Self-Regulation Mediates the Relationship Between Stress and Quality of Life in Shift-Working Healthcare Professionals: Behavioral Clustering Insights
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
- Perceived Stress Scale—4 item version (PSS-4):
- Executive Skills Questionnaire—Revised (ESQ-R):
- Quality of Life Scale (QOLS):
2.3. Statistical Analysis
3. Results
3.1. Self-Regulation as a Mediator in the Effect of Perceived Stress on Quality of Life
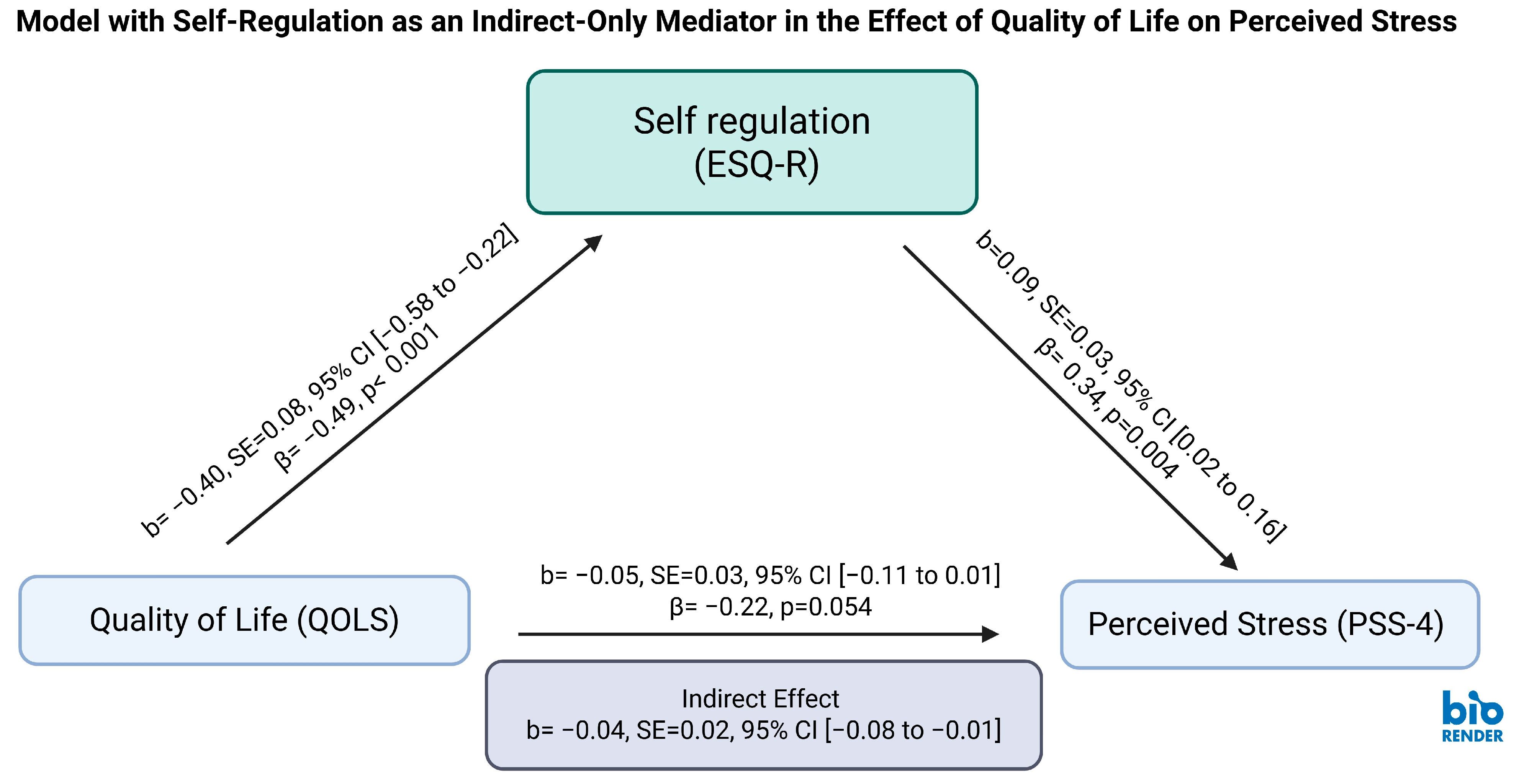
3.2. Self-Regulation Partially Mediates the Relationship Between Quality of Life and Perceived Stress
3.3. K-Means Analysis Identifies Behavioral Phenotypes Among Shift-Working Healthcare Professionals
- Cluster 0 (“resilient cluster”) included participants with relatively high stress (M = 8.58) but moderate regulation difficulty (M = 23.73) and preserved QOL (M = 86.97).
