Consensus Statement on the Assessment of Comorbidities in People Living with HIV in Romania
Abstract
Introduction
Methods
Consensus statement
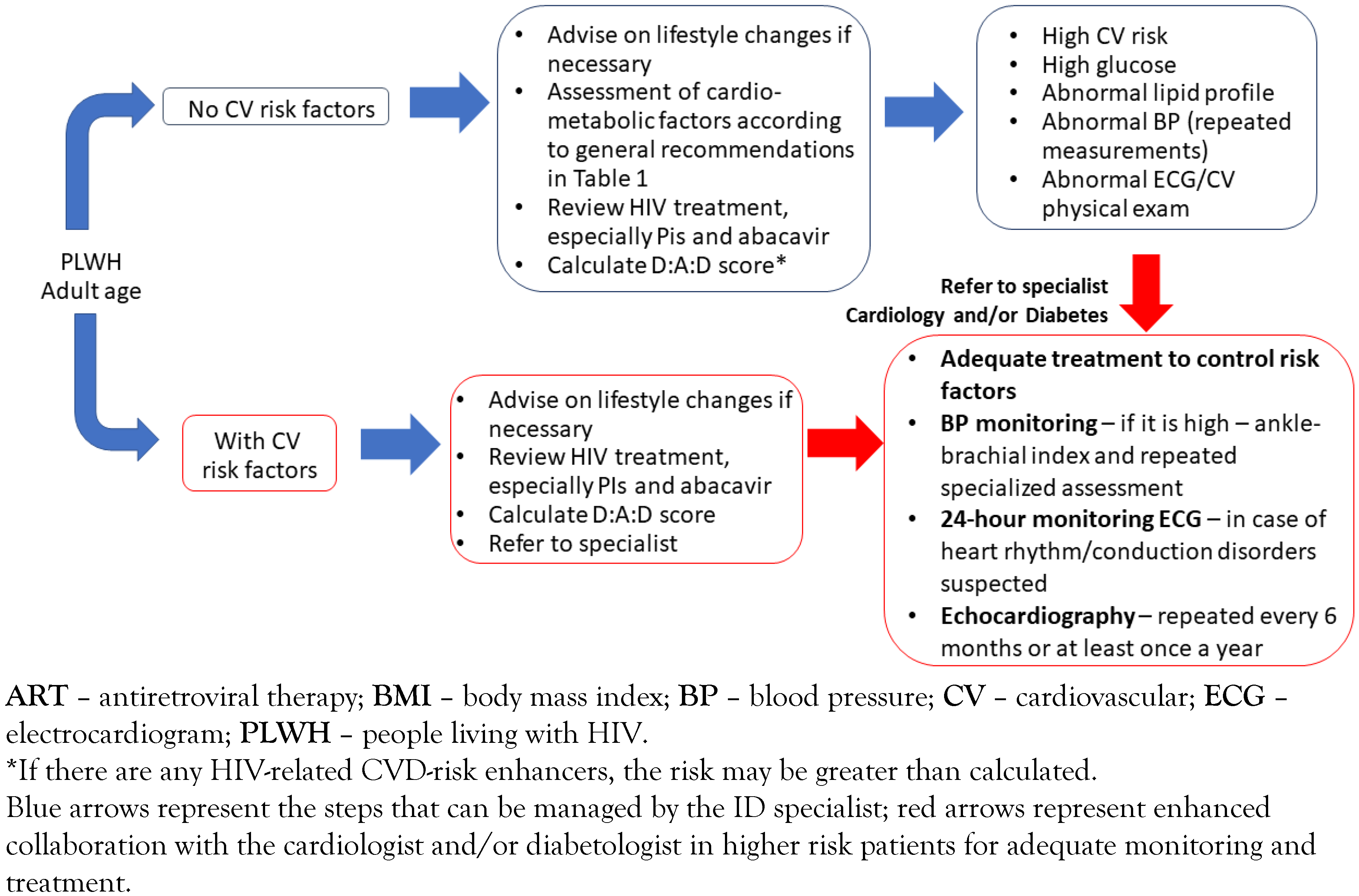
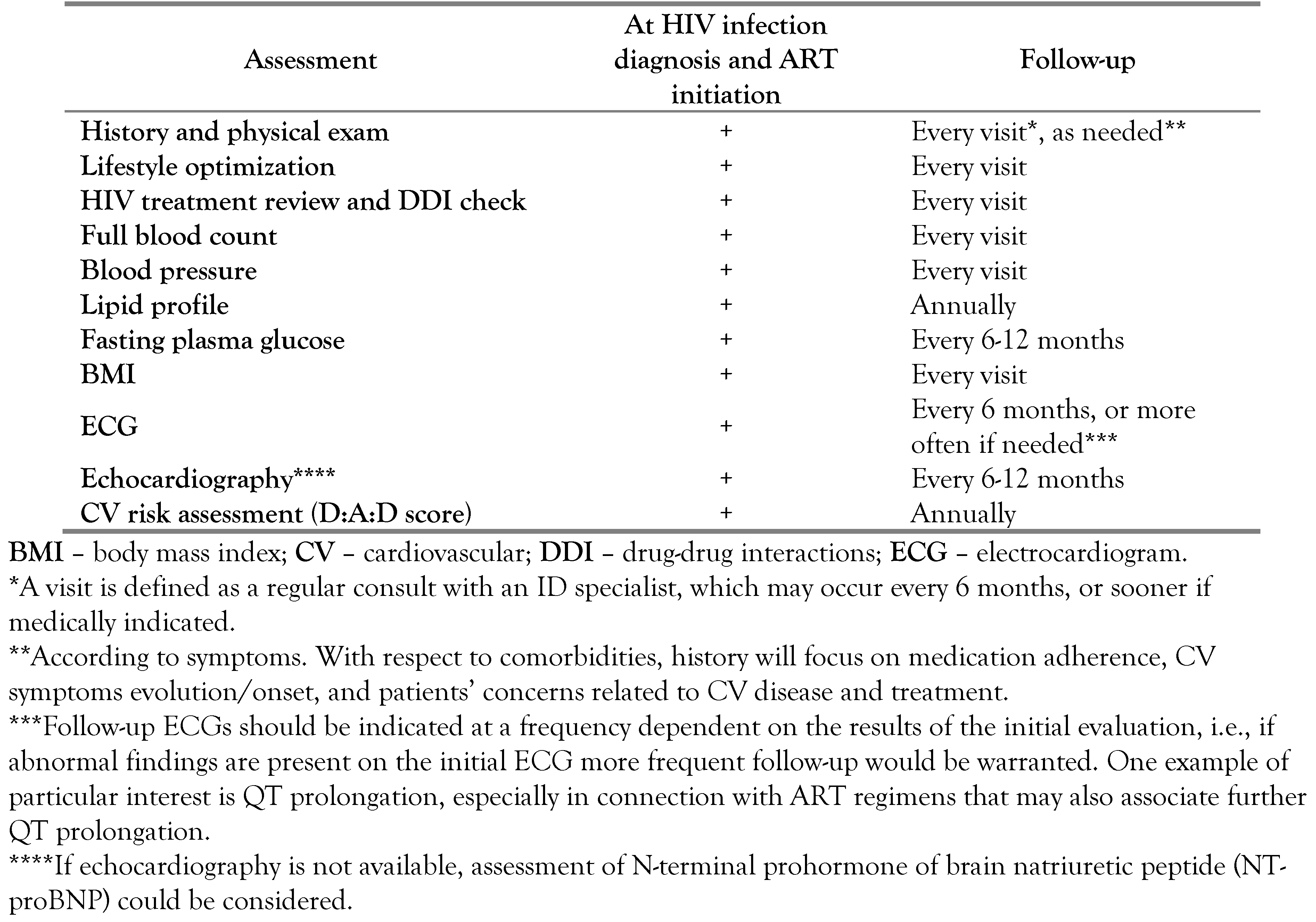
Cardio-metabolic disease
General information
High blood pressure
Myocardial infarction (MI) and stroke
Heart failure
Diabetes
Cardiovascular risk assessment
Summary
- All adult PLWH should be adequately informed about the CV risk associated with HIV infection and the importance of controlling modifiable risk factors—smoking, obesity, blood pressure and plasma glucose levels.
