Introduction
Sore throat is one of the most common reasons to refer to a primary care physician (either a pediatrician or a general practice physician). In 60-70% of cases acute pharyngitis is caused by viruses, including rhinoviruses, adenoviruses, enteroviruses, coronaviruses and others. However, about 5-15% of pharyngitis cases in adults and around 20-30% of cases in children are caused by bacterial infections, among which group A β hemolytic streptococci (GAS) rank first [
1,
2]. Some studies have demonstrated as much as 37% of cases of pharyngitis in children to be caused by GAS [
3].
Among other causative agents of bacterial pharyngitis, group C and group G streptococci,
Mycoplasma pneumoniae,
Chlamydia pneumoniae and
Arcanobacterium haemolyticum are also reported, although much less frequently [
4]. GAS is responsible for a large number of diseases ranging from mild nasopharyngeal infections to autoimmune disorders and severe purulent infections [
5,
6,
7,
8,
9]. Severe GAS-related diseases, such as acute rheumatic fever (ARF), rheumatic heart disease (RHD), post-streptococcal glomerulonephritis, and invasive infections remain an important cause of global morbidity and mortality with a particular impact in low-resource settings [
7].
ARF also remains a problem in developing countries around the world and in indigenous populations living among developed nations [
10,
11]. Therefore, the issue of proper management of streptococcal pharyngitis is very important [
12]. Rational antibiotic therapy is one of the key approaches for the primary prevention of ARF: on the one hand, it plays an important role in the disease prevention while on the other hand, unreasonable use of antibiotics may be associated with hazards rather than benefits, especially in countries with low ARF risk [
13]. Sore throat results in prescription of an antibiotic in 72-90% of cases by Australian primary care physicians, in spite of GAS causing less than 30% of cases [
14]. Primary prevention strategies of GAS infections remain an important issue of health care [
7]. Currently the data about the burden of GAS infections in the pediatric population of Ukraine is unknown. There are only a few studies about prescription of antibiotics in patients with GAS infection that preceded ARF [
6,
11].
The aim of our study was to evaluate the knowledge of pediatricians in diagnosis and management of sore throat in children and to identify further ways to raise their awareness.
Methods
Between December 1, 2020 and February 28, 2021, we conducted a survey among pediatricians on evaluation of diagnosis and management of pharyngitis in children. Pediatricians of Ternopil region, Ukraine, participated in the survey. Ternopil region is located in Western Ukraine and its population is 1,038,695 people of whom 194,180 (18.7%) are children. The total number of pediatricians in Ternopil region is 266, of whom 98 are primary care physicians, and others are secondary and tertiary care pediatricians. There are two children’s hospitals in Ternopil city (regional – 405 beds and municipal – 206 beds). Besides that, there are several children’s departments in district hospitals. There are 6 outpatient pediatric departments in Ternopil city. The pediatricians follow up children mostly in Ternopil city, whereas in districts children are followed up by family physicians. Overall, 112 pediatricians responded to participate in the study. Among the participants, 79 (70.5%) were physicians of the first contact, which was 80.6% of the total number of the primary care pediatricians and 33 (29.5%) physicians worked in the secondary or tertiary care hospital. The inclusion criteria were doctor's consent to participate in the study and cases of GAS pharyngitis in their practice. Therefore, the survey of secondary and tertiary care pediatricians was mainly conducted among pediatricians of the emergency (admission) or diagnostic departments, which led to a relatively lower percentage of physicians in this group. Questionnaires were distributed on-site during the working hours.
The survey included 18 questions. The first four questions were concerning the general data: participant’s age, gender, place of work and experience as a medical practitioner. Other questions were concerning the diagnosis and management of GAS pharyngitis in children: 15 of them were multiple choice questions and 3 – open-ended questions. The questionnaire was based on the items that were used by the Italian researchers [
15] and adapted according to the Ukrainian recommendations [
16]. The survey was conducted by a pediatrician and a pediatric rheumatologist.
Informed consent was obtained before conducting the survey. The participants were informed of the reasons why the information was collected and how it would be used. The participants acknowledged that their participation was voluntary, and they were assured that their answers would be anonymous and confidential.
Ethical approval for the study was provided by the scientific ethics committee at I. Horbachevsky Ternopil National Medical University (Ethics protocol nr. 60 of 01.09.2020).
The study conformed to the principles outlined in the World Medical Association Declaration of Helsinki.
