The Association between Nonsuicidal Self-Injury and Perfectionism in Adolescence: The Role of Mental Disorders
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. Participants and Data Collection
2.3. Measures
2.4. Statistical Analysis
3. Results
3.1. Sample and Descriptive Statistics
3.2. Statistical Analysis Related to Our Hypotheses
3.2.1. Regression Analysis
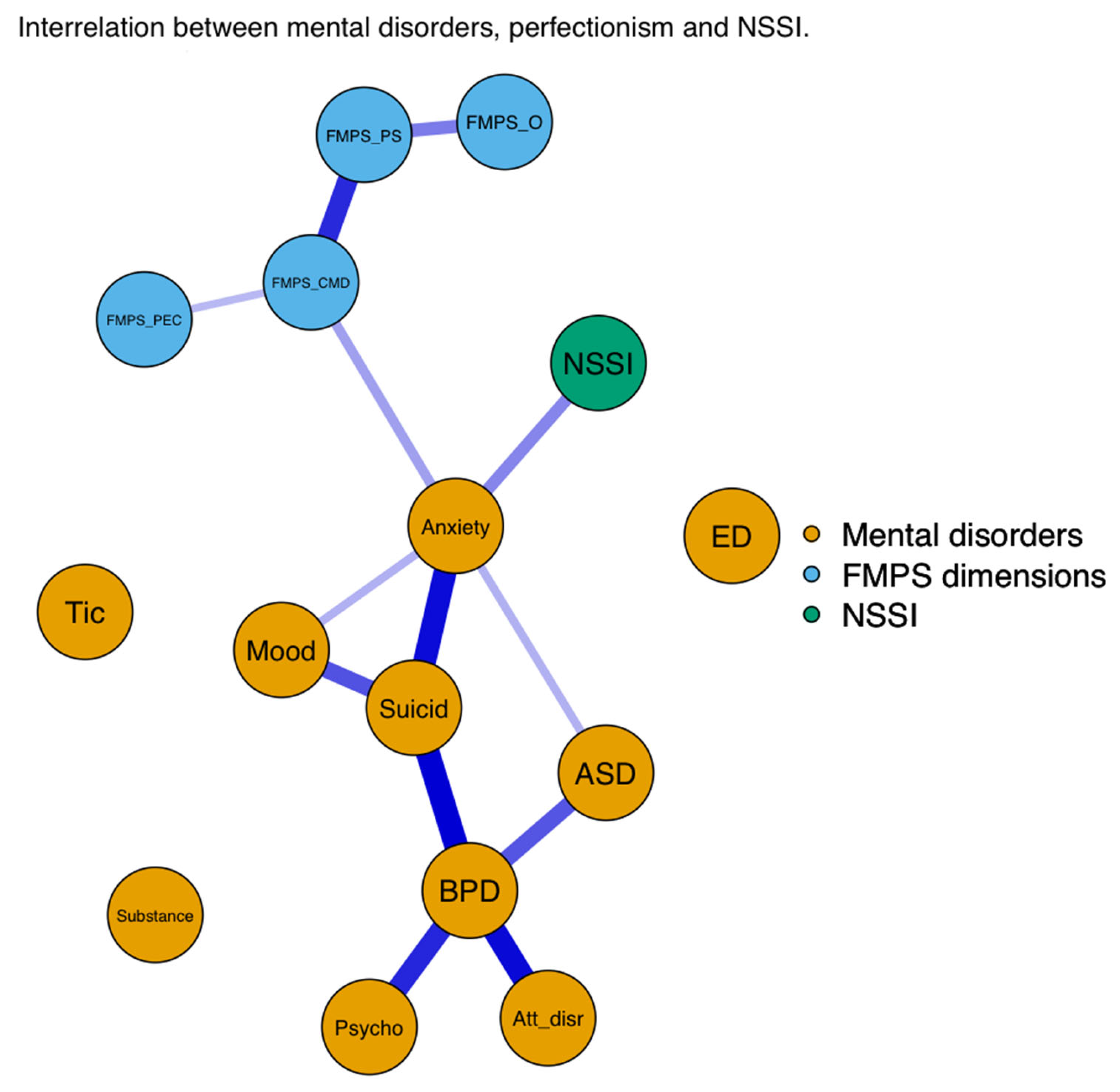
3.2.2. Network Analysis


4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Variable | Variable 1 | Variable 2 | Value | prop0 | q2.5 | q97.5 | q2.5_non0 | q97.5_non0 |
|---|---|---|---|---|---|---|---|---|
| FMPS_CMD—FMPS_PS | FMPS_CMD | FMPS_PS | 0.49 | <0.01 | 0.38 | 0.58 | 0.38 | 0.58 |
| FMPS_PS—FMPS_O | FMPS_PS | FMPS_O | 0.36 | <0.01 | 0.22 | 0.48 | 0.22 | 0.48 |
| Anxiety—Suicid | Anxiety | Suicid | 0.82 | 0.07 | <0.01 | 1.60 | 0.28 | 1.62 |
| BPD—Suicid | BPD | Suicid | 4.23 | 0.14 | <0.01 | 37.02 | 0.37 | 40.29 |
| Mood—Suicid | Mood | Suicid | 0.45 | 0.19 | <0.01 | 1.02 | 0.21 | 1.06 |
| Anxiety—NSSI | Anxiety | NSSI | 0.49 | 0.29 | <0.01 | 1.61 | 0.23 | 1.76 |
| ASD—BPD | ASD | BPD | 2.84 | 0.41 | <0.01 | 28.78 | 0.34 | 31.78 |
| FMPS_CMD—FMPS_PEC | FMPS_CMD | FMPS_PEC | 0.13 | 0.43 | <0.01 | 0.32 | 0.14 | 0.34 |
| Anxiety—ASD | Anxiety | ASD | 0.38 | 0.44 | <0.01 | 1.22 | 0.21 | 1.39 |
| Psychotic—BPD | Psychotic | BPD | 1.98 | 0.44 | <0.01 | 20.43 | 0.32 | 24.71 |
| Atten_disr—BPD | Atten_disr | BPD | 2.59 | 0.45 | <0.01 | 23.83 | 0.41 | 29.20 |
| Anxiety—FMPS_CMD | Anxiety | FMPS_CMD | 0.21 | 0.48 | <0.01 | 0.65 | 0.15 | 0.94 |
| Mood—Anxiety | Mood | Anxiety | 0.20 | 0.58 | <0.01 | 0.76 | 0.17 | 0.85 |
| ED—FMPS_CMD | ED | FMPS_CMD | 0.23 | 0.59 | <0.01 | 0.54 | 0.12 | 0.87 |
| ED—Suicid | ED | Suicid | 0.24 | 0.68 | <0.01 | 0.84 | 0.21 | 1.20 |
| Tic—Psychotic | Tic | Psychotic | 0.62 | 0.68 | <0.01 | 4.13 | 0.43 | 15.90 |
| Mood—ED | Mood | ED | 0.18 | 0.69 | <0.01 | 0.71 | 0.17 | 0.89 |
| Psychotic—Suicid | Psychotic | Suicid | 0.65 | 0.71 | <0.01 | 5.23 | 0.27 | 21.95 |
| Anxiety—Psychotic | Anxiety | Psychotic | 0.73 | 0.71 | <0.01 | 3.04 | 0.26 | 31.76 |
| Anxiety—ED | Anxiety | ED | 0.25 | 0.72 | <0.01 | 0.99 | 0.19 | 7.67 |
| ED—BPD | ED | BPD | 0.87 | 0.74 | <0.01 | 10.14 | 0.25 | 27.91 |
| Tic—ASD | Tic | ASD | 0.37 | 0.74 | <0.01 | 1.20 | 0.30 | 12.55 |
| ASD—FMPS_O | ASD | FMPS_O | −0.06 | 0.76 | −0.38 | <0.01 | −0.45 | −0.15 |
| Anxiety—FMPS_PEC | Anxiety | FMPS_PEC | 0.07 | 0.77 | <0.01 | 0.42 | 0.14 | 0.53 |
| Mood—Psychotic | Mood | Psychotic | 0.27 | 0.78 | <0.01 | 1.49 | 0.22 | 7.86 |
| ED—NSSI | ED | NSSI | 0.18 | 0.79 | <0.01 | 0.78 | 0.19 | 1.07 |
| BPD—FMPS_CMD | BPD | FMPS_CMD | 0.20 | 0.81 | <0.01 | 2.53 | 0.18 | 7.58 |
| ASD—FMPS_CMD | ASD | FMPS_CMD | 0.04 | 0.84 | <0.01 | 0.35 | 0.14 | 0.53 |
| Atten_disr—Suicid | Atten_disr | Suicid | 0.31 | 0.84 | <0.01 | 2.72 | 0.30 | 15.99 |
| Mood—Substance | Mood | Substance | 0.06 | 0.87 | <0.01 | 0.60 | 0.22 | 0.84 |
| Mood—NSSI | Mood | NSSI | 0.05 | 0.88 | <0.01 | 0.46 | 0.14 | 0.94 |
| Mood—Atten_disr | Mood | Atten_disr | 0.15 | 0.90 | <0.01 | 1.06 | 0.21 | 10.76 |
| FMPS_PEC—FMPS_O | FMPS_PEC | FMPS_O | 0.01 | 0.91 | <0.01 | 0.14 | 0.07 | 0.20 |
| Anxiety—Atten_disr | Anxiety | Atten_disr | 0.16 | 0.91 | <0.01 | 1.39 | 0.28 | 13.90 |
| Anxiety—BPD | Anxiety | BPD | −0.74 | 0.91 | −12.29 | <0.01 | −29.94 | 4.32 |
| Tic—BPD | Tic | BPD | 0.49 | 0.92 | <0.01 | 3.92 | 0.26 | 47.45 |
| BPD—NSSI | BPD | NSSI | 0.68 | 0.92 | <0.01 | 8.67 | 0.26 | 53.21 |
| Anxiety—Substance | Anxiety | Substance | 0.04 | 0.92 | <0.01 | 0.53 | 0.19 | 0.97 |
| Atten_disr—ASD | Atten_disr | ASD | 0.29 | 0.93 | <0.01 | 2.37 | 0.28 | 24.33 |
| ASD—Suicid | ASD | Suicid | 0.03 | 0.94 | <0.01 | 0.45 | 0.16 | 0.93 |
| Atten_disr—FMPS_PEC | Atten_disr | FMPS_PEC | 0.05 | 0.94 | <0.01 | 0.47 | 0.17 | 5.44 |
| Substance—FMPS_PEC | Substance | FMPS_PEC | 0.02 | 0.94 | <0.01 | 0.26 | 0.10 | 0.45 |
| ED—ASD | ED | ASD | −0.08 | 0.95 | −0.63 | <0.01 | −20.18 | 0.39 |
| Mood—FMPS_CMD | Mood | FMPS_CMD | 0.01 | 0.96 | <0.01 | 0.19 | 0.09 | 0.35 |
| Substance—ASD | Substance | ASD | −0.02 | 0.96 | −0.51 | <0.01 | −1.85 | −0.24 |
| Mood—FMPS_PEC | Mood | FMPS_PEC | 0.01 | 0.96 | <0.01 | 0.21 | 0.10 | 0.49 |
| NSSI—FMPS_O | NSSI | FMPS_O | −0.01 | 0.96 | −0.17 | <0.01 | −0.44 | −0.10 |
| Substance—Atten_disr | Substance | Atten_disr | 0.05 | 0.97 | <0.01 | 0.52 | −0.98 | 12.60 |
| ED—FMPS_PEC | ED | FMPS_PEC | 0.01 | 0.97 | <0.01 | 0.19 | −0.40 | 1.03 |
| Substance—BPD | Substance | BPD | 0.16 | 0.97 | <0.01 | 0.52 | 0.28 | 49.07 |
| Substance—ED | Substance | ED | 0.05 | 0.97 | <0.01 | 0.28 | 0.22 | 37.25 |
| Atten_disr—Psychotic | Atten_disr | Psychotic | <0.01 | 0.97 | <0.01 | 0.32 | −17.63 | 4.15 |
| Psychotic—FMPS_CMD | Psychotic | FMPS_CMD | 0.04 | 0.97 | <0.01 | 0.19 | 0.14 | 14.80 |
| FMPS_PEC—FMPS_PS | FMPS_PEC | FMPS_PS | <0.01 | 0.97 | <0.01 | 0.11 | 0.09 | 0.25 |
| Mood—BPD | Mood | BPD | 0.04 | 0.97 | <0.01 | 0.13 | −1.23 | 8.30 |
| Substance—NSSI | Substance | NSSI | 0.01 | 0.97 | <0.01 | 0.23 | 0.22 | 0.89 |
| Atten_disr—ED | Atten_disr | ED | <0.01 | 0.98 | <0.01 | <0.01 | −22.10 | 6.21 |
| Tic—Suicid | Tic | Suicid | −0.13 | 0.98 | <0.01 | <0.01 | −38.17 | −0.37 |
| Mood—Tic | Mood | Tic | 0.05 | 0.98 | <0.01 | <0.01 | 0.35 | 26.08 |
| Suicid—NSSI | Suicid | NSSI | <0.01 | 0.98 | <0.01 | <0.01 | −1.02 | 1.00 |
| Mood—ASD | Mood | ASD | −0.01 | 0.98 | <0.01 | <0.01 | −1.63 | 0.26 |
| NSSI—FMPS_CMD | NSSI | FMPS_CMD | <0.01 | 0.98 | <0.01 | <0.01 | 0.12 | 0.27 |
| ED—Psychotic | ED | Psychotic | 0.04 | 0.98 | <0.01 | <0.01 | −3.87 | 42.14 |
| Mood—FMPS_O | Mood | FMPS_O | <0.01 | 0.98 | <0.01 | <0.01 | −0.30 | −0.12 |
| Psychotic—FMPS_O | Psychotic | FMPS_O | −0.03 | 0.98 | <0.01 | <0.01 | −11.18 | −0.19 |
| Tic—FMPS_O | Tic | FMPS_O | <0.01 | 0.98 | <0.01 | <0.01 | −0.73 | −0.16 |
| Psychotic—ASD | Psychotic | ASD | −0.03 | 0.99 | <0.01 | <0.01 | −16.12 | 1.98 |
| ASD—FMPS_PEC | ASD | FMPS_PEC | <0.01 | 0.99 | <0.01 | <0.01 | 0.11 | 0.37 |
| Tic—FMPS_PEC | Tic | FMPS_PEC | −0.01 | 0.99 | <0.01 | <0.01 | −2.31 | −0.15 |
| Suicid—FMPS_CMD | Suicid | FMPS_CMD | <0.01 | 0.99 | <0.01 | <0.01 | 0.09 | 0.55 |
| Atten_disr—Tic | Atten_disr | Tic | −0.06 | 0.99 | <0.01 | <0.01 | −52.09 | 0.71 |
| ASD—NSSI | ASD | NSSI | <0.01 | 0.99 | <0.01 | <0.01 | −0.41 | 0.56 |
| Anxiety—Tic | Anxiety | Tic | 0.01 | 0.99 | <0.01 | <0.01 | −0.37 | 6.12 |
| Substance—Psychotic | Substance | Psychotic | <0.01 | 0.99 | <0.01 | <0.01 | −0.97 | 1.97 |
| Tic—NSSI | Tic | NSSI | 0.03 | 1.00 | <0.01 | <0.01 | −2.50 | 18.05 |
| Anxiety—FMPS_PS | Anxiety | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | −0.83 | −0.35 |
| Anxiety—FMPS_O | Anxiety | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | −0.28 | 0.81 |
| Atten_disr—NSSI | Atten_disr | NSSI | −0.05 | 1.00 | <0.01 | <0.01 | −32.97 | −1.63 |
| BPD—FMPS_O | BPD | FMPS_O | −0.02 | 1.00 | <0.01 | <0.01 | −9.99 | −1.86 |
| Tic—ED | Tic | ED | 0.01 | 1.00 | <0.01 | <0.01 | 0.23 | 10.70 |
| Substance—Suicid | Substance | Suicid | <0.01 | 1.00 | <0.01 | <0.01 | 0.25 | 0.50 |
| Suicid—FMPS_PS | Suicid | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | −0.47 | −0.29 |
| ASD—FMPS_PS | ASD | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | −0.48 | 0.15 |
| Atten_disr—FMPS_CMD | Atten_disr | FMPS_CMD | <0.01 | 1.00 | <0.01 | <0.01 | −3.73 | −0.81 |
| BPD—FMPS_PEC | BPD | FMPS_PEC | <0.01 | 1.00 | <0.01 | <0.01 | −2.42 | −0.48 |
| Psychotic—FMPS_PEC | Psychotic | FMPS_PEC | <0.01 | 1.00 | <0.01 | <0.01 | −0.56 | −0.35 |
| ED—FMPS_O | ED | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | 0.20 | 0.39 |
| Suicid—FMPS_PEC | Suicid | FMPS_PEC | <0.01 | 1.00 | <0.01 | <0.01 | 0.17 | 0.36 |
| Psychotic—NSSI | Psychotic | NSSI | <0.01 | 1.00 | <0.01 | <0.01 | −3.28 | −3.28 |
| Substance—Tic | Substance | Tic | <0.01 | 1.00 | <0.01 | <0.01 | −0.47 | −0.47 |