- Cluster 1 (“low-strain cluster”) represented individuals with low stress (M = 3.84), low regulation difficulty (M = 15.00), and high QOL (M = 97.34).
- Cluster 2 (“high-strain cluster”) exhibited elevated stress (M = 9.36), severe regulation difficulty (M = 40.36), and markedly reduced QOL (M = 67.64).
4. Discussion
4.1. Self-Regulation as a Mediator Between Stress and Quality of Life
4.2. Behavioral Profiles Support Personalized Intervention Targets
4.3. Quality of Life Exhibits a Partial Indirect Effect on Stress via Self-Regulation
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Academy of Sleep Medicine. (2014). International classification of sleep disorders: Diagnostic and coding manual (3rd ed.). American Academy of Sleep Medicine. [Google Scholar]
- Bakker, A. B., & Demerouti, E. (2017). Job demands-resources theory: Taking stock and looking forward. Journal of Occupational Health Psychology, 22, 273–285. [Google Scholar] [CrossRef]
- Barnett, I., Torous, J., Staples, P., Sandoval, L., Keshavan, M., & Onnela, J. P. (2018). Relapse prediction in schizophrenia through digital phenotyping: A pilot study. Neuropsychopharmacology, 43, 1660–1666. [Google Scholar] [CrossRef]
- Batanda, I. (2024). Prevalence of burnout among healthcare professionals: A survey at fort portal regional referral hospital. NPJ Mental Health Research, 3, 16. [Google Scholar] [CrossRef]
- Baumeister, R. F., Bratslavsky, E., Muraven, M., & Tice, D. M. (1998). Ego depletion: Is the active self a limited resource? Journal of Personality and Social Psychology, 74, 1252–1265. [Google Scholar] [CrossRef] [PubMed]
- Baumeister, R. F., Vohs, K. D., & Tice, D. M. (2007). The strength model of self-control. Current Directions in Psychological Science, 16, 351–355. [Google Scholar] [CrossRef]
- Billore, S., Anisimova, T., & Vrontis, D. (2023). Self-regulation and goal-directed behavior: A systematic literature review, public policy recommendations, and research agenda. Journal of Business Research, 156, 113435. [Google Scholar] [CrossRef]
- Burckhardt, C. S., & Anderson, K. L. (2003). The Quality of Life Scale (QOLS): Reliability, validity, and utilization. Health and Quality of Life Outcomes, 1, 60. [Google Scholar] [CrossRef]
- Cates, M. E., Clark, A., Woolley, T. W., & Saunders, A. (2015). Sleep quality among pharmacy students. American Journal of Pharmaceutical Education, 79, 9. [Google Scholar] [CrossRef]
- Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396. [Google Scholar] [CrossRef]
- Cutuli, D. (2014). Cognitive reappraisal and expressive suppression strategies role in the emotion regulation: An overview on their modulatory effects and neural correlates. Frontiers in Systems Neuroscience, 8, 175. [Google Scholar] [CrossRef]
- da Silva, C. C. M., Santos, A. B. D., Leoci, I. C., Leite, E. G., Antunes, E. P., Torres, W., Mesquita, E. D. L., Delfino, L. D., & Beretta, V. S. (2024). The association between perceived stress, quality of life, and level of physical activity in public school teachers. International Journal of Environmental Research and Public Health, 21, 88. [Google Scholar] [CrossRef]
- Dawson, P., & Guare, R. (2016). The smart but scattered guide to success: How to use your brain’s executive skills to keep up, stay calm, and get organized at work and at home. The Guilford Press. [Google Scholar]
