A Causal Analysis of Young Adults’ Binge Drinking Reduction and Cessation
Abstract
1. Introduction
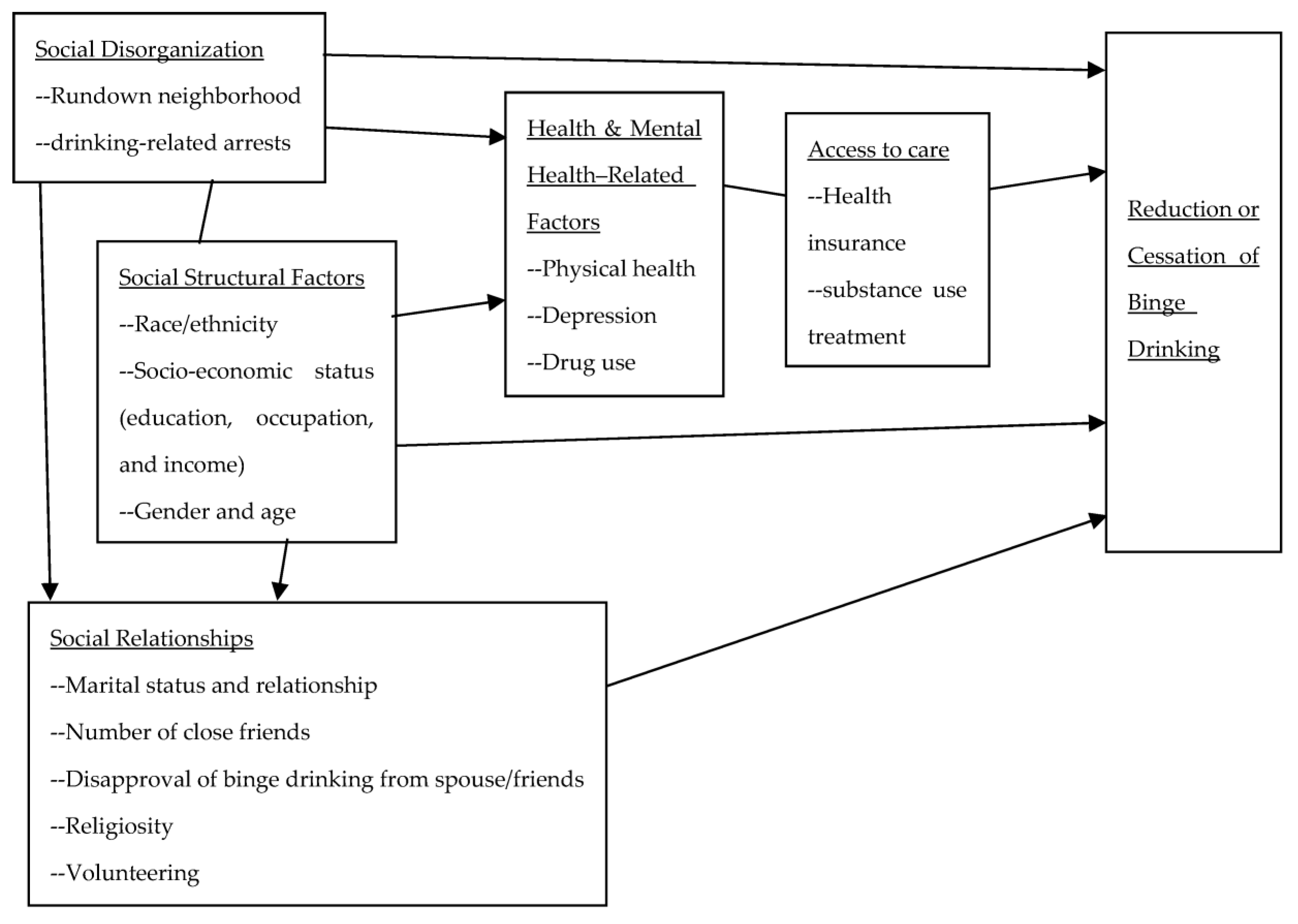
Literature Review
2. Materials and Methods
2.1. Sample
2.2. Measures
2.3. Data Analysis
3. Results
Multivariate Analysis Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2019 National Survey on Drug Use and Health; PEP20-07-01-001, NSDUH Series H-55; Substance Abuse and Mental Health Services Administration: Rockville, MD, USA, 2020. [Google Scholar]
- Centers for Disease Control and Prevention. Alcohol Use and Your Health; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2018. [Google Scholar]
- Centers for Disease Control and Prevention. Binge Drinking; Center for Disesae Control and Prevention: Washington, DC, USA, 2022. [Google Scholar]
- Centers for Disease Control and Prevention. Alcohol Poisoning Dealths: A Deadly Consequence of Binge Drinking; Centers for Diseases Control and Prevention: Atlanta, GA, USA, 2022. [Google Scholar]
- Cheng, T.C.; Lo, C.C. Risk and protective factors in adult-onset drinking: Application of the multiple disadvantage model. Int. J. Health Wellness Soc. 2018, 8, 29–41. [Google Scholar] [CrossRef]
- Cheng, T.C.; Lo, C.C. Racial disparities in intimate partner violence examined through the multiple disadvantage model. J. Interpers. Violence 2016, 31, 2026–2051. [Google Scholar] [CrossRef]
- Lo, C.C.; Howell, R.J.; Cheng, T.C. Explaining Black-White Differences in Homicide Victimization. Aggress. Violent Behav. 2013, 18, 125–134. [Google Scholar] [CrossRef]
- Lo, C.C.; Howell, R.J.; Cheng, T.C. Racial Disparities in Age at Time of Homicide Victimization: A Test of the Multiple Disadvantage Model. J. Interpers. Violence 2015, 30, 152–167. [Google Scholar] [CrossRef] [PubMed]
- Kedia, S.K.; Schmidt, M.; Dillon, P.J.; Arshad, H.; Yu, X. Substance use treatment in Appalachian Tennessee amid COVID-19: Challenges and preparing for the future. J. Subst. Abus. Treat. 2021, 124, 108270. [Google Scholar] [CrossRef]
- Brenner, A.B.; Borrell, L.N.; Barrientos-Gutierrez, T.; Roux, A.V.D. Longitudinal associations of neighborhood socioeconomic characteristics and alcohol availability on drinking: Results from the Multi-Ethnic Study of Atherosclerosis (MESA). Soc. Sci. Med. 2015, 145, 17–25. [Google Scholar] [CrossRef]
- Brenner, A.B.; Roux, A.V.D.; Barrientos-Gutierrez, T.; Borrell, L.N. Associations of Alcohol Availability and Neighborhood Socioeconomic Characteristics with Drinking: Cross-Sectional Results from the Multi-Ethnic Study of Atherosclerosis (MESA). Subst. Use Misuse 2015, 50, 1606–1617. [Google Scholar] [CrossRef] [PubMed]
