Microbial Profile, Antimicrobial Resistance, and Molecular Characterization of Diabetic Foot Infections in a University Hospital
Abstract
Introduction
Methods
- Detailed history and physical examination including age, sex, previous hospitalization, type and duration of diabetes, body mass index (BMI), presence of diabetic complications such as retinopathy (assessed by an ophthalmologist), hypertension, nephropathy (micro or macro- albuminuria or creatinine >1.5 mg/dL).
- Full clinical assessment of diabetic foot, including the presence of sensory neuropathy, peripheral vascular disease. DFUs were graded according to Wagner-Meggitt classification system [4]. The DFUs were also classified according to IDSA/IWGD [5]. classification. The presence of signs of inflammation/infection (erythema, hotness, swelling, tenderness, purulent discharge) was also evaluated.
- Routine laboratory investigations including complete blood count, fasting blood glucose, HbA1c, inflammatory markers (C- reactive protein – CRP), serum creatinine, urinary albumin creatinine ratio were performed.
- Microbiological investigations.
Sample collection
Quantitative aerobic bacterial and fungal culture
Antimicrobial susceptibility testing
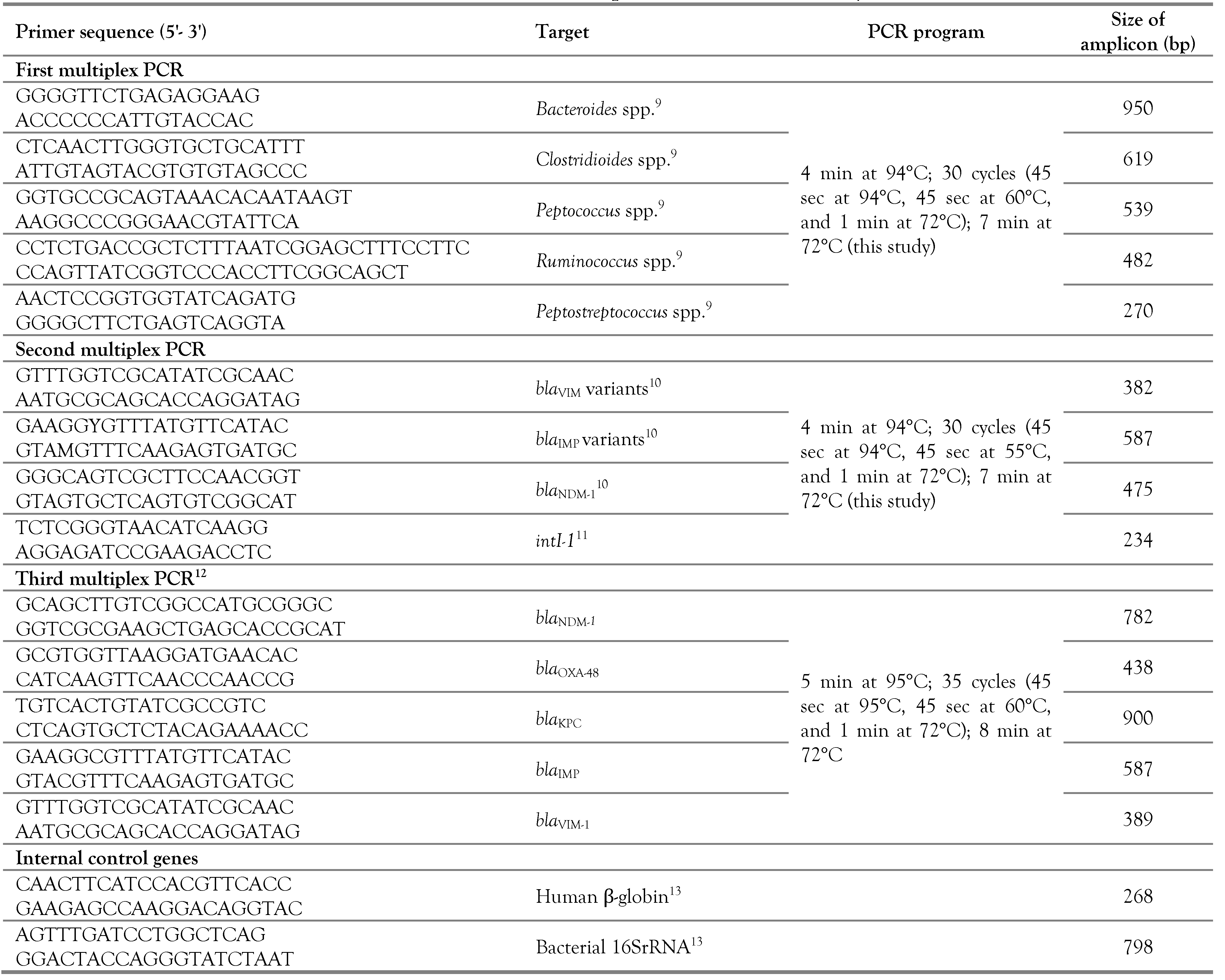
Molecular analysis
Statistical analysis
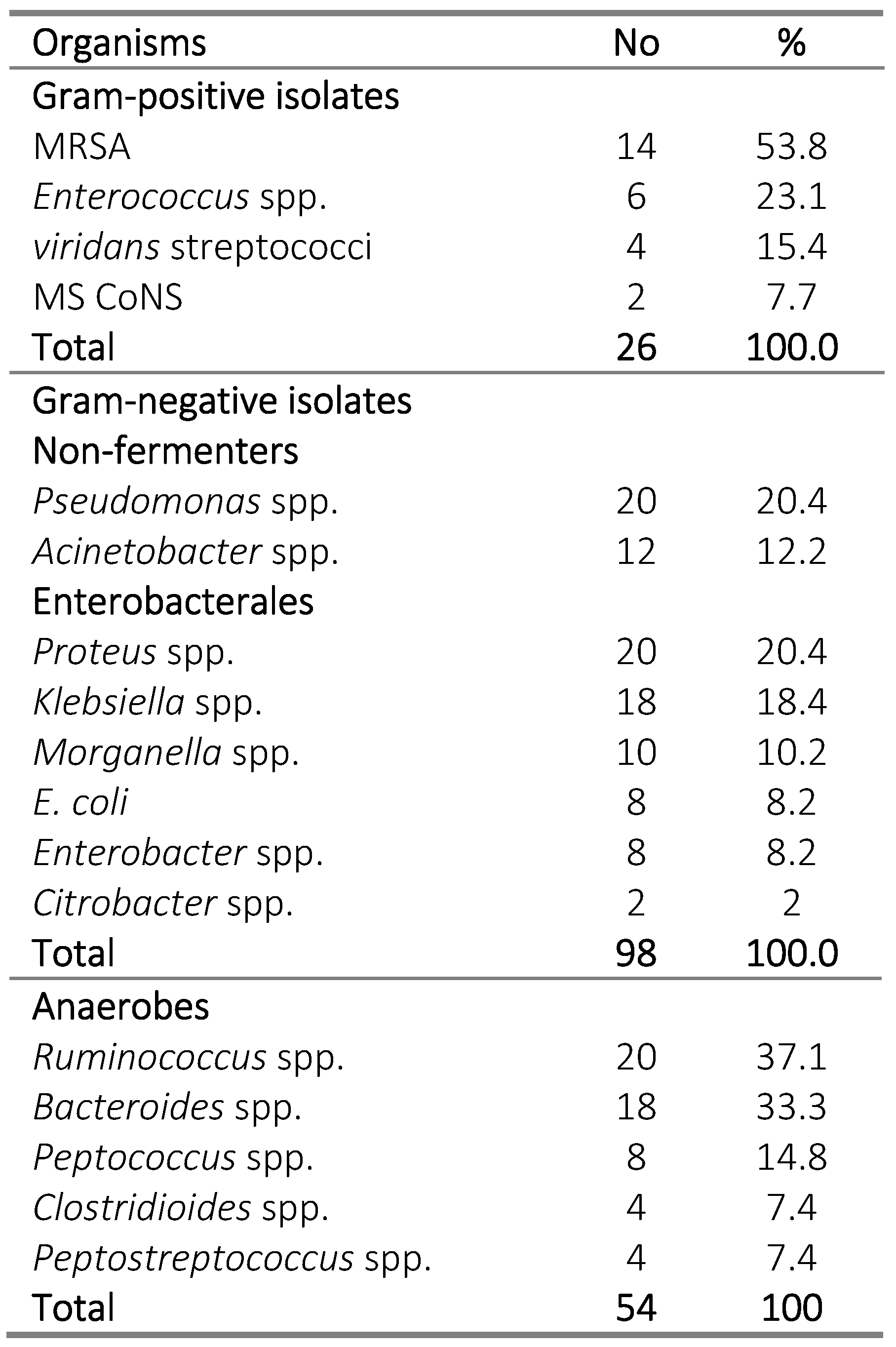