| Substance—FMPS_CMD | Substance | FMPS_CMD | <0.01 | 1.00 | <0.01 | <0.01 | 0.32 | 0.32 |
| Suicid—FMPS_O | Suicid | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | −0.30 | −0.30 |
| NSSI—FMPS_PEC | NSSI | FMPS_PEC | <0.01 | 1.00 | <0.01 | <0.01 | −0.28 | −0.28 |
| ED—FMPS_PS | ED | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | 0.27 | 0.27 |
| NSSI—FMPS_PS | NSSI | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | 0.22 | 0.22 |
| Atten_disr—FMPS_O | Atten_disr | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Atten_disr—FMPS_PS | Atten_disr | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| BPD—FMPS_PS | BPD | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| FMPS_CMD—FMPS_O | FMPS_CMD | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Mood—FMPS_PS | Mood | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Psychotic—FMPS_PS | Psychotic | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Substance—FMPS_O | Substance | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Substance—FMPS_PS | Substance | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Tic—FMPS_CMD | Tic | FMPS_CMD | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Tic—FMPS_PS | Tic | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Variable | Variable 1 | Variable 2 | Value | prop0 | q2.5 | q97.5 | q2.5_non0 | q97.5_non0 |
|---|---|---|---|---|---|---|---|---|
| Anxiety—Atten_disr | Anxiety | Atten_disr | 0.16 | 0.90 | <0.01 | 0.79 | 0.25 | 18.67 |
| Anxiety—ASD | Anxiety | ASD | 0.26 | 0.63 | <0.01 | 1.25 | 0.21 | 2.17 |
| Anxiety—BPD | Anxiety | BPD | −0.91 | 0.89 | −12.67 | <0.01 | −36.68 | 2.34 |
| Anxiety—ED | Anxiety | ED | 0.34 | 0.75 | <0.01 | 1.21 | 0.17 | 14.88 |
| Anxiety—FMPS_CMD | Anxiety | FMPS_CMD | 0.15 | 0.60 | <0.01 | 0.50 | 0.14 | 0.65 |
| Anxiety—FMPS_O | Anxiety | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | 0.28 | 1.88 |
| Anxiety—FMPS_PEC | Anxiety | FMPS_PEC | 0.09 | 0.70 | <0.01 | 0.46 | 0.16 | 0.57 |
| Anxiety—FMPS_PS | Anxiety | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Anxiety—NSSI_intra | Anxiety | NSSI_intra | 0.76 | 0.12 | <0.01 | 1.58 | 0.25 | 1.67 |
| Anxiety—Psychotic | Anxiety | Psychotic | 0.83 | 0.68 | <0.01 | 7.19 | 0.26 | 22.18 |
| Anxiety—Substance | Anxiety | Substance | 0.02 | 0.96 | <0.01 | 0.45 | 0.16 | 1.19 |
| Anxiety—Suicid | Anxiety | Suicid | 1.07 | 0.05 | <0.01 | 2.68 | 0.32 | 2.70 |
| Anxiety—Tic | Anxiety | Tic | −0.05 | 1.00 | <0.01 | <0.01 | −44.40 | −8.14 |
| Atten_disr—ASD | Atten_disr | ASD | 0.20 | 0.94 | <0.01 | 1.26 | 0.23 | 22.30 |
| Atten_disr—BPD | Atten_disr | BPD | 1.79 | 0.54 | <0.01 | 15.35 | 0.43 | 24.66 |
| Atten_disr—ED | Atten_disr | ED | 0.10 | 0.97 | <0.01 | 0.43 | −3.61 | 50.86 |
| Atten_disr—FMPS_CMD | Atten_disr | FMPS_CMD | <0.01 | 1.00 | <0.01 | <0.01 | 0.25 | 0.25 |
| Atten_disr—FMPS_O | Atten_disr | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Atten_disr—FMPS_PEC | Atten_disr | FMPS_PEC | 0.03 | 0.94 | <0.01 | 0.46 | 0.20 | 4.45 |
| Atten_disr—FMPS_PS | Atten_disr | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Atten_disr—NSSI_intra | Atten_disr | NSSI_intra | <0.01 | 1.00 | <0.01 | <0.01 | −1.42 | −1.42 |
| Atten_disr—Psychotic | Atten_disr | Psychotic | 0.03 | 0.98 | <0.01 | <0.01 | −11.64 | 13.81 |
| Atten_disr—Suicid | Atten_disr | Suicid | 0.20 | 0.88 | <0.01 | 1.44 | 0.27 | 10.17 |
| Atten_disr—Tic | Atten_disr | Tic | −0.01 | 0.99 | <0.01 | <0.01 | −21.38 | 13.62 |
| ASD—BPD | ASD | BPD | 4.15 | 0.35 | <0.01 | 32.82 | 0.33 | 36.56 |
| ASD—FMPS_CMD | ASD | FMPS_CMD | 0.05 | 0.83 | <0.01 | 0.38 | 0.12 | 0.62 |
| ASD—FMPS_O | ASD | FMPS_O | −0.04 | 0.86 | −0.37 | <0.01 | −0.53 | −0.14 |
| ASD—FMPS_PEC | ASD | FMPS_PEC | <0.01 | 0.98 | <0.01 | <0.01 | 0.10 | 0.38 |
| ASD—FMPS_PS | ASD | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | −0.35 | −0.27 |
| ASD—NSSI_intra | ASD | NSSI_intra | <0.01 | 0.99 | <0.01 | <0.01 | −0.62 | 0.82 |
| ASD—Suicid | ASD | Suicid | −0.05 | 0.97 | <0.01 | <0.01 | −46.84 | 2.07 |
| BPD—FMPS_CMD | BPD | FMPS_CMD | 0.10 | 0.88 | <0.01 | 0.75 | 0.18 | 5.04 |
| BPD—FMPS_O | BPD | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | −4.41 | −4.41 |
| BPD—FMPS_PEC | BPD | FMPS_PEC | −0.02 | 0.99 | <0.01 | <0.01 | −2.98 | −0.40 |
| BPD—FMPS_PS | BPD | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| BPD—NSSI_intra | BPD | NSSI_intra | 2.23 | 0.58 | <0.01 | 19.10 | 0.30 | 26.05 |
| BPD—Suicid | BPD | Suicid | 5.50 | 0.16 | <0.01 | 41.77 | 0.39 | 43.17 |
| ED—ASD | ED | ASD | −0.43 | 0.94 | −1.35 | <0.01 | −60.63 | −0.30 |
| ED—BPD | ED | BPD | 0.95 | 0.74 | <0.01 | 12.33 | 0.27 | 32.50 |
| ED—FMPS_CMD | ED | FMPS_CMD | 0.30 | 0.76 | <0.01 | 0.88 | 0.14 | 13.52 |
| ED—FMPS_O | ED | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | 0.11 | 0.11 |
| ED—FMPS_PEC | ED | FMPS_PEC | 0.02 | 0.96 | <0.01 | 0.22 | 0.11 | 7.27 |
| ED—FMPS_PS | ED | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| ED—NSSI_intra | ED | NSSI_intra | 0.89 | 0.32 | <0.01 | 5.71 | 0.24 | 9.82 |
| ED—Psychotic | ED | Psychotic | −0.17 | 0.98 | <0.01 | <0.01 | −97.13 | 31.82 |
| ED—Suicid | ED | Suicid | 0.26 | 0.80 | <0.01 | 0.97 | 0.23 | 17.47 |
| FMPS_CMD—FMPS_O | FMPS_CMD | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| FMPS_CMD—FMPS_PEC | FMPS_CMD | FMPS_PEC | 0.14 | 0.41 | <0.01 | 0.33 | 0.14 | 0.35 |
| FMPS_CMD—FMPS_PS | FMPS_CMD | FMPS_PS | 0.49 | <0.01 | 0.38 | 0.59 | 0.38 | 0.59 |
| FMPS_PEC—FMPS_O | FMPS_PEC | FMPS_O | 0.01 | 0.91 | <0.01 | 0.15 | 0.08 | 0.21 |
| FMPS_PEC—FMPS_PS | FMPS_PEC | FMPS_PS | <0.01 | 0.98 | <0.01 | <0.01 | 0.09 | 0.21 |
| FMPS_PS—FMPS_O | FMPS_PS | FMPS_O | 0.35 | <0.01 | 0.21 | 0.49 | 0.22 | 0.49 |
| Mood—Anxiety | Mood | Anxiety | 0.08 | 0.84 | <0.01 | 0.50 | 0.14 | 1.51 |
| Mood—Atten_disr | Mood | Atten_disr | 0.13 | 0.89 | <0.01 | 0.89 | 0.25 | 10.88 |
| Mood—ASD | Mood | ASD | <0.01 | 0.99 | <0.01 | <0.01 | −1.00 | 0.89 |
| Mood—BPD | Mood | BPD | 0.09 | 0.97 | <0.01 | 0.50 | −0.38 | 17.36 |
| Mood—ED | Mood | ED | 0.27 | 0.68 | <0.01 | 0.75 | 0.17 | 1.02 |
| Mood—FMPS_CMD | Mood | FMPS_CMD | 0.01 | 0.96 | <0.01 | 0.17 | 0.11 | 0.35 |
| Mood—FMPS_O | Mood | FMPS_O | <0.01 | 0.99 | <0.01 | <0.01 | −0.38 | −0.12 |
| Mood—FMPS_PEC | Mood | FMPS_PEC | 0.01 | 0.94 | <0.01 | 0.26 | 0.08 | 0.40 |
| Mood—FMPS_PS | Mood | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Mood—NSSI_intra | Mood | NSSI_intra | 0.08 | 0.76 | <0.01 | 0.51 | 0.16 | 0.65 |
| Mood—Psychotic | Mood | Psychotic | 0.33 | 0.75 | <0.01 | 1.71 | 0.22 | 11.56 |
| Mood—Substance | Mood | Substance | 0.01 | 0.98 | <0.01 | <0.01 | 0.19 | 1.57 |
| Mood—Suicid | Mood | Suicid | 0.52 | 0.15 | <0.01 | 1.14 | 0.25 | 1.16 |
| Mood—Tic | Mood | Tic | <0.01 | 0.99 | <0.01 | <0.01 | 0.34 | 0.93 |
| NSSI_intra—FMPS_CMD | NSSI_intra | FMPS_CMD | 0.01 | 0.95 | <0.01 | 0.20 | 0.11 | 0.66 |
| NSSI_intra—FMPS_O | NSSI_intra | FMPS_O | −0.01 | 0.94 | −0.25 | <0.01 | −0.47 | −0.11 |
| NSSI_intra—FMPS_PEC | NSSI_intra | FMPS_PEC | <0.01 | 0.99 | <0.01 | <0.01 | −0.36 | 0.19 |
| NSSI_intra—FMPS_PS | NSSI_intra | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Psychotic—ASD | Psychotic | ASD | −0.07 | 0.97 | <0.01 | <0.01 | −56.08 | 16.12 |
| Psychotic—BPD | Psychotic | BPD | 1.56 | 0.54 | <0.01 | 14.07 | 0.34 | 20.52 |
| Psychotic—FMPS_CMD | Psychotic | FMPS_CMD | 0.04 | 0.97 | <0.01 | 0.27 | 0.16 | 10.82 |
| Psychotic—FMPS_O | Psychotic | FMPS_O | −0.04 | 0.98 | <0.01 | <0.01 | −19.63 | −0.27 |
| Psychotic—FMPS_PEC | Psychotic | FMPS_PEC | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Psychotic—FMPS_PS | Psychotic | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Psychotic—NSSI_intra | Psychotic | NSSI_intra | <0.01 | 0.99 | <0.01 | <0.01 | −7.85 | 2.45 |
| Psychotic—Suicid | Psychotic | Suicid | 0.68 | 0.75 | <0.01 | 2.60 | 0.24 | 30.18 |
| Substance—Atten_disr | Substance | Atten_disr | 0.04 | 0.95 | <0.01 | 0.64 | −2.07 | 7.42 |
| Substance—ASD | Substance | ASD | −0.02 | 0.98 | <0.01 | <0.01 | −4.00 | −0.36 |
