Network Structure of Post-Traumatic Stress and Social/Emotional/Behavioral Difficulties in a Post-Earthquake Child and Adolescent Sample
Abstract
1. Introduction
2. Materials and Method
2.1. Participants and Procedure
2.2. Measures
- Exposure: an ad hoc questionnaire was developed to gather demographic information and data on the extent of exposure to the earthquake. It included questions about personal, family, or friends’ injuries or deaths, property damage, displacement. The questionnaire used a binary scale (“yes” = 1, “no” = 0) to assess each item (Forresi et al., 2020). For primary school children, the interviewer administered the questionnaires, while secondary school children and adolescents completed the questionnaires on their own.
- UCLA Post-Traumatic Stress Disorder Reaction Index (PTSD-RI; R. Pynoos et al., 1998): This instrument, designed for children and adolescents aged 7–17 who have experienced a potentially traumatic event, screening for trauma exposure and PTSD symptoms as defined by DSM-IV. It is widely used and well-validated (Steinberg et al., 2004). As described in the scoring sheet provided by the developers of the PTSD-RI, the questionnaire includes 20 items rated on a five-point Likert-type scale, allowing calculation of severity scores of three symptoms clusters (Reexperiencing, Avoidance, and Increased Arousal) as well as an overall total severity score (R. Pynoos et al., 1998). High internal consistency has been reported with a Cronbach’s alpha of 0.90, and test–retest reliability of 0.84 (Steinberg et al., 2004). Although no formal Italian validation exists, the questionnaire was translated following rigorous standards, including independent back-translation (Goenjian et al., 1995). Within the present sample, the analysis revealed a Cronbach’s alpha of 0.84 reflecting a strong internal consistency, comparable to the data from the original instrument.
- Strengths and Difficulties Questionnaire (SDQ; R. Goodman, 1997; Italian version: Tobia et al., 2013): The SDQ is a 25-item screening instrument for emotional and behavioral problems in children and adolescents, organized into five subscales of five items each: Emotional Problems, Conduct Problems, Hyperactivity–Inattention, Peer Relationship Problems, and Prosocial Behavior. Items are rated on a three-point Likert scale (“not true,” “somewhat true,” “certainly true”). An overall difficulty score (0–40) is obtained by summing the first four subscales (excluding Prosocial Behavior). Italian normative data are available (Tobia & Marzocchi, 2018), and the Italian SDQ has demonstrated solid psychometric properties, with subscale Cronbach’s alphas ranging from 0.73 to 0.89 (Tobia & Marzocchi, 2018). In the present sample, internal consistency was acceptable (Cronbach’s α = 0.71).