- Cardiovascular risk should be assessed yearly in all patients with HIV infection, regardless of age.
- HIV-related treatment should be reviewed at every visit, considering the specific CV issues associated with particular ARV drugs. If a change in ART is warranted, a thorough assessment of the risk-benefit ratio should be performed first.
- Clinicians should continue regular monitoring of CV risk factors in patients with adequate ART.
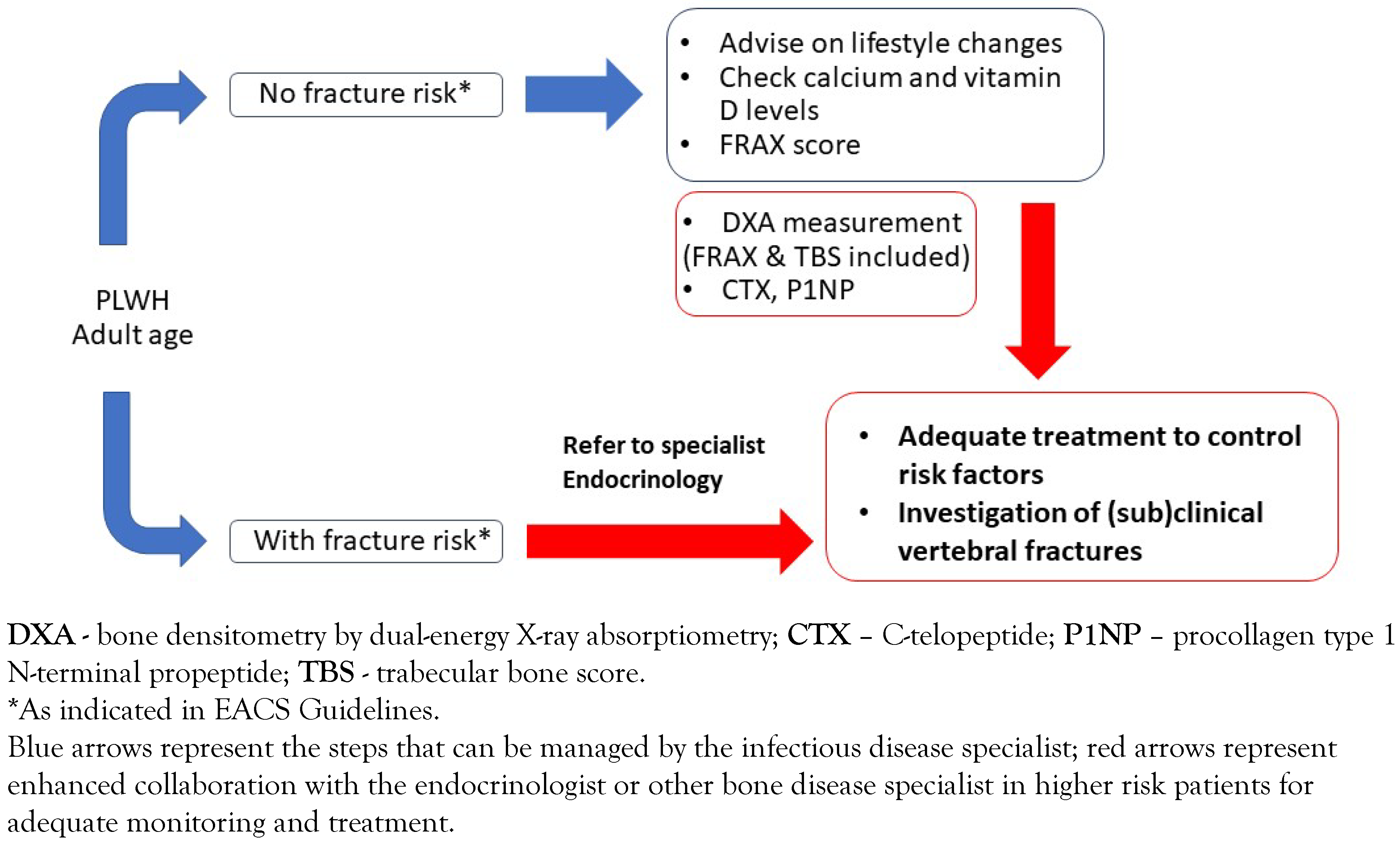
Bone disease
General information
Risk assessment for bone disease
Summary
- Smoking cessation, increase in physical activity and reduction of alcohol consumption should be recommended to all adult PLWH, irrespective of ART treatment regimen.