- Deci, E. L., & Ryan, R. M. (2000). The “what” and “why” of goal pursuits: Human needs and the self-determination of behavior. Psychological Inquiry, 11, 227–268. [Google Scholar] [CrossRef]
- Drysdale, A. T., Grosenick, L., Downar, J., Dunlop, K., Mansouri, F., Meng, Y., Fetcho, R. N., Zebley, B., Oathes, D. J., Etkin, A., Schatzberg, A. F., Sudheimer, K., Keller, J., Mayberg, H. S., Gunning, F. M., Alexopoulos, G. S., Fox, M. D., Pascual-Leone, A., Voss, H. U., … Liston, C. (2017). Resting-state connectivity biomarkers define neurophysiological subtypes of depression. Nature Medicine, 23, 28–38. [Google Scholar] [CrossRef]
- Ghosh, S., Kim, S., Ijaz, M. F., Singh, P. K., & Mahmud, M. (2022). Classification of mental stress from wearable physiological sensors using image-encoding-based deep neural network. Biosensors, 12, 1153. [Google Scholar] [CrossRef] [PubMed]
- Gross, J. J. (1998). The emerging field of emotion regulation: An integrative review. Review of General Psychology, 2(3), 271–299. [Google Scholar] [CrossRef]
- Hagemann, T. M., Reed, B. N., Bradley, B. A., Clements, J. N., Cohen, L. J., Coon, S. A., Derington, C. G., DiScala, S. L., El-Ibiary, S., Lee, K. C., May, A., Oh, S., Phillips, J. A., & Rogers, K. M. (2020). Burnout among clinical pharmacists: Causes, interventions, and a call to action. Journal of the American College of Clinical Pharmacy, 3, 832–842. [Google Scholar] [CrossRef]
- Hayes, A. F. (2017). Partial, conditional, and moderated moderated mediation: Quantification, inference, and interpretation. Communication Monographs, 85, 4–40. [Google Scholar] [CrossRef]
- Heatherton, T. F. (2011). Neuroscience of self and self-regulation. Annual Review of Psychology, 62, 363–390. [Google Scholar] [CrossRef]
- Huckvale, K., Venkatesh, S., & Christensen, H. (2019). Toward clinical digital phenotyping: A timely opportunity to consider purpose, quality, and safety. NPJ Digital Medicine, 2, 88. [Google Scholar] [CrossRef]
- Hudon, A., Beaudoin, M., Phraxayavong, K., Potvin, S., & Dumais, A. (2023). Unsupervised machine learning driven analysis of verbatims of treatment-resistant schizophrenia patients having followed avatar therapy. Journal of Personalized Medicine, 13, 801. [Google Scholar] [CrossRef]
- Insel, T. R. (2014). The NIMH Research Domain Criteria (RDoC) Project: Precision medicine for psychiatry. American Journal of Psychiatry, 171, 395–397. [Google Scholar] [CrossRef]
- Jehan, S., Zizi, F., Pandi-Perumal, S. R., Myers, A. K., Auguste, E., Jean-Louis, G., & McFarlane, S. I. (2017). Shift work and sleep: Medical implications and management. Sleep Medicine and Disorders: International Journal, 1(2), 00008. [Google Scholar] [CrossRef]
- Johnson, J. K., Lui, L. Y., & Yaffe, K. (2007). Executive function, more than global cognition, predicts functional decline and mortality in elderly women. Journal of Gerontology: Series A, Biological Sciences and Medical Sciences, 62, 1134–1141. [Google Scholar] [CrossRef]
- Kadović, M., Mikšić, Š., & Lovrić, R. (2022). Ability of emotional regulation and control as a stress predictor in healthcare professionals. International Journal of Environmental Research and Public Health, 20, 541. [Google Scholar] [CrossRef]
