High Frequency of Mycoplasma pneumoniae Among Patients with Atypical Pneumonia in Tehran, Iran
Abstract
Introduction
Methods
Patients and clinical specimens
Cultivation of M. pneumoniae
Biochemical identification
DNA extraction
Molecular identification
Statistical analysis
Results
General characteristics of the study population
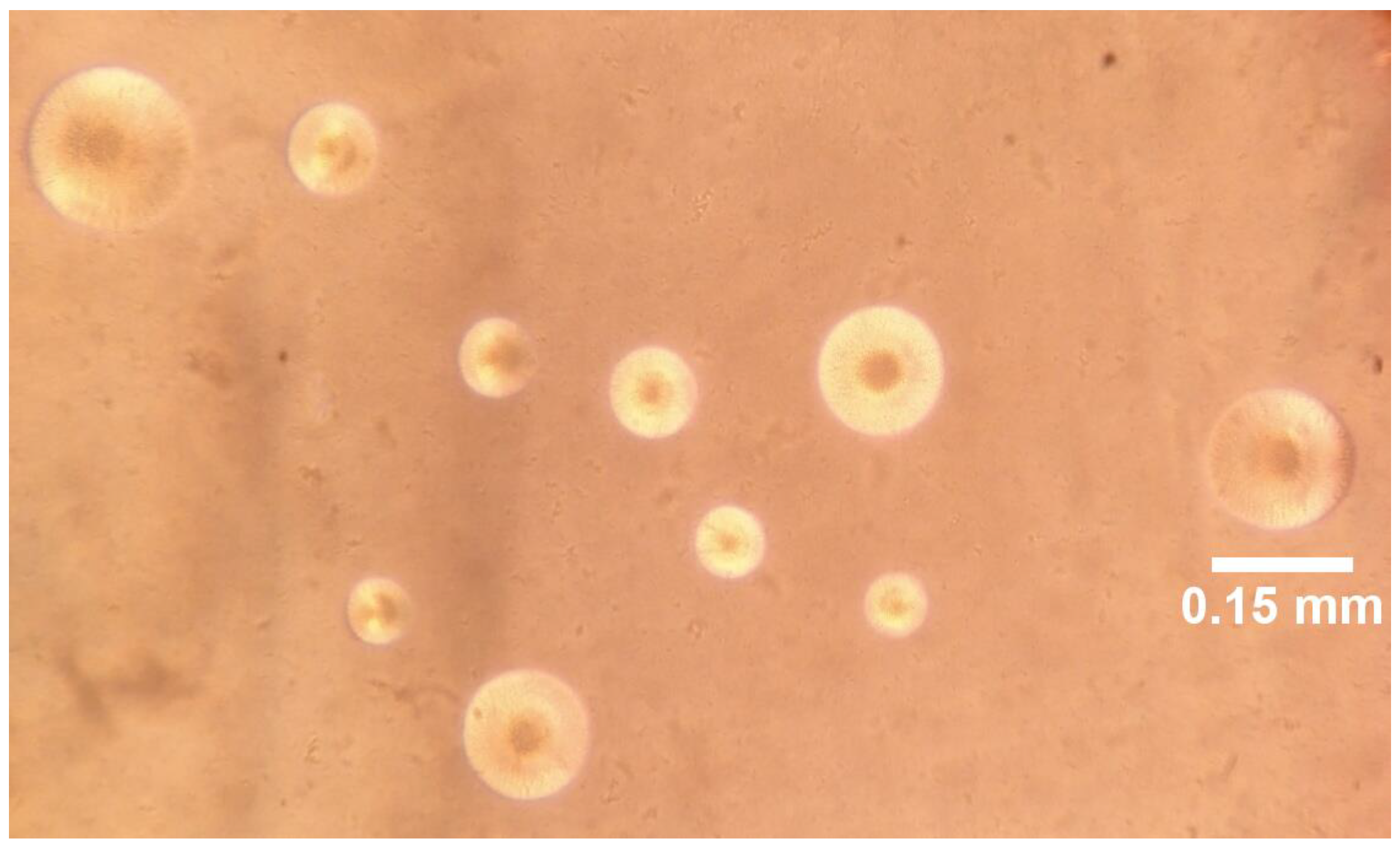
Culture characteristics and biochemical tests
Molecular detection
Comparison of PCR and culture
Discussion
Conclusion
Author Contributions
Conflicts of Interest
Acknowledgments and Funding Support
References
- Restrepo, M.I.; Reyes, L.F.; Anzueto, A. Complication of community-acquired pneumonia (including cardiac complications). Semin Respir Crit Care Med 2016, 37, 897–904. [Google Scholar] [PubMed]
- Foering, A. Community acquired pneumonia. Kabod 2017, 3, 8. [Google Scholar]
- Ratliff, A.E.; Duffy, L.B.; Waites, K.B. Comparison of the illumigene Mycoplasma DNA amplification assay and culture for detection of Mycoplasma pneumoniae. J Clin Microbiol 2014, 52, 1060–1063. [Google Scholar] [CrossRef] [PubMed]
- Meyer Sauteur, P.M.; Unger, W.W.; Nadal, D.; Berger, C.; Vink, C.; van Rossum, A. Infection with and carriage of Mycoplasma pneumoniae in children. Front Microbiol 2016, 7, 329. [Google Scholar] [CrossRef] [PubMed]
- Winchell, J.M. Mycoplasma pneumoniae—A national public health perspective. Curr Pediatr Rev 2013, 9, 324–333. [Google Scholar] [CrossRef]
- Dumke, R.; Schnee, C.; Pletz, M.W.; et al. Mycoplasma pneumoniae and Chlamydia spp. infection in community-acquired pneumonia, Germany, 2011–2012. Emerg Infect Dis 2015, 21, 426–434. [Google Scholar]
- Petrone, B.L.; Wolff, B.J.; DeLaney, A.A.; Diaz, M.H.; Winchell, J.M. Isothermal detection of Mycoplasma pneumoniae directly from respiratory clinical specimens. J Clin Microbiol 2015, 53, 2970–2976. [Google Scholar] [CrossRef] [PubMed]
- Waites, K.B.; Talkington, D.F. Mycoplasma pneumoniae and its role as a human pathogen. Clin Microbiol Rev 2004, 17, 697–728. [Google Scholar] [CrossRef] [PubMed]
- Ieven, M.M.; Loens, K. Should serology be abolished in favor of PCR for the diagnosis of Mycoplasma pneumoniae infections? Curr Pediatr Rev 2013, 9, 304–313. [Google Scholar] [CrossRef]
- Whistler, T.; Sawatwong, P.; Diaz, M.H.; et al. Molecular characterization of Mycoplasma pneumoniae infections in two rural populations of Thailand from 2009-2012. J Clin Microbiol 2017, 55, 2222–2233. [Google Scholar] [CrossRef] [PubMed]
- Colle, J.G.; Marmion, B.P.; Fraser, A.G.; Simmons, A. (Eds.) Mackie & McCartney Practical Medical Microbiology, 13th ed.; Churchill Livingstone: New York, 1996. [Google Scholar]