The results were analyzed using standard procedures with Statistica StatSoft 6.0 software package. The mean data are presented as mean ± standard deviation (SD) unless otherwise noted. The categorical variables are presented as percentages. The internal consistency (reliability) of the questionnaire was assessed using the Chronbach’s alpha (α). Items with reliabilities of 0.70 or greater are recommended for comparing patient groups. Construct validity was evaluated using exploratory factor analysis to examine the structure of relationships between the items of questionnaire. To extract factor we applied Principal Component Analysis, with oblique rotation (Direct Oblimin). The differences between frequency distributions (percentages) between the groups were assessed by chi-square (χ2) test with the level of statistical significance set at an α=0.05 level.
Results
All surveyed pediatricians were aged from 24 to 76 years (mean age 45.7±12.3 years). The majority of respondents were women (104 [92.9%]). The duration of work experience ranged from 1 to 46 years (mean: 20.5±12.3 years).
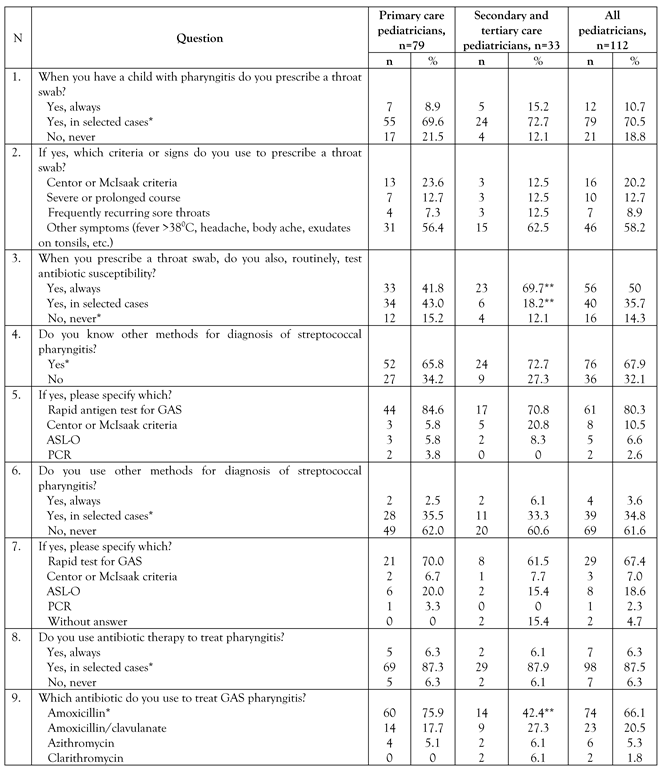
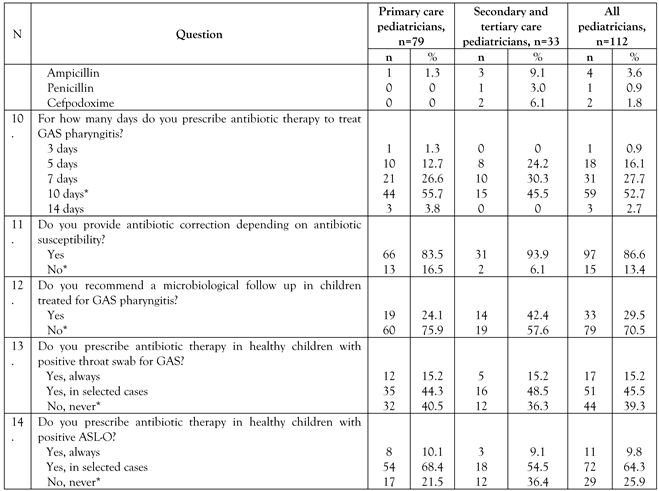
The list of the questions and answers of all the respondents are presented in
Table 1.
Τhe questionnaire was found to be reliable: Cronbach’s alpha coefficient >0.70 for all scales in primary care pediatrician and secondary and tertiary care pediatrician reports. Almost all items of primary care pediatrician and secondary and tertiary care pediatrician reports had a clear factor loading. These results confirm reliability and validity of the questionnaire.
The correct answer for the first question was “yes, in selected cases” and it was given by 70.5% of all participants. There were no significant differences between the answers of primary care and secondary or tertiary care pediatricians. While answering the second question, the majority of respondents of both groups (58.2%) mentioned that they use only one or two symptoms to prescribe a throat swab. There was also no significant difference between the answers of two groups of respondents.