- Kalisch, R., Müller, M. B., & Tüscher, O. (2015). A conceptual framework for the neurobiological study of resilience. Behavioral and Brain Sciences, 38, e92. [Google Scholar] [CrossRef]
- Kalmbach, D. A., Anderson, J. R., & Drake, C. L. (2018). The impact of stress on sleep: Pathogenic sleep reactivity as a vulnerability to insomnia and circadian disorders. Journal of Sleep Research, 27, e12710. [Google Scholar] [CrossRef]
- Kamath, J., Leon Barriera, R., Jain, N., Keisari, E., & Wang, B. (2022). Digital phenotyping in depression diagnostics: Integrating psychiatric and engineering perspectives. World Journal of Psychiatry, 12, 393–409. [Google Scholar] [CrossRef] [PubMed]
- Kapur, S., Phillips, A. G., & Insel, T. R. (2012). Why has it taken so long for biological psychiatry to develop clinical tests and what to do about it? Molecular Psychiatry, 17, 1174–1179. [Google Scholar] [CrossRef] [PubMed]
- Khan, W. A. A., Jackson, M. L., Kennedy, G. A., & Conduit, R. (2021). A field investigation of the relationship between rotating shifts, sleep, mental health and physical activity of Australian paramedics. Scientific Reports, 11, 866. [Google Scholar] [CrossRef] [PubMed]
- Kinlein, S. A., Wilson, C. D., & Karatsoreos, I. N. (2015). Dysregulated hypothalamic-pituitary-adrenal axis function contributes to altered endocrine and neurobehavioral responses to acute stress. Frontiers in Psychiatry, 6, 31. [Google Scholar] [CrossRef] [PubMed]
- Langran, C., Mantzourani, E., Hughes, L., Hall, K., & Willis, S. (2022). “I’m at breaking point”: Exploring pharmacists’ resilience, coping and burnout during the COVID-19 pandemic. Exploratory Research in Clinical and Social Pharmacy, 5, 100104. [Google Scholar] [CrossRef]
- Lazarou, E., & Exarchos, T. P. (2024). Predicting stress levels using physiological data: Real-time stress prediction models utilizing wearable devices. AIMS Neuroscience, 11, 76–102. [Google Scholar] [CrossRef]
- Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal and coping. Springer. [Google Scholar]
- Lee, Y., Ragguett, R.-M., Mansur, R. B., Boutilier, J. J., Rosenblat, J. D., Trevizol, A., Brietzke, E., Lin, K., Pan, Z., Subramaniapillai, M., Chan, T. C. Y., Fus, D., Park, C., Musial, N., Zuckerman, H., Chen, V. C.-H., Ho, R., Rong, C., & McIntyre, R. S. (2018). Applications of machine learning algorithms to predict therapeutic outcomes in depression: A meta-analysis and systematic review. Journal of Affective Disorders, 241, 519–532. [Google Scholar] [CrossRef] [PubMed]
- Lin, L., Zhang, X., & Wang, P. (2025). Interconnected stressors and well-being in healthcare professionals. Applied Research in Quality of Life, 20, 459–481. [Google Scholar] [CrossRef]
- Luciana, M. (2016). Executive function in adolescence: A commentary on regulatory control and depression in adolescents: Findings from neuroimaging and neuropsychological research. Journal of Clinical Child and Adolescent Psychology, 45, 84–89. [Google Scholar] [CrossRef]
