Prevention of Work Absence Due to Back Pain: A Network Meta-Analysis
Abstract
1. Introduction
- Which preventive strategy is most effective in decreasing work absences due to BP (the number of people reporting sickness absenteeism due to BP and the number of days of work absence because of BP) among people with BP?
- Which preventive strategy is most effective in reducing BP episodes (the number of people reporting BP) among people with BP?
2. Materials and Methods
2.1. Study Selection
2.2. Search Strategy
2.3. Data Collection
2.4. Risk of Bias (ROB) and Certainty Assessment
2.5. Summary Measures
2.6. Data Analysis
3. Results
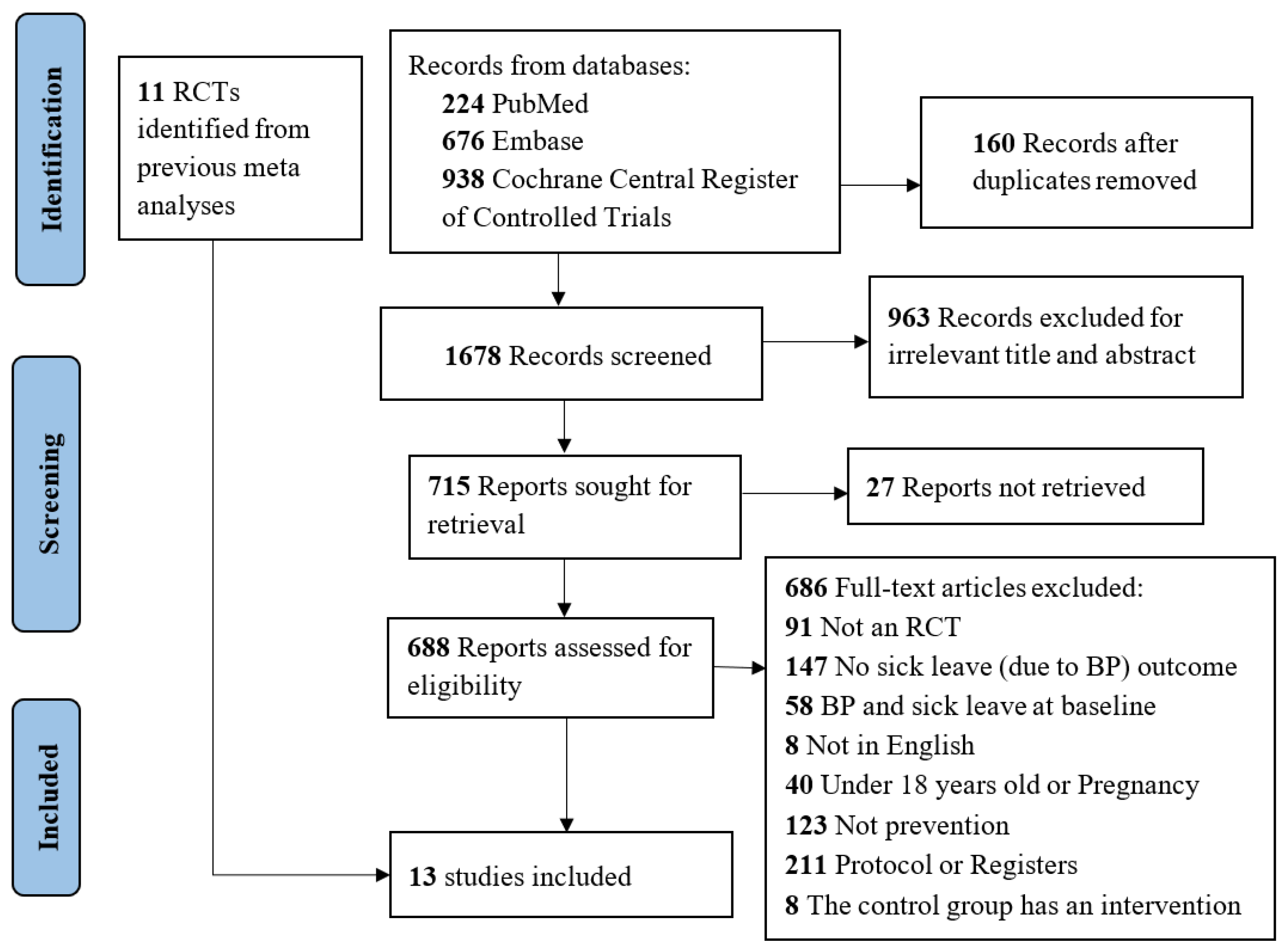
3.1. Study Selection
3.2. Risk of Bias (ROB)
3.3. Certainty Assessment
3.4. Network Graphs
3.5. Treatment Rankings
3.6. Sensitivity Analysis
3.7. Publication Bias
3.8. Subgroup Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO Scientific Group on the Burden of Musculoskeletal Conditions at the Start of the New Millennium. In The Burden of Musculoskeletal Conditions at the Start of the New Millenium: Report of a WHO Scientific Group; World Health Organization: Geneva, Switzerland, 2003.