- Mericle, A.A.; Kaskutas, L.A.; Polcin, D.L.; Karriker-Jaffe, K.J. Independent and Interactive Effects of Neighborhood Disadvantage and Social Network Characteristics on Problem Drinking After Treatment. J. Soc. Clin. Psychol. 2018, 37, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Steinman, K.J. College Students’ Early Cessation From Episodic Heavy Drinking: Prevalence and Correlates. J. Am. Coll. Health 2003, 51, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Walters, S.T.; Vader, A.M.; Harris, T.R.; Field, C.A.; Jouriles, E.N. Dismantling motivational interviewing and feedback for college drinkers: A randomized clinical trial. J. Consult. Clin. Psychol. 2009, 77, 64–73. [Google Scholar] [CrossRef]
- Banta, J.E.; Mukaire, P.E.; Haviland, M.G. Binge drinking by gender and race/ethnicity among California adults, 2007/2009. Am. J. Drug Alcohol Abus. 2014, 40, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Tenkku, L.E.; Morris, D.S.; Salas, J.; Xaverius, P.K. Racial Disparities in Pregnancy-Related Drinking Reduction. Matern. Child Health J. 2009, 13, 604–613. [Google Scholar] [CrossRef]
- Gause, N.K.; Elliott, J.C.; Delker, E.; Stohl, M.; Hasin, D.; Aharonovich, E. Association between change in self-efficacy to resist drinking and drinking behaviors among an HIV-infected sample: Results from a large randomized controlled trial. J. Health Psychol. 2018, 23, 829–839. [Google Scholar] [CrossRef]
- Hanson, J.D.; Noonan, C.; Harris, A.; Oziel, K.; Sarche, M.; MacLehose, R.F.; O’Leary, M.; Buchwald, D. Alcohol Consumption during COVID among Women with an Existing Alcohol-Use Disorder. Int. J. Environ. Res. Public Health 2021, 18, 9460. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, M.; Osilla, K.C.; Kennedy, D.P.; Paddock, S.M. Longitudinal effects of social network changes on drinking outcomes for individuals with a first-time DUI. J. Subst. Abus. Treat. 2021, 131, 108392. [Google Scholar] [CrossRef]
- Hoeppner, B.B.; Hoeppner, S.S.; Kelly, J.F. Do young people benefit from AA as much, and in the same ways, as adult aged 30+? A moderated multiple mediation analysis. Drug Alcohol Depend. 2014, 143, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.F.; Hoeppner, B.; Stout, R.L.; Pagano, M. Determining the relative importance of the mechanisms of behavior change within Alcoholics Anonymous: A multiple mediator analysis. Addiction 2012, 107, 289–299. [Google Scholar] [CrossRef] [PubMed]
- Stone, R.A.T.; Whitbeck, L.B.; Chen, X.J.; Johnson, K.; Olson, D.M. Traditional practices, traditional spirituality, and alcohol cessation among American Indians. J. Stud. Alcohol 2006, 67, 236–244. [Google Scholar] [CrossRef] [PubMed]
- Lambert, N.M.; Fincham, F.D.; Marks, L.D.; Stillman, T.F. Invocations and intoxication: Does prayer decrease alcohol consumption? Psychol. Addict. Behav. 2010, 24, 209. [Google Scholar] [CrossRef] [PubMed]
- Dawson, D.A.; Goldstein, R.B.; Grant, B.F. Prospective correlates of drinking cessation: Variation across the life-course. Addiction 2013, 108, 712–722. [Google Scholar] [CrossRef]