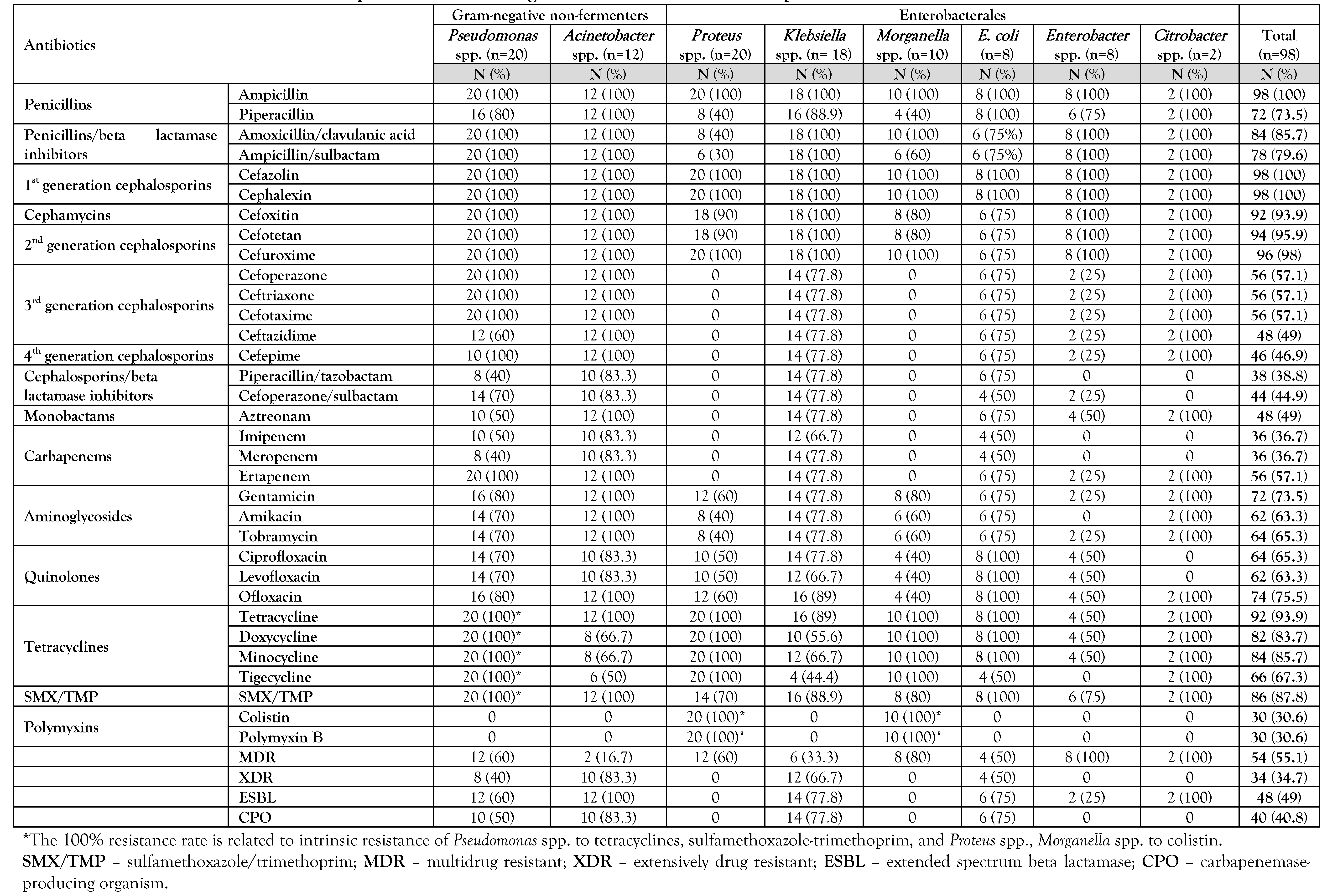
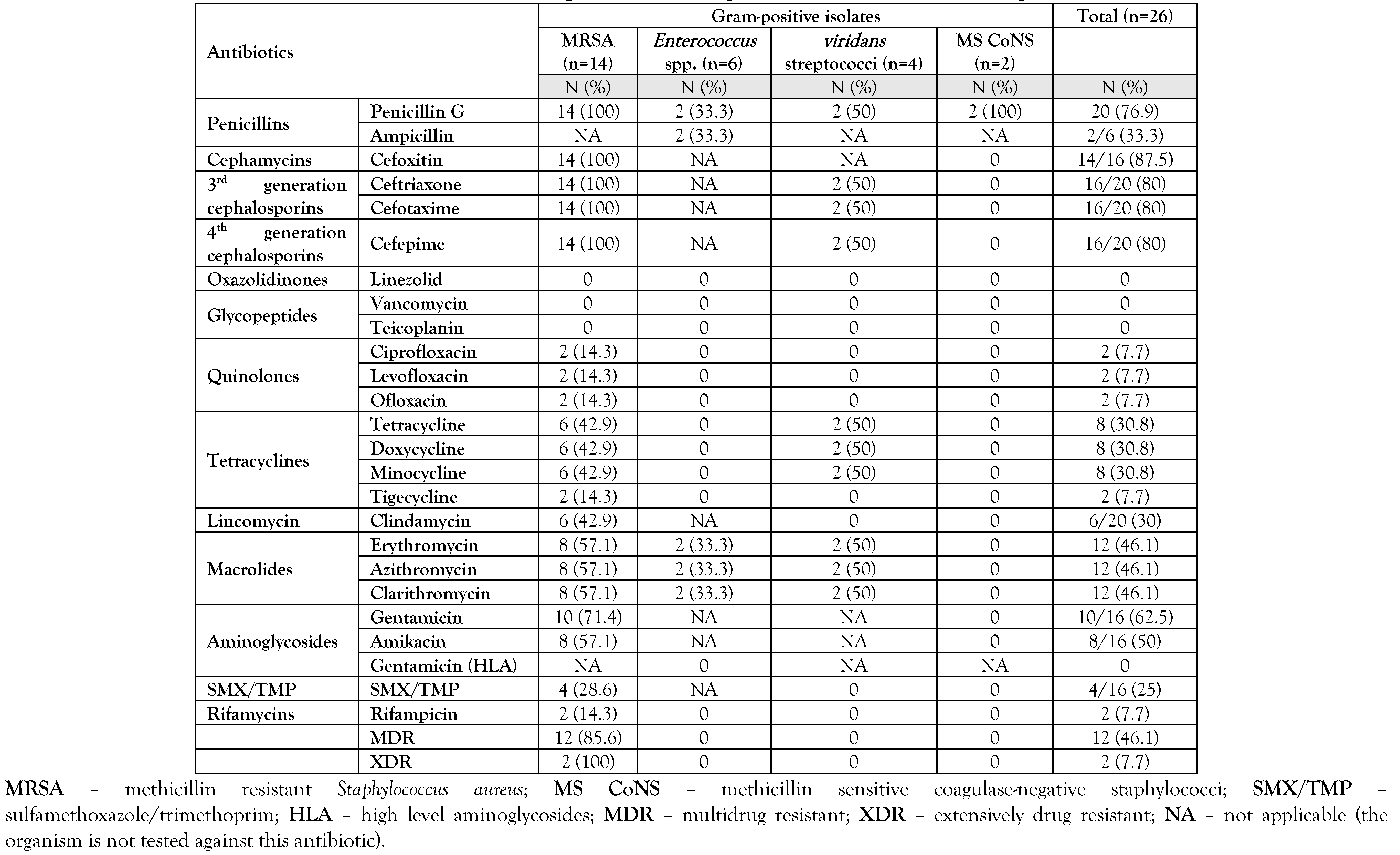
Results
Discussion
Conclusions
Author Contributions
Funding
Conflicts of interest
References
- Armstrong, D.G.; Boulton, A.J.M.; Bus, S.A. Diabetic foot ulcers and their recurrence. N Engl J Med. 2017, 376, 2367–2375. [Google Scholar] [CrossRef]
- Noor, S.; Zubair, M.; Ahmad, J. Diabetic foot ulcer – a review on pathophysiology, classification and microbial etiology. Diabetes Metab Syndr. 2015, 9, 192–199. [Google Scholar] [CrossRef]
- Pitocco, D.; Spanu, T.; Di Leo, M.; et al. Diabetic foot infections: a comprehensive overview. Eur Rev Med Pharmacol Sci. 2019, 23 (Suppl. 2), 26–37. [Google Scholar] [CrossRef] [PubMed]
- Wagner, F.W., Jr. The dysvascular foot: a system for diagnosis and treatment. Foot Ankle. 1981, 2, 64–122. [Google Scholar] [CrossRef]
- Monteiro-Soares, M.; Russell, D.; Boyko, E.J.; et al. Guidelines on the classification of diabetic foot ulcers (IWGDF 2019). Diabetes Metab Res Rev. 2020, 36 (Suppl. 1). [Google Scholar] [CrossRef] [PubMed]
- Tille, P. Bailey and Scott's Diagnostic Microbiology, 14th ed.; Mosby Elsevier: St Louis, MI, USA, 2014. [Google Scholar]
- Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. CLSI supplement M100, 30th ed.CLSI: Wayne, PN, USA.