2.3. Statistical Analysis
3. Results
3.1. Descriptives
3.2. Network Analysis
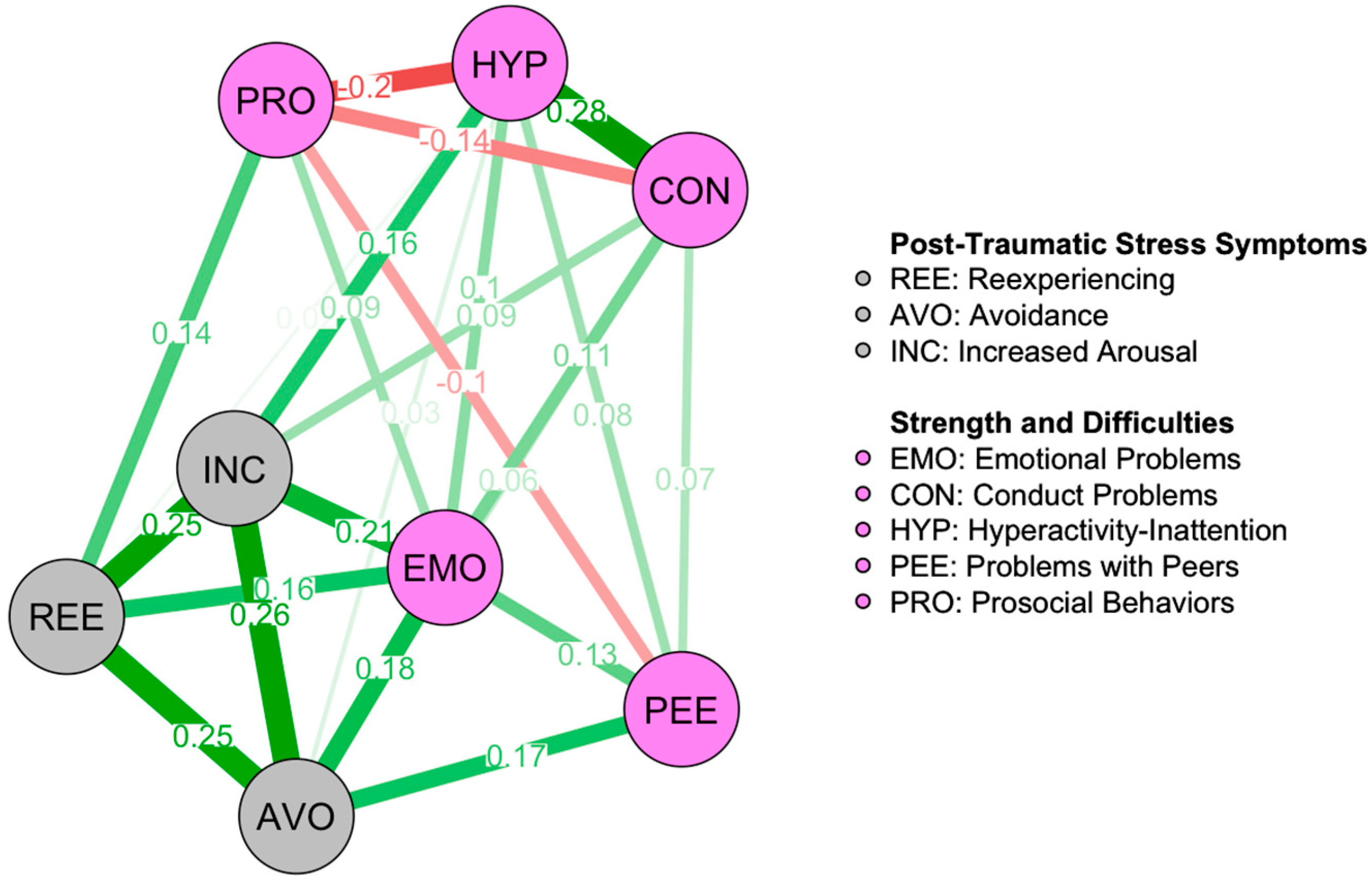
3.2.1. Overall Sample
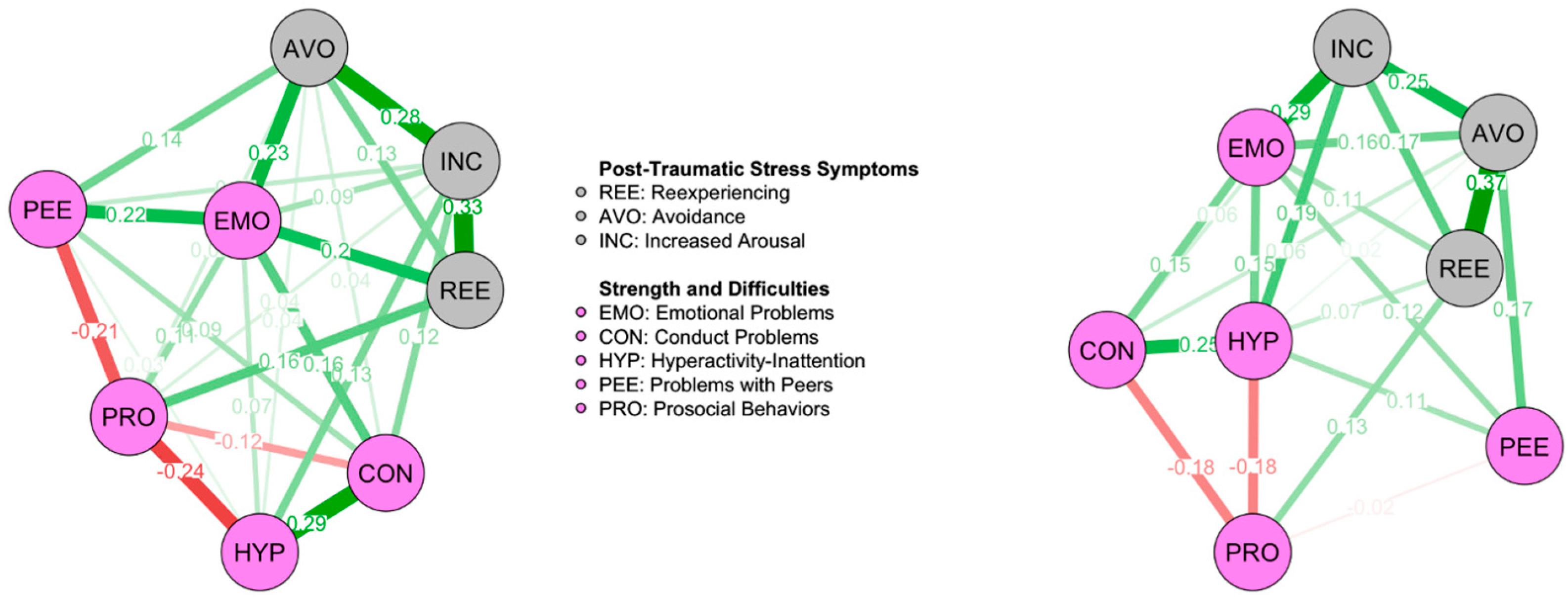
3.2.2. Network Comparison According to Gender
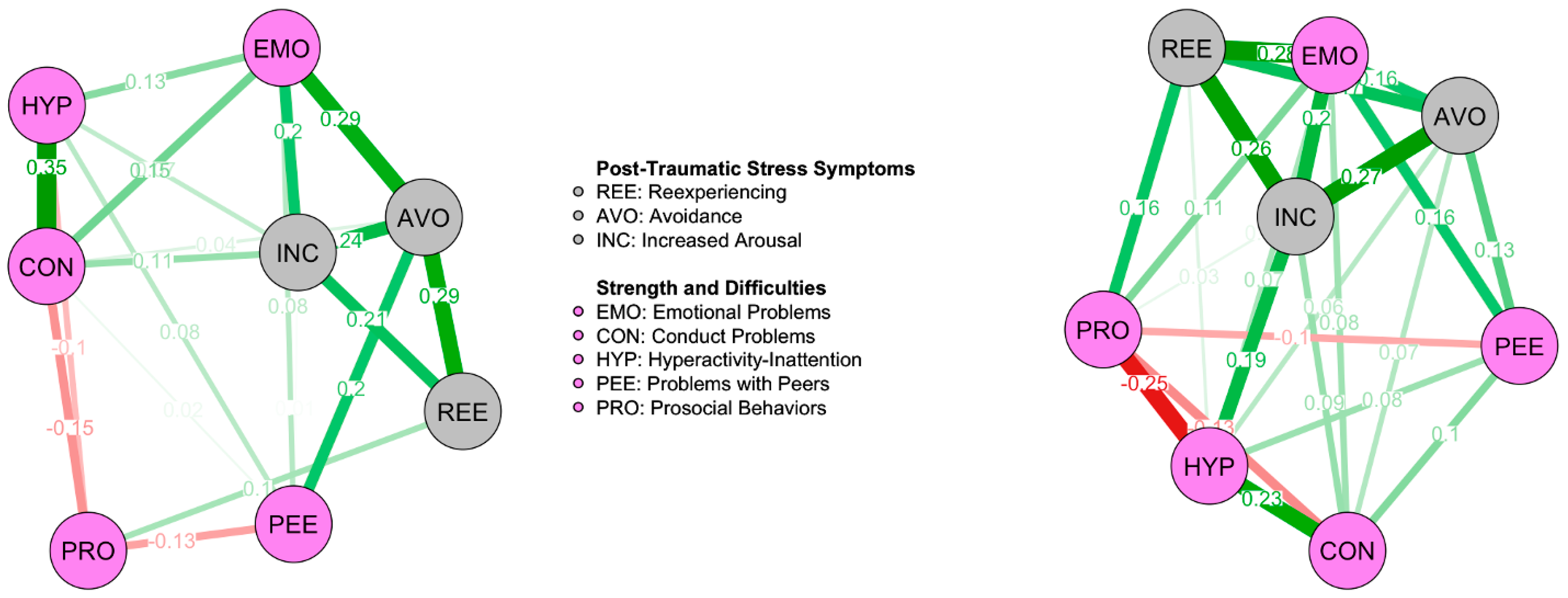
3.2.3. Network Comparison According to Age Group
3.2.4. Network Comparison According to Proximity to the Epicenter
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alisic, E., Zalta, A. K., Van Wesel, F., Larsen, S. E., Hafstad, G. S., Hassanpour, K., & Smid, G. E. (2014). Rates of post-traumatic stress disorder in trauma-exposed children and adolescents: Meta-analysis. The British Journal of Psychiatry, 204(5), 335–340. [Google Scholar] [CrossRef]
- American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders, fifth edition, text revision, DSM-5-TR. American Psychiatric Association Publishing. [Google Scholar]
- Armour, C., Greene, T., Contractor, A. A., Weiss, N., Dixon-Gordon, K., & Ross, J. (2020). Post-traumatic stress disorder symptoms and reckless behaviors: A network analysis approach. Journal of Traumatic Stress, 33(1), 29–40. [Google Scholar] [CrossRef]
- Bastien, R. J.-B., Jongsma, H. E., Kabadayi, M., & Billings, J. (2020). The effectiveness of psychological interventions for post-traumatic stress disorder in children, adolescents and young adults: A systematic review and meta-analysis. Psychological Medicine, 50(10), 1598–1612. [Google Scholar] [CrossRef]
- Benjet, C., Bromet, E., Karam, E. G., Kessler, R. C., McLaughlin, K. A., Ruscio, A. M., Shahly, V., Stein, D. J., Petukhova, M., Hill, E., Alonso, J., Atwoli, L., Bunting, B., Bruffaerts, R., Caldas-de-Almeida, J. M., de Girolamo, G., Florescu, S., Gureje, O., Huang, Y., … Koenen, K. C. (2016). The epidemiology of traumatic event exposure worldwide: Results from the World Mental Health Survey Consortium. Psychological Medicine, 46(2), 327–343. [Google Scholar] [CrossRef]
- Betancourt, T. S., Borisova, I., Williams, T. P., Meyers-Ohki, S. E., Rubin-Smith, J. E., Annan, J., & Kohrt, B. A. (2013). Research Review: Psychosocial adjustment and mental health in former child soldiers—A systematic review of the literature and recommendations for future research. Journal of Child Psychology and Psychiatry, 54(1), 17–36. [Google Scholar] [CrossRef]
- Birkeland, M. S., Greene, T., & Spiller, T. R. (2020). The network approach to post-traumatic stress disorder: A systematic review. European Journal of Psychotraumatology, 11(1), 1700614. [Google Scholar] [CrossRef]
- Borsboom, D. (2017). A network theory of mental disorders. World Psychiatry, 16(1), 5–13. [Google Scholar] [CrossRef]
