Mastering Sedation and Associated Respiratory Events through Simulation-Based Training: A Randomised Controlled Trial Involving Non-Anaesthesiology Residents
Abstract
1. Introduction
2. Materials and Methods
2.1. Simulation-Based Learning Sedation Module
- Learn the pharmacology of drugs commonly used for sedation and their antidotes.
- Assimilate the mandatory safety rules related to sedation.
- Understand the mechanisms of sedation-related respiratory events.
- Identify the risk factors for sedation-related respiratory events.
- Master the technical management of sedation-related respiratory events.
- Apply the critical resource management principles to sedation-related respiratory events.
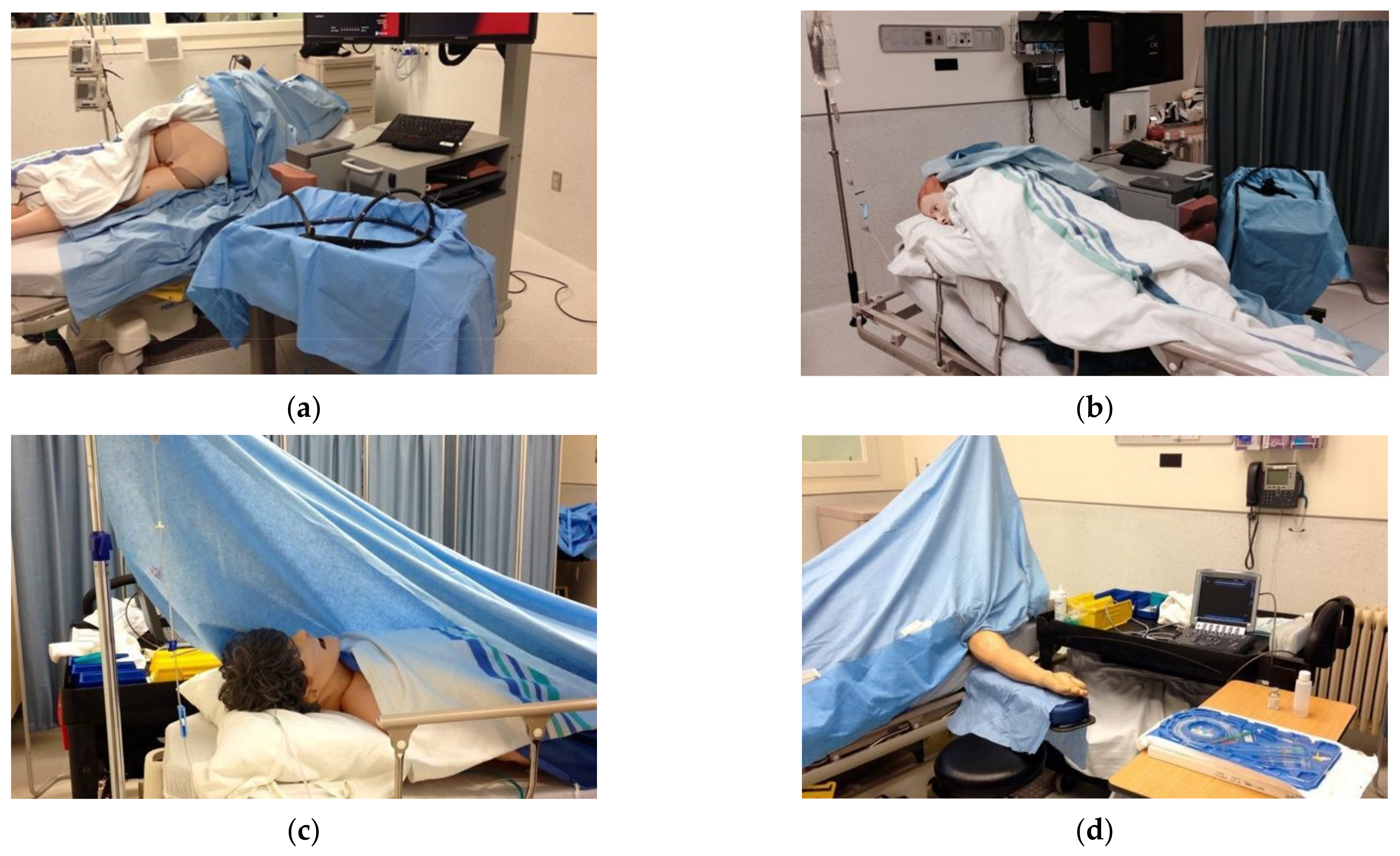
2.2. Setting and Population
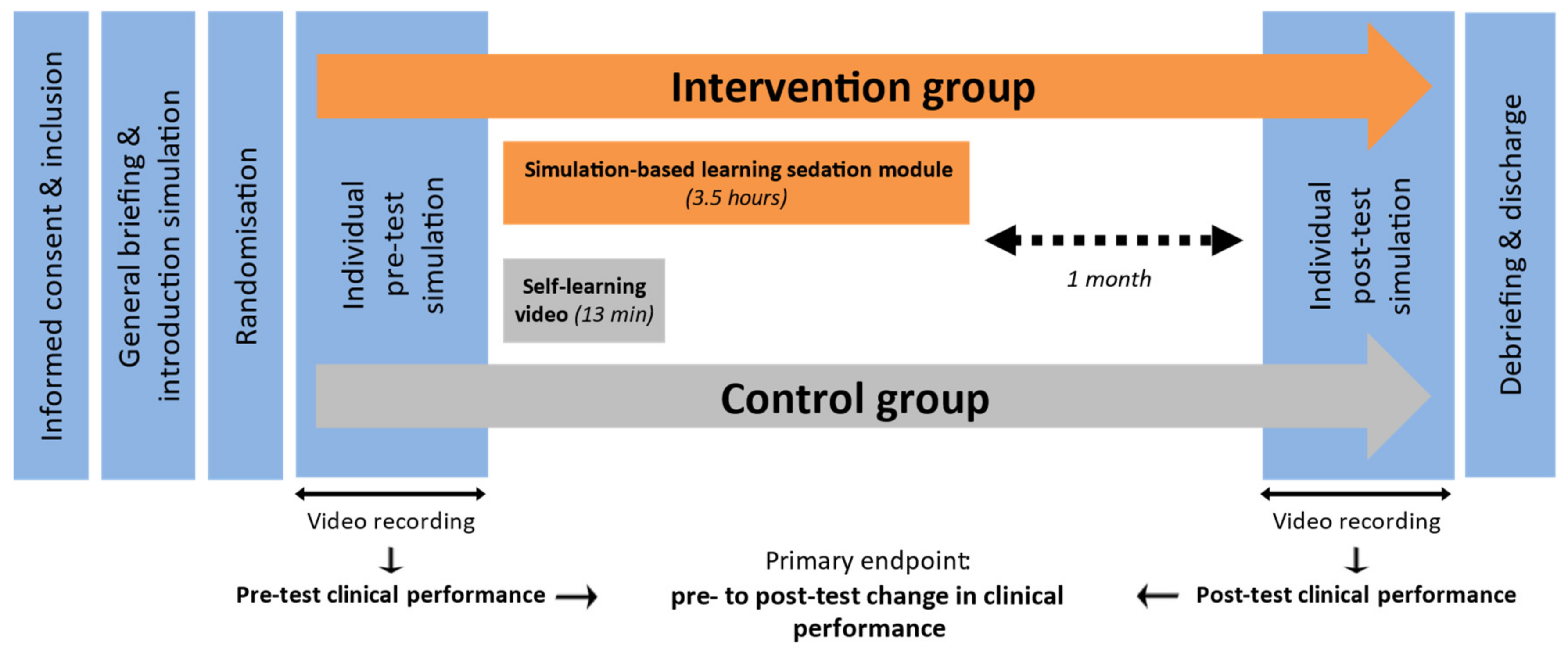
2.3. Study Design
2.4. Primary Outcome Assessment
2.5. Statistical Analysis
3. Results
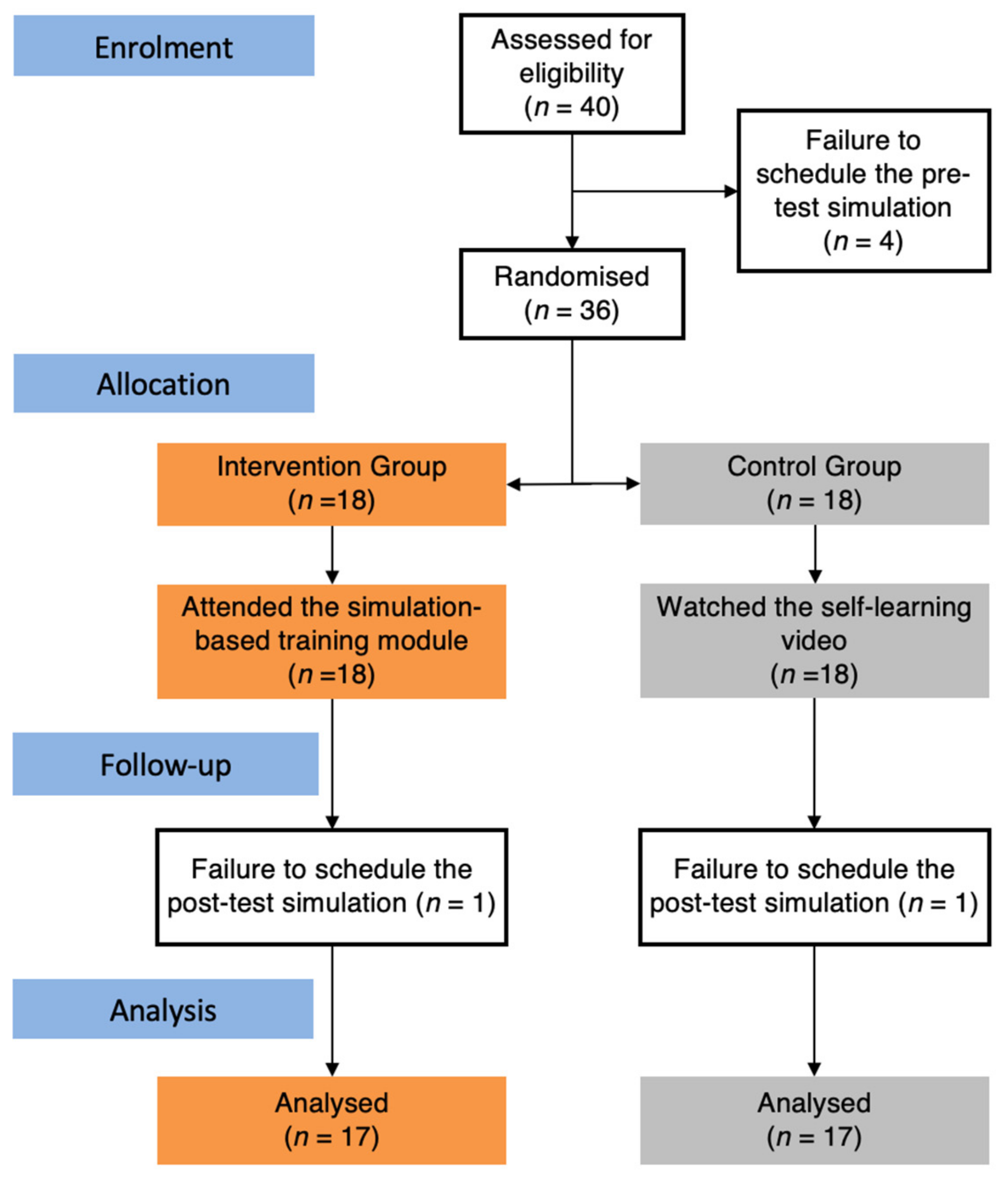
3.1. Study Population
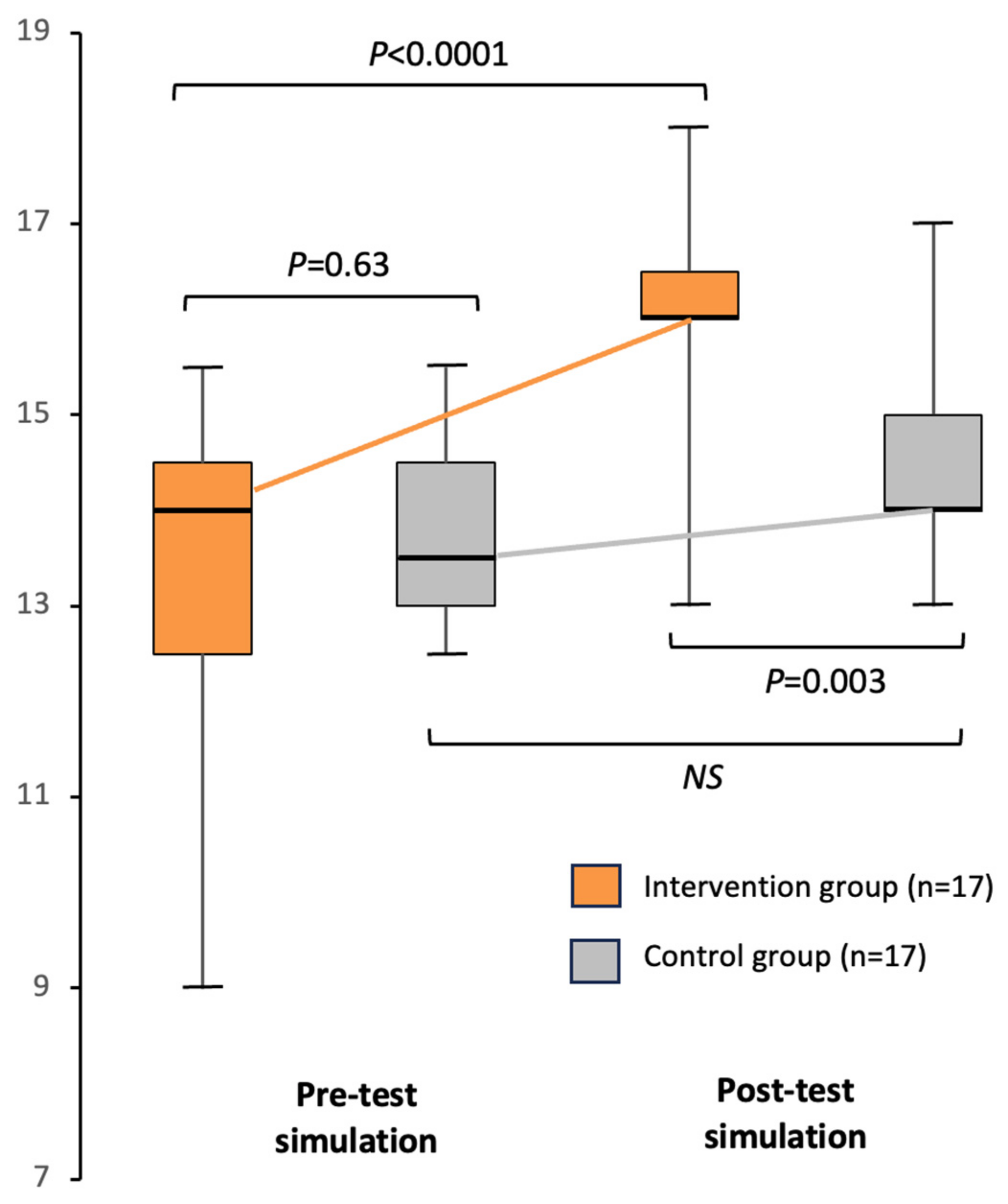
3.2. Clinical Performance Scores
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sneyd, J.R.F. Developments in procedural sedation for adults. BJA Educ. 2022, 22, 258–264. [Google Scholar] [CrossRef]
- Sappenfield, J.W.; White, J.D. Do we really need an anesthesiologist for routine colonoscopy in American Society of Anesthesiologist 1 and 2 patients? Curr. Opin. Anaesthesiol. 2018, 31, 463–468. [Google Scholar] [CrossRef]