- Armstrong, M.A.; Midanik, L.T.; Klatsky, A.L. Alcohol consumption and utilization of health services in a health maintenance organization. Med. Care 1998, 36, 1599–1605. [Google Scholar] [CrossRef] [PubMed]
- Ambrogne, J.A. Managing depressive symptoms in the context of abstinence: Findings from a qualitative study of women. Perspect. Psychiatr. Care 2007, 43, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Dodge, R.; Sindelar, J.; Sinha, R. The role of depression symptoms in predicting drug abstinence in outpatient substance abuse treatment. J. Subst. Abus. Treat. 2005, 28, 189–196. [Google Scholar] [CrossRef]
- Ahmedani, B.K.; McBride, O.; Cheng, H.G. Factors Related to Recent Alcohol Abstinence among Individuals Who Received Previous Treatment. Am. J. Drug Alcohol Abus. 2012, 38, 87–92. [Google Scholar] [CrossRef] [PubMed]
- LaBrie, J.W.; Pedersen, E.R.; Lamb, T.F.; Quinlan, T. A campus-based motivational enhancement group intervention reduces problematic drinking in freshmen male college students. Addict. Behav. 2007, 32, 889–901. [Google Scholar] [CrossRef]
- Aharonovich, E.; Stohl, M.; Ellis, J.; Amrhein, P.; Hasin, D. Commitment strength, alcohol dependence and HealthCall participation: Effects on drinking reduction in HIV patients. Drug Alcohol Depend. 2014, 135, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Lau-Barraco, C.; Dunn, M.E. Evaluation of a single-session expectancy challenge intervention to reduce alcohol use among college students. Psychol. Addict. Behav. 2008, 22, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Boyle, S.C.; Earle, A.M.; McCabe, N.; LaBrie, J.W. Increasing Chance-Based Uncertainty Reduces Heavy Drinkers’ Cognitive Reactance to Web-Based Personalized Normative Feedback. J. Stud. Alcohol Drugs 2018, 79, 601–610. [Google Scholar] [CrossRef]
- Hasin, D.S.; Aharonovich, E.; O’Leary, A.; Greenstein, E.; Pavlicova, M.; Arunajadai, S.; Waxman, R.; Wainberg, M.; Helzer, J.; Johnston, B. Reducing heavy drinking in HIV primary care: A randomized trial of brief intervention, with and without technological enhancement. Addiction 2013, 108, 1230–1240. [Google Scholar] [CrossRef] [PubMed]
- Grekin, E.R.; Beatty, J.R.; McGoron, L.; Kugler, K.C.; McClure, J.B.; Pop, D.E.; Ondersma, S.J. Testing the efficacy of motivational strategies, empathic reflections, and lifelike features in a computerized intervention for alcohol use: A factorial trial. Psychol. Addict. Behav. 2019, 33, 511–519. [Google Scholar] [CrossRef]
- Harris, K.M.; Udry, J.R. National Longitudinal Study of Adolescent Health (Add Health) 1994–2008: Description; Inter-University Consortium for Political and Social Research: Ann Arbor, MI, USA, 2008. [Google Scholar]