While answering the third question, 85.7% of respondents indicated they practiced routine testing of antibiotic susceptibility “always or in selected cases” when they were prescribing a throat swab. Besides, secondary or tertiary care pediatricians more often responded that they prescribed antibiotic susceptibility test “always” (χ2=7.26; p=0.007), whereas primary care pediatricians more often prescribed it “in selected cases” (χ2=6.26; p=0.012). Accordingly, only 14.3% of pediatricians gave the correct answer.
The majority of surveyed pediatricians knew other methods for diagnosis of streptococcal pharyngitis (67.9%). Overall, 54.5% of participants knew that rapid test can be used for diagnosis of GAS pharyngitis (question 5), but only 25.9% of respondents said they used it “in selected cases” (question 7).
Antibiotic therapy to treat pharyngitis in selected cases was used by 87.5% of respondents, without differences with regard to places of their work. Amoxicillin as antibiotic of the first choice was chosen by 66.1% of respondents, and the primary care pediatricians prescribed it more often than the pediatricians in hospitals (χ2=11.67; p<0.001), whereas antibiotics of the second line (amoxicillin/clavulanate, azithromycin, clarithromycin) were more frequently prescribed by the secondary or tertiary care physicians. Antibiotic therapy was prescribed for 10 days only by 52.7% of respondents.
The majority of surveyed pediatricians (86.6%) responded that they corrected antibiotic therapy depending on antibiotic susceptibility. Overall, 29.5% of pediatricians recommended a microbiological follow-up in children treated for GAS pharyngitis and secondary or tertiary care physicians did that frequently (χ2=3.78; p=0.052). Less than a half of the correct answers were given to questions related to prescription of antibacterial therapy in healthy children, in whom GAS was detected in throat swab (39.3%) and in cases of positive antistreptolysin O (ASL- O) (25.9%), with no significant difference in the percentage of correct answers between the groups.
Discussion
A previous cross-sectional survey in five countries (Australia, Germany, Sweden, UK and USA) showed differences in guidelines describing the management of patients with an acute sore throat between countries [
16]. Moreover, different interpretation of the same scientific studies was found in the guidelines. Different perception of physicians from countries with low risk for rheumatic fever regarding management of patients with acute sore throat indicates the need of an agreement on how to achieve the best practice [
16]. There are no unified guidelines for the management of patients with acute pharyngitis in Ukraine. The basic principles of rational use of antibiotic therapy in children with acute pharyngitis are described in the national Resolution (2010) [
16].
Currently, rapid antigen test for GAS is the most common method for diagnosis of streptococcal pharyngitis / tonsillitis in the primary care practice. This test can be performed in an outpatient clinic with the result available in 5 to 10 minutes with specificity of >95% and sensitivity of 76-87% [
4]. The American Academy of Pediatrics and the American Heart Association recommend antibacterial therapy when the test is positive [
12]. In the case of a negative test and clinically suspected streptococcal pharyngitis, a throat swab is recommended to confirm the etiology of pharyngitis. However, in Ukraine rapid tests for GAS are not available free of charge in public health facilities. Therefore, in our study, we modified the questionnaire that was proposed by Italian researchers [
15] and determined the knowledge about the indications for the prescribing of a throat culture. Throat culture is the “gold standard” for the diagnosis of streptococcal pharyngitis. In ideal conditions, the sensitivity of this method for GAS is 90%, and the specificity is 99%. In real conditions, its sensitivity ranges between 29-90%, and its specificity between 76-99% [
4]. Although primary care physicians in Ukraine have limited opportunities to use the rapid test method, respondents have shown a good awareness of the possibilities of their use (in general, 54.5% knew about this possibility). Instead, the national Resolution calls for a wider use of Centor or McIsaak criteria by practitioners. Moreover, a previous study did not find clear advantages of antigen tests and clinical score using over a clinical score alone [
18]. At the same time, the survey showed insufficient awareness of the possibilities of use Centor or McIsaak criteria for the diagnosis of streptococcal pharyngitis: 20.2% used to prescribe a throat swab and only 3 used them for diagnosis of streptococcal pharyngitis.
