Loss of CD34 Expression within an Interstitial Dermal Lymphoid Cell Infiltrate Is a Helpful Clue to the Diagnosis of Morphea
Abstract
:1. Introduction
2. Case Report
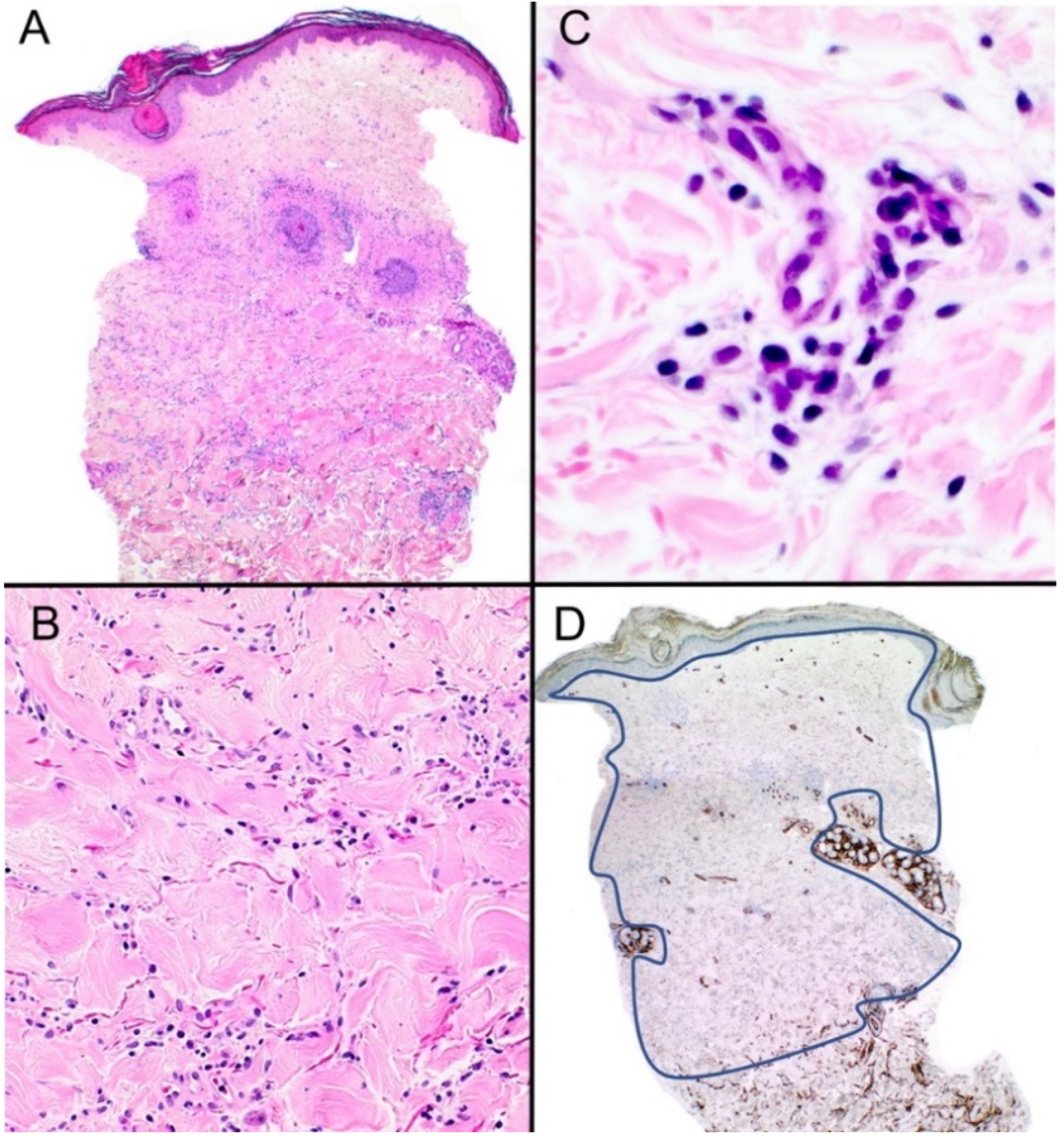
2.1. Case (1)
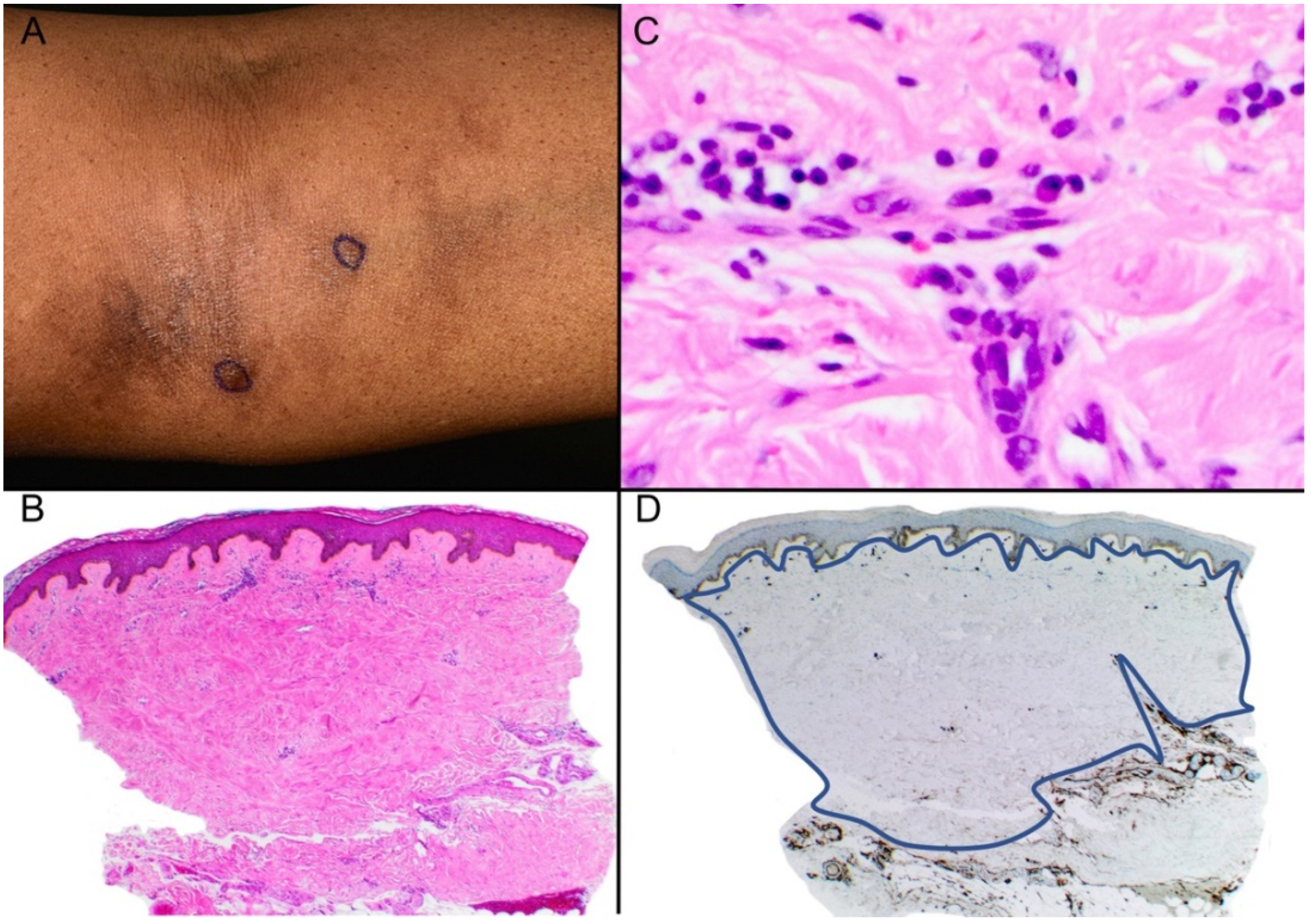
2.2. Case (2)
2.3. Case (3)
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Chiu, Y.E.; Abban, C.Y.; Konicke, K.; Segura, A.; Sokumbi, O. Histopathologic Spectrum of Morphea. Am. J. Dermatopathol. 2021, 43, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Jindal, R.; Shirazi, N.; Chauhan, P. Histopathology of morphea: Sensitivity of various named signs, a retrospective study. Indian J. Pathol. Microbiol. 2020, 63, 600–603. [Google Scholar] [CrossRef]
- Böer-Auer, A. Interstitial dermal infiltrate: An intriguing pattern. Diagn. Histopathol. 2020, 27, 13–25. [Google Scholar] [CrossRef]
- Lee, J.S.; Park, H.S.; Yoon, H.S.; Chung, J.H.; Cho, S. CD34 stromal expression is inversely proportional to smooth muscle actin expression and extent of morphea. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 2208–2216. [Google Scholar] [CrossRef] [PubMed]
