The Mediating Role of Posttraumatic Stress Symptoms in the Relationship between Adult Attachment and Quality of Life
Abstract
1. Introduction
1.1. Attachment Orientations and Quality of Life
1.2. Posttraumatic Stress Symptoms and Quality of Life
1.3. The Role of Posttraumatic Stress Symptoms in the Relationships between Attachment Orientations and Quality of Life
1.4. Aims of the Study
- Attachment anxiety and avoidance are associated with increased levels of PTSSs;
- Attachment anxiety and avoidance are associated with a poor quality of physical health, psychological status, social relationships, and environment;
- PTSSs are associated with a poor quality of physical health, psychological status, social relationships, and environment;
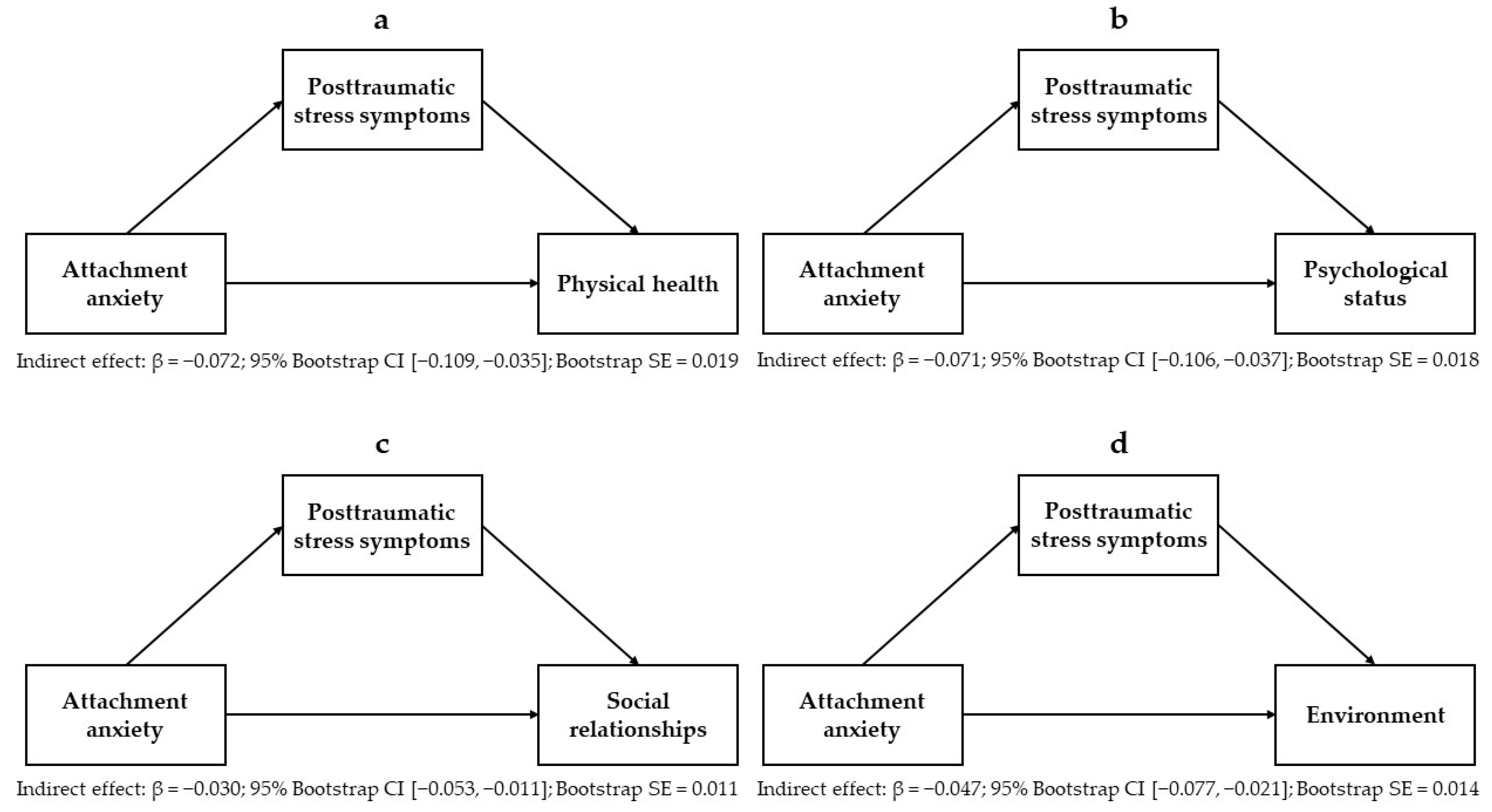
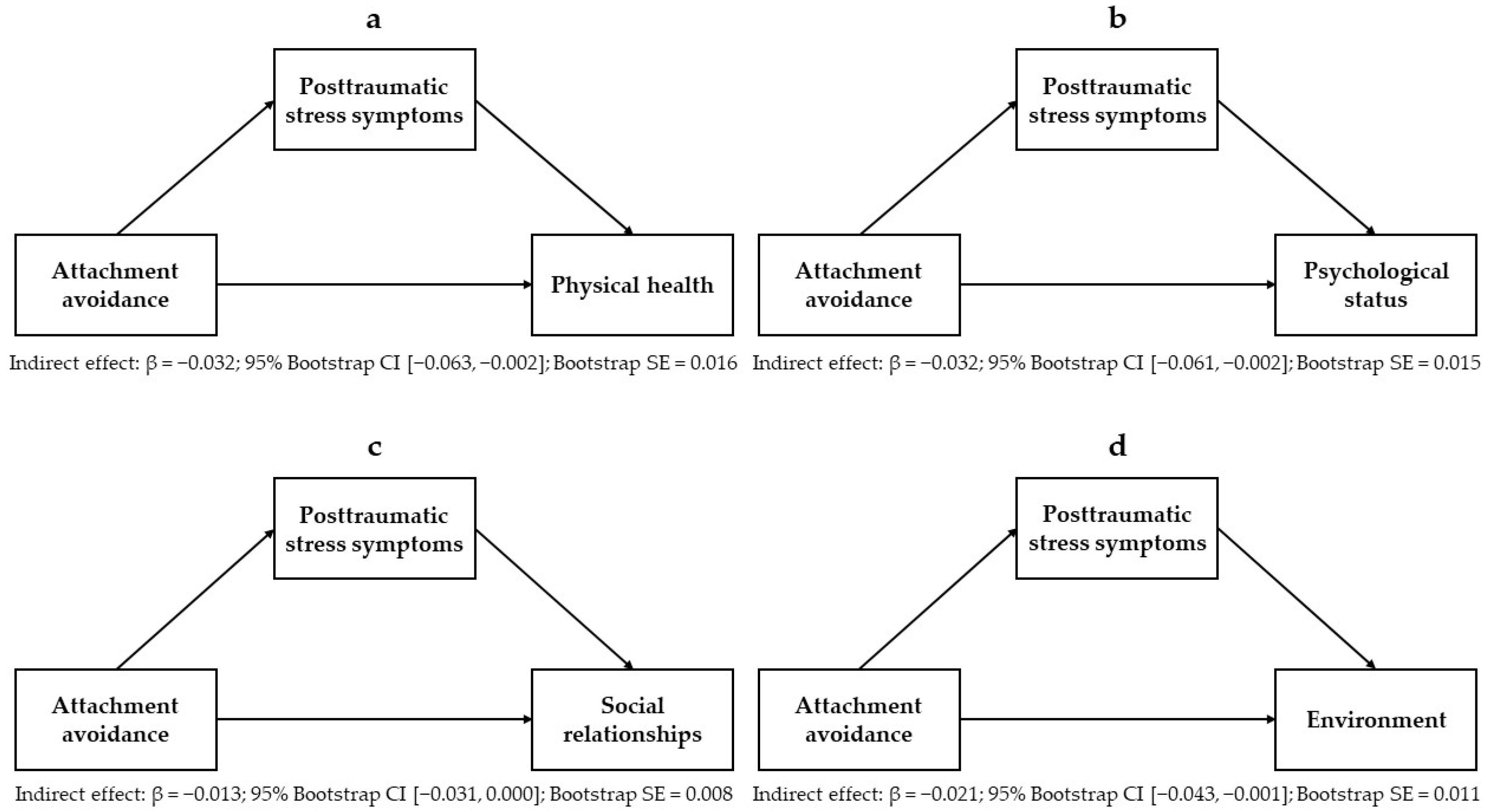
- Attachment anxiety and avoidance are indirectly associated with various domains of quality of life, including physical health, psychological status, social relationships, and environment, through the mediating effects of PTSSs (the hypothesized model is displayed in Figure 1).
2. Materials and Methods
2.1. Participants and Procedures
2.2. Measures
2.3. Statistical Analyses
3. Results
3.1. Descriptive Statistics and Sex Differences
3.2. Correlation Analyses
3.3. Multiple Linear Regression Analyses
3.4. Mediation and Moderated Mediation Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- The WHOQOL Group. The World Health Organization Quality of Life Assessment (WHOQOL): Position Paper from the World Health Organization. Soc. Sci. Med. 1995, 41, 1403–1409. [Google Scholar] [CrossRef] [PubMed]
- The WHOQOL Group. Development of the World Health Organization WHOQOL-BREF Quality of Life Assessment. Psychol. Med. 1998, 28, 551–558. [Google Scholar] [CrossRef] [PubMed]
- The WHOQOL Group. The World Health Organization Quality of Life Assessment (WHOQOL): Development and General Psychometric Properties. Soc. Sci. Med. 1998, 46, 1569–1585. [Google Scholar] [CrossRef] [PubMed]
- Alshraifeen, A.; Al-Rawashdeh, S.; Alnuaimi, K.; Alzoubi, F.; Tanash, M.; Ashour, A.; Al-Hawamdih, S.; Al-Ghabeesh, S. Social Support Predicted Quality of Life in People Receiving Haemodialysis Treatment: A Cross-sectional Survey. Nurs. Open 2020, 7, 1517–1525. [Google Scholar] [CrossRef]
- Yang, Y.; Zhao, S.; Lin, L.; Qian, J.; Zhang, H.; Cai, F. Social Support and Quality of Life in Migrant Workers: Focusing on the Mediating Effect of Healthy Lifestyle. Front. Public Health 2023, 11, 1061579. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Xue, J.; Jiang, Y.; Zhu, T.; Chen, S. Mediating Effects of Depressive Symptoms on Social Support and Quality of Life among Rural Older Chinese. Health Qual. Life Outcomes 2020, 18, 242. [Google Scholar] [CrossRef]
- Kuczynski, A.M.; Kanter, J.W.; Robinaugh, D.J. Differential Associations between Interpersonal Variables and Quality-of-Life in a Sample of College Students. Qual. Life Res. 2020, 29, 127–139. [Google Scholar] [CrossRef]
- Kim, H.; Bae, E.J.; Choi, Y.; Son, H. Biopsychosocial Factors of Quality of Life among Middle-Aged Adults Living Alone in South Korea: A Secondary Data Analysis Using the 2017 Korea Community Health Survey. Arch. Public Health 2024, 82, 108. [Google Scholar] [CrossRef]