- Da Silva, T.; Mills, K.; Brown, B.T.; Pocovi, N.; de Campos, T.; Maher, C.; Hancock, M.J. Recurrence of Low Back Pain Is Common: A Prospective Inception Cohort Study. J. Physiother. 2019, 65, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Wu, A.; March, L.; Zheng, X.; Huang, J.; Wang, X.; Zhao, J.; Blyth, F.M.; Smith, E.; Buchbinder, R.; Hoy, D. Global Low Back Pain Prevalence and Years Lived with Disability from 1990 to 2017: Estimates from the Global Burden of Disease Study 2017. Ann. Transl. Med. 2020, 8, 299. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, S.A.; Merryweather, A.; Thiese, M.S.; Hegmann, K.T.; Lu, M.-L.; Kapellusch, J.M.; Marras, W.S. Prevalence of Low Back Pain, Seeking Medical Care, and Lost Time Due to Low Back Pain among Manual Material Handling Workers in the United States. BMC Musculoskelet. Disord. 2019, 20, 243. [Google Scholar] [CrossRef] [PubMed]
- Abolfotouh, S.M.; Mahmoud, K.; Faraj, K.; Moammer, G.; ElSayed, A.; Abolfotouh, M.A. Prevalence, Consequences and Predictors of Low Back Pain among Nurses in a Tertiary Care Setting. Int. Orthop. (SICOT) 2015, 39, 2439–2449. [Google Scholar] [CrossRef] [PubMed]
- Mesas, A.E.; González, A.D.; Mesas, C.E.; de Andrade, S.M.; Magro, I.S.; del Llano, J. The Association of Chronic Neck Pain, Low Back Pain, and Migraine with Absenteeism Due to Health Problems in Spanish Workers. Spine 2014, 39, 1243–1253. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Steffens, D.; Maher, C.G.; Pereira, L.S.M.; Stevens, M.L.; Oliveira, V.C.; Chapple, M.; Teixeira-Salmela, L.F.; Hancock, M.J. Prevention of Low Back Pain: A Systematic Review and Meta-Analysis. JAMA Intern. Med. 2016, 176, 199. [Google Scholar] [CrossRef] [PubMed]
- Huang, R.; Ning, J.; Chuter, V.H.; Taylor, J.B.; Christophe, D.; Meng, Z.; Xu, Y.; Jiang, L. Exercise Alone and Exercise Combined with Education Both Prevent Episodes of Low Back Pain and Related Absenteeism: Systematic Review and Network Meta-Analysis of Randomised Controlled Trials (RCTs) Aimed at Preventing Back Pain. Br. J. Sports Med. 2020, 54, 766–770. [Google Scholar] [CrossRef]
- Ferreira, G.E.; Lin, C.-W.C.; Stevens, M.L.; Hancock, M.J.; Latimer, J.; Kelly, P.; Wisbey-Roth, T.; Maher, C.G. Exercise Is Medicine, But Perhaps Not for Preventing Low Back Pain: A Randomized Trial of Exercise and Education to Prevent Low Back Pain Recurrence. J. Orthop. Sports Phys. Ther. 2021, 51, 188–195. [Google Scholar] [CrossRef]
- Suni, J.H.; Kolu, P.; Tokola, K.; Raitanen, J.; Rinne, M.; Taulaniemi, A.; Parkkari, J.; Kankaanpää, M. Effectiveness and Cost-Effectiveness of Neuromuscular Exercise and Back Care Counseling in Female Healthcare Workers with Recurrent Non-Specific Low Back Pain: A Blinded Four-Arm Randomized Controlled Trial. BMC Public. Health 2018, 18, 1376. [Google Scholar] [CrossRef]