| Substance—BPD | Substance | BPD | 0.19 | 0.95 | <0.01 | 2.06 | 0.44 | 20.39 |
| Substance—ED | Substance | ED | 0.01 | 0.99 | <0.01 | <0.01 | 0.34 | 0.68 |
| Substance—FMPS_CMD | Substance | FMPS_CMD | <0.01 | 1.00 | <0.01 | <0.01 | 0.26 | 0.26 |
| Substance—FMPS_O | Substance | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Substance—FMPS_PEC | Substance | FMPS_PEC | 0.03 | 0.90 | <0.01 | 0.33 | 0.13 | 0.45 |
| Substance—FMPS_PS | Substance | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Substance—NSSI_intra | Substance | NSSI_intra | 0.01 | 0.98 | <0.01 | <0.01 | 0.19 | 0.68 |
| Substance—Psychotic | Substance | Psychotic | −0.04 | 1.00 | <0.01 | <0.01 | −32.19 | 0.72 |
| Substance—Suicid | Substance | Suicid | <0.01 | 1.00 | <0.01 | <0.01 | −0.44 | 0.79 |
| Substance—Tic | Substance | Tic | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Suicid—FMPS_CMD | Suicid | FMPS_CMD | 0.01 | 0.98 | <0.01 | <0.01 | 0.14 | 7.34 |
| Suicid—FMPS_O | Suicid | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | −0.35 | −0.35 |
| Suicid—FMPS_PEC | Suicid | FMPS_PEC | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Suicid—FMPS_PS | Suicid | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | −1.08 | −0.35 |
| Suicid—NSSI_intra | Suicid | NSSI_intra | 0.05 | 0.90 | <0.01 | 0.46 | 0.17 | 1.75 |
| Tic—ASD | Tic | ASD | 0.42 | 0.78 | <0.01 | 1.91 | 0.28 | 18.46 |
| Tic—BPD | Tic | BPD | 0.64 | 0.90 | <0.01 | 8.80 | 0.33 | 36.51 |
| Tic—ED | Tic | ED | 0.09 | 0.99 | <0.01 | <0.01 | −10.94 | 40.63 |
| Tic—FMPS_CMD | Tic | FMPS_CMD | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Tic—FMPS_O | Tic | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | −0.32 | −0.23 |
| Tic—FMPS_PEC | Tic | FMPS_PEC | −0.03 | 0.99 | <0.01 | <0.01 | −22.92 | −0.16 |
| Tic—FMPS_PS | Tic | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Tic—NSSI_intra | Tic | NSSI_intra | −0.03 | 1.00 | <0.01 | <0.01 | −27.90 | −0.52 |
| Tic—Psychotic | Tic | Psychotic | 1.00 | 0.68 | <0.01 | 8.01 | 0.37 | 38.19 |
| Tic—Suicid | Tic | Suicid | −0.16 | 0.98 | <0.01 | <0.01 | −44.99 | −0.37 |
| Variable | Variable 1 | Variable 2 | Value | prop0 | q2.5 | q97.5 | q2.5_non0 | q97.5_non0 |
|---|---|---|---|---|---|---|---|---|
| FMPS_CMD—FMPS_PS | FMPS_CMD | FMPS_PS | 0.49 | <0.01 | 0.38 | 0.59 | 0.38 | 0.59 |
| FMPS_PS—FMPS_O | FMPS_PS | FMPS_O | 0.35 | <0.01 | 0.19 | 0.48 | 0.19 | 0.48 |
| Anxiety—Suicid | Anxiety | Suicid | 1.41 | 0.04 | <0.01 | 5.60 | 0.35 | 5.89 |
| Anxiety—NSSI_inter | Anxiety | NSSI_inter | 0.91 | 0.13 | <0.01 | 2.16 | 0.27 | 3.09 |
| Mood—Suicid | Mood | Suicid | 0.57 | 0.13 | <0.01 | 1.17 | 0.26 | 1.21 |
| BPD—Suicid | BPD | Suicid | 5.07 | 0.15 | <0.01 | 40.04 | 0.39 | 43.35 |
| ASD—BPD | ASD | BPD | 4.14 | 0.35 | <0.01 | 30.40 | 0.39 | 34.97 |
| ED—NSSI_inter | ED | NSSI_inter | 0.71 | 0.37 | <0.01 | 3.08 | 0.24 | 7.61 |
| FMPS_CMD—FMPS_PEC | FMPS_CMD | FMPS_PEC | 0.14 | 0.39 | <0.01 | 0.34 | 0.15 | 0.37 |
| BPD—NSSI_inter | BPD | NSSI_inter | 2.45 | 0.53 | <0.01 | 19.85 | 0.29 | 26.04 |
| Psychotic—BPD | Psychotic | BPD | 1.55 | 0.54 | <0.01 | 13.82 | 0.39 | 24.97 |
| Atten_disr—BPD | Atten_disr | BPD | 1.67 | 0.56 | <0.01 | 16.00 | 0.44 | 27.76 |
| Anxiety—FMPS_CMD | Anxiety | FMPS_CMD | 0.26 | 0.56 | <0.01 | 0.70 | 0.14 | 2.31 |
| Anxiety—ASD | Anxiety | ASD | 0.35 | 0.57 | <0.01 | 1.34 | 0.22 | 2.67 |
| Tic—Psychotic | Tic | Psychotic | 0.84 | 0.65 | <0.01 | 5.69 | 0.39 | 19.02 |
| Mood—ED | Mood | ED | 0.29 | 0.66 | <0.01 | 0.85 | 0.20 | 4.02 |
| Anxiety—Psychotic | Anxiety | Psychotic | 0.81 | 0.69 | <0.01 | 7.45 | 0.26 | 26.60 |
| ED—FMPS_CMD | ED | FMPS_CMD | 0.37 | 0.72 | <0.01 | 2.63 | 0.14 | 14.57 |
| Anxiety—FMPS_PEC | Anxiety | FMPS_PEC | 0.11 | 0.73 | <0.01 | 0.49 | 0.14 | 0.77 |
| Mood—Psychotic | Mood | Psychotic | 0.35 | 0.73 | <0.01 | 1.46 | 0.23 | 10.44 |
| Psychotic—Suicid | Psychotic | Suicid | 0.46 | 0.74 | <0.01 | 2.31 | 0.28 | 14.26 |
| ED—Suicid | ED | Suicid | 0.22 | 0.76 | <0.01 | 1.00 | 0.20 | 5.52 |
| Tic—ASD | Tic | ASD | 0.54 | 0.77 | <0.01 | 2.88 | 0.30 | 20.34 |
| ED—BPD | ED | BPD | 0.97 | 0.77 | <0.01 | 10.60 | 0.27 | 34.20 |
| Anxiety—ED | Anxiety | ED | 0.38 | 0.79 | <0.01 | 1.90 | 0.17 | 20.95 |
| Mood—Anxiety | Mood | Anxiety | 0.16 | 0.79 | <0.01 | 0.62 | 0.17 | 2.91 |
| ASD—FMPS_CMD | ASD | FMPS_CMD | 0.06 | 0.80 | <0.01 | 0.40 | 0.12 | 0.54 |
| ASD—FMPS_O | ASD | FMPS_O | −0.05 | 0.82 | −0.34 | <0.01 | −0.46 | −0.13 |
| BPD—FMPS_CMD | BPD | FMPS_CMD | 0.19 | 0.85 | <0.01 | 1.97 | 0.18 | 8.92 |
| Atten_disr—Suicid | Atten_disr | Suicid | 0.29 | 0.85 | <0.01 | 2.57 | 0.30 | 15.59 |
| Substance—FMPS_PEC | Substance | FMPS_PEC | 0.03 | 0.88 | <0.01 | 0.36 | 0.13 | 0.55 |
| Mood—Atten_disr | Mood | Atten_disr | 0.11 | 0.89 | <0.01 | 0.80 | 0.26 | 6.01 |
| Anxiety—BPD | Anxiety | BPD | −1.22 | 0.89 | −15.38 | <0.01 | −59.78 | −0.44 |
| Tic—BPD | Tic | BPD | 0.66 | 0.90 | <0.01 | 7.87 | 0.47 | 32.39 |
| Anxiety—Atten_disr | Anxiety | Atten_disr | 0.15 | 0.92 | <0.01 | 1.10 | 0.25 | 19.11 |
| FMPS_PEC—FMPS_O | FMPS_PEC | FMPS_O | 0.01 | 0.92 | <0.01 | 0.15 | 0.07 | 0.22 |
| Atten_disr—ASD | Atten_disr | ASD | 0.26 | 0.93 | <0.01 | 1.47 | 0.23 | 21.32 |
| ED—ASD | ED | ASD | −0.33 | 0.94 | −1.78 | <0.01 | −34.11 | −0.32 |
| Mood—FMPS_PEC | Mood | FMPS_PEC | 0.01 | 0.94 | <0.01 | 0.24 | 0.10 | 0.51 |
| Substance—NSSI_inter | Substance | NSSI_inter | 0.02 | 0.95 | <0.01 | 0.40 | 0.16 | 0.87 |
| Atten_disr—FMPS_PEC | Atten_disr | FMPS_PEC | 0.03 | 0.95 | <0.01 | 0.37 | 0.15 | 4.44 |
| Substance—BPD | Substance | BPD | 0.13 | 0.95 | <0.01 | 1.09 | 0.35 | 16.46 |
| ED—FMPS_PEC | ED | FMPS_PEC | −0.01 | 0.95 | <0.01 | 0.29 | −25.61 | 6.27 |
| Anxiety—Substance | Anxiety | Substance | 0.05 | 0.96 | <0.01 | 0.47 | 0.29 | 13.36 |
| Suicid—NSSI_inter | Suicid | NSSI_inter | 0.01 | 0.96 | <0.01 | 0.25 | −1.93 | 3.74 |
| Substance—Atten_disr | Substance | Atten_disr | 0.04 | 0.96 | <0.01 | 0.62 | 0.30 | 9.28 |
| Mood—FMPS_CMD | Mood | FMPS_CMD | 0.01 | 0.96 | <0.01 | 0.18 | 0.09 | 0.34 |
| Mood—BPD | Mood | BPD | 0.07 | 0.96 | <0.01 | 0.38 | −2.85 | 24.49 |
| Substance—ASD | Substance | ASD | −0.03 | 0.97 | −0.55 | <0.01 | −5.83 | −0.32 |
| Psychotic—FMPS_CMD | Psychotic | FMPS_CMD | 0.01 | 0.97 | <0.01 | 0.20 | 0.15 | 1.47 |
| NSSI_inter—FMPS_CMD | NSSI_inter | FMPS_CMD | 0.01 | 0.97 | <0.01 | 0.12 | 0.12 | 0.35 |
| NSSI_inter—FMPS_PS | NSSI_inter | FMPS_PS | 0.01 | 0.98 | <0.01 | <0.01 | 0.10 | 0.50 |
| ASD—Suicid | ASD | Suicid | 0.01 | 0.98 | <0.01 | <0.01 | −2.33 | 2.12 |
| Atten_disr—ED | Atten_disr | ED | 0.05 | 0.98 | <0.01 | <0.01 | 0.27 | 18.67 |
| ED—Psychotic | ED | Psychotic | −0.11 | 0.98 | <0.01 | <0.01 | −46.25 | 10.41 |
| ASD—FMPS_PEC | ASD | FMPS_PEC | 0.01 | 0.98 | <0.01 | <0.01 | 0.09 | 0.42 |
| Suicid—FMPS_CMD | Suicid | FMPS_CMD | 0.01 | 0.98 | <0.01 | <0.01 | 0.11 | 3.42 |
| Tic—Suicid | Tic | Suicid | −0.30 | 0.98 | <0.01 | <0.01 | −120.68 | −0.42 |
| Mood—Substance | Mood | Substance | 0.01 | 0.98 | <0.01 | <0.01 | 0.25 | 0.85 |
| NSSI_inter—FMPS_O | NSSI_inter | FMPS_O | <0.01 | 0.98 | <0.01 | <0.01 | −0.50 | −0.14 |
| Mood—NSSI_inter | Mood | NSSI_inter | <0.01 | 0.98 | <0.01 | <0.01 | −1.00 | 0.57 |
| FMPS_PEC—FMPS_PS | FMPS_PEC | FMPS_PS | <0.01 | 0.98 | <0.01 | <0.01 | 0.09 | 0.25 |
| Tic—FMPS_PEC | Tic | FMPS_PEC | −0.02 | 0.98 | <0.01 | <0.01 | −6.02 | −0.16 |
| Psychotic—FMPS_O | Psychotic | FMPS_O | −0.01 | 0.98 | <0.01 | <0.01 | −0.95 | −0.25 |
| Atten_disr—Psychotic | Atten_disr | Psychotic | 0.03 | 0.98 | <0.01 | <0.01 | 0.25 | 10.27 |
| Psychotic—ASD | Psychotic | ASD | 0.18 | 0.98 | <0.01 | <0.01 | −1.98 | 85.01 |
| Mood—ASD | Mood | ASD | −0.01 | 0.99 | <0.01 | <0.01 | −1.45 | 0.45 |
| Psychotic—NSSI_inter | Psychotic | NSSI_inter | <0.01 | 0.99 | <0.01 | <0.01 | −15.19 | 23.88 |
| ASD—NSSI_inter | ASD | NSSI_inter | <0.01 | 0.99 | <0.01 | <0.01 | −0.44 | 0.63 |
| Mood—FMPS_O | Mood | FMPS_O | <0.01 | 0.99 | <0.01 | <0.01 | −0.29 | −0.18 |
