Uncommon Collision Tumors: Dermoscopic and Histopathological Features of Basal Cell Carcinoma Overlying Dermatofibroma
Abstract
1. Introduction
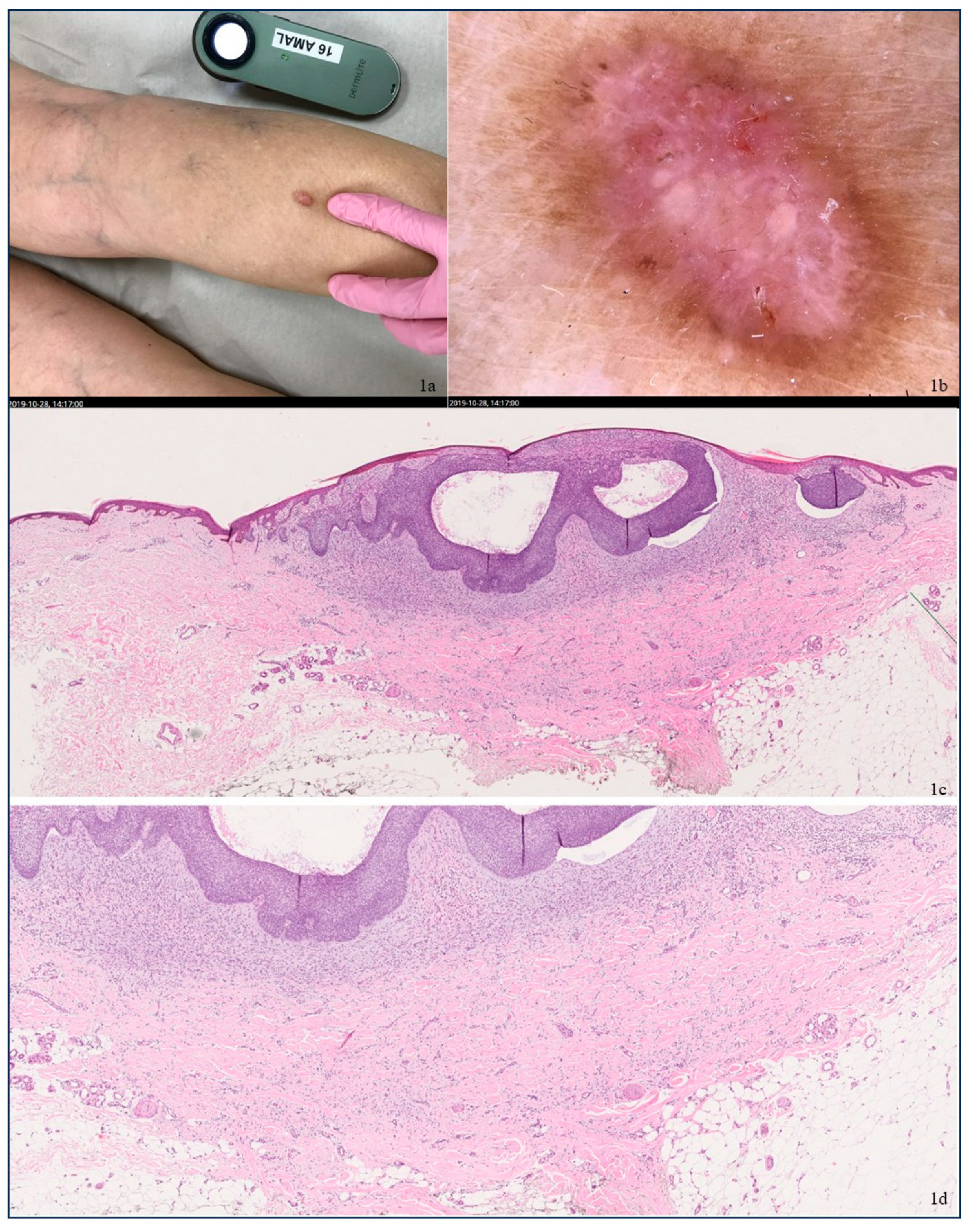
2. Case 1
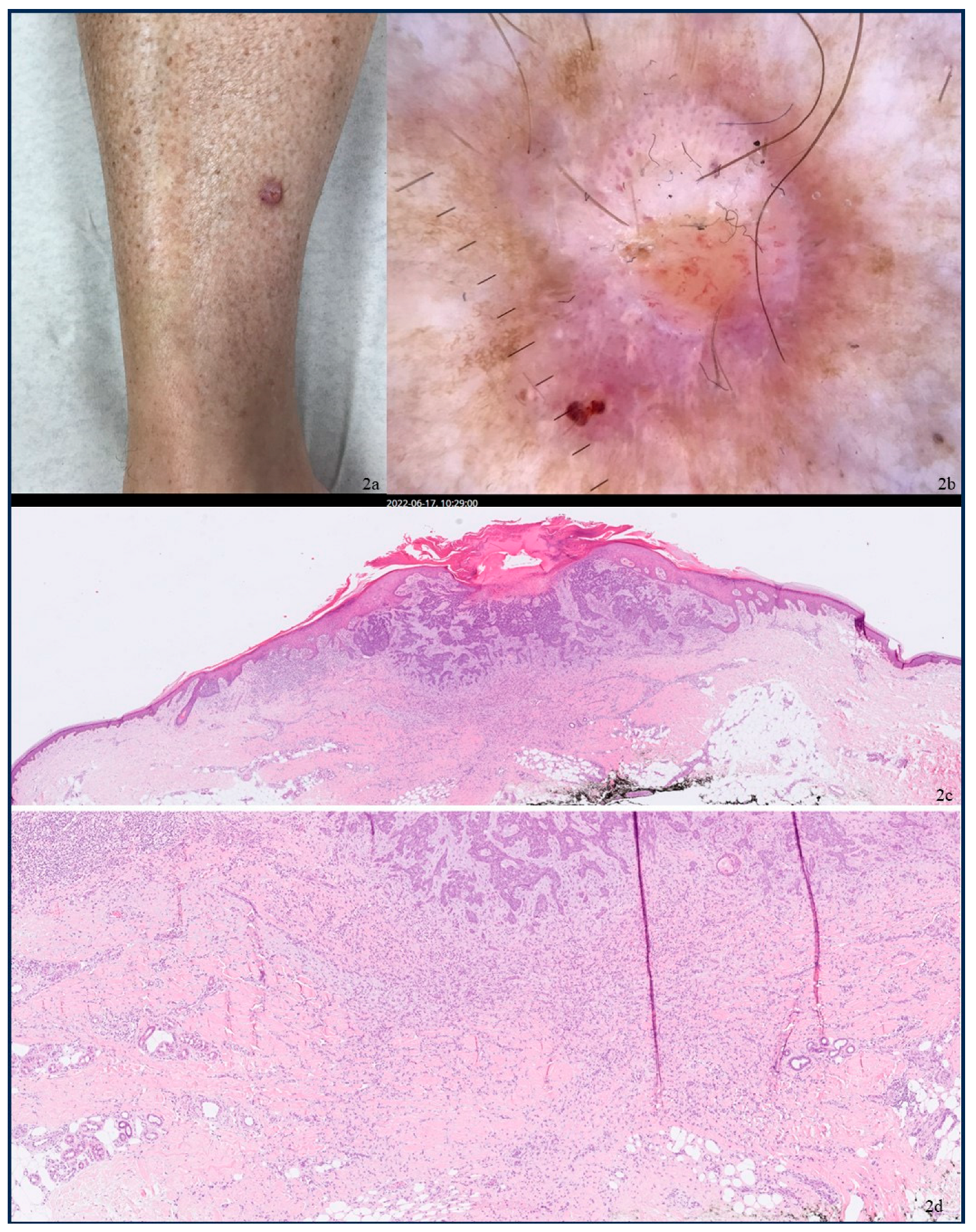
3. Case 2
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gulin, S.J.; Loncaric, D.; Rados, J. Basal Cell Carcinoma Overlying a Dermatofibroma: A Rare Collision Tumor. Dermatol. Pract. Concept. 2019, 10, e2020015. [Google Scholar] [PubMed]
- Mortimore, A.; Muir, J.; Muir, J. Basal cell carcinoma in dermatofibroma: Dual diagnosis. Aust. J. Gen. Pract. 2020, 49, 842–844. [Google Scholar] [PubMed]
- McKenna, K.E.; Somervilk, J.E.; Walsh, M.Y.; Dawson, J.F.; Burrows, D. Basal cell carcinoma occurring in association with dermatofibroma. Dermatology 1993, 187, 54–57. [Google Scholar] [CrossRef] [PubMed]
- Jain, M.; Carrera, C.; Marghoob, A.A. Basal cell carcinoma and balloon cell nevus collision mimicking a melanoma on reflectance confocal microscopy. JAAD Case Rep. 2020, 6, 339–340. [Google Scholar] [CrossRef] [PubMed]
- Boyd, A.S.; Rapini, R.P. Cutaneous collision tumors. An analysis of 69 cases and review of the literature. Am. J. Dermatopathol. 1994, 16, 253–257. [Google Scholar] [CrossRef] [PubMed]
- Speiser, J.J.; Aggarwal, S.; Wold, L.; Tung, R.; Hutchens, K.A. A Rare Collision in Dermatopathology: Basal Cell Carcinoma and Atypical Fibroxanthoma. Am. J. Dermatopathol. 2015, 37, 950–953. [Google Scholar] [PubMed]