- Golmohammadi, R.; Ataee, R.A.; Alishiri, G.H.; et al. Molecular diagnosis of Mycoplasma pneumoniae in synovial fluid of rheumatoid arthritis patients. Iran J Med Microbiol 2014, 8, 1–8. [Google Scholar]
- Pooladgar, A.R.; Looni, R.; Ghaemmaghami, S.; Pourbakhsh, A.; Ashtari, A.; Shirudi, A. Isolation and identification of Mycoplasma agalactiae by culture and polymerase chain reaction (PCR) from affected sheep to contagious agalactia of Khuzestan province, Iran. Arch Razi Inst 2015, 70, 21–27. [Google Scholar]
- Clinical Laboratory Management. Bailey & Scott’s Diagnostic Microbiology, 12th ed.; Forbes, B., Sahm, D., Weissfeld, A., Eds.; Mosby: St. Louis, MO, USA, 2007; p. 1056. [Google Scholar]
- She, R.C.; Thurber, A.; Hymas, W.C.; et al. Limited utility of culture for Mycoplasma pneumoniae and Chlamydophila pneumoniae for diagnosis of respiratory tract infections. J Clin Microbiol 2010, 48, 3380–3382. [Google Scholar] [CrossRef] [PubMed]
- Bajantri, B.; Venkatram, S.; Diaz-Fuentes, G. Mycoplasma pneumoniae: A potentially severe infection. J Clin Med Res 2018, 10, 535–544. [Google Scholar]
- Ghotaslou, R.; Sharifi, S.; Akhi, M.T.; Soroush, M.H. Epidemiology, clinical features, and laboratory detection of Mycoplasma pneumoniae infection in East Azerbaijan, Iran. Turk J Med Sci 2013, 43, 521–524. [Google Scholar] [CrossRef]
- Oskooee, M.B.; Karimi, A.; Shiva, F.; et al. Detection of Mycoplasma pneumoniae and Chlamydia trachomatis in Iranian children with acute lower respiratory infections by polymerase chain reaction. Asian Pac J Trop Dis 2014, 4, S302–S306. [Google Scholar] [CrossRef]
- Elkholy, A.; Elkaraksy, H.; Fattouh, A.; Bazaraa, H.; Hegazy, R.; AbdElhalim, M. Acute lower respiratory tract infection due to Chlamydia and Mycoplasma spp. in Egyptian children under 5 years of age. J Trop Pediatr 2009, 55, 195–197. [Google Scholar] [CrossRef]
- Meijer, A.; Dagnelie, C.; De Jong, J.; et al. Low prevalence of Chlamydia pneumoniae and Mycoplasma pneumoniae among patients with symptoms of respiratory tract infections in Dutch general practices. Eur J Epidemiol 2000, 16, 1099–1106. [Google Scholar] [CrossRef] [PubMed]
- Bosnak, M.; Dikici, B.; Bosnak, V.; et al. Prevalence of Mycoplasma pneumoniae in children in Diyarbakir, the south-east of Turkey. Pediatr Int 2002, 44, 510–512. [Google Scholar] [CrossRef] [PubMed]
- Maltezou, H.C.; La-Scola, B.; Astra, H.; et al. Mycoplasma pneumoniae and Legionella pneumophila in community-acquired lower respiratory tract infections among hospitalized children: Diagnosis by real time, P. C.R. Scand J Infect Dis 2004, 36, 639–642. [Google Scholar]