- Homma, Y.; Norii, T.; Kanazawa, T.; Hoshino, A.; Arino, S.; Takase, H.; Albright, D.; Funakoshi, H.; Japan Society of Procedural Sedation and Analgesia. A mini-review of procedural sedation and analgesia in the emergency department. Acute Med. Surg. 2020, 7, e574. [Google Scholar] [CrossRef]
- Cornelis, F.H.; Monard, E.; Moulin, M.A.; Vignaud, E.; Laveissiere, F.; Ben Ammar, M.; Nouri-Neuville, M.; Barral, M.; Lombart, B. Sedation and analgesia in interventional radiology: Where do we stand, where are we heading and why does it matter? Diagn. Interv. Imaging 2019, 100, 753–762. [Google Scholar] [CrossRef]
- Hession, P.M.; Joshi, G.P. Sedation: Not quite that simple. Anesthesiol. Clin. 2010, 28, 281–294. [Google Scholar] [CrossRef]
- Metzner, J.; Domino, K.B. Risks of anesthesia or sedation outside the operating room: The role of the anesthesia care provider. Curr. Opin. Anaesthesiol. 2010, 23, 523–531. [Google Scholar] [CrossRef]
- Dupont, S.; Durand, S.; Garner, M.; Gélinas, C.; Haig, M.J.; Hébert, F.; Morin, L.; Ouellet, J.; Parent, J.; Tétreault, M. Sédation-Analgésie [Internet]. 2015. Available online: https://cms.cmq.org/files/documents/Pratique-medicale/p-1-2015-04-01-fr-sedation-analgesie.pdf (accessed on 19 December 2023).