- Borsboom, D., Deserno, M. K., Rhemtulla, M., Epskamp, S., Fried, E. I., McNally, R. J., Robinaugh, D. J., Perugini, M., Dalege, J., Costantini, G., Isvoranu, A.-M., Wysocki, A. C., van Borkulo, C. D., van Bork, R., & Waldorp, L. J. (2021). Network analysis of multivariate data in psychological science. Nature Reviews Methods Primers, 1(1), 58. [Google Scholar] [CrossRef]
- Brewin, C. R., Gregory, J. D., Lipton, M., & Burgess, N. (2010). Intrusive images in psychological disorders: Characteristics, neural mechanisms, and treatment implications. Psychological Review, 117(1), 210. [Google Scholar] [CrossRef]
- Briggs-Gowan, M. J., Grasso, D., Bar-Haim, Y., Voss, J., McCarthy, K. J., Pine, D. S., & Wakschlag, L. S. (2016). Attention bias in the developmental unfolding of post-traumatic stress symptoms in young children at risk. Journal of Child Psychology and Psychiatry, 57(9), 1083–1091. [Google Scholar] [CrossRef]
- Bringmann, L. F., Elmer, T., Epskamp, S., Krause, R. W., Schoch, D., Wichers, M., Wigman, J. T. W., & Snippe, E. (2019). What do centrality measures measure in psychological networks? Journal of Abnormal Psychology, 128(8), 892. [Google Scholar] [CrossRef]
- Bryant, R. A., Creamer, M., O’Donnell, M., Forbes, D., McFarlane, A. C., Silove, D., & Hadzi-Pavlovic, D. (2017). Acute and chronic post-traumatic stress symptoms in the emergence of post-traumatic stress disorder: A network analysis. JAMA Psychiatry, 74(2), 135–142. [Google Scholar] [CrossRef]
- Caffo, E., Forresi, B., & Lievers, L. S. (2005). Impact, psychological sequelae and management of trauma affecting children and adolescents. Current Opinion in Psychiatry, 18(4), 422–428. [Google Scholar] [CrossRef]
- Cao, X., Wang, L., Cao, C., Fang, R., Chen, C., Hall, B. J., & Elhai, J. D. (2019). Sex differences in global and local connectivity of adolescent post-traumatic stress disorder symptoms. Journal of Child Psychology and Psychiatry, 60(2), 216–224. [Google Scholar] [CrossRef]
- Chen, X.-Y., Li, C., & Fan, F. (2025). Post-traumatic stress disorder symptoms in mothers and adolescents after the Wenchuan earthquake: A cross-sectional and longitudinal network analysis. Journal of Affective Disorders, 368, 555–563. [Google Scholar] [CrossRef]
- Cialdini, R. B., Darby, B. L., & Vincent, J. E. (1973). Transgression and altruism: A case for hedonism. Journal of Experimental Social Psychology, 9(6), 502–516. [Google Scholar] [CrossRef]
- Cicchetti, D., & Toth, S. L. (1995). A developmental psychopathology perspective on child abuse and neglect. Journal of the American Academy of Child & Adolescent Psychiatry, 34(5), 541–565. [Google Scholar] [CrossRef]