- The FRAX score could be used for assessing and monitoring the risk of fracture.
- Periodic monitoring with DXA measurement, especially in high-risk patients could be beneficial to identify the candidates for medical intervention.
- Adequate supplementation with calcium and vitamin D, as well as hormonal substitution should only be prescribed based on laboratory results and in collaboration with an endocrinologist for treatment adjustment and monitoring.
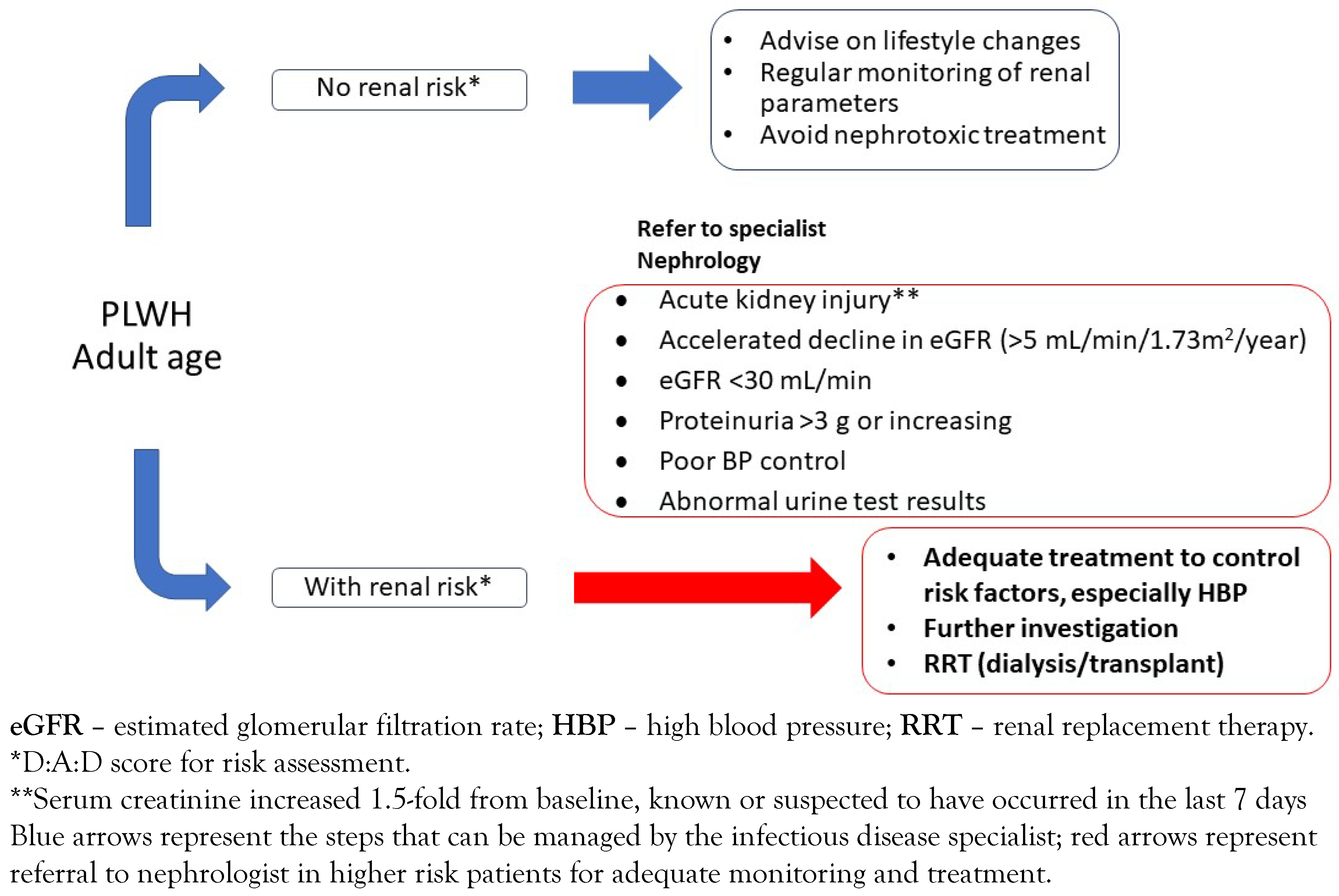
Kidney disease
General information
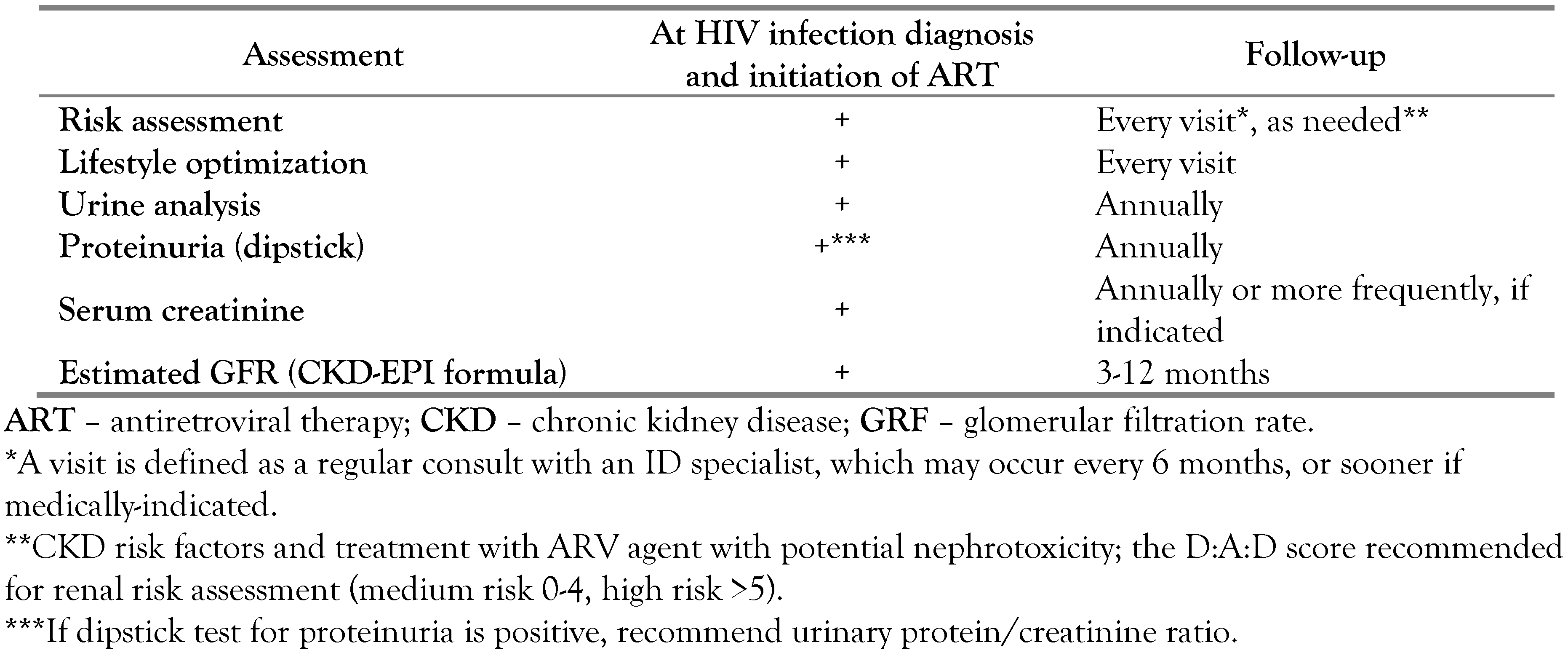
Risk assessment for kidney disease
Summary
- The risk of CKD is higher in PLWH than in uninfected individuals. It should be assessed at HIV infection diagnosis and ART initiation and then at every visit.