| BPD—FMPS_PEC | BPD | FMPS_PEC | −0.01 | 0.99 | <0.01 | <0.01 | −2.47 | −0.30 |
| Tic—ED | Tic | ED | 0.01 | 0.99 | <0.01 | <0.01 | −13.67 | 15.92 |
| Substance—ED | Substance | ED | <0.01 | 0.99 | <0.01 | <0.01 | 0.13 | 0.71 |
| Mood—Tic | Mood | Tic | <0.01 | 0.99 | <0.01 | <0.01 | 0.32 | 0.63 |
| Tic—NSSI_inter | Tic | NSSI_inter | 0.01 | 0.99 | <0.01 | <0.01 | −0.31 | 3.66 |
| Atten_disr—Tic | Atten_disr | Tic | 0.09 | 0.99 | <0.01 | <0.01 | −7.95 | 62.98 |
| Anxiety—Tic | Anxiety | Tic | −0.03 | 1.00 | <0.01 | <0.01 | −19.25 | 1.54 |
| Substance—Suicid | Substance | Suicid | <0.01 | 1.00 | <0.01 | <0.01 | −0.66 | 0.51 |
| Substance—Psychotic | Substance | Psychotic | <0.01 | 1.00 | <0.01 | <0.01 | −6.27 | 4.68 |
| Suicid—FMPS_PS | Suicid | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | −0.70 | −0.34 |
| ASD—FMPS_PS | ASD | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | −0.86 | −0.28 |
| Suicid—FMPS_PEC | Suicid | FMPS_PEC | <0.01 | 1.00 | <0.01 | <0.01 | −0.81 | 0.22 |
| Atten_disr—NSSI_inter | Atten_disr | NSSI_inter | −0.04 | 1.00 | <0.01 | <0.01 | −43.39 | −1.54 |
| BPD—FMPS_O | BPD | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | −3.28 | −1.06 |
| NSSI_inter—FMPS_PEC | NSSI_inter | FMPS_PEC | <0.01 | 1.00 | <0.01 | <0.01 | −0.28 | −0.18 |
| Tic—FMPS_O | Tic | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | −0.25 | −0.21 |
| Substance—FMPS_CMD | Substance | FMPS_CMD | <0.01 | 1.00 | <0.01 | <0.01 | −0.24 | 0.23 |
| Psychotic—FMPS_PEC | Psychotic | FMPS_PEC | <0.01 | 1.00 | <0.01 | <0.01 | 0.17 | 0.75 |
| Tic—FMPS_PS | Tic | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | −3.02 | −3.02 |
| Anxiety—FMPS_PS | Anxiety | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | −1.00 | −1.00 |
| Suicid—FMPS_O | Suicid | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | −0.24 | −0.24 |
| FMPS_CMD—FMPS_O | FMPS_CMD | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | −0.16 | −0.16 |
| Substance—FMPS_PS | Substance | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | 0.12 | 0.12 |
| Atten_disr—FMPS_CMD | Atten_disr | FMPS_CMD | <0.01 | 1.00 | <0.01 | <0.01 | 0.20 | 0.20 |
| Tic—FMPS_CMD | Tic | FMPS_CMD | 0.01 | 1.00 | <0.01 | <0.01 | 7.19 | 7.19 |
| Anxiety—FMPS_O | Anxiety | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Atten_disr—FMPS_O | Atten_disr | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Atten_disr—FMPS_PS | Atten_disr | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| BPD—FMPS_PS | BPD | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| ED—FMPS_O | ED | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| ED—FMPS_PS | ED | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Mood—FMPS_PS | Mood | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Psychotic—FMPS_PS | Psychotic | FMPS_PS | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Substance—FMPS_O | Substance | FMPS_O | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Substance—Tic | Substance | Tic | <0.01 | 1.00 | <0.01 | <0.01 | <0.01 | <0.01 |
| Outcome Variables | NSSI Intrapersonal Motivation | NSSI Interpersonal Motivation | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| (n = 134) | (n = 134) | |||||||||
| Estimate | SE | t | df | Pr (>|t|) | Estimate | SE | t | df | Pr (>|t|) | |
| FMPS–CMD | 0.04 | 0.02 | 2.00 | 128 | 0.05 * | 0.04 | 0.02 | 1.88 | 128 | 0.06 |
| FMPS–PEC | 0.01 | 0.03 | 0.24 | 128 | 0.81 | 0.00 | 0.03 | 0.02 | 128 | 0.99 |
| FMPS–PS | 0.00 | 0.04 | 0.01 | 128 | 0.99 | 0.01 | 0.04 | 0.22 | 128 | 0.82 |
| FMPS–O | −0.06 | 0.04 | −1.40 | 128 | 0.16 | −0.12 | 0.04 | −2.74 | 128 | 0.01 * |
| Intercept | 1.43 | 0.96 | 1.49 | 128 | 0.14 | 2.08 | 0.89 | 2.33 | 128 | 0.02 * |
| Outcome Variable | NSSI Intrapersonal Motivation | NSSI Interpersonal Motivation | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| (n = 134) | (n = 134) | |||||||||
| Estimate | SE | t | df | Pr (>|t|) | Estimate | SE | t | df | Pr (>|t|) | |
| Intercept | 2.66 | 0.85 | 3.12 | 118 | <0.01 ** | 2.34 | 0.82 | 2.84 | 118 | <0.01 ** |
| Mood | 0.59 | 0.40 | 1.47 | 118 | 0.14 | 0.06 | 0.41 | 0.14 | 118 | 0.89 |
| Anxiety disorder | 1.29 | 0.44 | 2.97 | 118 | <0.01 ** | 1.21 | 0.43 | 2.81 | 118 | <0.01 ** |
| Substance use disorder | 0.29 | 0.42 | 0.69 | 118 | 0.49 | 0.45 | 0.42 | 1.09 | 118 | 0.28 |
| Attention-disruptive disorders | −0.48 | 0.66 | −0.73 | 118 | 0.47 | −0.10 | 0.64 | −0.16 | 118 | 0.88 |
| Tic | −0.36 | 0.57 | −0.63 | 118 | 0.53 | 0.47 | 0.54 | 0.87 | 118 | 0.38 |
| Eating disorders | 0.89 | 0.47 | 1.89 | 118 | 0.06 | 0.81 | 0.47 | 1.74 | 118 | 0.08 |
| Psychotic disorders | −0.28 | 0.63 | −0.45 | 118 | 0.65 | −0.54 | 0.61 | −0.88 | 118 | 0.38 |
| Autism spectrum disorders | −0.11 | 0.36 | −0.29 | 118 | 0.77 | 0.01 | 0.36 | 0.03 | 118 | 0.98 |
| Borderline personality disorders | 1.05 | 0.60 | 1.76 | 118 | 0.08 | 1.11 | 0.59 | 1.88 | 118 | 0.06 |
| Suicidality | −0.04 | 0.44 | −0.09 | 118 | 0.93 | −0.27 | 0.44 | −0.61 | 118 | 0.54 |
| FMPS–CMD | 0.01 | 0.02 | 0.51 | 118 | 0.61 | 0.00 | 0.02 | 0.19 | 118 | 0.85 |
| FMPS–PEC | −0.04 | 0.02 | −1.50 | 118 | 0.13 | −0.01 | 0.02 | −0.28 | 118 | 0.78 |
| FMPS–PS | 0.01 | 0.04 | 0.17 | 118 | 0.87 | 0.03 | 0.04 | 0.84 | 118 | 0.4 |
| FMPS–O | −0.09 | 0.04 | −2.23 | 118 | 0.03 * | −0.13 | 0.04 | −3.35 | 118 | <0.01 ** |
References
- American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-5); American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Klonsky, E.D. The Functions of Deliberate Self-Injury: A Review of the Evidence. Clin. Psychol. Rev. 2007, 27, 226–239. [Google Scholar] [CrossRef] [PubMed]
- Nock, M.K. Self-Injury. Annu. Rev. Clin. Psychol. 2010, 6, 339–363. [Google Scholar] [CrossRef]
- Xiao, Q.; Song, X.; Huang, L.; Hou, D.; Huang, X. Global Prevalence and Characteristics of Non-Suicidal Self-Injury between 2010 and 2021 among a Non-Clinical Sample of Adolescents: A Meta-Analysis. Front. Psychiatry 2022, 13, 912441. [Google Scholar] [CrossRef] [PubMed]
- Duarte, E.; Silva, S.; Gouveia-Pereira, M. Non-Suicidal Self-Injury, Suicidal Ideation and Suicide Attempts. Eur. J. Ment. Health 2023, 18, 1–11. [Google Scholar] [CrossRef]
- Horváth, L.O.; Győri, D.; Komáromy, D.; Mészáros, G.; Szentiványi, D.; Balázs, J. Nonsuicidal Self-Injury and Suicide: The Role of Life Events in Clinical and Non-Clinical Populations of Adolescents. Front. Psychiatry 2020, 11, 370. [Google Scholar] [CrossRef] [PubMed]
- Brunner, R.; Kaess, M.; Parzer, P.; Fischer, G.; Carli, V.; Hoven, C.W.; Wasserman, C.; Sarchiapone, M.; Resch, F.; Apter, A.; et al. Life-Time Prevalence and Psychosocial Correlates of Adolescent Direct Self-Injurious Behavior: A Comparative Study of Findings in 11 European Countries. J. Child Psychol. Psychiatry 2014, 55, 337–348. [Google Scholar] [CrossRef]
- Gu, H.; Hu, C.; Wang, L. Maladaptive Perfectionism and Adolescent NSSI: A Moderated Mediation Model of Psychological Distress and Mindfulness. J. Clin. Psychol. 2022, 78, 1137–1150. [Google Scholar] [CrossRef]
- Lloyd-Richardson, E.; Perrine, N.; Dierker, L.; Kelley, M.L. Characteristics and Functions of Non-Suicidal Self-Injury in a Community Sample of Adolescents. Psychol. Med. 2007, 37, 1183–1192. [Google Scholar] [CrossRef]
- Swannell, S.V.; Martin, G.E.; Page, A.; Hasking, P.; St John, N.J. Prevalence of Nonsuicidal Self-Injury in Nonclinical Samples: Systematic Review, Meta-Analysis and Meta-Regression. Suicide Life Threat. Behav. 2014, 44, 273–303. [Google Scholar] [CrossRef]
- Zetterqvist, M.; Lundh, L.-G.; Dahlström, Ö.; Svedin, C.G. Prevalence and Function of Non-Suicidal Self-Injury (NSSI) in a Community Sample of Adolescents, Using Suggested DSM-5 Criteria for a Potential NSSI Disorder. J. Abnorm. Child Psychol. 2013, 41, 759–773. [Google Scholar] [CrossRef]
