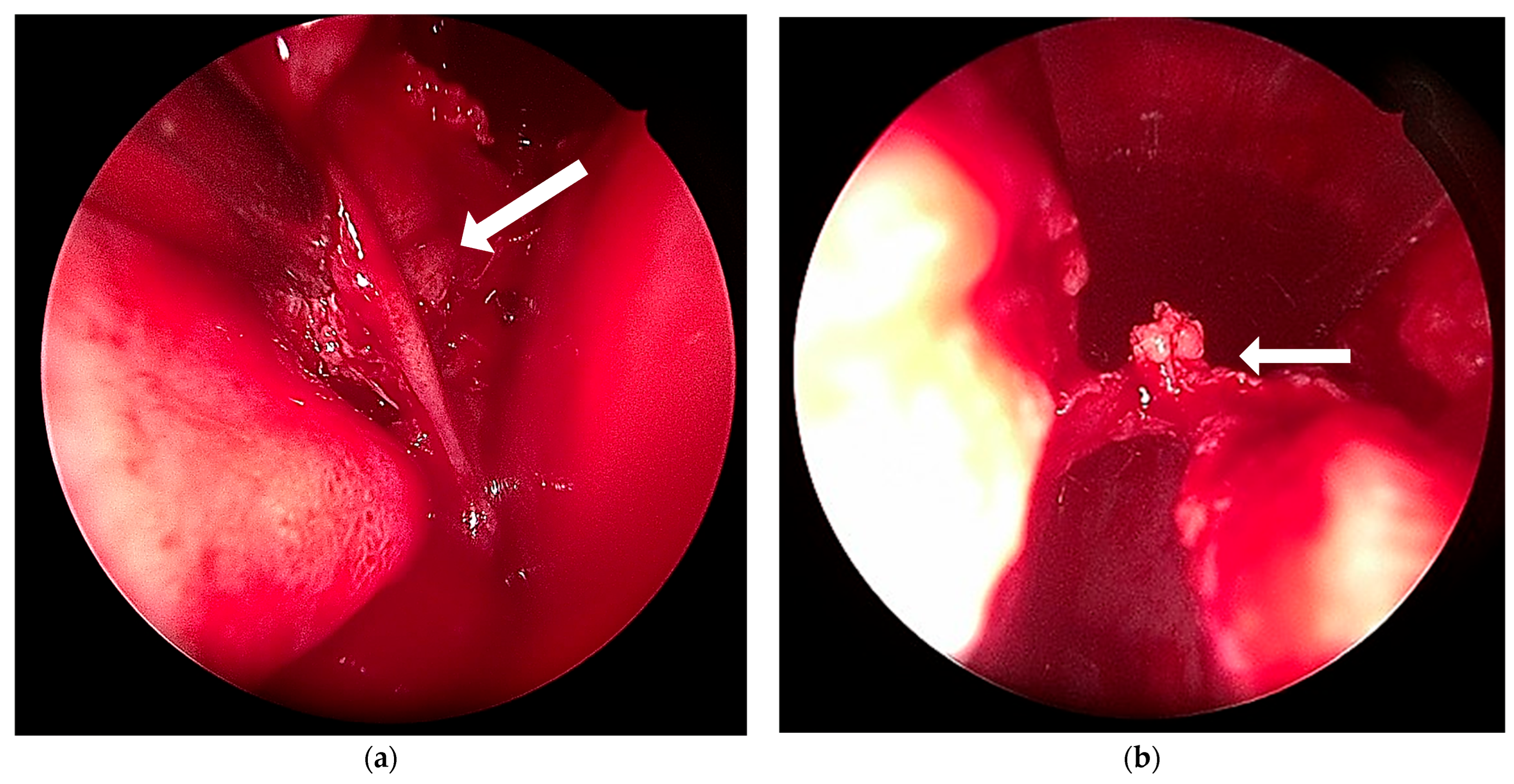
2.3. Treatment and Outcome
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| SCL | Spindle cell lipoma |
| CD34 | Cluster of Differentiation 34, a transmembrane glycoprotein expressed on hematopoietic stem cells, endothelial cells, and certain soft tissue tumors |
| Ki-67 | Nuclear protein used as a proliferation marker in histopathology |
| MDM2 | Murine Double Minute 2 |
| CDK4 | Cyclin-Dependent Kinase 4 |
| ALT/WDL | Atypical Lipomatous Tumor/Well-Differentiated Liposarcoma |
| DFSP | Dermatofibrosarcoma Protuberans |
| SFT | Solitary Fibrous Tumor |
| US | Soft tissue ultrasound |
| CT | Computed tomography |
| MRI | Magnetic resonance imaging |
| FNAC | Fine needle aspiration cytology |
References
- Cunha, B.; Kuroedov, D.; Conceição, C. Imaging of pediatric nasal masses: A review. J. Neuroimaging 2022, 32, 230–244. [Google Scholar] [CrossRef]
- Duarte, V.M.; Liu, Y.F.; Shapiro, N.L. Uncommon presentation of a benign nasopharyngeal mass in an adolescent: Comprehensive review of pediatric nasopharyngeal masses. Case Rep. Pediatr. 2013, 2013, 816409. [Google Scholar] [CrossRef]
- Clarke, R.W.; Kinshuck, A.J. Nasal masses in children. Otorhinolaryngologist 2012, 5, 133–138. [Google Scholar]
- Kotowski, M. The differential diagnosis of congenital developmental midline nasal masses: Histopathological, clinical, and radiological aspects. Diagnostics 2023, 13, 2796. [Google Scholar] [CrossRef]
- Billings, S.; Folpe, A. Diagnostically challenging spindle cell lipomas: A report of 34 “low-fat” and “fat-free” variants. Am. J. Dermatopathol. 2007, 29, 437–442. [Google Scholar] [CrossRef]
- Ohshima, Y.; Nishio, J.; Nakayama, S.; Koga, K.; Aoki, M.; Yamamoto, T. Spindle cell lipoma and pleomorphic lipoma: An update and review. Cancer Diagn. Progn. 2023, 3, 282–290. [Google Scholar] [CrossRef]
- Zhu, C.S.; Kwan, E.A.; Wohltmann, W.E. A fat tumor goes on a diet: Rare case of low-fat spindle cell lipoma. J. Cutan. Pathol. 2021, 49, 839–841. [Google Scholar] [CrossRef]
- Cheah, A.; Billings, S.; Goldblum, J.; Hornick, J.; Uddin, N.; Rubin, B. Spindle cell/pleomorphic lipomas of the face: An under-recognized diagnosis. Histopathology 2015, 66, 430–437. [Google Scholar] [CrossRef]