- In clinical practice, we recommend risk assessment with the D:A:D score, checking for proteinuria and assessing serum creatinine, and repeating tests depending on the initial response (low risk—at 12 months, moderate risk—at 6 months, high risk—at 3 months).
- If proteinuria is higher than 1+ or eGFR is lower than 60 mL/min/1.73m2 for at least 3 months, diagnose CKD.
- Increase in creatinine, accelerated decline of eGFR, increasing proteinuria, and persistent abnormal urine test results are indicators for referral to nephrology department.
- In addition to lifestyle changes (smoking cessation, weight control, low sodium diet), clinicians should pay attention to potentially nephrotoxic ARV agents or drugs administered for the management of comorbidities, as well as to drug-drug interactions.
Depression
General information
Risk assessment for depression
Summary
- The PLWH’s journey is characterized by many emotional ups and downs, which can vary from person to person.
- Depression may be associated with a negative impact on patient outcomes, including quality of life, life plans, social and vocational functioning and treatment adherence.
- The first two weeks after diagnosing HIV infection may represent a critical timeframe for the patient. Other potential triggers for depression may include any major life changes on a personal, social or professional level.
- The ID physician should pay close attention, to ensure timely identification of any signs of depression, which would warrant referral to a psychologist.
Discussion
Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- UNAIDS Global HIV & AIDS Statistics–2019 Fact Sheet. Available online: https://www.unaids.org/en/resources/fact-sheet (accessed on 12 September 2019).
- Romanian National Committee for Fighting Against AIDS. HIV/AIDS infection in Romania—Update 30 June 2019. Available online: http://cnlas.ro/images/doc/30062019_rom.pdf (accessed on 12 September 2019).
- Gokengin, D.; Oprea, C.; Begovac, J.; et al. HIV care in Central and Eastern Europe: How close are we to the target? Int J Infect Dis 2018, 70, 121–130. [Google Scholar] [CrossRef]
- European AIDS Clinical Society. EACS Guidelines 2015 (version 8.0). Available online: https://www.eacsociety.org/files/guidelines_8.0-englishrevised_20160610.pdf (accessed on 12 September 2019).
- European AIDS Clinical Society. EACS Guidelines 2018 (version 9.1). Available online: https://www.eacsociety.org/files/2018_guidelines-9.1english.pdf (accessed on 12 September 2019).