- Kang, H.; Kim, D.K.; Choi, Y.S.; Yoo, Y.C.; Chung, H.S. Practice guidelines for propofol sedation by non-anesthesiologists: The Korean Society of Anesthesiologists Task Force recommendations on propofol sedation. Korean J. Anesthesiol. 2016, 69, 545–554. [Google Scholar] [CrossRef] [PubMed]
- Hinkelbein, J.; Lamperti, M.; Akeson, J.; Santos, J.; Costa, J.; De Robertis, E.; Longrois, D.; Novak-Jankovic, V.; Petrini, F.; Struys, M.M.; et al. European Society of Anaesthesiology and European Board of Anaesthesiology guidelines for procedural sedation and analgesia in adults. Eur. J. Anaesthesiol. 2018, 35, 6–24. [Google Scholar] [CrossRef] [PubMed]
- Hara, T.; Ozawa, A.; Shibutani, K.; Tsujino, K.; Miyauchi, Y.; Kawano, T.; Ito, K.; Sakai, H.; Yokota, M. Practical guide for safe sedation. J. Anesth. 2023, 37, 340–356. [Google Scholar] [CrossRef] [PubMed]
- Pieczynski, L.M.; Raiten, J.M.; Lane-Fall, M.B. From Root Cause to Action Plan: How an Adverse Event Uncovered Deficiencies in Resident Knowledge of Sedation Policies and Practices. A A Case Rep. 2016, 6, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.R.; Salgo, P.; Meltzer, J. Videos in clinical medicine. Conscious sedation for minor procedures in adults. N. Engl. J. Med. 2011, 364, e54. [Google Scholar] [CrossRef] [PubMed]
- Roussin, C.J.; Weinstock, P. SimZones: An Organizational Innovation for Simulation Programs and Centers. Acad. Med. 2017, 92, 1114–1120. [Google Scholar] [CrossRef]
- Kolb, A.Y.; Kolb, D.A. The learning way: Meta-cognitive aspects of experiential learning. Simul. Gaming 2009, 40, 297–327. [Google Scholar] [CrossRef]
- Grau Canét-Wittkampf, C.; Diemers, A.; van den Bogerd, K.; Schönrock-Adema, J.; Damoiseaux, R.; Zwart, D.; Jaarsma, D.; Mol, S.; Bombeke, K.; de Groot, E. Learning patient-centredness with simulated/standardized patients: A realist review: BEME Guide No. 68. Med. Teach. 2023, 45, 347–359. [Google Scholar] [CrossRef] [PubMed]
- Cook, D.A.; Hatala, R.; Brydges, R.; Zendejas, B.; Szostek, J.H.; Wang, A.T.; Erwin, P.J.; Hamstra, S.J. Technology-enhanced simulation for health professions education: A systematic review and meta-analysis. JAMA 2011, 306, 978–988. [Google Scholar] [CrossRef] [PubMed]
- McGaghie, W.C.; Issenberg, S.B.; Cohen, E.R.; Barsuk, J.H.; Wayne, D.B. Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Acad. Med. 2011, 86, 706–711. [Google Scholar] [CrossRef]
- Barsuk, J.H.; Cohen, E.R.; Feinglass, J.; Kozmic, S.E.; McGaghie, W.C.; Ganger, D.; Wayne, D.B. Cost savings of performing paracentesis procedures at the bedside after simulation-based education. Simul. Healthc. 2014, 9, 312–318. [Google Scholar] [CrossRef]
- Van de Ven, J.; van Baaren, G.J.; Fransen, A.F.; van Runnard Heimel, P.J.; Mol, B.W.; Oei, S.G. Cost-effectiveness of simulation-based team training in obstetric emergencies (TOSTI study). Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 216, 130–137. [Google Scholar] [CrossRef]
- Boet, S.; Bould, M.D.; Fung, L.; Qosa, H.; Perrier, L.; Tavares, W.; Reeves, S.; Tricco, A.C. Transfer of learning and patient outcome in simulated crisis resource management: A systematic review. Can. J. Anaesth. 2014, 61, 571–582. [Google Scholar] [CrossRef]