- Hutton, B.; Salanti, G.; Caldwell, D.M.; Chaimani, A.; Schmid, C.H.; Cameron, C.; Ioannidis, J.P.A.; Straus, S.; Thorlund, K.; Jansen, J.P.; et al. The PRISMA Extension Statement for Reporting of Systematic Reviews Incorporating Network Meta-Analyses of Health Care Interventions: Checklist and Explanations. Ann. Intern. Med. 2015, 162, 777–784. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 88, n71. [Google Scholar] [CrossRef] [PubMed]
- Newell, D.J. Intention-to-Treat Analysis: Implications for Quantitative and Qualitative Research. Int. J. Epidemiol. 1992, 21, 837–841. [Google Scholar] [CrossRef]
- Walter, S.D.; Yao, X. Effect Sizes Can Be Calculated for Studies Reporting Ranges for Outcome Variables in Systematic Reviews. J. Clin. Epidemiol. 2007, 60, 849–852. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-Bias VISualization (Robvis): An R Package and Shiny Web App for Visualizing Risk-of-Bias Assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Puhan, M.A.; Schunemann, H.J.; Murad, M.H.; Li, T.; Brignardello-Petersen, R.; Singh, J.A.; Kessels, A.G.; Guyatt, G.H. For the GRADE Working Group A GRADE Working Group Approach for Rating the Quality of Treatment Effect Estimates from Network Meta-Analysis. BMJ 2014, 349, g5630. [Google Scholar] [CrossRef] [PubMed]
- GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations. Updated October 2013. The GRADE Working Group. 2013. Available online: http://guidelinedevelopment.org/handbook (accessed on 7 June 2022).
- GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. McMaster University and Evidence Prime. 2022. Available online: http://Gradepro.Org (accessed on 15 January 2023).
- Rücker, G.; Schwarzer, G. Ranking Treatments in Frequentist Network Meta-Analysis Works without Resampling Methods. BMC Med. Res. Methodol. 2015, 15, 58. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.-W.; Lin, S.-H.; Wang, L.-C.; Chiu, H.-Y.; Lee, J.-A. Comparison of Antiviral Agents for Seasonal Influenza Outcomes in Healthy Adults and Children: A Systematic Review and Network Meta-Analysis. JAMA Netw. Open 2021, 4, e2119151. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing: Vienna, Austria, 2023. [Google Scholar]
- Rücker, G.; Krahn, U.; König, J.; Efthimiou, O.; Schwarzer, G. Netmeta: Network Meta-Analysis Using Frequentist Methods. Version 2.1-0. Available online: https://cran.r-project.org/web/packages/netmeta/index.html (accessed on 12 May 2022).
- Jackson, D.; Barrett, J.K.; Rice, S.; White, I.R.; Higgins, J.P.T. A Design-by-Treatment Interaction Model for Network Meta-Analysis with Random Inconsistency Effects. Stat. Med. 2014, 33, 3639–3654. [Google Scholar] [CrossRef]
- Chaimani, A.; Caldwell, D.M.; Li, T.; Higgins, J.P.T.; Salanti, G. Chapter 11: Undertaking Network Meta-Analyses. In Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (Updated February 2021); Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Cochrane: Newcastle, UK, 2021; Available online: www.training.cochrane.org/handbook (accessed on 7 June 2022).