- INSIGHTSTARTStudy Group; Lundgren, J. D.; Babiker, A.G.; et al. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med 2015, 373, 795–807. [Google Scholar] [CrossRef]
- Appay, V.; Almeida, J.R.; Sauce, D.; Autran, B.; Papagno, L. Accelerated immune senescence and HIV-1 infection. Exp Gerontol 2007, 42, 432–437. [Google Scholar] [CrossRef]
- Guaraldi, G.; Orlando, G.; Zona, S.; et al. Premature agerelated comorbidities among HIV-infected persons compared with the general population. Clin Infect Dis 2011, 53, 1120–1126. [Google Scholar] [CrossRef] [PubMed]
- Guaraldi, G. The transition from co-morbidities to geriatric syndromes in HIV. Germs 2016, 6, 79–81. [Google Scholar] [CrossRef] [PubMed]
- Rockstroh, J.; Guaraldi, G.; Deray, G. HIV and the body: A review of multidisciplinary management. HIV Med 2010, 11 (Suppl. 2), 1–8. [Google Scholar] [CrossRef] [PubMed]
- Hentzein, M.; Dramé, M.; Delpierre, C.; et al. HIV-related excess mortality and age-related comorbidities in patients with HIV aged ≥60, a relative survival analysis in the French Dat’AIDS cohort. BMJ Open 2019, 9, e024841. [Google Scholar] [CrossRef]
- Streinu-Cercel, A.; Săndulescu, O.; Ceapraga, G.; et al. Prevalence of osteo-renal impairment in the Romanian HIV cohort. BMC Infect Dis 2016, 16 (Suppl. 1). [Google Scholar] [CrossRef]
- Feinstein, M.J.; Hsue, P.Y.; Benjamin, L.A.; et al. Characteristics, prevention, and management of cardiovascular disease in people living with HIV: A scientific statement from the American Heart Association. Circulation 2019, 140, e98–e124. [Google Scholar] [CrossRef]
- Dorjee, K.; Choden, T.; Baxi, S.M.; Steinmaus, C.; Reingold, A.L. Risk of cardiovascular disease associated with exposure to abacavir among individuals with HIV: A systematic review and meta-analysis of results from 17 epidemiological studies. Int J Antimicrob Agents 2018, 52, 541–553. [Google Scholar] [CrossRef]
- Schouten, J.; Wit, F.W.; Stolte, I.G.; et al. Cross-sectional comparison of the prevalence of age-associated comorbidities and their risk factors between HIVinfected and uninfected individuals: The AGEhIV cohort study. Clin Infect Dis 2014, 59, 1787–1797. [Google Scholar] [CrossRef]
- Pelchen-Matthews, A.; Ryom, L.; Borges, Á.H.; et al. Aging and the evolution of comorbidities among HIV-positive individuals in a European cohort. AIDS 2018, 32, 240516. [Google Scholar] [CrossRef] [PubMed]
- Cerrato, E.; D’Ascenzo, F.; Biondi-Zoccai, G.; et al. Cardiac dysfunction in pauci symptomatic human immunodeficiency virus patients: A meta-analysis in the highly active antiretroviral therapy era. Eur Heart J 2013, 34, 1432–1436. [Google Scholar] [CrossRef]
- Freiberg, M.S.; Chang, C.H.; Skanderson, M.; et al. Association between HIV infection and the risk of heart failure with reduced ejection fraction and preserved ejection fraction in the antiretroviral therapy era: Results from the Veterans Aging Cohort Study. JAMA Cardiol 2017, 2, 536–546. [Google Scholar] [CrossRef]
- Guaraldi, G.; Orlando, G.; Squillace, N.; et al. Multidisciplinary approach to the treatment of metabolic and morphologic alterations of HIV-related lipodystrophy. HIV Clin Trials 2006, 7, 97–106. [Google Scholar] [CrossRef]
- Murata, H.; Hruz, P.W.; Mueckler, M. The mechanism of insulin resistance caused by HIV protease inhibitor therapy. Biol Chem 2000, 275, 20251–20254. [Google Scholar] [CrossRef]
- Worm, S.V.; De Wit, S.; Weber, R.; et al. Diabetes mellitus, preexisting coronary heart disease, and the risk of subsequent coronary heart disease events in patients infected with human immunodeficiency virus: The Data Collection on Adverse Events of Anti-HIV Drugs (D:A:D Study). Circulation 2009, 119, 805–811. [Google Scholar] [CrossRef]