- Gyori, D.; Farkas, B.F.; Horvath, L.O.; Komaromy, D.; Meszaros, G.; Szentivanyi, D.; Balazs, J. The Association of Nonsuicidal Self-Injury with Quality of Life and Mental Disorders in Clinical Adolescents-A Network Approach. Int. J. Environ. Res. Public Health 2021, 18, 1840. [Google Scholar] [CrossRef] [PubMed]
- Kaess, M.; Parzer, P.; Mattern, M.; Plener, P.L.; Bifulco, A.; Resch, F.; Brunner, R. Adverse Childhood Experiences and Their Impact on Frequency, Severity, and the Individual Function of Nonsuicidal Self-Injury in Youth. Psychiatry Res. 2013, 206, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Nock, M.K.; Prinstein, M.J. A Functional Approach to the Assessment of Self-Mutilative Behavior. J. Consult. Clin. Psychol. 2004, 72, 885–890. [Google Scholar] [CrossRef]
- Wester, K.; Trepal, H.; King, K. Nonsuicidal Self-Injury: Increased Prevalence in Engagement. Suicide Life Threat. Behav. 2018, 48, 690–698. [Google Scholar] [CrossRef]
- Gratz, K.L. Measurement of Deliberate Self-Harm: Preliminary Data on the Deliberate Self-Harm Inventory. J. Psychopathol. Behav. Assess. 2001, 23, 253–263. [Google Scholar] [CrossRef]
- Klonsky, E.D.; Glenn, C.R. Assessing the Functions of Non-Suicidal Self-Injury: Psychometric Properties of the Inventory of Statements About Self-Injury (ISAS). J. Psychopathol. Behav. Assess. 2009, 31, 215–219. [Google Scholar] [CrossRef] [PubMed]
- Klonsky, E.D.; Muehlenkamp, J.J. Self-Injury: A Research Review for the Practitioner. J. Clin. Psychol. 2007, 63, 1045–1056. [Google Scholar] [CrossRef]
- Taylor, P.J.; Jomar, K.; Dhingra, K.; Forrester, R.; Shahmalak, U.; Dickson, J.M. A Meta-Analysis of the Prevalence of Different Functions of Non-Suicidal Self-Injury. J. Affect. Disord. 2018, 227, 759–769. [Google Scholar] [CrossRef]
- Klonsky, E.D.; Glenn, C.R.; Styer, D.M.; Olino, T.M.; Washburn, J.J. The Functions of Nonsuicidal Self-Injury: Converging Evidence for a Two-Factor Structure. Child Adolesc. Psychiatry Ment. Health 2015, 9, 44. [Google Scholar] [CrossRef]
- Reinhardt, M.; Kökönyei, G.; Rice, K.G.; Drubina, B.; Urbán, R. Functions of Nonsuicidal Self-Injury in a Hungarian Community Adolescent Sample: A Psychometric Investigation. BMC Psychiatry 2021, 21, 618. [Google Scholar] [CrossRef]
- Gyori, D.; Balazs, J. Nonsuicidal Self-Injury and Perfectionism: A Systematic Review. Front. Psychiatry 2021, 12, 1076. [Google Scholar] [CrossRef] [PubMed]
- Frost, R.O.; Marten, P.; Lahart, C.; Rosenblate, R. The Dimensions of Perfectionism. Cogn. Ther. Res. 1990, 14, 449–468. [Google Scholar] [CrossRef]
- Hewitt, P.L.; Flett, G.L. Perfectionism in the Self and Social Contexts: Conceptualization, Assessment, and Association with Psychopathology. Pers. Soc. Psychol. 1991, 60, 456–470. [Google Scholar] [CrossRef]
- Bieling, P.J.; Israeli, A.L.; Antony, M.M. Is Perfectionism Good, Bad, or Both? Examining Models of the Perfectionism Construct. Pers. Individ. Differ. 2004, 36, 1373–1385. [Google Scholar] [CrossRef]
- Dunkley, D.M.; Blankstein, K.R.; Masheb, R.M.; Grilo, C.M. Personal Standards and Evaluative Concerns Dimensions of “Clinical” Perfectionism: A Reply to Shafran et al. (2002, 2003) and Hewitt et al. (2003). Behav. Res. Ther. 2006, 44, 63–84. [Google Scholar] [CrossRef] [PubMed]
- Frost, R.O.; Heimberg, R.G.; Holt, C.S.; Mattia, J.I.; Neubauer, A.L. A Comparison of Two Measures of Perfectionism. Pers. Individ. Differ. 1993, 14, 119–126. [Google Scholar] [CrossRef]
- Stoeber, J.; Otto, K. Positive Conceptions of Perfectionism: Approaches, Evidence, Challenges. Pers. Soc. Psychol. Rev. 2006, 10, 295–319. [Google Scholar] [CrossRef]
- Hawkins, C.C.; Watt, H.M.G.; Sinclair, K.E. Psychometric Properties of the Frost Multidimensional Perfectionism Scale with Australian Adolescent Girls: Clarification of Multidimensionality and Perfectionist Typology. Educ. Psychol. Meas. 2006, 66, 1001–1022. [Google Scholar] [CrossRef]
- Rice, K.G.; Ashby, J.S.; Gilman, R. Classifying Adolescent Perfectionists. Psychol. Assess. 2011, 23, 563–577. [Google Scholar] [CrossRef]
- Sironic, A.; Reeve, R.A. A Combined Analysis of the Frost Multidimensional Perfectionism Scale (FMPS), Child and Adolescent Perfectionism Scale (CAPS), and Almost Perfect Scale-Revised (APS-R): Different Perfectionist Profiles in Adolescent High School Students. Psychol. Assess. 2015, 27, 1471–1483. [Google Scholar] [CrossRef]
- Stornæs, A.V.; Rosenvinge, J.H.; Sundgot-Borgen, J.; Pettersen, G.; Friborg, O. Profiles of Perfectionism Among Adolescents Attending Specialized Elite- and Ordinary Lower Secondary Schools: A Norwegian Cross-Sectional Comparative Study. Front. Psychol. 2019, 10, 2039. [Google Scholar] [CrossRef] [PubMed]
- Curran, T.; Hill, A.P. Perfectionism Is Increasing over Time: A Meta-Analysis of Birth Cohort Differences from 1989 to 2016. Psychol. Bull. 2019, 145, 410–429. [Google Scholar] [CrossRef] [PubMed]
- Portešová, Š.; Urbánek, T. Typology of Perfectionism in a Group of Mathematically Gifted Czech Adolescents over One Decade. J. Early Adolesc. 2013, 33, 1116–1144. [Google Scholar] [CrossRef]
- Nock, M.K.; Prinstein, M.J. Contextual Features and Behavioral Functions of Self-Mutilation Among Adolescents. J. Abnorm. Psychol. 2005, 114, 140–146. [Google Scholar] [CrossRef]
- Claes, L.; Soenens, B.; Vansteenkiste, M.; Vandereycken, W. The Scars of the Inner Critic: Perfectionism and Nonsuicidal Self-Injury in Eating Disorders. Eur. Eat. Disord. Rev. 2012, 20, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Reinhardt, M.; Rice, K.G.; Durán, B.S.; Kökönyei, G. A Person-Centered Approach to Adolescent Nonsuicidal Self-Injury: Predictors and Correlates in a Community Sample. J. Youth Adolesc. 2022, 51, 1760–1773. [Google Scholar] [CrossRef]
- Luyckx, K.; Gandhi, A.; Bijttebier, P.; Claes, L. Non-Suicidal Self-Injury in Female Adolescents and Psychiatric Patients: A Replication and Extension of the Role of Identity Formation. Pers. Individ. Differ. 2015, 77, 91–96. [Google Scholar] [CrossRef]
- Tonta, K.E.; Boyes, M.; Howell, J.; McEvoy, P.; Johnson, A.; Hasking, P. Modeling Pathways to Non-Suicidal Self-Injury: The Roles of Perfectionism, Negative Affect, Rumination, and Attention Control. J. Clin. Psychol. 2022, 78, 1463–1477. [Google Scholar] [CrossRef]
- Boone, L.; Soenens, B.; Braet, C.; Goossens, L. An Empirical Typology of Perfectionism in Early-to-Mid Adolescents and Its Relation with Eating Disorder Symptoms. Behav. Res. Ther. 2010, 48, 686–691. [Google Scholar] [CrossRef]
- Dickie, L.; Wilson, M.; McDowall, J.; Surgenor, L.J. What Components of Perfectionism Predict Drive for Thinness? Eat. Disord. 2012, 20, 232–247. [Google Scholar] [CrossRef]
- Flett, G.L.; Coulter, L.-M.; Hewitt, P.L.; Nepon, T. Perfectionism, Rumination, Worry, and Depressive Symptoms in Early Adolescents. Can. J. Sch. Psychol. 2011, 26, 159–176. [Google Scholar] [CrossRef]
- Hewitt, P.L.; Caelian, C.F.; Flett, G.L.; Sherry, S.B.; Collins, L.; Flynn, C.A. Perfectionism in Children: Associations with Depression, Anxiety, and Anger. Pers. Individ. Dif. 2002, 32, 1049–1061. [Google Scholar] [CrossRef]
- Limburg, K.; Watson, H.J.; Hagger, M.S.; Egan, S.J. The Relationship between Perfectionism and Psychopathology: A Meta-Analysis. J. Clin. Psychol. 2017, 73, 1301–1326. [Google Scholar] [CrossRef] [PubMed]
- Magson, N.R.; Oar, E.L.; Fardouly, J.; Johnco, C.J.; Rapee, R.M. The Preteen Perfectionist: An Evaluation of the Perfectionism Social Disconnection Model. Child Psychiatry Hum. Dev. 2019, 50, 960–974. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, R.C.; Rasmussen, S.; Hawton, K. Predicting Depression, Anxiety and Self-Harm in Adolescents: The Role of Perfectionism and Acute Life Stress. Behav. Res. Ther. 2010, 48, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Soreni, N.; Streiner, D.; McCabe, R.; Bullard, C.; Swinson, R.; Greco, A.; Pires, P.; Szatmari, P. Dimensions of Perfectionism in Children and Adolescents with Obsessive-Compulsive Disorder. J. Can. Acad. Child Adolesc. Psychiatry 2014, 23, 136–143. [Google Scholar]