- Tsolia, M.N.; Psarras, S.; Bossios, A.; et al. Etiology of community-acquired pneumonia in hospitalized school-age children: Evidence for high prevalence of viral infections. Clin Infect Dis 2004, 39, 681–686. [Google Scholar] [CrossRef] [PubMed]
- Del Valle-Mendoza, J.; Orellana-Peralta, F.; Marcelo-Rodríguez, A.; et al. High prevalence of Mycoplasma pneumoniae and Chlamydia pneumoniae in children with acute respiratory infections from Lima, Peru. PLoS ONE 2017, 12, e0170787. [Google Scholar] [CrossRef] [PubMed]
- Fisher-Hoch, S.P.; Mathews, C.E.; McCormick, J.B. Obesity, diabetes and pneumonia: The menacing interface of non-communicable and infectious diseases. Trop Med Int Health 2013, 18, 1510–1519. [Google Scholar] [CrossRef] [PubMed]
| Inhibition of growth by | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Species | Requirement for yeast extracts | Thallium acetate (0.001% w/v)) | Methylene blue (0.001% w/v)) | Erythromycin (100 µg/mL) | Lincomycin (100 µg/mL) | Hemolysis | Hemadsorption | Acid from glucose | Arginine | Urea | Aerobic reduction of tetrazolium |
| M. pneumoniae | + | - | - | + | - | β | + | + | - | - | + |
| M. fermentans | - | - | + | + | + | - | - | + | + | - | - |
| M. hominis | - | - | + | - | + | - or x | - | - | + | - | - |
| M. orale 1 (M. orale) | + | - | + | - | + | - | +* | - | + | - | - |
| M. orale 2 (buccale) | - | - | + | - | - | - | - | - | + | - | - |
| M. orale 3 (faucium) | + | - | + | - | - | - | +* | - | + | - | - |
| M. salivarium | - | - | + | - | - | - | - | - | + | - | - |
| M. genitalium | + | + | … | … | … | … | + | + | - | - | ± |
| Ureaplasma urealyticum | + | + | - | + | - | β | - | - | - | + | - |
| M. pneumoniae positive No. (%) | M. pneumoniae negative No. (%) | Total No. (%) | P-value | Odds ratio | 95% confidence interval | ||
|---|---|---|---|---|---|---|---|
| Age | 1-20 | 5 (41.7) | 7 (58.3) | 12 (10.9) | 0.44 | 1.93 | (0.35-10.49) |
| 20-40 | 3 (20) | 12 (80) | 15 (13.6) | 0.19 | 0.29 | (0.04-1.88) | |
| 40-60 | 9 (18.8) | 39 (81.3) | 48 (43.6) | 0.17 | 0.41 | (0.11-1.45) | |
| Sex | Male | 11 (25.6) | 32 (74.4) | 43 (39.1) | 0.46 | 1.50 | (0.05-4.46) |
| Female | 18 (26.9) | 49 (73.1) | 67 (60.9) | ||||
| Chest pain | Yes | 18 (26.9) | 49 (73.1) | 67 (60.9) | 0.003 | 6.45 | (1.91-21.7) |
| No | 10 (17.2) | 48 (82.8) | 58 (52.7) | ||||
| Fever | Yes | 3 (18.8) | 13 (81.3) | 16 (14.5) | 0.59 | 0.61 | (0.10-3.67) |
| No | 26 (27.7) | 68 (72.3) | 94 (85.5) | ||||