- Kumar, P.; Mahajan, N.; Jain, R.; Khatri, A. Spindle cell lipoma, dorsum of hand in a 4 year old child: A rare entity. Indian J. Pathol. Microbiol. 2020, 63, 301–303. [Google Scholar] [CrossRef]
- McCarthy, A.J.; Chetty, R. Tumours composed of fat are no longer a simple diagnosis: An overview of fatty tumours with a spindle cell component. J. Clin. Pathol. 2018, 71, 483–492. [Google Scholar] [CrossRef]
- Wood, L.; Fountaine, T.J.; Rosamilia, L.; Helm, K.F.; Clarke, L.E. Cutaneous CD34+ spindle cell neoplasms: Histopathologic features distinguish spindle cell lipoma, solitary fibrous tumor, and dermatofibrosarcoma protuberans. Am. J. Dermatopathol. 2010, 32, 764–768. [Google Scholar] [CrossRef]
- Vecchio, G.; Caltabiano, R.; Gurrera, A.; Lanzafame, S. Lipoma with osteocartilaginous metaplasia: Case report and literature review. Pathologica 2010, 102, 28–29. [Google Scholar]
- Park, J.Y.; Park, H.; Park, N.J.; Park, J.S.; Sung, H.J.; Lee, S.S. Use of Calretinin, CD56, and CD34 for Differential Diagnosis of Schwannoma and Neurofibroma. J. Pathol. Transl. Med. 2011, 45, 30–35. [Google Scholar] [CrossRef]
- Doyle, L.A.; Vivero, M.; Fletcher, C.D.M.; Mertens, F.; Hornick, J.L. Nuclear expression of STAT6 distinguishes solitary fibrous tumor from histologic mimics. Mod. Pathol. 2014, 27, 390–395. [Google Scholar] [CrossRef]
- Kubin, M.E.; Laanto, U.; Lindgren, O.; Tasanen, K. A rare, recurrent spindle cell lipoma of the nose. Acta Derm. Venereol. 2021, 101, adv00571. [Google Scholar] [CrossRef]
- Gupta, C.; Gupta, R.; Bhardwaj, S. Role of fine needle aspiration cytology in the diagnosis of cutaneous and subcutaneous swellings. IP Arch. Cytol. Histopathol. Res. 2023, 8, 41–45. [Google Scholar] [CrossRef]
- Bhowmik, A.; Mallick Sinha, M.G.; Barman, D.C. Role of Fine Needle Aspiration Cytology in the Diagnosis of Skin and Superficial Soft Tissue Lesions: A Study of 510 Cases. Turk. Patoloji Derg. 2015, 31, 200–205. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gupta, R.; John, J.; Ranganathan, N.; Stepanian, R.; Gupta, M.; Hart, J.; Nossoni, F.; Shaheen, K.; Folbe, A.; Chaiyasate, K. Outcomes of closed versus open rhinoplasty: A systematic review. Arch. Plast. Surg. 2022, 49, 569–579. [Google Scholar] [CrossRef]
- Radulesco, T.; Medawar, C.; Michel, J. Video-assisted septorhinoplasty, the future of endonasal rhinoplasty—A technical note. Aesthetic Plast. Surg. 2023, 47, 2651–2657. [Google Scholar] [CrossRef]