- Magiorakos, A.P.; Srinivasan, A.; Carey, R.B.; et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 2012, 18, 268–281. [Google Scholar] [CrossRef] [PubMed]
- Rekha, R.; Rizvi, M.A.; Jaishree, P. Designing and validation of genus-specific primers for human gut flora study. Electron J Biotechnol 2006, 9, 505–511. [Google Scholar] [CrossRef]
- Jovcic, B.; Lepsanovic, Z.; Suljagic, V.; et al. Emergence of NDM-1 metallo-β-lactamase in Pseudomonas aeruginosa clinical isolates from Serbia. Antimicrob Agents Chemother. 2011, 55, 3929–3931. [Google Scholar] [CrossRef]
- Rao, A.N.; Barlow, M.; Clark, L.A.; Boring, J.R., 3rd; Tenover, F.C.; McGowan, J.E., Jr. Class 1 integrons in resistant Escherichia coli and Klebsiella spp., US hospitals. Emerg Infect Dis. 2006, 12, 1011–1014. [Google Scholar] [CrossRef]
- Doyle, D.; Peirano, G.; Lascols, C.; Lloyd, T.; Church, D.L.; Pitout, J.D. Laboratory detection of Enterobacteriaceae that produce carbapenemases. J Clin Microbiol. 2012, 50, 3877–3880. [Google Scholar] [CrossRef]
- Kane, T.D.; Alexander, J.W.; Johannigman, J.A. The detection of microbial DNA in the blood: a sensitive method for diagnosing bacteremia and/or bacterial translocation in surgical patients. Ann Surg. 1998, 227, 1–9. [Google Scholar] [CrossRef]
- Cervantes-García, E.; Salazar-Schettino, P.M. Clinical and surgical characteristics of infected diabetic foot ulcers in a tertiary hospital of Mexico. Diabet Foot Ankle. 2017, 8, 1367210. [Google Scholar] [CrossRef]