Regarding the prescribing of antibacterial therapy, the results of our study showed that most pediatricians chose amoxicillin (66%), and primary care physicians chose it in 76%, which showed better results than in some other studies in which amoxicillin was used to treat GAS pharyngitis in 34-53% of cases [
15,
19]. Our study has found that secondary and tertiary care physicians were more likely to choose second-line antibiotics (amoxicillin/clavulanate, azithromycin, clarithromycin) and even third-generation cephalosporins as compared with the primary care physicians. A study from Italy showed that general practice physicians often prescribed amoxicillin and clavulanic acid (55%) [
15]. Our study has also demonstrated a significantly high percentage of macrolides use (7%), especially by the secondary and tertiary care physicians (12%) as compared with Italian primary care physicians (2%) [
15]. Although some studies indicate the successful use of macrolides, in particular azithromycin for the treatment of tonsillitis / pharyngitis [
20], the high level of resistance to macrolides should be kept in mind [
21,
22]. According to the recent AURA study evaluating the current state of antibiotic resistance in Ukraine, the resistance of
Streptococcus spp. to macrolides was as high as 30% for azithromycin, erythromycin and clarithromycin, and even higher (34%) for clindamycin [
22].
Besides, slightly more than half of all respondents (52.7%) and less than half of secondary and tertiary care physicians (45.5%) gave the correct answer regarding the duration of antibiotic therapy. At the same time, 88% of general practice physicians in Italy correctly recommended a 10-day course of treatment for GAS pharyngitis [
15].
A microbiological follow-up in children treated for GAS pharyngitis was not recommended by 70.5% of physicians; while in Italy only 43% of pediatricians do not perform a microbiological follow-up [
15].
Correct answers regarding routine prescription of antibiotic susceptibility test with a throat swab were given only by 14.3% of all respondents and more often it was prescribed always by secondary and tertiary care pediatricians, whereas in selected cased it was prescribed more frequently by the primary care physicians. Another study demonstrated a higher proportion of correct answers (42%) [
15].
A small number of pediatricians gave the correct answers about the need to prescribe treatment in healthy children with positive throat swab for GAS and with positive ASL-O (39.3% and 25.9%, respectively). Whereas 81% of Italian pediatricians agreed that the carrier state should not be treated [
15]. This may be due to the fact that the national Resolution does not contain information on the strategies related to the GAS carrier, which requires a raise of awareness on this issue [
22].
A study conducted in Sweden also showed that two-thirds of general practice physicians were non-adherent to the national guideline for the management of patients with sore throat and they had a liberal attitude to antibiotics, and one- third were guideline-adherent with a restricted view on antibiotics [
23]. Non-adherent GPs demonstrated significant knowledge gaps.
Thus, our study showed a satisfactory knowledge on some aspects of the diagnosis and management of acute pharyngitis in children, in particular the prescribing of throat swab, the possibility of using a rapid test for GAS, prescribing antibiotics. Significant gaps have been identified in some knowledge, including clinical criteria for streptococcal pharyngitis, duration of antibacterial therapy, interpretation of streptococcal tests in healthy children that indicate the need to create a national guideline and improve physician awareness. A comparison of the awareness of primary and secondary, tertiary care pediatricians showed better awareness of primary care physicians in certain aspects, including the prescribing of amoxicillin. Physicians of the first contact face the problem of acute pharyngitis more often, so obviously, this problem is more relevant for them. Secondary and tertiary care physicians are more focused on second-line antibiotics or reserve antibiotics. However, patients with sore throat can be admitted to inpatient departments due to high fever or comorbid conditions, so improving the knowledge of doctors in hospitals is also important.
GAS remains a major pathogen of acute pharyngitis in the pediatric population, and may be associated with significant complications in the absence of a proper therapeutic attitude. Therefore, improving physician awareness is important for disease control. The use of educational programs may be helpful in improving outcomes, as this has already been demonstrated in the management of other diseases [
24].
This is the first survey addressing the current state of diagnosis and management of pharyngitis in children as well as revealing the pediatricians’ knowledge gaps regarding this issue in Ternopil region of Ukraine which is a low-risk area with an annual incidence of ARF of 1 per 100,000 population [
11]. The limitations of this study are, first of all, related to the self-reported nature of the questionnaire which is not allowing the verification of responses. Hence some participants could skew their answers. In other words, the obtained results were based only on the answers of respondents, which might differ to some extent from the real prescribing. The second possible limitation of our study is that it was performed during a coronavirus disease 2019 (COVID-19) pandemic when physicians seeing patients with sore throat were focused mainly on confirmation or exclusion of COVID-19.