- Dias, S.; Welton, N.J.; Caldwell, D.M.; Ades, A.E. Checking Consistency in Mixed Treatment Comparison Meta-Analysis. Stat. Med. 2010, 29, 932–944. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Sutton, A.J.; Ioannidis, J.P.A.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rücker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for Examining and Interpreting Funnel Plot Asymmetry in Meta-Analyses of Randomised Controlled Trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef] [PubMed]
- Owen, P.J.; Miller, C.T.; Mundell, N.L.; Verswijveren, S.J.J.M.; Tagliaferri, S.D.; Brisby, H.; Bowe, S.J.; Belavy, D.L. Which Specific Modes of Exercise Training Are Most Effective for Treating Low Back Pain? Network Meta-Analysis. Br. J. Sports Med. 2020, 54, 1279–1287. [Google Scholar] [CrossRef] [PubMed]
- Powell, K.E.; Paluch, A.E.; Blair, S.N. Physical Activity for Health: What Kind? How Much? How Intense? On Top of What? Annu. Rev. Public. Health 2011, 32, 349–365. [Google Scholar] [CrossRef] [PubMed]
- Thacker, S.B.; Gilchrist, J.; Stroup, D.F.; Kimsey, C.D. The Impact of Stretching on Sports Injury Risk: A Systematic Review of the Literature: Med. Sci. Sports Exerc. 2004, 36, 371–378. [Google Scholar] [CrossRef] [PubMed]
- Macedo, L.G.; Maher, C.G.; Latimer, J.; McAuley, J.H. Motor Control Exercise for Persistent, Nonspecific Low Back Pain: A Systematic Review. Phys. Ther. 2009, 89, 9–25. [Google Scholar] [CrossRef] [PubMed]
- Lønn, J.H.; Glomsrød, B.; Soukup, M.G.; Bø, K.; Larsen, S. Active Back School: Prophylactic Management for Low Back Pain. A Randomized, Controlled, 1-Year Follow-up Study. Spine 1999, 24, 865–871. [Google Scholar] [CrossRef] [PubMed]
- Glomsrød, B.; Lønn, J.H.; Soukup, M.G.; Bø, K.; Larsen, S. “Active Back School”, Prophylactic Management for Low Back Pain: Three-Year Follow-up of a Randomized, Controlled Trial. J. Rehabil. Med. 2001, 33, 26–30. [Google Scholar] [CrossRef]
- Gundewall, B.; Liljeqvist, M.; Hansson, T. Primary Prevention of Back Symptoms and Absence from Work. A Prospective Randomized Study among Hospital Employees. Spine 1993, 18, 587–594. [Google Scholar] [CrossRef]
- IJzelenberg, H.; Meerding, W.-J.; Burdorf, A. Effectiveness of a Back Pain Prevention Program: A Cluster Randomized Controlled Trial in an Occupational Setting. Spine 2007, 32, 711–719. [Google Scholar] [CrossRef]
- Kellett, K.M.; Kellett, D.A.; Nordholm, L.A. Effects of an Exercise Program on Sick Leave Due to Back Pain. Phys. Ther. 1991, 71, 283–291. [Google Scholar] [CrossRef]
- Soukup, M.G.; Glomsröd, B.; Lönn, J.H.; Bö, K.; Larsen, S. The Effect of a Mensendieck Exercise Program as Secondary Prophylaxis for Recurrent Low Back Pain: A Randomized, Controlled Trial With 12-Month Follow-Up. Spine 1999, 24, 1585–1591. [Google Scholar] [CrossRef]
- Soukup, M.G.; LÖnn, J.; GlomsrÖd, B.; Bö, K.; Larsen, S. Exercises and Education as Secondary Prevention for Recurrent Low Back Pain. Physiother. Res. Int. 2001, 6, 27–39. [Google Scholar] [CrossRef] [PubMed]