- Taylor, E.P.; Couper, R.; Butler, C.M. Adolescent Perfectionism: Structural Features of the Frost Multidimensional Perfectionism Scale and Correlates with Attachment and Psychopathology. Psychol. Psychother. 2017, 90, 686–704. [Google Scholar] [CrossRef]
- Cipriano, A.; Cella, S.; Cotrufo, P. Nonsuicidal Self-Injury: A Systematic Review. Front. Psychol. 2017, 8, 1946. [Google Scholar] [CrossRef]
- In-Albon, T.; Ruf, C.; Schmid, M. Proposed Diagnostic Criteria for the DSM-5 of Nonsuicidal Self-Injury in Female Adolescents: Diagnostic and Clinical Correlates. Available online: https://www.hindawi.com/journals/psychiatry/2013/159208/ (accessed on 1 January 2021).
- Nock, M.; Joiner, T., Jr.; Gordon, K.; Lloyd-Richardson, E.; Prinstein, M. Non-Suicidal Self-Injury among Adolescents: Diagnostic Correlates and Relation to Suicide Attempts. Psychiatry Res. 2006, 144, 65–72. [Google Scholar] [CrossRef]
- Hewitt, P.L.; Caelian, C.F.; Chen, C.; Flett, G.L. Perfectionism, Stress, Daily Hassles, Hopelessness, and Suicide Potential in Depressed Psychiatric Adolescents. J. Psychopathol. Behav. Assess. 2014, 36, 663–674. [Google Scholar] [CrossRef]
- Klonsky, E.D.; May, A.M.; Glenn, C.R. The Relationship between Nonsuicidal Self-Injury and Attempted Suicide: Converging Evidence from Four Samples. J. Abnorm. Psychol. 2013, 122, 231–237. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, R.C. The Relations between Perfectionism and Suicidality: A Systematic Review. Suicide Life Threat. Behav. 2007, 37, 698–714. [Google Scholar] [CrossRef] [PubMed]
- Victor, S.E.; Klonsky, E.D. Correlates of Suicide Attempts among Self-Injurers: A Meta-Analysis. Clin. Psychol. Rev. 2014, 34, 282–297. [Google Scholar] [CrossRef]
- James, K.; Verplanken, B.; Rimes, K.A. Self-Criticism as a Mediator in the Relationship between Unhealthy Perfectionism and Distress. Personal. Individ. Differ. 2015, 79, 123–128. [Google Scholar] [CrossRef]
- Nagy, L.M.; Shanahan, M.L.; Baer, R.A. An Experimental Investigation of the Effects of Self-Criticism and Self-Compassion on Implicit Associations with Non-Suicidal Self-Injury. Behav. Res. Ther. 2021, 139, 103819. [Google Scholar] [CrossRef] [PubMed]
- Xavier, A.; Pinto Gouveia, J.; Cunha, M. Non-Suicidal Self-Injury in Adolescence: The Role of Shame, Self-Criticism and Fear of Self-Compassion. Child Youth Care Forum 2016, 45, 571–586. [Google Scholar] [CrossRef]
- Vois, D.; Damian, L.E. Perfectionism and Emotion Regulation in Adolescents: A Two-Wave Longitudinal Study. Pers. Individ. Differ. 2020, 156, 109756. [Google Scholar] [CrossRef]
- Wolff, J.C.; Thompson, E.; Thomas, S.A.; Nesi, J.; Bettis, A.H.; Ransford, B.; Scopelliti, K.; Frazier, E.A.; Liu, R.T. Emotion Dysregulation and Non-Suicidal Self-Injury: A Systematic Review and Meta-Analysis. Eur. Psychiatry 2019, 59, 25–36. [Google Scholar] [CrossRef]
- Fedewa, B.A.; Burns, L.R.; Gomez, A.A. Positive and Negative Perfectionism and the Shame/Guilt Distinction: Adaptive and Maladaptive Characteristics. Pers. Individ. Differ. 2005, 38, 1609–1619. [Google Scholar] [CrossRef]
- Stoeber, J.; Schneider, N.; Hussain, R.; Matthews, K. Perfectionism and Negative Affect after Repeated Failure: Anxiety, Depression, and Anger. J. Individ. Differ. 2014, 35, 87–94. [Google Scholar] [CrossRef]
- Stoeber, J.; Kempe, T.; Keogh, E.J. Facets of Self-Oriented and Socially Prescribed Perfectionism and Feelings of Pride, Shame, and Guilt Following Success and Failure. Pers. Individ. Differ. 2008, 44, 1506–1516. [Google Scholar] [CrossRef]
- Chester, D.S.; Merwin, L.M.; DeWall, C.N. Maladaptive Perfectionism’s Link to Aggression and Self-Harm: Emotion Regulation as a Mechanism. Aggress. Behav. 2015, 41, 443–454. [Google Scholar] [CrossRef] [PubMed]
- Mahtani, S.; Melvin, G.A.; Hasking, P. Shame Proneness, Shame Coping, and Functions of Nonsuicidal Self-Injury (NSSI) Among Emerging Adults: A Developmental Analysis. Emerg. Adulthood. 2017, 6, 159–171. [Google Scholar] [CrossRef]
- Schoenleber, M.; Berenbaum, H.; Motl, R. Shame-Related Functions of and Motivations for Self-Injurious Behavior. Personal. Disord. 2014, 5, 204–211. [Google Scholar] [CrossRef] [PubMed]
- Kiekens, G.; Hasking, P.; Boyes, M.; Claes, L.; Mortier, P.; Auerbach, R.P.; Cuijpers, P.; Demyttenaere, K.; Green, J.G.; Kessler, R.C.; et al. The Associations between Non-Suicidal Self-Injury and First Onset Suicidal Thoughts and Behaviors. J. Affect. Disord. 2018, 239, 171–179. [Google Scholar] [CrossRef]
- Brown, R.C.; Plener, P.L. Non-Suicidal Self-Injury in Adolescence. Curr. Psychiatry Rep. 2017, 19, 20. [Google Scholar] [CrossRef]
- Kaess, M.; Koenig, J.; Bauer, S.; Moessner, M.; Fischer-Waldschmidt, G.; Mattern, M.; Herpertz, S.C.; Resch, F.; Brown, R.; In-Albon, T.; et al. Self-Injury: Treatment, Assessment, Recovery (STAR): Online Intervention for Adolescent Non-Suicidal Self-Injury—Study Protocol for a Randomized Controlled Trial. Trials 2019, 20, 425. [Google Scholar] [CrossRef]
- Balazs, J.; Horvath, L.O.; Meszaros, P.; Perczely, D. Az Élet Iskolája. In Egy Új Iskolai Mentális Egészségfejlesztő Program Bemutatása—A Magyar Pszichiátriai Társaság XXIII; Vándorgyűlése: Budapest, Hungary, 2020. [Google Scholar]
- Amorim, P.; Lecrubier, Y.; Weiller, E.; Hergueta, T.; Sheehan, D. DSM-IH-R Psychotic Disorders: Procedural Validity of the Mini International Neuropsychiatric Interview (MINI). Concordance and Causes for Discordance with the CIDI. Eur. Psychiatry 1998, 13, 26–34. [Google Scholar] [CrossRef]
- Balazs, J.; Biro, A.; Dalnoki, D.; Lefkovics, E.; Tamas, Z.; Nagy, P.; Gadoros, J.A.; Gyermek, M.I.N.I. Kérdőív Magyar Nyelvű Változatának Ismertetése [Introduction of the Hungarian Version of the M.I.N.I. Kid]. Psychiatr. Hung. 2004, 19, 358–364. [Google Scholar]
- Lecrubier, Y.; Sheehan, D.; Weiller, E.; Amorim, P.; Bonora, I.; Harnett Sheehan, K.; Janavs, J.; Dunbar, G. The Mini International Neuropsychiatric Interview (MINI). A Short Diagnostic Structured Interview: Reliability and Validity According to the CIDI. Eur. Psychiatry 1997, 12, 224–231. [Google Scholar] [CrossRef]
- Sheehan, D.; Lecrubier, Y.; Harnett Sheehan, K.; Janavs, J.; Weiller, E.; Keskiner, A.; Schinka, J.; Knapp, E.; Sheehan, M.; Dunbar, G. The Validity of the Mini International Neuropsychiatric Interview (MINI) According to the SCID-P and Its Reliability. Eur. Psychiatry 1997, 12, 232–241. [Google Scholar] [CrossRef]
- Sheehan, D.V.; Sheehan, K.H.; Shytle, R.D.; Janavs, J.; Bannon, Y.; Rogers, J.E.; Milo, K.M.; Stock, S.L.; Wilkinson, B. Reliability and Validity of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID). J. Clin. Psychiatry 2010, 71, 313–326. [Google Scholar] [CrossRef] [PubMed]
- Sheehan, D.V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Baker, R.; Dunbar, G.C. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The Development and Validation of a Structured Diagnostic Psychiatric Interview for DSM-IV and ICD-10. J. Clin. Psychiatry 1998, 59, 22–33. [Google Scholar] [PubMed]
- Kuder, G.F.; Richardson, M.W. The theory of the estimation of test reliability. Psychometrika 1937, 2, 151–160. [Google Scholar] [CrossRef]
- Reinhardt, M.; Kökönyei, G.; Drubina, B.; Urbán, R. A nem szuicidális önsértés és motivációjának mérése serdülőknél: Az Állítások az Önsértés Kapcsán Kérdőív (ISAS-HU) magyar adaptációja. Magy. Pszichol. Szmle. 2021, 76, 515–548. [Google Scholar] [CrossRef]
- Pérez, S.; García-Alandete, J.; Cañabate, M.; Marco, J.H. Confirmatory Factor Analysis of the Inventory of Statements About Self-Injury in a Spanish Clinical Sample. J. Clin. Psychol. 2020, 76, 102–117. [Google Scholar] [CrossRef]
- Piotrowski, K.; Bojanowska, A. Factor Structure and Psychometric Properties of a Polish Adaptation of the Frost Multidimensional Perfectionism Scale. Curr. Psychol. 2019, 40, 2754–2763. [Google Scholar] [CrossRef]
- Pearson, C.A.; Gleaves, D.H. The Multiple Dimensions of Perfectionism and Their Relation with Eating Disorder Features. Pers. Individ. Differ. 2006, 41, 225–235. [Google Scholar] [CrossRef]