- D’Agostino, R.B., Sr.; Vasan, R.S.; Pencina, M.J.; et al. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation 2008, 117, 743–753. [Google Scholar] [CrossRef] [PubMed]
- Catapano, A.L.; Reiner, Z.; De Backer, G.; et al. ESC/EAS Guidelines for the management of dyslipidaemias. The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Atherosclerosis 2011, 217, 3–46. [Google Scholar] [CrossRef]
- Friis-Møller, N.; Ryom, L.; Smith, C.; et al. An updated prediction model of the global risk of cardiovascular disease in HIV-positive persons: The Data-collection on Adverse Effects of Anti-HIV Drugs (D:A:D) study. Eur J Prev Cardiol 2016, 23, 214–223. [Google Scholar] [CrossRef] [PubMed]
- Stone, B.; Dockrell, D.; Bowmann, C.; McCloskey, E. HIV and bone disease. Arch Biochem Biophys 2010, 503, 6677. [Google Scholar] [CrossRef] [PubMed]
- Ilha, T.A.S.H.; Comim, F.V.; Copes, R.M.; Compston, J.E.; Premaor, M.O. HIV and vertebral fractures: A systematic review and metanalysis. Sci Rep 2018, 8, 7838. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, L.D.; May, M.T.; Kronborg, G.; et al. Time trends for risk of severe age-related diseases in individuals with and without HIV infection in Denmark: A nationwide population-based cohort study. Lancet HIV 2015, 2, e288–e298. [Google Scholar] [CrossRef]
- McComsey, G.A.; Tebas, P.; Shane, E.; et al. Bone disease in HIV infection: A practical review and recommendations for HIV care providers. Clin Infect Dis 2010, 51, 937–946. [Google Scholar] [CrossRef]
- Poiana, C.; Capatina, C.; Streinu-Cercel, A.; Sandulescu, O.; Streinu-Cercel, A. Hypovitaminosis D in HIV-infected patients. Acta Endocrinol (Buchar) 2019, 5, 102–106. [Google Scholar] [CrossRef] [PubMed]
- Horosanu, G.C.; Streinu-Cercel, A.; Tudor, A.M.; StreinuCercel, A. A profile of specific risk factors for chronic kidney disease-mineral and bone disorder in Romanian HIV-positive patients. J Contemp Clin Pract 2016, 2, 18–24. [Google Scholar] [CrossRef]
- Saracho, R.; Martín Escobar, E.; Comas Farnés, J.; et al. Clinical evolution of chronic renal patients with HIV infection in replacement therapy. Nefrologia 2015, 35, 457–464. [Google Scholar] [CrossRef]
- Gonzalez, J.; Batchelder, A.W.; Psaros, C.; Safren, S.A. Depression and HIV/AIDS treatment nonadherence: A review and meta-analysis. J Acquir Immune Defic Syndr 2011, 58, 181–187. [Google Scholar] [CrossRef]

© GERMS 2025.
Share and Cite
Streinu-Cercel, A.; Săndulescu, O.; Poiană, C.; Dorobanţu, M.; Mircescu, G.; Lăzureanu, V.E.; Dumitru, I.-M.; Chirilă, O.; Streinu-Cercel, A.; Extended Consensus Group. Consensus Statement on the Assessment of Comorbidities in People Living with HIV in Romania. GERMS 2019, 9, 198-210. https://doi.org/10.18683/germs.2019.1178
Streinu-Cercel A, Săndulescu O, Poiană C, Dorobanţu M, Mircescu G, Lăzureanu VE, Dumitru I-M, Chirilă O, Streinu-Cercel A, Extended Consensus Group. Consensus Statement on the Assessment of Comorbidities in People Living with HIV in Romania. GERMS. 2019; 9(4):198-210. https://doi.org/10.18683/germs.2019.1178
Chicago/Turabian StyleStreinu-Cercel, Anca, Oana Săndulescu, Cătălina Poiană, Maria Dorobanţu, Gabriel Mircescu, Voichiţa Elena Lăzureanu, Irina-Magdalena Dumitru, Odette Chirilă, Adrian Streinu-Cercel, and Extended Consensus Group. 2019. "Consensus Statement on the Assessment of Comorbidities in People Living with HIV in Romania" GERMS 9, no. 4: 198-210. https://doi.org/10.18683/germs.2019.1178
APA StyleStreinu-Cercel, A., Săndulescu, O., Poiană, C., Dorobanţu, M., Mircescu, G., Lăzureanu, V. E., Dumitru, I.-M., Chirilă, O., Streinu-Cercel, A., & Extended Consensus Group. (2019). Consensus Statement on the Assessment of Comorbidities in People Living with HIV in Romania. GERMS, 9(4), 198-210. https://doi.org/10.18683/germs.2019.1178