- Skobieranda, K.; Helm, K.F. Decreased expression of the human progenitor cell antigen (CD34) in morphea. Am. J. Dermatopathol. 1995, 17, 471–475. [Google Scholar] [CrossRef] [PubMed]
- Aiba, S.; Tabata, N.; Ohtani, H.; Tagami, H. CD34+ spindle-shaped cells selectively disappear from the skin lesion of scleroderma. Arch. Dermatol. 1994, 130, 593–597. [Google Scholar] [CrossRef] [PubMed]
- Borretta, L.J.; Crawford, R.I. CD34 Staining in Disorders of Collagen Degeneration Other Than Morphea. Am. J. Dermatopathol. 2020, 42, 623–624. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.M.C.; Borretta, L.J.; Crawford, R.I. CD34 Staining as a Useful Tool in Disorders of Collagen Degeneration. Am. J. Dermatopathol. 2022, 44, 103–105. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, P.E.; Pinto, F.J. The histologic spectrum of mycosis fungoides/Sézary syndrome (cutaneous T-cell lymphoma). A review of 222 biopsies, including newly described patterns and the earliest pathologic changes. Am. J. Surg. Pathol. 1994, 18, 645–667. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.; Fagan, K.K.; Grider, D.J. Interstitial Mycosis Fungoides: An Unusual Mimic of Interstitial Granuloma Annulare Not to Miss. Case Rep. Dermatol. Med. 2022, 2022, 3506738. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Daruish, M.; Zidan, A.; Greenblatt, D.T.; Stefanato, C.M. Loss of CD34 Expression within an Interstitial Dermal Lymphoid Cell Infiltrate Is a Helpful Clue to the Diagnosis of Morphea. Dermatopathology 2023, 10, 70-74. https://doi.org/10.3390/dermatopathology10010010
Daruish M, Zidan A, Greenblatt DT, Stefanato CM. Loss of CD34 Expression within an Interstitial Dermal Lymphoid Cell Infiltrate Is a Helpful Clue to the Diagnosis of Morphea. Dermatopathology. 2023; 10(1):70-74. https://doi.org/10.3390/dermatopathology10010010
Chicago/Turabian StyleDaruish, Maged, Anoud Zidan, Danielle T. Greenblatt, and Catherine M. Stefanato. 2023. "Loss of CD34 Expression within an Interstitial Dermal Lymphoid Cell Infiltrate Is a Helpful Clue to the Diagnosis of Morphea" Dermatopathology 10, no. 1: 70-74. https://doi.org/10.3390/dermatopathology10010010
APA StyleDaruish, M., Zidan, A., Greenblatt, D. T., & Stefanato, C. M. (2023). Loss of CD34 Expression within an Interstitial Dermal Lymphoid Cell Infiltrate Is a Helpful Clue to the Diagnosis of Morphea. Dermatopathology, 10(1), 70-74. https://doi.org/10.3390/dermatopathology10010010