- Rice, K.G.; Lapsley, D. Perfectionism, Coping, and Emotional Adjustment. J. Coll. Stud. Dev. 2001, 42, 157–168. [Google Scholar]
- Burgess, A.M.; Frost, R.O.; DiBartolo, P.M. Development and Validation of the Frost Multidimensional Perfectionism Scale–Brief. J. of Psychoeduc. Assess. 2016, 34, 620–633. [Google Scholar] [CrossRef]
- Khawaja, N.G.; Armstrong, K.A. Factor Structure and Psychometric Properties of the Frost Multidimensional Perfectionism Scale: Developing Shorter Versions Using an Australian Sample. Aust. J. Psychol. 2005, 57, 129–138. [Google Scholar] [CrossRef][Green Version]
- Stoeber, J.; Hotham, S. Perfectionism and Attitudes toward Cognitive Enhancers (“Smart Drugs”). Pers. Individ. Differ. 2016, 88, 170–174. [Google Scholar] [CrossRef]
- Stumpf, H.; Parker, W.D. A Hierarchical Structural Analysis of Perfectionism and Its Relation to Other Personality Characteristics. Pers. Individ. Differ. 2000, 28, 837–852. [Google Scholar] [CrossRef]
- Baron, R.M.; Kenny, D.A. The Moderator–Mediator Variable Distinction in Social Psychological Research: Conceptual, Strategic, and Statistical Considerations. J. Pers. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef] [PubMed]
- Epskamp, S.; Borsboom, D.; Fried, E.I. Estimating psychological networks and their accuracy: A tutorial paper. Behav. Res. 2017, 50, 195–212. [Google Scholar] [CrossRef]
- De Nooy, W.; Mrvar, A.; Batagelj, V. Exploratory Social Network Analysis with Pajek, 2nd ed.; Cambridge University Press: Cambridge, UK, 2011; p. 7. [Google Scholar]
- Mannekote Thippaiah, S.; Shankarapura Nanjappa, M.; Gude, J.G.; Voyiaziakis, E.; Patwa, S.; Birur, B.; Pandurangi, A. Non-Suicidal Self-Injury in Developing Countries: A Review. Int. J. Soc. Psychiatry 2021, 67, 472–482. [Google Scholar] [CrossRef]
- Brown, R.C.; Fischer, T.; Goldwich, A.D.; Keller, F.; Young, R.; Plener, P.L. #cutting: Non-Suicidal Self-Injury (NSSI) on Instagram. Psychol. Med. 2018, 48, 337–346. [Google Scholar] [CrossRef]
- Nesi, J.; Burke, T.A.; Lawrence, H.R.; MacPherson, H.A.; Spirito, A.; Wolff, J.C. Online Self-Injury Activities among Psychiatrically Hospitalized Adolescents: Prevalence, Functions, and Perceived Consequences. Res. Child Adolesc. Psychopathol. 2021, 49, 519–531. [Google Scholar] [CrossRef]
- Memon, A.M.; Sharma, S.G.; Mohite, S.S.; Jain, S. The Role of Online Social Networking on Deliberate Self-Harm and Suicidality in Adolescents: A Systematized Review of Literature. Indian J. Psychiatry 2018, 60, 384–392. [Google Scholar] [CrossRef]
- Breen, A.V.; Lewis, S.P.; Sutherland, O. Brief Report: Non-Suicidal Self-Injury in the Context of Self and Identity Development. J. Adult Dev. 2013, 20, 57–62. [Google Scholar] [CrossRef]
- Marchant, A.; Hawton, K.; Stewart, A.; Montgomery, P.; Singaravelu, V.; Lloyd, K.; Purdy, N.; Daine, K.; John, A. A systematic review of the relationship between internet use, self-harm and suicide behaviour in young people: The good, the bad and the unknow. PLoS ONE 2017, 12, e0181722. [Google Scholar] [CrossRef]
- Brown, R.C.; Fischer, T.; Goldwich, D.A.; Plener, P.L. “I just finally wanted to belong somewhere”—Qualitative Analysis of Experiences with Posting Pictures of Self-Injury on Instagram. Front. Psychiatry 2020, 11, 274. [Google Scholar] [CrossRef] [PubMed]
- Bresin, K.; Schoenleber, M. Gender Differences in the Prevalence of Nonsuicidal Self-Injury: A Meta-Analysis. Clin. Psychol. Rev. 2015, 38, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Xiao, Y.; Ran, H.; He, X.; Jiang, L.; Wang, T.; Yang, R.; Xu, X.; Yang, G.; Lu, J. Association between Parenting and Non-Suicidal Self-Injury among Adolescents in Yunnan, China: A Cross-Sectional Survey. PeerJ 2020, 8, e10493. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira Costa, R.P.; Peixoto, A.L.R.P.; Lucas, C.C.A.; Falcão, D.N.; da Silva Farias, J.T.; Viana, L.F.P.; Pereira, M.A.d.A.; Sandes, M.L.B.; Lopes, T.B.; Mousinho, K.C.; et al. Profile of Non-Suicidal Self-Injury in Adolescents: Interface with Impulsiveness and Loneliness. J. Pediatr. 2021, 97, 184–190. [Google Scholar] [CrossRef]
- Wasserman, D.; Carli, V.; Wasserman, C.; Apter, A.; Balazs, J.; Bobes, J.; Bracale, R.; Brunner, R.; Bursztein-Lipsicas, C.; Corcoran, P.; et al. Saving and Empowering Young Lives in Europe (SEYLE): A Randomized Controlled Trial. BMC Public Health 2010, 10, 192. [Google Scholar] [CrossRef]
- Balázs, J. Öngyilkosság-prevenció az iskolákban: A Fiatalkori Mentális Egészség-öntudatosság Program (YAM) bemutatása. Educatio 2019, 28, 541–549. [Google Scholar] [CrossRef]
- Ahmed, S.P.; Bittencourt-Hewitt, A.; Sebastian, C.L. Neurocognitive Bases of Emotion Regulation Development in Adolescence. Dev. Cogn. Neurosci. 2015, 15, 11–25. [Google Scholar] [CrossRef]
- Pfeifer, J.H.; Allen, N.B. Puberty Initiates Cascading Relationships Between Neurodevelopmental, Social, and Internalizing Processes Across Adolescence. Biol. Psychiatry 2021, 89, 99–108. [Google Scholar] [CrossRef]
- Hoff, E.R.; Muehlenkamp, J.J. Nonsuicidal Self-Injury in College Students: The Role of Perfectionism and Rumination. Suicide Life Threat. Behav. 2009, 39, 576–587. [Google Scholar] [CrossRef]
- Selby, E.A.; Bender, T.W.; Gordon, K.H.; Nock, M.K.; Joiner, T.E. Non-Suicidal Self-Injury (NSSI) Disorder: A Preliminary Study. Personal. Disord. 2012, 3, 167–175. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, J.; Zhang, X.; Lin, X.; Sun, Y.; Wang, N.; Wang, J.; Luo, F. The Relationship between Perfectionism and Social Anxiety: A Moderated Mediation Model. Int. J. Environ. Res. Public Health 2022, 19, 12934. [Google Scholar] [CrossRef] [PubMed]
- Gnilka, P.B.; Ashby, J.S.; Noble, C.M. Multidimensional Perfectionism and Anxiety: Differences Among Individuals with Perfectionism and Tests of a Coping-Mediation Model. J. Couns. Dev. 2012, 90, 427–436. [Google Scholar] [CrossRef]
- Bentley, K.H.; Cassiello-Robbins, C.F.; Vittorio, L.; Sauer-Zavala, S.; Barlow, D.H. The Association between Nonsuicidal Self-Injury and the Emotional Disorders: A Meta-Analytic Review. Clin. Psychol. Rev. 2015, 37, 72–88. [Google Scholar] [CrossRef] [PubMed]
- Silverman, M.M.; Berman, A.L.; Sanddal, N.D.; O’carroll, P.W.; Joiner, T.E. Rebuilding the Tower of Babel: A Revised Nomenclature for the Study of Suicide and Suicidal Behaviors. Part 2: Suicide-Related Ideations, Communications, and Behaviors. Suicide Life-Threat. Behav. 2007, 37, 264–277. [Google Scholar] [CrossRef] [PubMed]
- Venta, A.; Sharp, C.; Hart, J. The Relation between Anxiety Disorder and Experiential Avoidance in Inpatient Adolescents. Psychol. Assess. 2012, 24, 240–248. [Google Scholar] [CrossRef]
- Chapman, A.L.; Gratz, K.L.; Brown, M.Z. Solving the Puzzle of Deliberate Self-Harm: The Experiential Avoidance Model. Behav. Res. Ther. 2006, 44, 371–394. [Google Scholar] [CrossRef]
- Bock, R.C.; Berghoff, C.R.; Baker, L.D.; Tull, M.T.; Gratz, K.L. The Relation of Anxiety to Nonsuicidal Self Injury Is Indirect Through Mindfulness. Mindfulness 2021, 12, 2022–2033. [Google Scholar] [CrossRef]
- Selby, E.A.; Franklin, J.; Carson-Wong, A.; Rizvi, S.L. Emotional Cascades and Self-Injury: Investigating Instability of Rumination and Negative Emotion. J. Clin. Psychol. 2013, 69, 1213–1227. [Google Scholar] [CrossRef]
- Roxborough, H.M.; Hewitt, P.L.; Kaldas, J.; Flett, G.L.; Caelian, C.M.; Sherry, S.; Sherry, D.L. Perfectionistic Self-Presentation, Socially Prescribed Perfectionism, and Suicide in Youth: A Test of the Perfectionism Social Disconnection Model. Suicide Life-Threat. Behav. 2012, 42, 217–233. [Google Scholar] [CrossRef]
- Flett, G.L.; Coulter, L.-M.; Hewitt, P.L. The Perfectionistic Self-Presentation Scale–Junior Form: Psychometric Properties and Association with Social Anxiety in Early Adolescents. Can. J. Sch. Psychol. 2012, 27, 136–149. [Google Scholar] [CrossRef]