- Szkody, E.; McKinney, C. Appraisal and Social Support as Moderators between Stress and Physical and Psychological Quality of Life. Stress Health 2020, 36, 586–595. [Google Scholar] [CrossRef]
- Merluzzi, T.V.; Chirico, A.; Serpentini, S.; Yang, M.; Philip, E.J. The Role of Coping in the Relationship between Stressful Life Events and Quality of Life in Persons with Cancer. Psychol. Health 2019, 34, 497–513. [Google Scholar] [CrossRef]
- Corless, I.B.; Voss, J.; Guarino, A.J.; Wantland, D.; Holzemer, W.; Jane Hamilton, M.; Sefcik, E.; Willard, S.; Kirksey, K.; Portillo, C.; et al. The Impact of Stressful Life Events, Symptom Status, and Adherence Concerns on Quality of Life in People Living with HIV. J. Assoc. Nurses AIDS Care 2013, 24, 478–490. [Google Scholar] [CrossRef] [PubMed]
- Meira, T.M.; Paiva, S.M.; Antelo, O.M.; Guimarães, L.K.; Bastos, S.Q.; Tanaka, O.M. Perceived Stress and Quality of Life among Graduate Dental Faculty. J. Dent. Educ. 2020, 84, 1099–1107. [Google Scholar] [CrossRef]
- Bowlby, J. Attachment and Loss: Vol. I: Attachment; Basic Books: New York, NY, USA, 1969. [Google Scholar]
- Bowlby, J. A Secure Base: Parent-Child Attachment and Healthy Human Development; Routledge: London, UK, 1988. [Google Scholar]
- Bowlby, J. Attachment and Loss: Vol. II: Separation, Anxiety and Anger; The Hogarth Press and the Institute of Psycho-Analysis: London, UK, 1973. [Google Scholar]
- Mikulincer, M.; Shaver, P.R. Attachment in Adulthood: Structure, Dynamics, and Change, 2nd ed.; The Guilford Press: New York, NY, USA, 2016. [Google Scholar]
- Mikulincer, M.; Shaver, P.R.; Solomon, Z. An Attachment Perspective on Traumatic and Posttraumatic Reactions. In Future Directions in Post-Traumatic Stress Disorder: Prevention, Diagnosis, and Treatment; Safir, M.P., Wallach, H.S., Rizzo, A.S., Eds.; Springer Science + Buisness Media: Boston, MA, USA, 2015; pp. 79–96. [Google Scholar] [CrossRef]
- Bartholomew, K.; Horowitz, L.M. Attachment Styles among Young Adults: A Test of a Four-Category Model. J. Pers. Soc. Psychol. 1991, 61, 226–244. [Google Scholar] [CrossRef]
- Agishtein, P.; Brumbaugh, C. Cultural Variation in Adult Attachment: The Impact of Ethnicity, Collectivism, and Country of Origin. J. Soc. Evol. Cult. Psychol. 2013, 7, 384–405. [Google Scholar] [CrossRef]
- Cyr, C.; Euser, E.M.; Bakermans-Kranenburg, M.J.; Van Ijzendoorn, M.H. Attachment Security and Disorganization in Maltreating and High-Risk Families: A Series of Meta-Analyses. Dev. Psychopathol. 2010, 22, 87–108. [Google Scholar] [CrossRef] [PubMed]
- Madigan, S.; Fearon, R.M.P.; van IJzendoorn, M.H.; Duschinsky, R.; Schuengel, C.; Bakermans-Kranenburg, M.J.; Ly, A.; Cooke, J.E.; Deneault, A.-A.; Oosterman, M.; et al. The First 20,000 Strange Situation Procedures: A Meta-Analytic Review. Psychol. Bull. 2023, 149, 99–132. [Google Scholar] [CrossRef]
- Schmitt, D.P.; Alcalay, L.; Allensworth, M.; Allik, J.; Ault, L.; Austers, I.; Bennett, K.L.; Bianchi, G.; Boholst, F.; Cunen, M.A.B.; et al. Patterns and Universals of Adult Romantic Attachment Across 62 Cultural Regions: Are Models of Self and of Other Pancultural Constructs? J. Cross-Cult. Psychol. 2004, 35, 367–402. [Google Scholar] [CrossRef]