- Cheng, A.; Kessler, D.; Mackinnon, R.; Chang, T.P.; Nadkarni, V.M.; Hunt, E.A.; Duval-Arnould, J.; Lin, Y.; Cook, D.A.; Pusic, M.; et al. Reporting Guidelines for Health Care Simulation Research: Extensions to the CONSORT and STROBE Statements. Simul. Healthc. 2016, 11, 238–248. [Google Scholar] [CrossRef]
- Hofmann, N.; Datz, C.; Schöchl, H. Sedation training using a human patient simulator. Digestion 2010, 82, 115–117. [Google Scholar] [CrossRef]
- Tanoubi, I.; Perron, R.; Bélanger, M.È.; Georgescu, M.; Robitaille, A.; Drolet, P. High-Fidelity Simulation-Based Education: Description of an Original Crisis Resource Management and Sedation Learning for Dental Surgeons. Eur. J. Investig. Health. Psychol. Educ. 2022, 12, 91–97. [Google Scholar] [CrossRef]
- Friedman, N.; Sagi, D.; Ziv, A.; Shavit, I. Pediatric residents’ simulation-based training in patient safety during sedation. Eur. J. Pediatr. 2018, 177, 1863–1867. [Google Scholar] [CrossRef]
- Komasawa, N.; Fujiwara, S.; Atagi, K.; Ueki, R.; Haba, M.; Ueshima, H.; Kaminoh, Y.; Minami, T. Effects of a simulation-based sedation training course on non-anesthesiologists’ attitudes toward sedation and analgesia. J. Anesth. 2014, 28, 785–789. [Google Scholar] [CrossRef] [PubMed]
- Sauter, T.C.; Hautz, W.E.; Hostettler, S.; Brodmann-Maeder, M.; Martinolli, L.; Lehmann, B.; Exadaktylos, A.K.; Haider, D.G. Interprofessional and interdisciplinary simulation-based training leads to safe sedation procedures in the emergency department. Scand. J. Trauma. Resusc. Emerg. Med. 2016, 24, 97. [Google Scholar] [CrossRef] [PubMed]
- Fehr, J.J.; Chao, J.; Kuan, C.; Zhong, J. The important role of simulation in sedation. Curr. Opin. Anaesthesiol. 2016, 29, S14–S20. [Google Scholar] [CrossRef] [PubMed]
- Komasawa, N. Challenges for interprofessional simulation-based sedation training courses: Mini review. Acute Med. Surg. 2023, 10, e913. [Google Scholar] [CrossRef] [PubMed]
- LeBlanc, V.R.; Piquette, D. Simulation comme objet de recherche. In La Simulation en Santé: De la Théorie à la Pratique; Boet, S., Savoldelli, G., Granry, J.C., Eds.; Springer: Paris, France, 2013; pp. 365–376. [Google Scholar]
- Piquette, D.; LeBlanc, V.R. Simulation comme outil de recherche. In La Simulation en Santé: De la Théorie à la Pratique; Boet, S., Savoldelli, G., Granry, J.C., Eds.; Springer: Paris, France, 2013; pp. 377–388. [Google Scholar]
- Rosen, M.A.; Pronovost, P.J. Advancing the use of checklists for evaluating performance in health care. Acad. Med. 2014, 89, 963–965. [Google Scholar] [CrossRef] [PubMed]
- Humphrey-Murto, S.; Varpio, L.; Gonsalves, C.; Wood, T.J. Using consensus group methods such as Delphi and Nominal Group in medical education research. Med. Teach. 2017, 39, 14–19. [Google Scholar] [CrossRef]
- Ilgen, J.S.; Ma, I.W.Y.; Hatala, R.; Cook, D.A. A systematic review of validity evidence for checklists versus global rating scales in simulation-based assessment. Med. Educ. 2015, 49, 161–173. [Google Scholar] [CrossRef]
- Kim, J.; Neilipovitz, D.; Cardinal, P.; Chiu, M. A Comparison of Global Rating Scale and Checklist Scores in the Validation of an Evaluation Tool to Assess Performance in the Resuscitation of Critically Ill Patients During Simulated Emergencies (Abbreviated as “CRM Simulator Study IB”). Simul. Healthc. 2009, 4, 6–16. [Google Scholar] [CrossRef] [PubMed]