| Lethargy | Yes | 13 (24.1) | 41 (75.9) | 54 (49.1) | 0.560 | 1.45 | (0.414-1.85) |
| No | 16 (28.6) | 40 (71.4) | 56 (50.9) | ||||
| Headache | Yes | 6 (18.8) | 26 (81.3) | 32 (29.1) | 0.08 | 0.26 | (0.06-1.20) |
| No | 23 (29.5) | 55 (70.5) | 78 (70.9) | ||||
| Nausea | Yes | 1 (5.1) | 16 (94.1) | 17 (15.5) | 0.09 | 0.12 | (0.01-1.38) |
| No | 28 (30.1) | 65 (69.9) | 93 (84.5) | ||||
| Sore throat | Yes | 6 (19.4) | 25 (80.6) | 31 (64.5) | 0.30 | 2.19 | (0.49-9.71) |
| No | 23 (29.1) | 56 (70.9) | 39 (35.5) | ||||
| Cough | Yes | 19 (26.8) | 52 (73.2) | 71 (64.5) | 0.84 | 1.13 | (0.31-4.11) |
| No | 10 (25.6) | 29 (74.4) | 39 (35.5) | ||||
| Sputum production | Yes | 10 (23.3) | 33 (76.7) | 43 (39.1) | 0.57 | 0.69 | (0.18-2.53) |
| No | 19 (28.4) | 48 (61.1) | 67 (60.9) | ||||
| Dyspnea | Yes | 16 (21.6) | 58 (78.4) | 74 (67.3) | 0.08 | 0.37 | (0.12-1.12) |
| No | 13 (36.1) | 23 (63.9) | 36 (32.7) | ||||
| Anxiety | Yes | 5 (19.2) | 21 (80.8) | 26 (23.6) | 0.98 | 1.01 | (0.21-4.88) |
| No | 24 (28.6) | 60 (71.4) | 84 (76.4) | ||||
| Diabetes | Yes | 7 (43.8) | 9 (56.3) | 16 (14.5) | 0.41 | 1.80 | (0.43-7.49) |
| No | 22 (23.4) | 72 (76.8) | 94 (85.5) | ||||
| Cardiovascular disease | Yes | 6 (25) | 18 (75) | 24 (21.8) | 0.59 | 0.70 | (0.19-2.53) |
| No | 23 (26.7) | 63 (73.3) | 86 (78.2) | ||||
| Kidney failure | Yes | 2 (40) | 3 (60) | 5 (4.5) | 0.57 | 1.99 | (0.17-22.90) |
| No | 27 (25.7) | 78 (74.3) | 105 (95.5) | ||||
© GERMS 2018.
Share and Cite
Arfaatabar, M.; Aminharati, F.; Azimi, G.; Ashtari, A.; Pourbakhsh, S.A.; Masoorian, E.; Pourmand, M.R. High Frequency of Mycoplasma pneumoniae Among Patients with Atypical Pneumonia in Tehran, Iran. Germs 2018, 8, 126-133. https://doi.org/10.18683/germs.2018.1139
Arfaatabar M, Aminharati F, Azimi G, Ashtari A, Pourbakhsh SA, Masoorian E, Pourmand MR. High Frequency of Mycoplasma pneumoniae Among Patients with Atypical Pneumonia in Tehran, Iran. Germs. 2018; 8(3):126-133. https://doi.org/10.18683/germs.2018.1139
Chicago/Turabian StyleArfaatabar, Maryam, Farzaneh Aminharati, Ghasem Azimi, Abbas Ashtari, Seyed Ali Pourbakhsh, Ensieh Masoorian, and Mohammad Reza Pourmand. 2018. "High Frequency of Mycoplasma pneumoniae Among Patients with Atypical Pneumonia in Tehran, Iran" Germs 8, no. 3: 126-133. https://doi.org/10.18683/germs.2018.1139
APA StyleArfaatabar, M., Aminharati, F., Azimi, G., Ashtari, A., Pourbakhsh, S. A., Masoorian, E., & Pourmand, M. R. (2018). High Frequency of Mycoplasma pneumoniae Among Patients with Atypical Pneumonia in Tehran, Iran. Germs, 8(3), 126-133. https://doi.org/10.18683/germs.2018.1139