- Mikulincer, M.; Shaver, P.R. Attachment Orientations and Emotion Regulation. Curr. Opin. Psychol. 2019, 25, 6–10. [Google Scholar] [CrossRef]
- Luyten, P.; Fonagy, P. The Neurobiology of Mentalizing. Pers. Disord. Theory Res. Treat. 2015, 6, 366–379. [Google Scholar] [CrossRef]
- Santoro, G.; Midolo, L.R.; Costanzo, A.; Schimmenti, A. The Vulnerability of Insecure Minds: The Mediating Role of Mentalization in the Relationship between Attachment Styles and Psychopathology. Bull. Menn. Clin. 2021, 85, 358–384. [Google Scholar] [CrossRef]
- Candel, O.-S.; Turliuc, M.N. Insecure Attachment and Relationship Satisfaction: A Meta-Analysis of Actor and Partner Associations. Pers. Individ. Differ. 2019, 147, 190–199. [Google Scholar] [CrossRef]
- Mark, K.P.; Vowels, L.M.; Murray, S.H. The Impact of Attachment Style on Sexual Satisfaction and Sexual Desire in a Sexually Diverse Sample. J. Sex Marital Ther. 2018, 44, 450–458. [Google Scholar] [CrossRef] [PubMed]
- Herstell, S.; Betz, L.T.; Penzel, N.; Chechelnizki, R.; Filihagh, L.; Antonucci, L.; Kambeitz, J. Insecure Attachment as a Transdiagnostic Risk Factor for Major Psychiatric Conditions: A Meta-Analysis in Bipolar Disorder, Depression and Schizophrenia Spectrum Disorder. J. Psychiatr. Res. 2021, 144, 190–201. [Google Scholar] [CrossRef] [PubMed]
- Midolo, L.R.; Santoro, G.; Ferrante, E.; Pellegriti, P.; Russo, S.; Costanzo, A.; Schimmenti, A. Childhood Trauma, Attachment and Psychopathology: A Correlation Network Approach. Mediterr. J. Clin. Psychol. 2020, 8. [Google Scholar] [CrossRef]
- Zhang, X.; Li, J.; Xie, F.; Chen, X.; Xu, W.; Hudson, N.W. The Relationship between Adult Attachment and Mental Health: A Meta-Analysis. J. Pers. Soc. Psychol. 2022, 123, 1089–1137. [Google Scholar] [CrossRef]
- Mikulincer, M.; Shaver, P.R. An Attachment Perspective on Psychopathology. World Psychiatry 2012, 11, 11–15. [Google Scholar] [CrossRef]
- Schimmenti, A.; Bifulco, A. Linking Lack of Care in Childhood to Anxiety Disorders in Emerging Adulthood: The Role of Attachment Styles. Child Adolesc. Ment. Health 2015, 20, 41–48. [Google Scholar] [CrossRef]
- Le, T.L.; Geist, R.; Hunter, J.; Maunder, R.G. Relationship between Insecure Attachment and Physical Symptom Severity Is Mediated by Sensory Sensitivity. Brain Behav. 2020, 10, e01717. [Google Scholar] [CrossRef]
- McWilliams, L.A. Adult Attachment Insecurity Is Positively Associated with Medically Unexplained Chronic Pain. Eur. J. Pain 2017, 21, 1378–1383. [Google Scholar] [CrossRef]
- McWilliams, L.A.; Bailey, S.J. Associations between Adult Attachment Ratings and Health Conditions: Evidence from the National Comorbidity Survey Replication. Health Psychol. 2010, 29, 446–453. [Google Scholar] [CrossRef]
- Brophy, K.; Brähler, E.; Hinz, A.; Schmidt, S.; Körner, A. The Role of Self-Compassion in the Relationship between Attachment, Depression, and Quality of Life. J. Affect. Disord. 2020, 260, 45–52. [Google Scholar] [CrossRef]
- Sechi, C.; Vismara, L.; Brennstuhl, M.J.; Tarquinio, C.; Lucarelli, L. Adult Attachment Styles, Self-Esteem, and Quality of Life in Women with Fibromyalgia. Health Psychol. Open 2020, 7, 2055102920947921. [Google Scholar] [CrossRef] [PubMed]