- Crum, K. I., Cornacchio, D., Coxe, S., Green, J. G., & Comer, J. S. (2018). A latent profile analysis of co-occurring youth post-traumatic stress and conduct problems following community trauma. Journal of Child and Family Studies, 27(11), 3638–3649. [Google Scholar] [CrossRef]
- Csárdi, G., Nepusz, T., Traag, V., Horvát, S., Zanini, F., Noom, D., & Müller, K. (2025). igraph: Network analysis and visualization in R (Versione 2.1.4) [R package]. Available online: https://zenodo.org/records/17354910 (accessed on 1 January 2025).
- Dablander, F., & Hinne, M. (2019). Node centrality measures are a poor substitute for causal inference. Scientific Reports, 9(1), 6846. [Google Scholar] [CrossRef]
- El-Khodary, B., & Samara, M. (2020). The relationship between multiple exposures to violence and war trauma, and mental health and behavioural problems among Palestinian children and adolescents. European Journal of Child and Adolescent Psychiatry, 29(5), 719–731. [Google Scholar] [CrossRef]
- Engelhard, I. M., van den Hout, M. A., Weerts, J., Hox, J. J., & van Doornen, L. J. (2009). A prospective study of the relation between post-traumatic stress and physical health symptoms. International Journal of Clinical and Health Psychology, 9(3), 365–372. [Google Scholar]
- Epskamp, S., Borsboom, D., & Fried, E. I. (2018). Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods, 50, 195–212. [Google Scholar] [CrossRef]
- Epskamp, S., Cramer, A. O., Waldorp, L. J., Schmittmann, V. D., & Borsboom, D. (2012). qgraph: Network visualizations of relationships in psychometric data. Journal of Statistical Software, 48, 1–18. [Google Scholar] [CrossRef]
- Epskamp, S., & Fried, E. I. (2018). A tutorial on regularized partial correlation networks. Psychological Methods, 23(4), 617. [Google Scholar] [CrossRef]
- Forresi, B., Caputi, M., Scaini, S., Caffo, E., Aggazzotti, G., & Righi, E. (2021). Parental internalizing psychopathology and PTSD in offspring after the 2012 earthquake in Italy. Children, 8(10), 930. [Google Scholar] [CrossRef]
- Forresi, B., Soncini, F., Bottosso, E., Di Pietro, E., Scarpini, G., Scaini, S., Aggazzotti, G., Caffo, E., & Righi, E. (2020). Post-traumatic stress disorder, emotional and behavioral difficulties in children and adolescents 2 years after the 2012 earthquake in Italy: An epidemiological cross-sectional study. European Child & Adolescent Psychiatry, 29, 227–238. [Google Scholar] [CrossRef]
- Friedman, M. J. (2013). Finalizing PTSD in DSM-5: Getting here from there and where to go next. Journal of Traumatic Stress, 26(5), 548–556. [Google Scholar] [CrossRef]
- Friedman, M. J., Hastie, T., & Tibshirani, R. (2014). glasso: Graphical lasso-estimation of Gaussian graphical models. R package version, 1(8). Available online: http://www-stat.stanford.edu/~tibs/glasso (accessed on 1 January 2025).