- van Poppel, M.N.M.; Koes, B.W.; van der Ploeg, T.; Smid, T.; Bouter, L.M. Lumbar Supports and Education for the Prevention of Low Back Pain in Industry: A Randomized Controlled Trial. JAMA 1998, 279, 1789–1794. [Google Scholar] [CrossRef] [PubMed]
- Warming, S.; Ebbehøj, N.E.; Wiese, N.; Larsen, L.H.; Duckert, J.; Tønnesen, H. Little Effect of Transfer Technique Instruction and Physical Fitness Training in Reducing Low Back Pain among Nurses: A Cluster Randomised Intervention Study. Ergonomics 2008, 51, 1530–1548. [Google Scholar] [CrossRef]
- Roussel, N.A.; Kos, D.; Demeure, I.; Heyrman, A.; Clerck, M.D.; Zinzen, E.; Struyf, F.; Nijs, J. Effect of a Multidisciplinary Program for the Prevention of Low Back Pain in Hospital Employees: A Randomized Controlled Trial. BMR 2015, 28, 539–549. [Google Scholar] [CrossRef] [PubMed]
- Chaléat-Valayer, E.; Denis, A.; Abelin-Genevois, K.; Zelmar, A.; Siani-Trebern, F.; Touzet, S.; Bergeret, A.; Colin, C.; Fassier, J.-B. Long-Term Effectiveness of an Educational and Physical Intervention for Preventing Low-Back Pain Recurrence: A Randomized Controlled Trial. Scand. J. Work. Environ. Health 2016, 42, 510–519. [Google Scholar] [CrossRef] [PubMed]
- Shiri, R.; Coggon, D.; Falah-Hassani, K. Exercise for the Prevention of Low Back Pain: Systematic Review and Meta-Analysis of Controlled Trials. Am. J. Epidemiol. 2018, 187, 1093–1101. [Google Scholar] [CrossRef]
- Choi, B.K.; Verbeek, J.H.; Tam, W.W.-S.; Jiang, J.Y. Exercises for Prevention of Recurrences of Low-Back Pain. Cochrane Database Syst. Rev. 2010, 1, CD006555. [Google Scholar] [CrossRef]
- Kool, J.; de Bie, R.; Oesch, P.; Knüsel, O.; Brandt, P.v.d.; Bachmann, S. Exercise Reduces Sick Leave in Patients with Non-Acute Non-Specific Low Back Pain: A Meta-Analysis. J. Rehabil. Med. 2004, 36, 49–62. [Google Scholar] [CrossRef][Green Version]

| No | Author, Year | Participants (Mean Age; SD or Range); Sex | Outcome | Intervention and Control Groups | Follow-Up Months |
|---|---|---|---|---|---|
| 1 | Lønn 1999 [32] | 81 participants recruited from referrals and advertisement; (39.4 years; 19.2–49.8); 46% male | Number of subjects reporting sick leave Number of days of sick leave due to BP Number of episodes of low BP | Exercise and education: resistance (strength training of muscles), stretching exercises Control group: no intervention | 12 months |
| 2 | Glomsrød 2001 [33] | 81 participants recruited from referrals and advertisement; (39.4 years; 19.2–49.8); 46% male | Number of subjects reporting sick leave Number of days of sick leave due to episodes of BP Number of episodes of low BP | Exercise and education: resistance (strength training of muscles), stretching exercises Control group: no intervention | 36 months |
| 3 | Gundewall 1993 [34] | 69 nurses and nurse’s aides; (37.5 years; 10.5); 1% male | Number of subjects with work absence Number of lost work-days due to BP | Exercise: resistance exercises (back muscle exercises to increase endurance and muscle strength) Control: no intervention | 13 months |
| 4 | Ijzelenberg 2007 [35] | 489 workers from physically demanding jobs; (41.3 years; 9.7); 98% male | Number of people absent from work during the previous six months due to BP Number of participants with low BP | Education and ergonomic adjustments Control: usual care | 12 months |