- Blum, A.; Siggs, G.; Marghoob, A.A.; Kreusch, J.; Cabo, H.; Campos-do-Carmo, G.; Shiraishi, A.F.C.; Kienitz, A.; Maldonado-Seral, C.; Maltagliati-Holzner, P.; et al. Collision skin lesions-results of a multicenter study of the International Dermoscopy Society (IDS). Dermatol. Pract. Concept. 2017, 7, 51–62. [Google Scholar] [PubMed]
- Savas, S.; Yuksel, E.; Erdemir, A.; Gurel, M.; Leblebici, C. A Collision Tumor: Reflectance Confocal Microscopy Features and Correlation between Dermoscopy and Histopathology. Indian. J. Dermatol. 2019, 64, 155–157. [Google Scholar] [PubMed]
- Liu, Y.A.; Ciurea, A.M.; Aung, P.P. A diagnostic approach to basaloid neoplasms of the skin: Squamous is red; basals are blue but alas! If only that were true. Diagn. Histopathol. 2024, 30, 60–76. [Google Scholar]
- Alves, J.V.P.; Matos, D.M.; Barreiros, H.F.; Bártolo, E.A.F.L.F. Variants of dermatofibroma—A histopathological study. An. Bras. Dermatol. 2014, 89, 472–477. [Google Scholar] [PubMed]
- Curry, J.L.; Goulder, S.J.; Nickoloff, B.J. Occurrence of a basal cell carcinoma and dermatofibroma in a smallpox vaccination scar. Dermatol. Surg. 2008, 34, 133–134. [Google Scholar]
- Cohen, P.R.; Calame, A. Multiple Skin Neoplasms at One Site (MUSK IN A NEST): A Comprehensive Review of Basal Cell Carcinoma and Benign or Malignant “Collision” Tumors at the Same Cutaneous Location. Clin. Cosmet. Investig. Dermatol. 2020, 13, 731–741. [Google Scholar] [CrossRef] [PubMed]
- Cohen, P.R. Basal cell carcinoma associated with non-neoplastic cutaneous conditions: A comprehensive review. Dermatol. Online J. 2021, 27, 1. [Google Scholar] [CrossRef]