- Luthar, S. S., & Cicchetti, D. (2000). The construct of resilience: Implications for interventions and social policies. Development and Psychopathology, 12, 857–885. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B. S. (1998). Stress, adaptation, and disease. Allostasis and allostatic load. Annals of the New York Academy of Sciences, 840, 33–44. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B. S., & Morrison, J. H. (2013). The brain on stress: Vulnerability and plasticity of the prefrontal cortex over the life course. Neuron, 79, 16–29. [Google Scholar] [CrossRef]
- Mika, A., Mazur, G. J., Hoffman, A. N., Talboom, J. S., Bimonte-Nelson, H. A., Sanabria, F., & Conrad, C. D. (2012). Chronic stress impairs prefrontal cortex-dependent response inhibition and spatial working memory. Behavioral Neuroscience, 126, 605–619. [Google Scholar] [CrossRef]
- Mohr, D. C., Zhang, M., & Schueller, S. M. (2017). Personal sensing: Understanding mental health using ubiquitous sensors and machine learning. Annual Review of Clinical Psychology, 13, 23–47. [Google Scholar] [CrossRef]
- Murry, L. T., & Witry, M. J. (2020). ‘Wasting time inside my mind’: Exploring student pharmacists’ perspectives on engaging in mindfulness oriented meditation using concepts from education research. Pharmacy Education, 20, 204–214. [Google Scholar] [CrossRef]
- Oudin, A., Maatoug, R., Bourla, A., Ferreri, F., Bonnot, O., Millet, B., Schoeller, F., Mouchabac, S., & Adrien, V. (2023). Digital phenotyping: Data-driven psychiatry to redefine mental health. Journal of Medical Internet Research, 25, e44502. [Google Scholar] [CrossRef]
- Pálfi, K., Major, J., Horváth-Sarródi, A., Deák, A., Fehér, G., & Gács, B. (2024). Adaptive emotion regulation might prevent burnout in emergency healthcare professionals: An exploratory study. BMC Public Health, 24(1), 3136. [Google Scholar] [CrossRef]
- Razai, M. S., Kooner, P., & Majeed, A. (2023). Strategies and interventions to improve healthcare professionals’ well-being and reduce burnout. Journal of Primary Care & Community Health, 14, 21501319231178641. [Google Scholar] [CrossRef] [PubMed]
- Rech, M. A., Jones, G. M., Naseman, R. W., & Beavers, C. (2022). Premature attrition of clinical pharmacists: Call to attention, action, and potential solutions. Journal of the American College of Clinical Pharmacy, 5(7), 689–696. [Google Scholar] [CrossRef]
- Rompilla, D. B., Stephens, J. E., Martinez, M., Mikels, J. A., & Haase, C. M. (2023). Can emotional acceptance buffer the link between executive functioning and mental health in late life? Emotion, 23, 2286–2299. [Google Scholar] [CrossRef]
- Salahuddin, M. F., Bugingo, R., Mahdi, F., Spencer, D., Manzar, M. D., & Paris, J. J. (2025a). Physiological and psychological impacts of shift work among student pharmacists: Sex differences in stress and health outcomes. Psychiatry International, 6(2), 47. [Google Scholar] [CrossRef]
- Salahuddin, M. F., Samuel, B. I., Bugingo, R., Spencer, D., Manzar, M. D., & BaHammam, A. S. (2025b). The mediating role of negative mood affect in the relationship between perceived stress and vulnerability to insomnia among student pharmacist shift workers. Nature and Science of Sleep, 17, 649–662. [Google Scholar] [CrossRef] [PubMed]
- Schommer, J. C., Gaither, C. A., Alvarez, N. A., Lee, S., Shaughnessy, A. M., Arya, V., Planas, L. G., Fadare, O., & Witry, M. J. (2022). Pharmacy workplace wellbeing and resilience: Themes identified from a hermeneutic phenomenological analysis with future recommendations. Pharmacy, 10(6), 158. [Google Scholar] [CrossRef]