- Carolina Population Center. Add Health: Study Design; University of North Carolina: Chapel Hill, NC, USA, 2016. [Google Scholar]
- Carolina Population Center. Add Health Research Design: Waves I–V; University of North Carolina: Chapel Hill, NC, USA, 2020. [Google Scholar]
- Finkel, S.E. Causal Analysis with Panel Data; SAGE: Thousand Oaks, CA, USA, 1995. [Google Scholar]
- Rexroat, C.; Shehan, C. Differential effects of industrial and workers resources on women’s wages. Soc. Sci. Res. 1986, 15, 1–27. [Google Scholar] [CrossRef]
- Rocheleau, G.C.; Olson, J.T.; Vito, A.G. Victimization, negative emotions, and substance use: Variability in general strain theory processes by marriage and relationship quality. Criminol. Crim. Justice 2023, 1–20. [Google Scholar] [CrossRef]
- Wickrama, K.; O’Neal, C.W. The Socioeconomic Pathways Leading to Romantic Relationship Outcomes: A Genetically Informed Early Life Course Investigation. J. Res. Adolesc. 2016, 26, 492–508. [Google Scholar] [CrossRef] [PubMed]
- Radimer, S.; Rowan-Kenyon, H. Undergraduate Men’s Alcohol Consumption: Masculine Norms, Ethnic Identity, and Social Dominance Orientation. J. Coll. Stud. Dev. 2019, 60, 1–16. [Google Scholar] [CrossRef]
- Chauhan, P.; Ahern, J.; Galea, S.; Keyes, K.M. Neighborhood Context and Binge Drinking by Race and Ethnicity in New York City. Alcohol. -Clin. Exp. Res. 2016, 40, 785–793. [Google Scholar] [CrossRef]
- Bryant, A.N.; Kim, G. The relation between acculturation and alcohol consumption patterns among older Asian and Hispanic immigrants. Aging Ment. Health 2013, 17, 147–156. [Google Scholar] [CrossRef]
- Kim, W. Drinking culture of elderly Korean immigrants in Canada: A focus group study. J. Cross-Cult. Gerontol. 2009, 24, 339–353. [Google Scholar] [CrossRef]
- Murphy, J.G.; Duchnick, J.J.; Vuchinich, R.E.; Davison, J.W.; Karg, R.S.; Olson, A.M.; Smith, A.F.; Coffey, T.T. Relative efficacy of a brief motivational intervention for college student drinkers. Psychol. Addict. Behav. 2001, 15, 373. [Google Scholar] [CrossRef]
| Variables | % | Mean | Range | s.d. | |
|---|---|---|---|---|---|
| Binge drinking type | |||||
| Binge drinking maintained | 44.7 | ||||
| Change to non-binge drinking | 46.6 | ||||
| Change to nondrinking | 8.7 | ||||
| Social disorganization factors | |||||
| Unsafe neighborhood at Wave 3 | (yes) | 3.0 | |||
| (no) | 97.0 | ||||
| Unsafe neighborhood difference | 0.01 | −1–1 | 0.3 | ||
| Involved in fights at Wave 3 | 0.3 | 0–4 | 0.7 | ||
| Being arrested at Wave 4 | 0.4 | 0–2 | 0.5 | ||
| Social structural and demographic factors | |||||
| Personal income at Wave 3 | USD 11,125.1 | USD 0–1,000,000 | USD 10,068.2 | ||
| Personal income difference | USD 23,344.3 | USD −80,000–401,100 | USD 31,254.2 | ||
| Education level at Wave 3 | 2.6 | 1–5 | 0.9 | ||
