Efficacy and Safety of Modified Huang-Lian-Jie-Du Decoction Cream on Cancer Patients with Skin Side Effects Caused by EGFR Inhibition
Abstract
:1. Introduction
2. Materials and Methods
2.1. Modified HLJD (mHLJD) Decoction Preparation
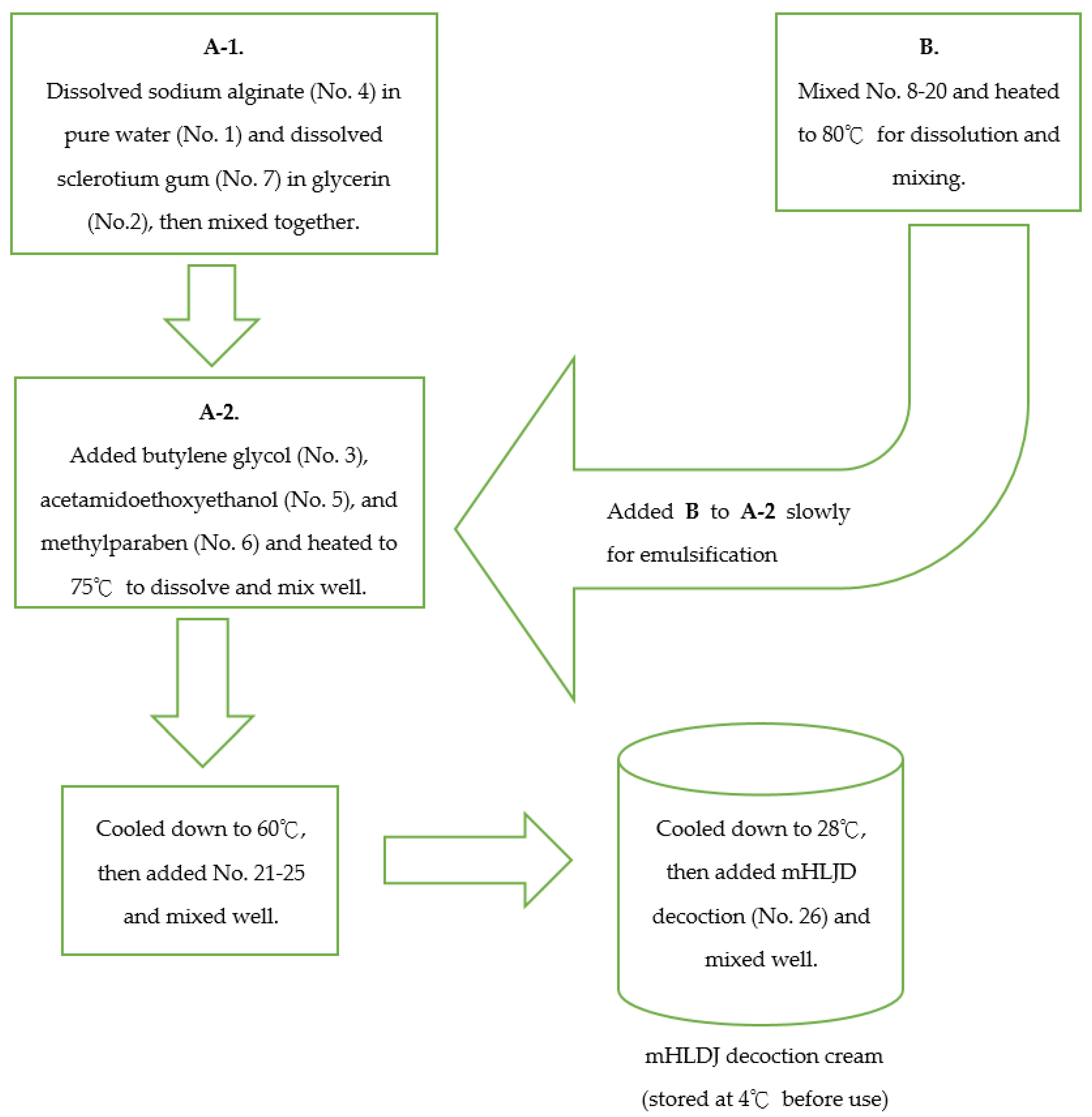
2.2. Production Process of Modified HLJD (mHLJD) Decoction Cream for Skin Use
2.3. Patients
- (1)
- Adult (over 20 years old) malignancy patients who received EGFRIs, such as monoclonal antibodies cetuximab or panitumumab, or who received TKIs, such as gefitinib, erlotinib, or afatinib, in Ditmanson Medical Foundation Chia-Yi Christian Hospital and were screened for this study.