- Furr, J. M., Comer, J. S., Edmunds, J. M., & Kendall, P. C. (2010). Disasters and youth: A meta-analytic examination of post-traumatic stress. Journal of Consulting and Clinical Psychology, 78(6), 765–780. [Google Scholar] [CrossRef] [PubMed]
- Galatzer-Levy, I. R., & Bryant, R. A. (2013). 636,120 ways to have post-traumatic stress disorder. Perspectives on Psychological Science, 8(6), 651–662. [Google Scholar] [CrossRef]
- Gauthier-Duchesne, A., Hébert, M., & Daspe, M. È. (2017). Gender as a predictor of post-traumatic stress symptoms and externalizing behavior problems in sexually abused children. Child Abuse & Neglect, 64, 79–88. [Google Scholar] [CrossRef]
- Gkintoni, E., Kourkoutas, E., Yotsidi, V., Stavrou, P. D., & Prinianaki, D. (2024). Clinical efficacy of psychotherapeutic interventions for post-traumatic stress disorder in children and adolescents: A systematic review and analysis. Children, 11(5), 579. [Google Scholar] [CrossRef]
- Goenjian, A. K., Pynoos, R. S., Steinberg, A. M., Najarian, L. M., Asarnow, J. R., Karayan, I., Ghurabi, M., & Fairbanks, L. A. (1995). Psychiatric comorbidity in children after the 1988: Earthquake in Armenia. Journal of the American Academy of Child & Adolescent Psychiatry, 34(9), 1174–1184. [Google Scholar] [CrossRef]
- Goodman, A., Lamping, D. L., & Ploubidis, G. B. (2010). When to use broader internalising and externalising subscales instead of the hypothesised five subscales on the Strengths and Difficulties Questionnaire (SDQ): Data from British parents, teachers and children. Journal of Abnormal Child Psychology, 38, 1179–1191. [Google Scholar] [CrossRef]
- Goodman, R. (1997). The strengths and difficulties questionnaire: A research note. Journal of Child Psychology and Psychiatry, 38(5), 581–586. [Google Scholar] [CrossRef]
- Grasser, L. R., Winters, S., Reda, M. H., France, J., Davie, W., Stenson, A. F., Marusak, H. A., & Jovanovic, T. (2023). The fear that remains: Associations between trauma-related psychopathology and fear-potentiated startle in youth resettled as refugees. Journal of Traumatic Stress, 36(3), 265–275. [Google Scholar] [CrossRef]
- Greene, T., Gelkopf, M., Fried, E. I., Robinaugh, D. J., & Lapid Pickman, L. (2020). Dynamic network analysis of negative emotions and DSM-5 post-traumatic stress disorder symptom clusters during conflict. Journal of Traumatic Stress, 33(1), 72–83. [Google Scholar] [CrossRef]
- Haslbeck, J. M., & Waldorp, L. J. (2020). mgm: Estimating time-varying mixed graphical models in high-dimensional data. Journal of Statistical Software, 93, 1–46. [Google Scholar] [CrossRef]
- Helpman, L., Rachamim, L., Aderka, I. M., Gabai-Daie, A., Schindel-Allon, I., & Gilboa-Schechtman, E. (2015). Post-traumatic symptom structure across age groups. Journal of Clinical Child & Adolescent Psychology, 44(4), 630–639. [Google Scholar] [CrossRef]
- IBM Corp. (2023). IBM SPSS statistics for windows. Version 29. IBM Corp. [Google Scholar]
- Isvoranu, A. M., Epskamp, S., & Cheung, M. W. L. (2021). Network models of post-traumatic stress disorder: A meta-analysis. Journal of Abnormal Psychology, 130(8), 841. [Google Scholar] [CrossRef]
- Jones, P. J. (2017). networktools: Tools for identifying important nodes in networks (Versione 1.6.0) [R package]. CRAN. [Google Scholar] [CrossRef]
- Jonkman, C. S., Verlinden, E., Bolle, E. A., Boer, F., & Lindauer, R. J. (2013). Traumatic stress symptomatology after child maltreatment and single traumatic events: Different profiles. Journal of Traumatic Stress, 26(2), 225–232. [Google Scholar] [CrossRef]
- Juen, F., Hecker, T., Hermenau, K., Teicher, M. H., Mikinga, G., Nkuba, M., Masath, F. B., & Schalinski, I. (2024). Child maltreatment in a high adversity context: Associations of age, type and timing of exposure with psychopathology in middle childhood. Child Abuse and Negectl, 157, 107060. [Google Scholar] [CrossRef]
- Keya, T. A., Leela, A., Habib, N., Rashid, M., Bakthavatchalam, P., & Habib, N. (2023). Mental health disorders due to disaster exposure: A systematic review and meta-analysis. Cureus, 15(4), e37031. [Google Scholar] [CrossRef]
- Kilpatrick, D. G., Resnick, H. S., Milanak, M. E., Miller, M. W., Keyes, K. M., & Friedman, M. J. (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. Journal of Traumatic Stress, 26(5), 537–547. [Google Scholar] [CrossRef]
- Kim, J., & Cicchetti, D. (2010). Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. Journal of Child Psychology and Psychiatry, 51(6), 706–716. [Google Scholar] [CrossRef] [PubMed]
- La Greca, A. M., Silverman, W. K., Vernberg, E. M., & Roberts, M. C. (2002). Children and disasters: Future directions for research and public policy. School Psychology Review, 31(4), 498–509. [Google Scholar]
- La Greca, A. M., Vernberg, E. M., Silverman, W. K., Vogel, A. L., & Prinstein, M. J. (2001). Helping children cope with disasters: A manual for professionals working with elementary school children. Retrieved April, 1, 2008. [Google Scholar]