| 5 | Kellett 1991 [36] | 111 employees of kitchen unit production; (41.7 years; 10.1); 70% male | Number of people with sick leave because of BP Number of sick leave days due to BP | Exercise and education: resistance, stretching exercises Control: no intervention | 18 months |
| 6 | Soukup 1999 [37] | 77 outpatients from general clinical practices; (39.6 years; 21.2–49.8); 47% male | Number of participants with sick leave for BP Number of days of sick leave due to BP Number of participants with recurrence of low BP episodes | Exercise and education: (Mensendieck) resistance, stretching exercises Control: no intervention | 12 months |
| 7 | Soukup 2001 [38] | 77 outpatients from general clinical practices; (37.7 years; 8.0); 47% male | Number of participants with sick leave due to BP Number of days of sick leave due to BP Number of subjects with recurrent episodes of low BP | Exercise and education: Mensendieck resistance, stretching exercises Control: no intervention | 36 months |
| 8 | van Poppel 1998 [39] | 312 airline employees; (35.1 years; 7.8); Not available | Number of subjects with sick leave because of BP Number of days per month of sick leave because of BP Number of subjects with low BP | Education and back belts Education Back belts Control: no intervention | 6 months |
| 9 | Warming 2008 [40] | 181 hospital nurses; (34.8 years; 9.3); Not available | Number of subjects with sick leave because of BP Number of subjects who experienced low BP | Education Exercise: aerobic and resistance exercises Control: no intervention | 12 months |
| 10 | Roussel 2015 [41] | 69 hospital workers; (40.8 years; not available); 18% male | Number of workers with work absenteeism because of BP Number of subjects with low BP | Exercise and ergonomics: (stabilization) motor control Control: no intervention | 6 months |
| 11 | Chaléat-Valayer 2016 [42] | 342 healthcare workers; (47.2 years; no information); 23% male | Percentage of participants with sick leave related to chronic low BP (pain for >3 months) Duration of sick leave due to BP episodes (days) Percentage of participants with ≥1 recurrence of low BP with sick leave | Exercise and education: stretching exercises Control: no intervention | 24 months |
| 12 | Suni 2018 [10] | 219 female healthcare workers; (46.4 years; 6.8); 0% male | Number of days absent from work due to low BP | Exercise: resistance, stretching exercises Exercise and counselling *: resistance, stretching exercises Counselling *: education Control: no intervention | 12 months |
| 13 | Ferreira 2021 [9] | 111 participants recruited from primary care and community facilities; (50.2 years; 13.1); 50% male | Number of people with sick leave because of BP Number of participants with recurrence of low BP | Exercise and education: resistance exercise Control: minimal intervention | 12 months |
| (a) | ||||||
| Exercise | 0.10 (0.01;0.69) | |||||
| 0.11 (0.02; 0.82) | Exercise education | 0.38 (0.08;1.81) | 0.86 (0.68; 1.08) | |||