- Choucair, J.; Saliba, G.; Chehata, N.; Nasnas, R.; Saad, N.R. Epidemiology of the diabetic foot infection in a tertiary care hospital in the Lebanon: a retrospective study between 2000 and 2011. J Infect Dis Ther. 2018, 6, 381. [Google Scholar] [CrossRef]
- Kathirvel, M.; Prabakaran, V.; Jayarajan, J.; Sivakumar, A.; Govinda, V. Risk factors for the diabetic foot infection with multidrug-resistant microorganisms in South India. Int Surg J. 2018, 5, 675–682. [Google Scholar] [CrossRef]
- Abd-El Mohsen, S.A. Diabetic foot ulcer infection rate, bacterial etiology and antibiotic susceptibility: a cross sectional study. Biomed Pharmacol J. 2020, 13. [Google Scholar] [CrossRef]
- Huang, Y.; Cao, Y.; Zou, M.; et al. A Comparison of tissue versus swab culturing of infected diabetic foot wounds. Int J Endocrinol. 2016, 2016, 8198714. [Google Scholar] [CrossRef]
- Gjødsbøl, K.; Skindersoe, M.E.; Christensen, J.J.; et al. No need for biopsies: comparison of three sample techniques for wound microbiota determination. Int Wound J 2012, 9, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Demetriou, M.; Papanas, N.; Panopoulou, M.; Papatheodorou, K.; Bounovas, A.; Maltezos, E. Tissue and swab culture in diabetic foot infections: neuropathic versus neuroischemic ulcers. Int J Low Extrem Wounds. 