- Pistorio, M.L.; Moretta, T.; Musumeci, M.L.; Russo, C.; Lacarrubba, F.; Petralia, A.; Micali, G.; De Pasquale, C. Impact of Attachment Style and Temperament Traits on the Quality of Life of Patients with Psoriasis. Behav. Sci. 2024, 14, 434. [Google Scholar] [CrossRef] [PubMed]
- Karveli, S.; Galanis, P.; Mitropoulou, E.M.; Karademas, E.; Markopoulos, C. The Role of Attachment Styles on Quality of Life and Distress Among Early-Stage Female Breast Cancer Patients: A Systematic Review. J. Clin. Psychol. Med. Settings 2023, 30, 724–739. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; text rev.; American Psychiatric Association: Washington, DC, USA, 2022. [Google Scholar]
- Koenen, K.C.; Ratanatharathorn, A.; Ng, L.; McLaughlin, K.A.; Bromet, E.J.; Stein, D.J.; Karam, E.G.; Meron Ruscio, A.; Benjet, C.; Scott, K.; et al. Posttraumatic Stress Disorder in the World Mental Health Surveys. Psychol. Med. 2017, 47, 2260–2274. [Google Scholar] [CrossRef] [PubMed]
- Asnaani, A.; Hall-Clark, B. Recent Developments in Understanding Ethnocultural and Race Differences in Trauma Exposure and PTSD. Curr. Opin. Psychol. 2017, 14, 96–101. [Google Scholar] [CrossRef]
- Jellestad, L.; Vital, N.A.; Malamud, J.; Taeymans, J.; Mueller-Pfeiffer, C. Functional Impairment in Posttraumatic Stress Disorder: A Systematic Review and Meta-Analysis. J. Psychiatr. Res. 2021, 136, 14–22. [Google Scholar] [CrossRef]
- Dedert, E.A.; Calhoun, P.S.; Watkins, L.L.; Sherwood, A.; Beckham, J.C. Posttraumatic Stress Disorder, Cardiovascular, and Metabolic Disease: A Review of the Evidence. Ann. Behav. Med. 2010, 39, 61–78. [Google Scholar] [CrossRef]
- Pietrzak, R.H.; Goldstein, R.B.; Southwick, S.M.; Grant, B.F. Physical Health Conditions Associated with Posttraumatic Stress Disorder in U.S. Older Adults: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J. Am. Geriatr. Soc. 2012, 60, 296–303. [Google Scholar] [CrossRef]
- Nygaard, E.; Heir, T. World Assumptions, Posttraumatic Stress and Quality of Life after a Natural Disaster: A Longitudinal Study. Health Qual. Life Outcomes 2012, 10, 76. [Google Scholar] [CrossRef]
- Giacco, D.; Matanov, A.; Priebe, S. Symptoms and Subjective Quality of Life in Post-Traumatic Stress Disorder: A Longitudinal Study. PLoS ONE 2013, 8, e60991. [Google Scholar] [CrossRef] [PubMed]
- Huijts, I.; Kleijn, W.C.; van Emmerik, A.A.P.; Noordhof, A.; Smith, A.J.M. Dealing with Man-made Trauma: The Relationship between Coping Style, Posttraumatic Stress, and Quality of Life in Resettled, Traumatized Refugees in the Netherlands. J. Trauma. Stress 2012, 25, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Lim, B.H.; Hodges, M.A.; Lilly, M.M. The Differential Effects of Insecure Attachment on Post-Traumatic Stress: A Systematic Review of Extant Findings and Explanatory Mechanisms. Trauma Violence Abus. 2020, 21, 1044–1060. [Google Scholar] [CrossRef] [PubMed]
- Woodhouse, S.; Ayers, S.; Field, A.P. The Relationship between Adult Attachment Style and Post-Traumatic Stress Symptoms: A Meta-Analysis. J. Anxiety Disord. 2015, 35, 103–117. [Google Scholar] [CrossRef] [PubMed]
- De Girolamo, G.; Rucci, P.; Scocco, P.; Becchi, A.; Coppa, F.; D’Addario, A.; Daru, E.; De Leo, D.; Galassi, L.; Mangelli, L.; et al. Quality of Life Assessment: Validation of the Italian Version of the WHOQOL-Brief. Epidemiol. Psychiatr. Soc. 2000, 9, 45–55. [Google Scholar] [CrossRef]