- Lai, B. S., La Greca, A. M., Colgan, C. A., Herge, W., Chan, S., Medzhitova, J., Short, M., & Auslander, B. (2020). Sleep problems and post-traumatic stress: Children exposed to a natural disaster. Journal of Pediatric Psychology, 45(9), 1016–1026. [Google Scholar] [CrossRef] [PubMed]
- Larsen, S. E., Fleming, C. J. E., & Resick, P. A. (2019). Residual symptoms following empirically supported treatment for PTSD. Psychological Trauma: Theory, Research, Practice, and Policy, 11(2), 207–215. [Google Scholar] [CrossRef]
- Liebman, R. E., Becker, K. R., Smith, K. E., Cao, L., Keshishian, A. C., Crosby, R. D., Eddy, K. T., & Thomas, J. J. (2021). Network analysis of post-traumatic stress and eating disorder symptoms in a community sample of adults exposed to childhood abuse. Journal of Traumatic Stress, 34(3), 665–674. [Google Scholar] [CrossRef]
- Lissek, S., & van Meurs, B. (2015). Learning models of PTSD: Theoretical accounts and psychobiological evidence. International Journal of Psychophysiology, 98(3), 594–605. [Google Scholar] [CrossRef]
- Mann, M., Li, J., Farfel, M. R., Maslow, C. B., Osahan, S., & Stellman, S. D. (2015). Adolescent behavior and PTSD 6–7 years after the World Trade Center terrorist attacks of September 11, 2001. Disaster Health, 2(3–4), 121–129. [Google Scholar] [CrossRef]
- McDermott, B. M., Lee, E. M., Judd, M., & Gibbon, P. (2005). Post-traumatic stress disorder and general psychopathology in children and adolescents following a wildfire disaster. Canadian Journal of Psychiatry, 50(3), 137–143. [Google Scholar] [CrossRef]
- McGuire, J. F., Orr, S. P., Essoe, J. K., McCracken, J. T., Storch, E. A., & Piacentini, J. (2016). Extinction learning in childhood anxiety disorders, obsessive-compulsive disorder and post-traumatic stress disorder: Implications for treatment. Expert Review of Neurotherapeutics, 16(10), 1155–1174. [Google Scholar] [CrossRef]
- McLaughlin, K. A., Green, J. G., Gruber, M. J., Sampson, N. A., Zaslavsky, A. M., & Kessler, R. C. (2012). Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. Archives of General Psychiatry, 69(11), 1151–1160. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, K. A., & Lambert, H. K. (2017). Child trauma exposure and psychopathology: Mechanisms of risk and resilience. Current Opinion in Psychology, 14, 29–34. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, K. A., Sheridan, M. A., & Lambert, H. K. (2014). Childhood adversity and neural development: Deprivation and threat as distinct dimensions of early experience. Neuroscience & Biobehavioral Reviews, 47, 578–591. [Google Scholar] [CrossRef]
- McNally, R. J., Heeren, A., & Robinaugh, D. J. (2017). A Bayesian network analysis of post-traumatic stress disorder symptoms in adults reporting childhood sexual abuse. European Journal of Psychotraumatology, 8(Suppl. S3), 1341276. [Google Scholar] [CrossRef]
- McNally, R. J., Robinaugh, D. J., Wu, G. W. Y., Wang, L., Deserno, M., & Borsboom, D. (2015). Mental disorders as causal systems: A network approach to post-traumatic stress disorder. Clinical Psychological Science, 3(6), 836–849. [Google Scholar] [CrossRef]
- Meiser-Stedman, R., McKinnon, A., Dixon, C., Boyle, A., Smith, P., & Dalgleish, T. (2019). A core role for cognitive processes in the acute onset and maintenance of post-traumatic stress in children and adolescents. Journal of Child Psychology and Psychiatry, 60(8), 875–884. [Google Scholar] [CrossRef] [PubMed]
- Misitano, A., Michelini, G., & Oppo, A. (2024). Understanding suicidal ideation through psychological flexibility and inflexibility: A network analysis perspective. Journal of Contextual Behavioral Science, 34, 100853. [Google Scholar] [CrossRef]
- Newnham, E. A., Mergelsberg, E. L., Chen, Y., Kim, Y., Gibbs, L., Dzidic, P. L., DaSilva, M. I., Chan, E. Y. Y., Shimomura, K., Narita, Z., Huang, Z., & Leaning, J. (2022). Long term mental health trajectories after disasters and pandemics: A multilingual systematic review of prevalence, risk and protective factors. Clinical Psychology Review, 97, 102203. [Google Scholar] [CrossRef]
- Nolting, I. K. L., Morina, N., Hoppen, T. H., Tam, K. P., & Kip, A. (2025). A meta-analysis on gender differences in prevalence estimates of mental disorders following exposure to natural hazards. European Journal of Psychotraumatology, 16(1), 2476809. [Google Scholar] [CrossRef]
- Norris, F. H., Friedman, M. J., & Watson, P. J. (2002a). 60,000 disaster victims speak: Part II. Summary and implications of disaster mental health research. Psychiatry, 65, 240–260. [Google Scholar] [CrossRef] [PubMed]
- Norris, F. H., Friedman, M. J., Watson, P. J., Byrne, C. M., Diaz, E., & Kaniasty, K. (2002b). 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981–2001. Psychiatry, 65(3), 207–239. [Google Scholar] [CrossRef]
- Olff, M. (2017). Sex and gender differences in post-traumatic stress disorder: An update. European Journal of Psychotraumatology, 8(Suppl. S4), 1351204. [Google Scholar] [CrossRef]
- Pine, D. S., Costello, E. J., & Masten, A. S. (2005). Trauma, proximity, and developmental psychopathology: The effects of war and terrorism on children. Neuropsychopharmacology, 30(10), 1781–1792. [Google Scholar] [CrossRef] [PubMed]