- Flett, G.L.; Hewitt, P.L. Disguised Distress in Children and Adolescents “Flying Under The Radar”: Why Psychological Problems Are Underestimated and How Schools Must Respond. Can. J. Sch. Psychol. 2013, 28, 12–27. [Google Scholar] [CrossRef]
- Valkenburg, P.M.; Peter, J. Online Communication Among Adolescents: An Integrated Model of Its Attraction, Opportunities, and Risks. J. Adolesc. Health 2011, 48, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Suh, H.; Sohn, H.; Kim, T.; Lee, D.-G. A Review and Meta-Analysis of Perfectionism Interventions: Comparing Face-to-Face with Online Modalities. J. Couns. Psychol. 2019, 66, 473–486. [Google Scholar] [CrossRef] [PubMed]
- Schuler, P.A. Perfectionism and Gifted Adolescents. J. Second. Gift. Educ. 2000, 11, 183–196. [Google Scholar] [CrossRef]
| Types of NSSI | NSSI | Male (n = 42) | Male % | Female (n = 104) | Female % | X2 (p-Value) |
|---|---|---|---|---|---|---|
| Cutting | No | 35 | 83.33% | 63 | 60.58% | 15.04 (0.52) |
| Yes | 7 | 16.67% | 41 | 39.42% | ||
| Biting | No | 30 | 71.43% | 81 | 77.88% | 11.80 (0.46) |
| Yes | 12 | 28.57% | 23 | 22.12% | ||
| Burning | No | 35 | 83.33% | 87 | 83.65% | 6.06 (0.64) |
| Yes | 7 | 16.67% | 17 | 16.35% | ||
| Carving | No | 34 | 80.95% | 84 | 80.77% | 6.92 (0.54) |
| Yes | 8 | 19.05% | 20 | 19.23% | ||
| Pinching | No | 31 | 73.81% | 88 | 84.62% | 8.67 (0.56) |
| Yes | 11 | 26.19% | 16 | 15.38% | ||
| Hair pulling | No | 35 | 83.33% | 96 | 92.31% | 6.24 (0.40) |
| Yes | 7 | 16.67% | 8 | 7.69% | ||
| Severe scratching | No | 38 | 90.48% | 86 | 82.69% | 7.50 (0.68) |
| Yes | 4 | 9.52% | 18 | 17.31% | ||
| Banging/hitting | No | 27 | 64.29% | 77 | 74.04% | 13.55 (0.63) |
| Yes | 15 | 35.71% | 27 | 25.96% | ||
| Wound picking | No | 26 | 61.90% | 73 | 70.19% | 29.21 (0.11) |
| Yes | 16 | 38.10% | 31 | 29.81% | ||
| Rubbing skin against rough surfaces | No | 37 | 88.10% | 94 | 90.38% | 4.50 (0.61) |
| Yes | 5 | 11.90% | 10 | 9.62% | ||
| Needle-sticking | No | 40 | 95.24% | 90 | 86.54% | 7.06 (0.53) |
| Yes | 2 | 4.76% | 14 | 13.46% | ||
| Swallowing chemicals | No | 37 | 88.10% | 99 | 95.19% | 7.72 (0.10) |
| Yes | 5 | 11.90% | 5 | 4.81% |
| Mental Disorder | N = 146 | % | NSSI (n = 90) | % | No NSSI (n = 56) | % |
|---|---|---|---|---|---|---|
| Autism spectrum disorder a | 70 | 47.95 | 47 | 52.22 | 23 | 41.07 |
| Suicidality | 44 | 30.14 | 33 | 36.67 | 11 | 19.64 |
| Mood disorders | 41 | 28.08 | 33 | 36.67 | 8 | 14.29 |
| Anxiety disorders | 40 | 27.40 | 35 | 38.89 | 5 | 8.93 |
| Substance use disorders | 25 | 17.12 | 19 | 21.11 | 6 | 10.71 |
| Eating disorders | 21 | 14.38 | 19 | 21.11 | 2 | 3.57 |
| Borderline personality disorder | 16 | 10.96 | 14 | 15.56 | 2 | 3.57 |
| Tic | 14 | 9.59 | 10 | 11.11 | 4 | 7.14 |
| Psychotic disorders | 11 | 7.53 | 8 | 8.89 | 3 | 5.36 |
| Attention-disruptive disorders | 9 | 6.16 | 6 | 6.67 | 3 | 5.36 |
| Outcome Variables | NSSI (N = 146) | NSSI Intrapersonal Motivation (n = 134) | NSSI Interpersonal Motivation (n = 134) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | SE | t | df | Pr (>|t|) | Estimate | SE | t | df | Pr (>|t|) | Estimate | SE | t | df | Pr (>|t|) | |
| FMPS–CMD | 0.04 | 0.02 | 1.70 | 141 | 0.09 | 0.05 | 0.02 | 2.94 | 128 | <0.01 ** | 0.04 | 0.01 | 2.58 | 128 | 0.01 * |
| FMPS–PEC | −0.01 | 0.03 | −0.46 | 141 | 0.65 | <0.01 | 0.02 | 0.02 | 128 | 0.98 | <0.01 | 0.02 | −0.09 | 128 | 0.93 |
| FMPS–PS | 0.01 | 0.05 | 0.29 | 141 | 0.77 | <0.01 | 0.04 | −0.1 | 128 | 0.95 | <0.01 | 0.03 | −0.03 | 128 | 0.98 |
| FMPS–O | −0.11 | 0.05 | −2.07 | 141 | 0.04 * | −0.06 | 0.04 | −1.7 | 128 | 0.1 | −0.09 | 0.03 | −2.82 | 128 | 0.01 * |
| Intercept | 1.56 | 1.12 | 1.39 | 141 | 0.17 | 1.06 | 0.75 | 1.41 | 128 | 0.16 | 2.07 | 0.65 | 3.18 | 128 | <0.01 ** |
| Outcome Variable | NSSI (N = 146) | NSSI Intrapersonal Motivation (n = 134) | NSSI Interpersonal Motivation (n = 134) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | SE | t | df | Pr (>|t|) | Estimate | SE | t | df | Pr (>|t|) | Estimate | SE | t | df | Pr (>|t|) | |
| Intercept | 2.73 | 1.36 | 2 | 130 | 0.05 * | 1.84 | 0.73 | 2.54 | 118 | 0.01 * | 2.15 | 0.67 | 3.20 | 118 | <0.01 ** |
| Mood | 0.88 | 0.62 | 1.43 | 130 | 0.16 | 0.63 | 0.34 | 1.83 | 118 | 0.07 | 0.02 | 0.33 | 0.05 | 118 | 0.96 |
| Anxiety disorder | 2.39 | 0.77 | 3.09 | 130 | <0.01 ** | 1.03 | 0.37 | 2.79 | 118 | <0.01 ** | 1.13 | 0.35 | 3.21 | 118 | <0.01 ** |
| Substance use disorder | 0.91 | 0.65 | 1.4 | 130 | 0.17 | 0.30 | 0.37 | 0.81 | 118 | 0.42 | 0.32 | 0.34 | 0.94 | 118 | 0.35 |
| Attention-disruptive disorders | −1.45 | 1.06 | −1.38 | 130 | 0.17 | −0.31 | 0.55 | −0.56 | 118 | 0.58 | −0.23 | 0.52 | −0.45 | 118 | 0.65 |
| Tic | 0.44 | 0.79 | 0.56 | 130 | 0.58 | −0.40 | 0.54 | −0.74 | 118 | 0.46 | 0.24 | 0.46 | 0.51 | 118 | 0.61 |
| Eating disorders | 1.85 | 1 | 1.85 | 130 | 0.07 | 0.72 | 0.38 | 1.89 | 118 | 0.06 | 0.58 | 0.37 | 1.56 | 118 | 0.12 |
| Psychotic disorders | −1.56 | 1.07 | −1.45 | 130 | 0.15 | −0.31 | 0.52 | −0.60 | 118 | 0.55 | −0.15 | 0.49 | −0.31 | 118 | 0.75 |
| Autism spectrum disorders | 0.01 | 0.5 | 0.01 | 130 | 0.99 | −0.11 | 0.33 | −0.34 | 118 | 0.74 | −0.05 | 0.31 | −0.17 | 118 | 0.87 |
| Borderline personality disorders | 1.73 | 1.1 | 1.56 | 130 | 0.12 | 0.96 | 0.51 | 1.89 | 118 | 0.06 | 0.66 | 0.48 | 1.38 | 118 | 0.17 |
| Suicidality | −0.27 | 0.63 | −0.44 | 130 | 0.66 | 0.06 | 0.39 | 0.16 | 118 | 0.88 | 0.08 | 0.36 | 0.21 | 118 | 0.83 |
| FMPS–CMD | <0.01 | 0.03 | −0.05 | 130 | 0.96 | 0.02 | 0.02 | 0.99 | 118 | 0.33 | 0.01 | 0.02 | 0.63 | 118 | 0.53 |
| FMPS–PEC | −0.07 | 0.04 | −1.83 | 130 | 0.07 | −0.03 | 0.02 | −1.29 | 118 | 0.20 | −0.02 | 0.02 | −0.92 | 118 | 0.36 |
| FMPS–PS | 0.07 | 0.06 | 1.15 | 130 | 0.25 | 0.01 | 0.04 | 0.15 | 118 | 0.88 | 0.02 | 0.03 | 0.52 | 118 | 0.60 |
| FMPS–O | −0.14 | 0.06 | −2.36 | 130 | 0.02 * | −0.08 | 0.04 | −2.13 | 118 | 0.04 * | −0.09 | 0.03 | −2.75 | 118 | <0.01 ** |
| Outcome Variable | Anxiety Disorders | ||||
|---|---|---|---|---|---|
| Estimate | SE | t | df | Pr (>|t|) | |
| Intercept | −4.72 | 1.73 | −2.73 | 140 | 0.01 ** |
| FMPS–CMD | 0.09 | 0.03 | 3.07 | 140 | <0.01 ** |
| FMPS–PEC | 0.06 | 0.03 | 1.83 | 140 | 0.07 |
| FMPS–PS | −0.08 | 0.07 | −1.15 | 140 | 0.25 |
| FMPS–O | 0.03 | 0.07 | 0.47 | 140 | 0.64 |
| Variable | FMPS–PS | FMPS–CMD | FMPS–PEC | |||
|---|---|---|---|---|---|---|
| ρ | p | ρ | p | ρ | p | |
| FMPS–CMD | 0.68 *** | <0.001 | ||||
| FMPS–PEC | 0.37 *** | <0.001 | 0.49 *** | <0.001 | ||
| FMPS–O | 0.45 *** | <0.001 | 0.16 | 0.05 | 0.11 | 0.17 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gyori, D.; Farkas, B.F.; Komaromy, D.; Horvath, L.O.; Kollarovics, N.; Garas, P.; Balazs, J. The Association between Nonsuicidal Self-Injury and Perfectionism in Adolescence: The Role of Mental Disorders. Eur. J. Investig. Health Psychol. Educ. 2023, 13, 2299-2327. https://doi.org/10.3390/ejihpe13110163
Gyori D, Farkas BF, Komaromy D, Horvath LO, Kollarovics N, Garas P, Balazs J. The Association between Nonsuicidal Self-Injury and Perfectionism in Adolescence: The Role of Mental Disorders. European Journal of Investigation in Health, Psychology and Education. 2023; 13(11):2299-2327. https://doi.org/10.3390/ejihpe13110163
Chicago/Turabian StyleGyori, Dora, Bernadett Frida Farkas, Daniel Komaromy, Lili Olga Horvath, Nora Kollarovics, Peter Garas, and Judit Balazs. 2023. "The Association between Nonsuicidal Self-Injury and Perfectionism in Adolescence: The Role of Mental Disorders" European Journal of Investigation in Health, Psychology and Education 13, no. 11: 2299-2327. https://doi.org/10.3390/ejihpe13110163
APA StyleGyori, D., Farkas, B. F., Komaromy, D., Horvath, L. O., Kollarovics, N., Garas, P., & Balazs, J. (2023). The Association between Nonsuicidal Self-Injury and Perfectionism in Adolescence: The Role of Mental Disorders. European Journal of Investigation in Health, Psychology and Education, 13(11), 2299-2327. https://doi.org/10.3390/ejihpe13110163