2013, 12, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Otta, S.; Debata, N.K.; Swain, B. Bacteriological profile of diabetic foot ulcers. CHRISMED J Health Res. 2019, 6, 7–11. [Google Scholar] [CrossRef]
- Hefni, A.; Ibrahim, A.R.; Attia, K.M.; et al. Bacteriological study of diabetic foot infection in Egypt. J Arab Soc Med Res 2013, 8, 26–32. [Google Scholar]
- Dwedar, R.; Ismail, D.K.; Abdulbaky, A. Diabetic foot infection: microbiological causes with special reference to their antibiotic resistance pattern. Egypt J Med Microbiol. 2015, 24, 95–102. [Google Scholar] [CrossRef]
- Miyan, Z.; Fawwad, A.; Sabir, R.; Basit, A. Microbiological pattern of diabetic foot infections at a tertiary care center in a developing country. J Pak Med Assoc. 2017, 67, 665–669. [Google Scholar]
- Ogba, O.M.; Nsan, E.; Eyam, E.S. Aerobic bacteria associated with diabetic foot ulcers and their susceptibility pattern. Biomed Dermatol. 2019, 3, 1. [Google Scholar] [CrossRef]
- Xie, X.; Bao, Y.; Ni, L.; et al. Bacterial profile and antibiotic resistance in patients with diabetic foot ulcer in Guangzhou, Southern China: focus on the differences among different Wagner's grades, IDSA/IWGDF grades, and ulcer types. Int J Endocrinol. 2017, 2017, 8694903. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.B.; Said, A.M.I.; Naira, E.A.; Fatani, A.J.; Emad, E.M.; Soma, A.E. Infection in diabetic foot. Menoufia Med J. 2013, 26, 49–53. [Google Scholar]