- Seo, E. J., Ahn, J. A., Hayman, L. L., & Kim, C. J. (2018). The association between perceived stress and quality of life in university students: The parallel mediating role of depressive symptoms and health-promoting behaviors. Asian Nursing Research, 12, 190–196. [Google Scholar] [CrossRef]
- Soleimani, E., Tahmasebi, R., Daneshmandi, H., Salimi, S. H., & Aliasghari, F. (2024). Work-life balance and health among pharmacists: Physical activity, sleep quality, and general health. BMC Health Services Research, 24, 1217. [Google Scholar] [CrossRef]
- Strait, J. E., Dawson, P., Walther, C. A. P., Strait, G. G., Barton, A. K., & Brunson McClain, M. (2020). Refinement and psychometric evaluation of the executive skills questionnaire-revised. Contemporary School Psychology, 24(4), 378–388. [Google Scholar] [CrossRef]
- Ugwu, L. E., Idemudia, E. S., & Onyedibe, M. C. C. (2024). Decoding the impact of night/day shiftwork on well-being among healthcare workers. Scientific Reports, 14, 10246. [Google Scholar] [CrossRef]
- Walker, W. H., Walton, J. C., DeVries, A. C., & Nelson, R. J. (2020). Circadian rhythm disruption and mental health. Translational Psychiatry, 10, 28. [Google Scholar] [CrossRef]
- Wang, Y., Tang, S., Zhang, L., Bu, X., Lu, L., Li, H., Gao, Y., Hu, X., Kuang, W., Jia, Z., Sweeney, J. A., Gong, Q., & Huang, X. (2021). Data-driven clustering differentiates subtypes of major depressive disorder with distinct brain connectivity and symptom features. British Journal of Psychiatry, 219, 606–613. [Google Scholar] [CrossRef]
- Wettstein, A., Jenni, G., Schneider, I., Kühne, F., Grosse Holtforth, M., & La Marca, R. (2023). Predictors of psychological strain and allostatic load in teachers: Examining the long-term effects of biopsychosocial risk and protective factors using a LASSO regression approach. International Journal of Environmental Research and Public Health, 20(10), 5760. [Google Scholar] [CrossRef]
- Wickwire, E. M., Geiger-Brown, J., Scharf, S. M., & Drake, C. L. (2017). Shift work and shift work sleep disorder: Clinical and organizational perspectives. Chest, 151, 1156–1172. [Google Scholar] [CrossRef] [PubMed]
- Wolff, M., Enge, S., Kräplin, A., Krönke, K.-M., Bühringer, G., Smolka, M. N., & Goschke, T. (2021). Chronic stress, executive functioning, and real-life self-control: An experience sampling study. Journal of Personality, 89, 402–421. [Google Scholar] [CrossRef] [PubMed]
- Zeek, M. L., Savoie, M. J., Song, M., Kennemur, L. M., Qian, J., Jungnickel, P. W., & Westrick, S. C. (2015). Sleep duration and academic performance among student pharmacists. American Journal of Pharmaceutical Education, 79, 63. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Mean ± SD/ Frequency (Percentage) |
|---|---|
| Age (years) | 18–25: 32 (39%) |
| 26–45: 42 (51.2%) | |
| >45: 8 (9.8%) | |
| Gender | Male: 21 (25.6%) |
| Female: 61 (74.4%) | |
| Residence | City: 76 (92.7%) |
| Countryside: 6 (7.3%) | |
| Marital Status | Single: 66 (80.5%) |
| Married: 14 (17.1%) | |
| Divorced/Separated: 2 (2.4%) | |
| Shift Hours Per Day | Less than or equal to 8 h: 44 (53.7%) |
| 8–12 h:35 (42.6%) | |