- Skevington, S.M.; Lotfy, M.; O’Connell, K.A. The World Health Organization’s WHOQOL-BREF Quality of Life Assessment: Psychometric Properties and Results of the International Field Trial. A Report from the WHOQOL Group. Qual. Life Res. 2004, 13, 299–310. [Google Scholar] [CrossRef] [PubMed]
- Carli, L. Attaccamento e Rapporto di Coppia: Il Modello di Bowlby Nell’interpretazione del Ciclo di Vita; Raffaello Cortina: Milano, Italy, 1995. [Google Scholar]
- Griffin, D.W.; Bartholomew, K. Models of the Self and Other: Fundamental Dimensions Underlying Measures of Adult Attachment. J. Pers. Soc. Psychol. 1994, 67, 430–445. [Google Scholar] [CrossRef]
- Scharfe, E.; Bartholomew, K. Reliability and Stability of Adult Attachment Patterns. Pers. Relatsh. 1994, 1, 23–43. [Google Scholar] [CrossRef]
- Weiss, D.S.; Marmar, C.R. The Impact of Event Scale—Revised. In Assessing Psychological Trauma and PTSD; The Guilford Press: New York, NY, USA, 1997; pp. 399–411. [Google Scholar]
- Craparo, G.; Faraci, P.; Rotondo, G.; Gori, A. The Impact of Event Scale—Revised: Psychometric Properties of the Italian Version in a Sample of Flood Victims. Neuropsychiatr. Dis. Treat. 2013, 9, 1427–1432. [Google Scholar] [CrossRef]
- Creamer, M.; Bell, R.; Failla, S. Psychometric Properties of the Impact of Event Scale—Revised. Behav. Res. Ther. 2003, 41, 1489–1496. [Google Scholar] [CrossRef]
- Sveen, J.; Low, A.; Dyster-Aas, J.; Ekselius, L.; Willebrand, M.; Gerdin, B. Validation of a Swedish Version of the Impact of Event Scale-Revised (IES-R) in Patients with Burns. J. Anxiety Disord. 2010, 24, 618–622. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, 3rd ed.; The Guilford Press: New York, NY, USA; London, UK, 2022. [Google Scholar]
- Schimmenti, A.; Billieux, J.; Starcevic, V. The Four Horsemen of Fear: An Integrated Model of Understanding Fear Experiences during the COVID-19 Pandemic. Clin. Neuropsychiatry 2020, 17, 41–45. [Google Scholar] [CrossRef]
- Kim, H.-Y. Statistical Notes for Clinical Researchers: Assessing Normal Distribution (2) Using Skewness and Kurtosis. Restor. Dent. Endod. 2013, 38, 52–54. [Google Scholar] [CrossRef] [PubMed]
- Christiansen, D.M.; Berke, E.T. Gender- and Sex-Based Contributors to Sex Differences in PTSD. Curr. Psychiatry Rep. 2020, 22, 19. [Google Scholar] [CrossRef] [PubMed]
- Hawthorne, G.; Herrman, H.; Murphy, B. Interpreting the WHOQOL-Brèf: Preliminary Population Norms and Effect Sizes. Soc. Indic. Res. 2006, 77, 37–59. [Google Scholar] [CrossRef]
- Segal, D.L.; Needham, T.N.; Coolidge, F.L. Age Differences in Attachment Orientations among Younger and Older Adults: Evidence from Two Self-Report Measures of Attachment. Int. J. Aging Hum. Dev. 2009, 69, 119–132. [Google Scholar] [CrossRef]
- Lataster, J.; Reijnders, J.; Janssens, M.; Simons, M.; Peeters, S.; Jacobs, N. Basic Psychological Need Satisfaction and Well-Being Across Age: A Cross-Sectional General Population Study among 1709 Dutch Speaking Adults. J. Happiness Stud. 2022, 23, 2259–2290. [Google Scholar] [CrossRef]
- Schnurr, P.P.; Lunney, C.A.; Bovin, M.J.; Marx, B.P. Posttraumatic Stress Disorder and Quality of Life: Extension of Findings to Veterans of the Wars in Iraq and Afghanistan. Clin. Psychol. Rev. 2009, 29, 727–735. [Google Scholar] [CrossRef]