| Objective | Pedagogical Approach | |
|---|---|---|
| Welcome and Simulator Presentation | Foster a positive learning climate Familiarize learners with the simulation environment and mannequin Explain the rules of simulation-based teaching: kindness and respect, confidentiality, and fictional commitment | Interactive discussion and didactic introduction Presentation of the simulation environment and mannequin |
| Stage 1 | Stimulate curiosity and create a learning desire Specify the module’s pedagogical objectives | First immersion in a full-scale, high-fidelity simulation of a complicated sedation case Rapid debriefing of the experience and problems encountered Didactic presentation of learning objectives |
| Stage 2 | Integrate basic knowledge of sedation and associated respiratory complications | Interactive didactic presentation |
| Stage 3 | Transfer basic technical skills in airway management during procedural sedation | Practice procedures on a task trainer Continuous, personalised feedback to optimize gestural behaviour |
| Stage 4 | Apply basic knowledge and technical skills in an immersive, contextualised situation Transfer the non-technical skills required for effective team-based crisis management | Second immersion in a full-scale, high-fidelity simulation of a complicated sedation case Structured debriefing with crisis management analysis |
| Conclusion and Discharge | Bring out take-home messages | Interactive discussion and didactic presentation |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Evain, J.-N.; Do, T.; Harkouk, H.; Drolet, P.; Perron, R.; Georgescu, M.; Robitaille, A.; Tanoubi, I. Mastering Sedation and Associated Respiratory Events through Simulation-Based Training: A Randomised Controlled Trial Involving Non-Anaesthesiology Residents. Eur. J. Investig. Health Psychol. Educ. 2024, 14, 463-473. https://doi.org/10.3390/ejihpe14030031
Evain J-N, Do T, Harkouk H, Drolet P, Perron R, Georgescu M, Robitaille A, Tanoubi I. Mastering Sedation and Associated Respiratory Events through Simulation-Based Training: A Randomised Controlled Trial Involving Non-Anaesthesiology Residents. European Journal of Investigation in Health, Psychology and Education. 2024; 14(3):463-473. https://doi.org/10.3390/ejihpe14030031
Chicago/Turabian StyleEvain, Jean-Noël, Tran Do, Hakim Harkouk, Pierre Drolet, Roger Perron, Mihai Georgescu, Arnaud Robitaille, and Issam Tanoubi. 2024. "Mastering Sedation and Associated Respiratory Events through Simulation-Based Training: A Randomised Controlled Trial Involving Non-Anaesthesiology Residents" European Journal of Investigation in Health, Psychology and Education 14, no. 3: 463-473. https://doi.org/10.3390/ejihpe14030031
APA StyleEvain, J.-N., Do, T., Harkouk, H., Drolet, P., Perron, R., Georgescu, M., Robitaille, A., & Tanoubi, I. (2024). Mastering Sedation and Associated Respiratory Events through Simulation-Based Training: A Randomised Controlled Trial Involving Non-Anaesthesiology Residents. European Journal of Investigation in Health, Psychology and Education, 14(3), 463-473. https://doi.org/10.3390/ejihpe14030031