| Greater than 12 h: 3 (3.7%) | |
| How long have you been working in the same shift? | 1–6 months: 16 (19.5%) |
| 6–12 months: 22 (26.8%) | |
| Greater than 12 months: 18 (22%) | |
| Greater than 24 months: 26 (31.7%) | |
| PSS -4 (Perceived Stress Score) | 6.49 ± 2.72 |
| ESQ- R Scores (Executive Skills Questionnaire–revised) | 21.91 ± 11.63 |
| QOLS (Quality of Life Score) | 89.18 ± 14.40 |
| Pathway | Total Effect (b) | Direct Effect (b) | Indirect Effect (b) | 95% CI (Indirect Effect) | Type of Mediation Model |
|---|---|---|---|---|---|
| Stress → Self-Regulation → Quality of Life (Forward) | −1.73 * | −0.94 | −0.79 * | [−1.63, −0.17] | Indirect-only mediation |
| Quality of Life → Self-Regulation → Stress (Reverse) | −0.09 * | −0.05 | −0.04 * | [−0.08, −0.01] | Indirect-only mediation |
| Cluster | PSS (Stress) Mean ± SD | ESQ-R (Regulation Difficulty) Mean ± SD | QOL (Quality of Life) Mean ± SD | Interpretation |
|---|---|---|---|---|
| 0 | 8.58 ± 2.11 | 23.73 ± 8.71 | 86.97 ± 11.53 |  High stress, moderate regulation difficulty, but high QOL—resilient cluster High stress, moderate regulation difficulty, but high QOL—resilient cluster |
| 1 | 3.84 ± 2.06 | 15.00 ± 6.70 | 97.34 ± 10.18 |  Low stress, low regulation difficulty, high QOL—low-strain cluster Low stress, low regulation difficulty, high QOL—low-strain cluster |
| 2 | 9.36 ± 1.96 | 40.36 ± 10.93 | 67.64 ± 9.55 |  High stress, high regulation difficulty, low QOL—high-strain cluster High stress, high regulation difficulty, low QOL—high-strain cluster |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the University Association of Education and Psychology. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salahuddin, M.F.; Walker, J.; Zambrana, E.H.; Gupta, V.; Jung, K.; Pandi-Perumal, S.R.; Manzar, M.D. Self-Regulation Mediates the Relationship Between Stress and Quality of Life in Shift-Working Healthcare Professionals: Behavioral Clustering Insights. Eur. J. Investig. Health Psychol. Educ. 2025, 15, 180. https://doi.org/10.3390/ejihpe15090180
Salahuddin MF, Walker J, Zambrana EH, Gupta V, Jung K, Pandi-Perumal SR, Manzar MD. Self-Regulation Mediates the Relationship Between Stress and Quality of Life in Shift-Working Healthcare Professionals: Behavioral Clustering Insights. European Journal of Investigation in Health, Psychology and Education. 2025; 15(9):180. https://doi.org/10.3390/ejihpe15090180
Chicago/Turabian StyleSalahuddin, Mohammed F., Jessica Walker, Ernesto Hernandez Zambrana, Vibhuti Gupta, Kwanghee Jung, Seithikurippu R. Pandi-Perumal, and Md Dilshad Manzar. 2025. "Self-Regulation Mediates the Relationship Between Stress and Quality of Life in Shift-Working Healthcare Professionals: Behavioral Clustering Insights" European Journal of Investigation in Health, Psychology and Education 15, no. 9: 180. https://doi.org/10.3390/ejihpe15090180
APA StyleSalahuddin, M. F., Walker, J., Zambrana, E. H., Gupta, V., Jung, K., Pandi-Perumal, S. R., & Manzar, M. D. (2025). Self-Regulation Mediates the Relationship Between Stress and Quality of Life in Shift-Working Healthcare Professionals: Behavioral Clustering Insights. European Journal of Investigation in Health, Psychology and Education, 15(9), 180. https://doi.org/10.3390/ejihpe15090180