- Zenginkinet, T.; Okay, E.; Çelik, A.; Yıldırım, A.N.T.; Öztürk, M.B. Clinical results after surgical treatment of spindle cell lipomas. Duzce Med. J. 2021, 23, 258–262. [Google Scholar] [CrossRef]
- Apaydin, F.; Stanic, L.; Unadkat, S.; Saleh, H.A. Postoperative care in aesthetic rhinoplasty patients. Facial Plast. Surg. 2018, 34, 553–560. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, N.; Warner, J.P.; Adamson, P. Adolescent rhinoplasty: Challenges and psychosocial and clinical outcomes. Aesthetic Plast. Surg. 2010, 34, 510–516. [Google Scholar] [CrossRef] [PubMed]
- Tanthry, D.; Devan, P.; Kumar, K.; Bhandary, R. A rare case of spindle cell lipoma of nose. J. Surg. Technol. Case Rep. 2012, 4, 110–112. [Google Scholar] [CrossRef][Green Version]
- Hellingman, C.A.; Datema, F.R. Management of a nasal spindle cell lipoma: Diagnostic and therapeutic considerations. Dermatol. Surg. 2015, 41, 1424–1426. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the European Society of Dermatopathology. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Serrone, A.; Rustichelli, C.; Fadda, G.L.; Riva, G.; Rizzo, M.; Cavallo, G. Indeterminate Subcutaneous Lesion of the Nasal Dorsum in an Adolescent: A Multidisciplinary Approach to a Rare Case of Spindle Cell Lipoma. Dermatopathology 2025, 12, 40. https://doi.org/10.3390/dermatopathology12040040
Serrone A, Rustichelli C, Fadda GL, Riva G, Rizzo M, Cavallo G. Indeterminate Subcutaneous Lesion of the Nasal Dorsum in an Adolescent: A Multidisciplinary Approach to a Rare Case of Spindle Cell Lipoma. Dermatopathology. 2025; 12(4):40. https://doi.org/10.3390/dermatopathology12040040
Chicago/Turabian StyleSerrone, Alessandro, Chiara Rustichelli, Gian Luca Fadda, Giuseppe Riva, Massimo Rizzo, and Giovanni Cavallo. 2025. "Indeterminate Subcutaneous Lesion of the Nasal Dorsum in an Adolescent: A Multidisciplinary Approach to a Rare Case of Spindle Cell Lipoma" Dermatopathology 12, no. 4: 40. https://doi.org/10.3390/dermatopathology12040040
APA StyleSerrone, A., Rustichelli, C., Fadda, G. L., Riva, G., Rizzo, M., & Cavallo, G. (2025). Indeterminate Subcutaneous Lesion of the Nasal Dorsum in an Adolescent: A Multidisciplinary Approach to a Rare Case of Spindle Cell Lipoma. Dermatopathology, 12(4), 40. https://doi.org/10.3390/dermatopathology12040040