- Córdoba, S.; Hernández, A.; Romero, A.; Arias, D.; Castaño, E.; García-Donoso, C.; Borbujo, J.M. Basal cell carcinoma overlying a dermatofibroma. Actas Dermosifiliogr. 2005, 96, 612–615. [Google Scholar] [CrossRef] [PubMed]
- Shuweiter, M.; Böer, A. Spectrum of follicular and sebaceous differentiation induced by dermatofibroma. Am. J. Dermatopathol. 2009, 31, 778–785. [Google Scholar] [CrossRef] [PubMed]
- Jernbeck, J.; Glaumann, B.; Glas, J.E. Basal cell carcinoma. Clinical evaluation of the histological grading of aggressive types of cancer. Lakartidningen 1988, 85, 3467–3470. [Google Scholar] [PubMed]
- Brancaccio, G.; Nuzzo, T.; Di Maio, R.; Lallas, A.; Gambardella, A.; Lupoli, A.; Caccavale, S.; Alfano, R.; Tschandl, P.; Argenziano, G. Dermatofibroma looks dermoscopically different on trunk versus extremities. G. Ital. Dermatol. Venereol. 2017, 152, 333–337. [Google Scholar] [PubMed]
- Ungureanu, L.; Cosgarea, I.; Şenilǎ, S.; Vasilovici, A. Role of Dermoscopy in the Assessment of Basal Cell Carcinoma. Front. Med. 2021, 8, 718855. [Google Scholar] [CrossRef] [PubMed]
- Lallas, A.; Apalla, Z.; Ioannides, D.; Argenziano, G.; Castagnetti, F.; Moscarella, E.; Longo, C.; Palmieri, T.; Ramundo, D.; Zalaudek, I. Dermoscopy in the diagnosis and management of basal cell carcinoma. Future Oncol. 2015, 11, 2975–2984. [Google Scholar] [CrossRef] [PubMed]
- Myers, D.J.; Fillman, E.P. Dermatofibroma. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024; pp. 83–84. [Google Scholar]