- Pynoos, R., Rodriguez, N., Steinberg, A., Stuber, M., & Frederick, C. (1998). UCLA PTSD index for DSM-IV. UCLA Trauma Psychiatry Service. [Google Scholar]
- Pynoos, R. S., Steinberg, A. M., & Piacentini, J. C. (1999). A developmental psychopathology model of childhood traumatic stress and intersection with anxiety disorders. Biological Psychiatry, 46(11), 1542–1554. [Google Scholar] [CrossRef] [PubMed]
- Qi, J., Ye, Y., Sun, R., Zhen, R., & Zhou, X. (2023). Comorbidity of post-traumatic stress disorder and depression among adolescents following an earthquake: A longitudinal study based on network analysis. Journal of Affective Disorders, 324, 354–363. [Google Scholar] [CrossRef]
- Quax, R., Apolloni, A., & Sloot, P. M. (2013). The diminishing role of hubs in dynamical processes on complex networks. Journal of The Royal Society Interface, 10(88), 20130568. [Google Scholar] [CrossRef]
- R Core Team. (2024). R: A language and environment for statistical computing (Versione 4.4.1) [Software]. R Foundation for Statistical Computing. [Google Scholar]
- Rezayat, A. A., Sahebdel, S., Jafari, S., Kabirian, A., Rahnejat, A. M., Farahani, R. H., Mosaed, R., & Nour, M. G. (2020). Evaluating the prevalence of PTSD among children and adolescents after earthquakes and floods: A systematic review and meta-analysis. Psychiatric Quarterly, 91, 1265–1290. [Google Scholar] [CrossRef] [PubMed]
- Rossi, R., Socci, V., Pacitti, F., Carmassi, C., Rossi, A., Di Lorenzo, G., & Hyland, P. (2022). The Italian version of the international trauma questionnaire: Symptom and network structure of post-traumatic stress disorder and complex post-traumatic stress disorder in a sample of late adolescents exposed to a natural disaster. Frontiers in Psychiatry, 13, 859877. [Google Scholar] [CrossRef] [PubMed]
- Rønning, L., Zelkowitz, R. L., Piccirillo, M. L., Liu, J., Thomas, J. L., Guler, J., Kyei, J. J., Hoeboer, C. M., Karchoud, J. F., Olff, M., Witteveen, A. B., & van Zuiden, M. (2025). Gender differences in early post-traumatic stress disorder symptoms: A network analysis. European Journal of Psychotraumatology, 16(1), 2448385. [Google Scholar] [CrossRef]
- Russell, J. D., Neill, E. L., Carrión, V. G., & Weems, C. F. (2017). The network structure of post-traumatic stress symptoms in children and adolescents exposed to disasters. Journal of the American Academy of Child & Adolescent Psychiatry, 56(8), 669–677. [Google Scholar] [CrossRef]
- Scharpf, F., Saupe, L., Crombach, A., Haer, R., Ibrahim, H., Neuner, F., Peltonen, K., Qouta, S., Saile, R., & Hecker, T. (2023). The network structure of post-traumatic stress symptoms in war-affected children and adolescents. JCPP Advances, 3(1), e12124. [Google Scholar] [CrossRef]
- Schäfer, J., & Strimmer, K. (2005). A shrinkage approach to large-scale covariance matrix estimation and implications for functional genomics. Statistical Applications in Genetics and Molecular Biology, 4(1). [Google Scholar] [CrossRef]
- Schnurr, P. P., & Lunney, C. A. (2015). Differential effects of prolonged exposure on post-traumatic stress disorder symptoms in female veterans. Journal of Consulting and Clinical Psychology, 83(6), 1154. [Google Scholar] [CrossRef]
- Shnaider, P., Vorstenbosch, V., Macdonald, A., Wells, S. Y., Monson, C. M., & Resick, P. A. (2014). Associations between functioning and PTSD symptom clusters in a dismantling trial of cognitive processing therapy in female interpersonal violence survivors. Journal of Traumatic Stress, 27(5), 526–534. [Google Scholar] [CrossRef]
- Spiller, T. R., Duek, O., Helmer, M., Murray, J. D., Fielstein, E., Pietrzak, R. H., von Känel, R., & Harpaz-Rotem, I. (2024). Unveiling the structure in mental disorder presentations. JAMA Psychiatry, 81(11), 1101–1107. [Google Scholar] [CrossRef] [PubMed]
- Spiller, T. R., Levi, O., Neria, Y., Suarez-Jimenez, B., Bar-Haim, Y., & Lazarov, A. (2020). On the validity of the centrality hypothesis in cross-sectional between-subject networks of psychopathology. BMC Medicine, 18, 297. [Google Scholar] [CrossRef]
- Staub, E., & Vollhardt, J. R. (2008). Altruism born of suffering: The roots of caring and helping after victimization and other trauma. American Journal of Orthopsychiatry, 78(3), 267–280. [Google Scholar] [CrossRef]
- Steinberg, A. M., Brymer, M. J., Decker, K. B., & Pynoos, R. S. (2004). The University of California at Los Angeles post-traumatic stress disorder reaction index. Current Psychiatry Reports, 6(2), 96–100. [Google Scholar] [CrossRef]
- Tedeschi, R. G., & Calhoun, L. G. (1996). The post-traumatic growth inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress, 9(3), 455–471. [Google Scholar] [CrossRef]
- Tobia, V., Gabriele, M. A., & Marzocchi, G. M. (2013). The Italian version of the strengths and difficulties questionnaire (SDQ)—Teacher: Psychometric properties. Journal of Psychoeducational Assessment, 31(5), 493–505. [Google Scholar] [CrossRef]
- Tobia, V., & Marzocchi, G. M. (2018). The strengths and difficulties questionnaire-parents for Italian school-aged children: Psychometric properties and norms. Child Psychiatry & Human Development, 49, 1–8. [Google Scholar] [CrossRef]