| Education level difference | 0.6 | 0–4 | 0.7 | ||
| Occupational skill at Wave 3 | 2.0 | 0–5 | 1.2 | ||
| Occupational skill difference | 1.1 | −5–5 | 1.9 | ||
| Male | 52.2 | ||||
| Female | 47.8 | ||||
| Age (in years) | 28.4 | 25–34 | 1.6 | ||
| Non-Hispanic White | 77.0 | ||||
| Hispanic | 10.2 | ||||
| Non-Hispanic African American | 9.8 | ||||
| Other non-Hispanic ethnic minority | 3.0 | ||||
| Social integration factors | |||||
| Being married at Wave 3 | (yes) | 21.2 | |||
| (no) | 78.8 | ||||
| Being married difference | 0.4 | −1–1 | 0.6 | ||
| Satisfactory spousal relationship at Wave 3 | 0.4 | 0–5 | 0.8 | ||
| Satisfactory spousal relationship at Wave 4 | 4.2 | 0–5 | 0.8 | ||
| Partner disapproved binge drinking at Wave 3 | 0.6 | 0–5 | 1.5 | ||
| Number of close friends at Wave 3 | 2.2 | 1–3 | 0.1 | ||
| Number of close friends difference | 1.1 | −1–3 | 1.0 | ||
| Close friends disapproved binge drinking at Wave 3 | 3.6 | 1–5 | 0.6 | ||
| Religiosity at Wave 3 | 1.3 | 0–5 | 1.3 | ||
| Religiosity difference | −0.1 | −5–5 | 1.4 | ||
| Volunteering at Wave 3 | (yes) | 28.6 | |||
| (no) | 71.4 | ||||
| Volunteering difference | 0.1 | −1–1 | 0.6 | ||
| Health/mental health/healthcare access factors | |||||
| General physical health at Wave 3 | 3.9 | 1–5 | 0.9 | ||
| General physical health difference | −0.3 | −4–4 | 1.0 | ||
| Depressive feelings at Wave 3 | 4.8 | 0–22 | 4.2 | ||
| Depressive feelings difference | 0.3 | −18–18 | 4.3 | ||
| Private insurance at Wave 4 | (yes) | 70.3 | |||
| (no) | 29.7 | ||||
| Public insurance at Wave 4 | (yes) | 5.5 | |||
| (no) | 94.5 | ||||
| Attended drug treatment at Wave 3 | (yes) | 4.4 | |||
| (no) | 95.6 | ||||
| Attended counseling services at Wave 4 | (yes) | 10.3 | |||
| (no) | 89.7 | ||||
| Drug use at Wave 4 | (yes) | 28.2 | |||
| (no) | 71.8 |
| Variables | Change to Non-Binge Drinking (Binge Drinking Maintained) | Change to Nondrinking (Binge Drinking Maintained) | ||
|---|---|---|---|---|
| RRR | LSE | RRR | LSE | |
| Social disorganization factors | ||||
| Unsafe neighborhood at Wave 3 (no) | 1.25 | 0.72 | 0.57 | 0.65 |
| Unsafe neighborhood difference | 1.00 | 0.41 | 0.55 | 0.59 |
| Involved in fights at Wave 3 | 0.83 | 0.10 | 0.92 | 0.21 |
| Being arrested at Wave 4 | 0.64 ** | 0.11 ** | 0.61 ** | 0.11 ** |
| Social structural and demographic factors | ||||
| Personal income at Wave 3 | 0.99 | 9.40 × 10−6 | 0.99 * | 0.00 * |
| Personal income difference | 0.99 * | 2.71 × 10−6 * | 0.99 | 7.81 × 10−6 |
| Education level at Wave 3 | 1.45 ** | 0.17 ** | 0.60 ** | 0.11 ** |
| Education level difference | 1.60 ** | 0.20 ** | 0.51 ** | 0.14 ** |
| Occupational skill at Wave 3 | 1.11 | 0.12 | 1.41 * | 0.25 * |
| Occupational skill difference | 1.05 | 0.07 | 1.22 * | 0.13 * |
| Male | 0.85 | 0.17 | 0.87 | 0.30 |