| 0.14 (0.01; 1.94) | 1.28 (0.23; 7.10) | Exercise ergonomics | 0.67 (0.12; 3.65) | |||
| 0.10 (0.01; 0.82) | 0.93 (0.50; 1.74) | 0.73 (0.12; 4.42) | Education | 0.86 (0.47; 1.57) | ||
| 0.10 (0.01; 0.80) | 0.90 (0.47; 1.74) | 0.70 (0.12; 4.31) | 0.96 (0.41; 2.26) | Education ergonomics | 0.95 (0.51; 1.76) | |
| 0.10 (0.01; 0.69) | 0.85 (0.68; 1.07) | 0.67 (0.12; 3.65) | 0.91 (0.51; 1.64) | 0.95 (0.51; 1.76) | Usual care | 0.69 (0.35; 1.37) |
| 0.07 (0.01; 0.53) | 0.59 (0.29; 1.21) | 0.46 (0.07; 2.89) | 0.63 (0.26; 1.55) | 0.65 (0.26; 1.65) | 0.69 (0.35; 1.37) | Back belts |
| (b) | ||||||
| Exercise education | −0.26 (−1.28; 0.75) | −0.14 (−1.17; 0.89) | −0.37 (−0.75; 0.01) | |||
| −0.16 (−0.88; 0.57) | Exercise | 0.12 (−0.91; 1.15) | −0.21 (−0.94; 0.51) | |||
| −0.19 (−1.09; 0.71) | −0.03 (−1.00; 0.93) | Education | 0.00 (−1.03; 1.03) | |||
| −0.39 (−0.77; −0.02) | −0.24 (−0.92; 0.44) | −0.20 (−1.09; 0.69) | Usual care | |||
| (c) | ||||||
| Exercise education | 0.81 (0.67;0.97) | 0.60 (0.34; 1.07) | ||||
| 0.80 (0.67; 0.96) | Usual care | 0.96 (0.61; 1.52) | 0.93 (0.63; 1.38) | 0.92 (0.66; 1.28) | 0.50 (0.05; 5.29) | |
| 0.77 (0.47; 1.26) | 0.96 (0.61; 1.52) | Back belts | ||||
| 0.75 (0.48; 1.15) | 0.93 (0.63; 1.38) | 0.97 (0.53; 1.78) | Education ergonomics | |||
| 0.72 (0.51; 1.02) | 0.90 (0.65; 1.23) | 0.93 (0.53; 1.63) | 0.96 (0.58; 1.60) | Education | ||
| 0.40 (0.04; 4.27) | 0.50 (0.05; 5.29) | 0.52 (0.05; 5.75) | 0.54 (0.05; 5.88) | 0.56 (0.05; 6.03) | Exercise ergonomics | |
| No. | Intervention | Number of People Reporting Work Absence | Number of Days of Work Absence | Number of People Reporting BP | |||
|---|---|---|---|---|---|---|---|
| p-Score | Rank | p-Score | Rank | p-Score | Rank | ||
| 1 | Exercise | 0.98 | 1 | 0.54 | 2 | - | - |
| 2 | Exercise education | 0.58 | 2 | 0.77 | 1 | 0.90 | 1 |
| 3 | Exercise ergonomics | 0.57 | 3 | - | - | 0.28 | 6 |
| 4 | Education | 0.47 | 4 | 0.49 | 3 | 0.36 | 5 |
| 5 | Education ergonomics | 0.43 | 5 | - | - | 0.43 | 4 |
| 6 | Usual care | 0.35 | 6 | 0.20 | 4 | 0.54 | 2 |
| 7 | Back belts | 0.13 | 7 | - | - | 0.49 | 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ta, K.-N.T.; Bai, C.-H.; Chuang, K.-J. Prevention of Work Absence Due to Back Pain: A Network Meta-Analysis. Eur. J. Investig. Health Psychol. Educ. 2023, 13, 2891-2903. https://doi.org/10.3390/ejihpe13120200
Ta K-NT, Bai C-H, Chuang K-J. Prevention of Work Absence Due to Back Pain: A Network Meta-Analysis. European Journal of Investigation in Health, Psychology and Education. 2023; 13(12):2891-2903. https://doi.org/10.3390/ejihpe13120200
Chicago/Turabian StyleTa, Kim-Ngan Thi, Chyi-Huey Bai, and Kai-Jen Chuang. 2023. "Prevention of Work Absence Due to Back Pain: A Network Meta-Analysis" European Journal of Investigation in Health, Psychology and Education 13, no. 12: 2891-2903. https://doi.org/10.3390/ejihpe13120200
APA StyleTa, K.-N. T., Bai, C.-H., & Chuang, K.-J. (2023). Prevention of Work Absence Due to Back Pain: A Network Meta-Analysis. European Journal of Investigation in Health, Psychology and Education, 13(12), 2891-2903. https://doi.org/10.3390/ejihpe13120200