- van Borkulo, C. D., van Bork, R., Boschloo, L., Kossakowski, J. J., Tio, P., Schoevers, R. A., Borsboom, D., & Waldorp, L. J. (2023). Comparing network structures on three aspects: A permutation test. Psychological Methods, 28(6), 1273–1285. [Google Scholar] [CrossRef]
- Vázquez, A. L., Flores, C. M. N., Feinberg, D. K., Gonzalez, J. C., Young, J., Stewart, R. W., & Orengo-Aguayo, R. E. (2024). A network analysis of Hurricane Maria–related traumatic stress and substance use among Puerto Rican youth. Journal of Traumatic Stress, 37(2), 267–279. [Google Scholar] [CrossRef] [PubMed]
- Villalta, L., Khadr, S., Chua, K. C., Kramer, T., Clarke, V., Viner, R. M., Stringaris, A., & Smith, P. (2020). Complex post-traumatic stress symptoms in female adolescents: The role of emotion dysregulation in impairment and trauma exposure after an acute sexual assault. European Journal of Psychotraumatology, 11(1), 1710400. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.-W., Chan, C. L. W., & Ho, R. T. H. (2013). Prevalence and trajectory of psychopathology among child and adolescent survivors of disasters: A systematic review of epidemiological studies across 1987–2011. Social Psychiatry and Psychiatric Epidemiology, 48(11), 1697–1720. [Google Scholar] [CrossRef]
- Weems, C. F., & Overstreet, S. (2008). Child and adolescent mental health research in the context of Hurricane Katrina: An ecological needs-based perspective and introduction to the special section. Journal of Clinical Child & Adolescent Psychology, 37(3), 487–494. [Google Scholar] [CrossRef]
- Weiss, N. H., Contractor, A. A., Raudales, A. M., Greene, T., & Short, N. A. (2020). Extending our understanding of the association between post-traumatic stress disorder and positive emotion dysregulation: A network analysis approach. Journal of Anxiety Disorders, 71, 102198. [Google Scholar] [CrossRef] [PubMed]
- Woolgar, F., Garfield, H., Dalgleish, T., & Meiser-Stedman, R. (2022). Systematic review and meta-analysis: Prevalence of post-traumatic stress disorder in trauma-exposed preschool-aged children. Journal of the American Academy of Child & Adolescent Psychiatry, 61(3), 366–377. [Google Scholar] [CrossRef]
- Xu, B., Yuan, H., Wu, X., & Wang, W. (2023). Comorbidity patterns of post-traumatic stress disorder and depression symptoms: Cross-validation in two postearthquake child and adolescent samples. Depression and Anxiety, 2023, 4453663. [Google Scholar] [CrossRef] [PubMed]
| Variable | Mean | SD | Min. | Max. | Skewness | Kurtosis |
|---|---|---|---|---|---|---|
| UCLA PTSD-RI | ||||||
| Reexperiencing | 3.30 | 3.544 | 0 | 19 | 1.313 | 1.328 |
| Avoidance | 5.10 | 4.119 | 0 | 23 | 0.986 | 0.505 |
| Increased Arousal | 5.60 | 3.281 | 0 | 18 | 0.820 | 0.647 |
| SDQ | ||||||
| Emotional Problems | 2.42 | 2.205 | 0 | 10 | 0.936 | 0.313 |
| Conduct Problems | 2.21 | 1.562 | 0 | 8 | 0.851 | 0.649 |
| Hyperactivity | 3.17 | 2.056 | 0 | 10 | 0.482 | −0.177 |
| Peer Problems | 1.51 | 1.648 | 0 | 10 | 1.499 | 2.677 |
| Prosocial Behavior | 7.13 | 1.941 | 0 | 10 | −0.456 | −0.047 |
| Node | Betweenness | Closeness | Strength | Expected Influence |
|---|---|---|---|---|
| Reexperiencing | 2 | 0.018 | 0.821 | 0.821 |
| Avoidance | 2 | 0.018 | 0.945 | 0.945 |
| Increased Arousal | 4 | 0.020 | 0.968 | 0.968 |
| Emotional Problems | 0 | 0.018 | 0.988 | 0.988 |
| Conduct Problems | 0 | 0.014 | 0.748 | 0.473 |
| Hyperactivity | 3 | 0.017 | 0.860 | 0.469 |
| Peer Problems | 0 | 0.015 | 0.561 | 0.352 |
| Prosocial Behaviors | 0 | 0.016 | 0.664 | −0.211 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the University Association of Education and Psychology. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Misitano, A.; Geddo, F.; Oppo, A.; Barbieri, A.; Righi, E.; Caffo, E.; Forresi, B. Network Structure of Post-Traumatic Stress and Social/Emotional/Behavioral Difficulties in a Post-Earthquake Child and Adolescent Sample. Eur. J. Investig. Health Psychol. Educ. 2025, 15, 225. https://doi.org/10.3390/ejihpe15110225
Misitano A, Geddo F, Oppo A, Barbieri A, Righi E, Caffo E, Forresi B. Network Structure of Post-Traumatic Stress and Social/Emotional/Behavioral Difficulties in a Post-Earthquake Child and Adolescent Sample. European Journal of Investigation in Health, Psychology and Education. 2025; 15(11):225. https://doi.org/10.3390/ejihpe15110225
Chicago/Turabian StyleMisitano, Alberto, Febe Geddo, Annalisa Oppo, Alice Barbieri, Elena Righi, Ernesto Caffo, and Barbara Forresi. 2025. "Network Structure of Post-Traumatic Stress and Social/Emotional/Behavioral Difficulties in a Post-Earthquake Child and Adolescent Sample" European Journal of Investigation in Health, Psychology and Education 15, no. 11: 225. https://doi.org/10.3390/ejihpe15110225
APA StyleMisitano, A., Geddo, F., Oppo, A., Barbieri, A., Righi, E., Caffo, E., & Forresi, B. (2025). Network Structure of Post-Traumatic Stress and Social/Emotional/Behavioral Difficulties in a Post-Earthquake Child and Adolescent Sample. European Journal of Investigation in Health, Psychology and Education, 15(11), 225. https://doi.org/10.3390/ejihpe15110225