- Stanoszek, L.M.; Wang, G.Y.; Harms, P.W. Histologic Mimics of Basal Cell Carcinoma. Arch. Pathol. Lab. Med. 2017, 141, 1490–1502. [Google Scholar] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the European Society of Dermatopathology. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Makansi, A.; Enerbäck, C.; Madentzoglou, M.; Kravvas, G.; Gulin, S.J. Uncommon Collision Tumors: Dermoscopic and Histopathological Features of Basal Cell Carcinoma Overlying Dermatofibroma. Dermatopathology 2025, 12, 10. https://doi.org/10.3390/dermatopathology12020010
Makansi A, Enerbäck C, Madentzoglou M, Kravvas G, Gulin SJ. Uncommon Collision Tumors: Dermoscopic and Histopathological Features of Basal Cell Carcinoma Overlying Dermatofibroma. Dermatopathology. 2025; 12(2):10. https://doi.org/10.3390/dermatopathology12020010
Chicago/Turabian StyleMakansi, Amal, Charlotta Enerbäck, Maria Madentzoglou, Georgios Kravvas, and Sandra Jerkovic Gulin. 2025. "Uncommon Collision Tumors: Dermoscopic and Histopathological Features of Basal Cell Carcinoma Overlying Dermatofibroma" Dermatopathology 12, no. 2: 10. https://doi.org/10.3390/dermatopathology12020010
APA StyleMakansi, A., Enerbäck, C., Madentzoglou, M., Kravvas, G., & Gulin, S. J. (2025). Uncommon Collision Tumors: Dermoscopic and Histopathological Features of Basal Cell Carcinoma Overlying Dermatofibroma. Dermatopathology, 12(2), 10. https://doi.org/10.3390/dermatopathology12020010