- Christiansen, D.M.; Hansen, M. Accounting for Sex Differences in PTSD: A Multi-Variable Mediation Model. Eur. J. Psychotraumatol. 2015, 6, 26068. [Google Scholar] [CrossRef] [PubMed]
- Marshall, E.M.; Frazier, P.A. Understanding Posttrauma Reactions within an Attachment Theory Framework. Curr. Opin. Psychol. 2019, 25, 167–171. [Google Scholar] [CrossRef]
- Kiviruusu, O.; Huurre, T.; Haukkala, A.; Aro, H. Changes in Psychological Resources Moderate the Effect of Socioeconomic Status on Distress Symptoms: A 10-Year Follow-up among Young Adults. Health Psychol. 2013, 32, 627–636. [Google Scholar] [CrossRef] [PubMed]
- Tareke, M.; Bayeh, A.B.; Birhanu, M.; Belete, A. Psychological Distress among People Living with Chronic Medical Illness and the General Population, Northwest Ethiopia: A Comparative Cross-Sectional Study. PLoS ONE 2022, 17, e0278235. [Google Scholar] [CrossRef] [PubMed]
- Rüfenacht, E.; Shaverin, L.; Stubley, J.; Smits, M.L.; Bateman, A.; Fonagy, P.; Luyten, P. Addressing Dissociation Symptoms with Trauma-Focused Mentalization-Based Treatment. Psychoanal. Psychother. 2023, 37, 467–491. [Google Scholar] [CrossRef]
- Ogden, P.; Minton, K. Sensorimotor Psychotherapy: One Method for Processing Traumatic Memory. Traumatology 2000, 6, 149–173. [Google Scholar] [CrossRef]

| Full Sample | |||||
|---|---|---|---|---|---|
| (n = 497) | |||||
| M | (SD) | Range | Skewness | Kurtosis | |
| Age | 32.48 | (13.26) | 18–65 | 0.87 | −0.63 |
| RQ–Attachment anxiety | −1.07 | (4.85) | −12–12 | 0.13 | −0.68 |
| RQ–Attachment avoidance | 0.4 | (3.95) | −12–12 | −0.09 | −0.30 |
| IES-R–Posttraumatic stress symptoms | 42.09 | (19.93) | 0–87 | −0.19 | −0.70 |
| WHOQOL-BREF–Physical health | 14.46 | (2.37) | 8–20 | −0.15 | −0.54 |
| WHOQOL-BREF–Psychological status | 12.69 | (2.65) | 4.67–20 | −0.05 | −0.21 |
| WHOQOL-BREF–Social relationships | 13.67 | (3.20) | 4–20 | −0.47 | 0.09 |
| WHOQOL-BREF–Environment | 13.11 | (2.24) | 6.5–19.5 | 0.04 | −0.12 |
| Males | Females | ||||
|---|---|---|---|---|---|
| (n = 122) | (n = 375) | ||||
| M | (SD) | M | (SD) | t(495) | |
| Age | 30.80 | (12.83) | 33.03 | (13.36) | −1.62 |
| RQ–Attachment anxiety | −1.81 | (4.64) | −0.83 | (4.89) | −1.95 |
| RQ–Attachment avoidance | 0.37 | (3.89) | 0.41 | (3.97) | −0.09 |
| IES-R–Posttraumatic stress symptoms | 36.31 | (20.37) | 43.97 | (19.44) | −3.74 ** |
| WHOQOL-BREF–Physical health | 14.83 | (2.50) | 14.33 | (2.31) | 2.03 * |
| WHOQOL-BREF–Psychological status | 13.18 | (2.88) | 12.53 | (2.56) | 2.36 * |
| WHOQOL-BREF–Social relationships | 13.33 | (3.62) | 13.79 | (3.04) | −1.36 |
| WHOQOL-BREF–Environment | 13.73 | (2.38) | 12.91 | (2.16) | 3.56 ** |
| 2. | 3. | 4. | 5. | 6. | 7. | 8. | |
|---|---|---|---|---|---|---|---|
| 1. Age | −0.19 *** | −0.02 | −0.24 *** | 0.06 | 0.13 ** | −0.01 | −0.05 |
| 2. RQ–Attachment anxiety | – | 0.08 | 0.25 *** | −0.30 *** | −0.40 *** | −0.42 *** | −0.25 *** |
| 3. RQ–Attachment avoidance | – | 0.10 * | −0.09 * | −0.13 ** | −0.18 *** | −0.09 * | |
| 4. IES-R–Posttraumatic stress symptoms | – | −0.42 *** | −0.45 *** | −0.22 *** | −0.28 *** | ||
| 5. WHOQOL-BREF–Physical health | – | 0.67 *** | 0.37 *** | 0.52 *** | |||
| 6. WHOQOL-BREF–Psychological status | – | 0.53 *** | 0.57 *** | ||||