 |
 |
 |
 |
 |
© GERMS 2021.
Share and Cite
Ismail, A.A.; Meheissen, M.A.; Elaaty, T.A.A.; Abd-Allatif, N.E.; Kassab, H.S. Microbial Profile, Antimicrobial Resistance, and Molecular Characterization of Diabetic Foot Infections in a University Hospital. GERMS 2021, 11, 39-51. https://doi.org/10.18683/germs.2021.1239
Ismail AA, Meheissen MA, Elaaty TAA, Abd-Allatif NE, Kassab HS. Microbial Profile, Antimicrobial Resistance, and Molecular Characterization of Diabetic Foot Infections in a University Hospital. GERMS. 2021; 11(1):39-51. https://doi.org/10.18683/germs.2021.1239
Chicago/Turabian StyleIsmail, Azza A., Marwa A. Meheissen, Talaat A. Abd Elaaty, Nermine E. Abd-Allatif, and Heba S. Kassab. 2021. "Microbial Profile, Antimicrobial Resistance, and Molecular Characterization of Diabetic Foot Infections in a University Hospital" GERMS 11, no. 1: 39-51. https://doi.org/10.18683/germs.2021.1239
APA StyleIsmail, A. A., Meheissen, M. A., Elaaty, T. A. A., Abd-Allatif, N. E., & Kassab, H. S. (2021). Microbial Profile, Antimicrobial Resistance, and Molecular Characterization of Diabetic Foot Infections in a University Hospital. GERMS, 11(1), 39-51. https://doi.org/10.18683/germs.2021.1239