| Age (in years) | 1.05 | 0.06 | 1.45 ** | 0.13 ** |
| Hispanic (Non-Hispanic White [NHW]) | 1.06 | 0.26 | 1.30 | 0.63 |
| Non-Hispanic African American (NHW) | 2.28 * | 0.74 * | 5.16 ** | 3.04 ** |
| Other non-Hispanic ethnic minority (NHW) | 1.05 | 0.64 | 3.22 * | 2.14 * |
| Social integration factors | ||||
| Being married at Wave 3 (no) | 0.73 | 0.19 | 0.87 | 0.48 |
| Being married difference | 0.91 | 0.17 | 1.09 | 0.41 |
| Satisfactory spousal relationship at Wave 3 | 1.06 | 0.11 | 0.92 | 0.15 |
| Satisfactory spousal relationship at Wave 4 | 1.13 | 0.13 | 0.89 | 0.21 |
| Partner disapproved binge drinking at Wave 3 | 0.95 | 0.05 | 1.09 | 0.11 |
| Number of close friends at Wave 3 | 0.18 ** | 0.11 ** | 0.03 ** | 0.04 ** |
| Number of close friends difference | 0.75 ** | 0.08 ** | 0.56 ** | 0.12 ** |
| Close friends disapproved binge drinking at Wave 3 | 0.97 | 0.12 | 0.63 ** | 0.12 ** |
| Religiosity at Wave 3 | 1.03 | 0.08 | 1.10 | 0.17 |
| Religiosity difference | 1.06 | 0.07 | 1.22 | 0.15 |
| Volunteering at Wave 3 (no) | 1.37 | 0.31 | 0.77 | 0.33 |
| Volunteering difference | 1.13 | 0.19 | 0.77 | 0.24 |
| Health/mental health/healthcare access factors | ||||
| General physical health at Wave 3 | 1.03 | 0.13 | 0.98 | 0.22 |
| General physical health difference | 1.17 | 0.13 | 1.47 ** | 0.23 ** |
| Depressive feelings at Wave 3 | 1.02 | 0.03 | 1.01 | 0.05 |
| Depressive feelings difference | 0.98 | 0.02 | 0.99 | 0.05 |
| Private insurance at Wave 4 (no) | 0.79 | 0.16 | 1.47 | 0.48 |
| Public insurance at Wave 4 (no) | 0.56 | 0.22 | 1.08 | 0.61 |
| Attended drug treatment at Wave 3 (no) | 1.19 | 0.53 | 1.06 | 0.65 |
| Attended counseling services at Wave 4 (no) | 1.02 | 0.35 | 1.73 | 0.75 |
| Drug use at Wave 4 (no) | 0.73 | 0.14 | 0.38 ** | 0.12 ** |
| Constant | 3.71 | 8.45 | 0.49 | 2.20 |
| F = | 5.26 ** | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, T.C.; Lo, C.C. A Causal Analysis of Young Adults’ Binge Drinking Reduction and Cessation. Eur. J. Investig. Health Psychol. Educ. 2023, 13, 870-882. https://doi.org/10.3390/ejihpe13050066
Cheng TC, Lo CC. A Causal Analysis of Young Adults’ Binge Drinking Reduction and Cessation. European Journal of Investigation in Health, Psychology and Education. 2023; 13(5):870-882. https://doi.org/10.3390/ejihpe13050066
Chicago/Turabian StyleCheng, Tyrone C., and Celia C. Lo. 2023. "A Causal Analysis of Young Adults’ Binge Drinking Reduction and Cessation" European Journal of Investigation in Health, Psychology and Education 13, no. 5: 870-882. https://doi.org/10.3390/ejihpe13050066
APA StyleCheng, T. C., & Lo, C. C. (2023). A Causal Analysis of Young Adults’ Binge Drinking Reduction and Cessation. European Journal of Investigation in Health, Psychology and Education, 13(5), 870-882. https://doi.org/10.3390/ejihpe13050066