| 7. WHOQOL-BREF–Social relationships | – | 0.39 *** | |||||
| 8. WHOQOL-BREF–Environment | – |
| β | SE | Partial r | t | |
|---|---|---|---|---|
| WHOQOL-BREF–Physical health | ||||
| [Model: F(5,491) = 28.016, p < 0.001, R2 = 0.22] | ||||
| Sex | 0.00 | 0.22 | −0.01 | −0.12 |
| Age | −0.07 | 0.01 | −0.07 | −1.61 |
| RQ—Attachment anxiety | −0.22 *** | 0.02 | −0.23 | −5.22 |
| RQ—Attachment avoidance | −0.04 | 0.02 | −0.04 | −0.89 |
| IES-R—Posttraumatic stress symptoms | −0.38 *** | 0.01 | −0.37 | −8.76 |
| WHOQOL-BREF–Psychological status | ||||
| [Model: F(5,491) = 41.987, p < 0.001, R2 = 0.30] | ||||
| Sex | −0.02 | 0.24 | −0.02 | −0.40 |
| Age | −0.02 | 0.01 | −0.02 | −0.52 |
| RQ—Attachment anxiety | −0.31 *** | 0.02 | −0.33 | −7.73 |
| RQ—Attachment avoidance | −0.07 | 0.03 | −0.08 | −1.82 |
| IES-R—Posttraumatic stress symptoms | −0.37 *** | 0.01 | −0.38 | −9.15 |
| WHOQOL-BREF–Social relationships | ||||
| [Model: F(5,491) = 30.556, p < 0.001, R2 = 0.24] | ||||
| Sex | 0.13 ** | 0.30 | 0.15 | 3.30 |
| Age | −0.14 ** | 0.01 | −0.15 | −3.45 |
| RQ—Attachment anxiety | −0.41 *** | 0.03 | −0.41 | −9.84 |
| RQ—Attachment avoidance | −0.14 ** | 0.03 | −0.15 | −3.39 |
| IES-R—Posttraumatic stress symptoms | −0.16 *** | 0.01 | −0.16 | −3.69 |
| WHOQOL-BREF–Environment | ||||
| [Model: F(5,491) = 16.564, p < 0.001, R2 = 0.14] | ||||
| Sex | −0.09 * | 0.22 | −0.09 | −2.10 |
| Age | −0.14 ** | 0.01 | −0.14 | −3.21 |
| RQ—Attachment anxiety | −0.20 *** | 0.02 | −0.21 | −4.63 |
| RQ—Attachment avoidance | −0.05 | 0.02 | −0.05 | −1.21 |
| IES-R—Posttraumatic stress symptoms | −0.24 *** | 0.01 | −0.24 | −5.43 |
| B * | 95% CI | se | β | |
|---|---|---|---|---|
| WHOQOL-BREF–Physical health | ||||
| [Total effect model: F(4,492) = 13.727, p < 0.001, R2 = 0.10] | ||||
| Predictor → Mediator | 0.785 | 0.437, 1.133 | 0.177 | 0.191 |
| Mediator → Outcome | −0.045 | −0.055, −0.035 | 0.005 | −0.375 |
| Direct effect (Predictor → Outcome) | −0.106 | −0.146, −0.066 | 0.020 | −0.218 |
| Total effect (Predictor → Outcome) | −0.141 | −0.183, −0.099 | 0.021 | −0.289 |
| WHOQOL-BREF–Psychological status | ||||
| [Total effect model: F(4,492) = 27.016, p < 0.001, R2 = 0.18] | ||||
| Predictor → Mediator | 0.785 | 0.437, 1.133 | 0.177 | 0.191 |
| Mediator → Outcome | −0.050 | −0.060, −0.039 | 0.005 | −0.372 |
| Direct effect (Predictor → Outcome) | −0.167 | −0.210, −0.125 | 0.022 | −0.306 |
| Total effect (Predictor → Outcome) | −0.206 | −0.251, −0.161 | 0.023 | −0.377 |
| WHOQOL-BREF–Social relationships | ||||
| Total effect model: F(4,492) = 33.914, p < 0.001, R2 = 0.22] | ||||
| Predictor → Mediator | 0.785 | 0.437, 1.133 | 0.177 | 0.191 |
| Mediator → Outcome | −0.025 | −0.038, −0.012 | 0.007 | −0.157 |
| Direct effect (Predictor → Outcome) | −0.268 | −0.322, −0.214 | 0.027 | −0.406 |
| Total effect (Predictor → Outcome) | −0.288 | −0.341, −0.235 | 0.027 | −0.436 |
| WHOQOL-BREF–Environment | ||||
| [Total effect model: F(4,492) = 12.618, p < 0.001, R2 = 0.09] | ||||
| Predictor → Mediator | 0.785 | 0.437, 1.133 | 0.177 | 0.191 |
| Mediator → Outcome | −0.027 | −0.037, −0.017 | 0.005 | −0.244 |
| Direct effect (Predictor → Outcome) | −0.094 | −0.133, −0.054 | 0.020 | −0.203 |
| Total effect (Predictor → Outcome) | −0.115 | −0.155, −0.075 | 0.020 | −0.249 |
| B | 95% CI | se | β | |
|---|---|---|---|---|
| WHOQOL-BREF–Physical health | ||||
| [Total effect model: F(4,492) = 13.727, p < 0.001, R2 = 0.10] | ||||
| Predictor → Mediatior | 0.428 * | 0.010, 0.845 | 0.212 | 0.085 |
| Mediator → Outcome | −0.045 ** | −0.055, −0.035 | 0.005 | −0.375 |
| Direct effect (Predictor → Outcome) | −0.021 | −0.069, 0.026 | 0.024 | −0.036 |
| Total effect (Predictor → Outcome) | −0.040 | −0.091, 0.010 | 0.026 | −0.068 |
| WHOQOL-BREF–Psychological status | ||||
| [Total effect model: F(4,492) = 27.016, p < 0.001, R2 = 0.18] | ||||
| Predictor → Mediator | 0.428 * | 0.010, 0.845 | 0.212 | 0.085 |
| Mediator → Outcome | −0.050 ** | −0.060, −0.039 | 0.005 | −0.372 |
| Direct effect (Predictor → Outcome) | −0.047 | −0.097, 0.004 | 0.026 | −0.069 |
| Total effect (Predictor → Outcome) | −0.068 * | −0.122, −0.014 | 0.028 | −0.101 |
| WHOQOL-BREF–Social relationships | ||||
| [Total effect model: F(4,492) = 33.914, p < 0.001, R2 = 0.22] | ||||
| Predictor → Mediator | 0.428 * | 0.010, 0.845 | 0.212 | 0.085 |
| Mediator → Outcome | −0.025 ** | −0.038, −0.012 | 0.007 | −0.157 |
| Direct effect (Predictor → Outcome) | −0.109 ** | −0.172, −0.046 | 0.032 | −0.135 |
| Total effect (Predictor → Outcome) | −0.120 ** | −0.184, −0.056 | 0.032 | −0.148 |
| WHOQOL-BREF–Environment | ||||
| [Total effect model: F(4,492) = 12.618, p < 0.001, R2 = 0.09] | ||||
| Predictor → Mediator | 0.428 * | 0.010, 0.845 | 0.212 | 0.085 |
| Mediator → Outcome | −0.027 ** | −0.037, −0.017 | 0.005 | −0.244 |
| Direct effect (Predictor → Outcome) | −0.029 | −0.076, 0.018 | 0.024 | −0.051 |
| Total effect (Predictor → Outcome) | −0.041 | −0.089, 0.008 | 0.024 | −0.071 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the University Association of Education and Psychology. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santoro, G.; Lenzo, V.; Musetti, A.; Caneglias, C.; Crimi, L.R.; Sideli, L.; Schimmenti, A. The Mediating Role of Posttraumatic Stress Symptoms in the Relationship between Adult Attachment and Quality of Life. Eur. J. Investig. Health Psychol. Educ. 2024, 14, 2735-2753. https://doi.org/10.3390/ejihpe14100180
Santoro G, Lenzo V, Musetti A, Caneglias C, Crimi LR, Sideli L, Schimmenti A. The Mediating Role of Posttraumatic Stress Symptoms in the Relationship between Adult Attachment and Quality of Life. European Journal of Investigation in Health, Psychology and Education. 2024; 14(10):2735-2753. https://doi.org/10.3390/ejihpe14100180
Chicago/Turabian StyleSantoro, Gianluca, Vittorio Lenzo, Alessandro Musetti, Cristiana Caneglias, Lina Rita Crimi, Lucia Sideli, and Adriano Schimmenti. 2024. "The Mediating Role of Posttraumatic Stress Symptoms in the Relationship between Adult Attachment and Quality of Life" European Journal of Investigation in Health, Psychology and Education 14, no. 10: 2735-2753. https://doi.org/10.3390/ejihpe14100180
APA StyleSantoro, G., Lenzo, V., Musetti, A., Caneglias, C., Crimi, L. R., Sideli, L., & Schimmenti, A. (2024). The Mediating Role of Posttraumatic Stress Symptoms in the Relationship between Adult Attachment and Quality of Life. European Journal of Investigation in Health, Psychology and Education, 14(10), 2735-2753. https://doi.org/10.3390/ejihpe14100180