- (2)
- Patients with 1–3 grade of skin toxicities caused by above medications.
- (3)
- If patients were using medications for treating the skin toxicities, they agreed to stop the medications for one week and, after one week, receive mHLJD decoction cream.
- (1)
- The patients’ age less than 20 years old.
- (2)
- Patients unable to achieve good compliance in using topical cream to skin lesions or with acute allergy reaction during first-time use.
- (3)
- During mHLJD treatment period, patients were excluded if they also used other medications for the skin toxicity.
2.4. Statistical Analysis
3. Results
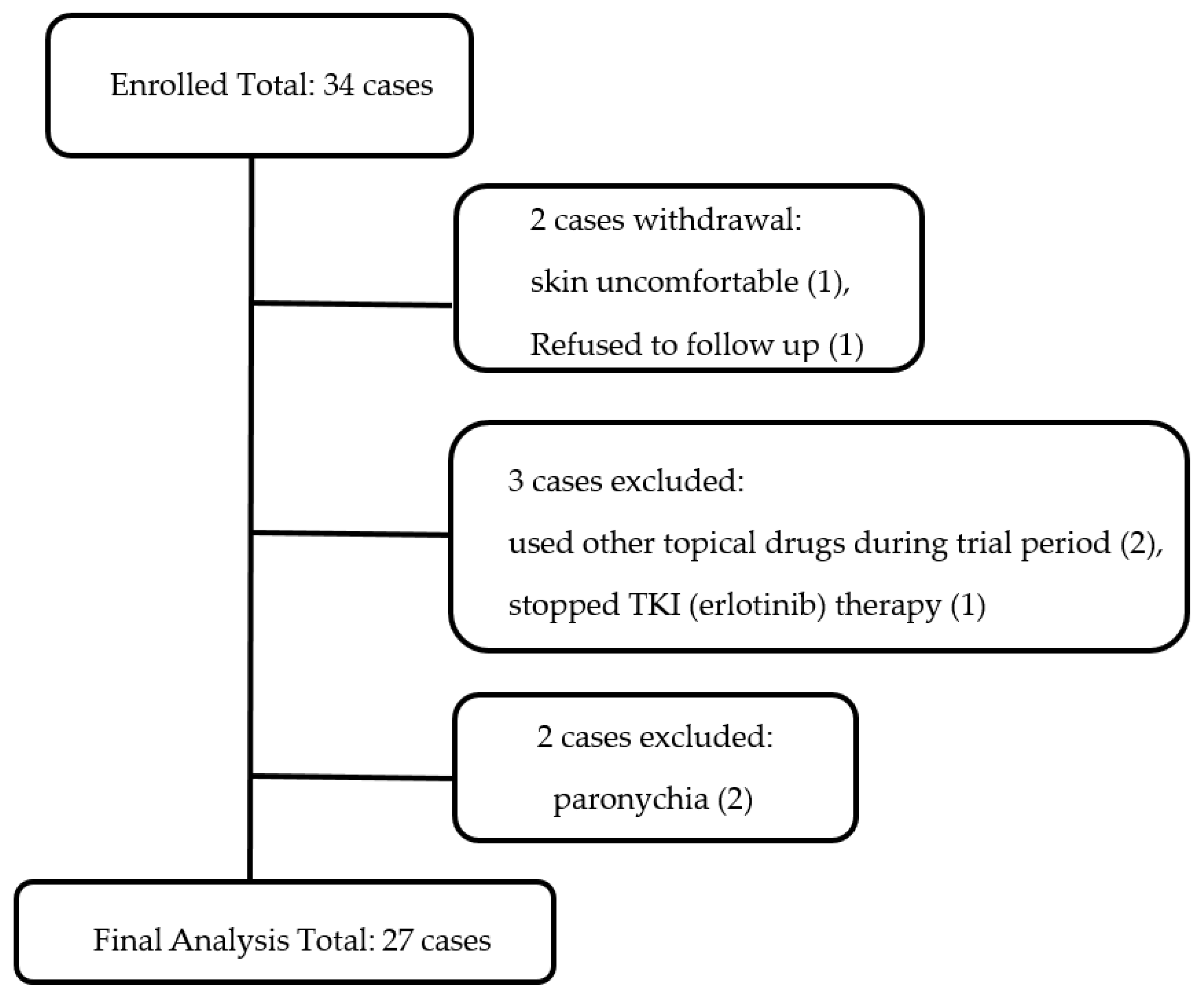
3.1. Patient Participation Status
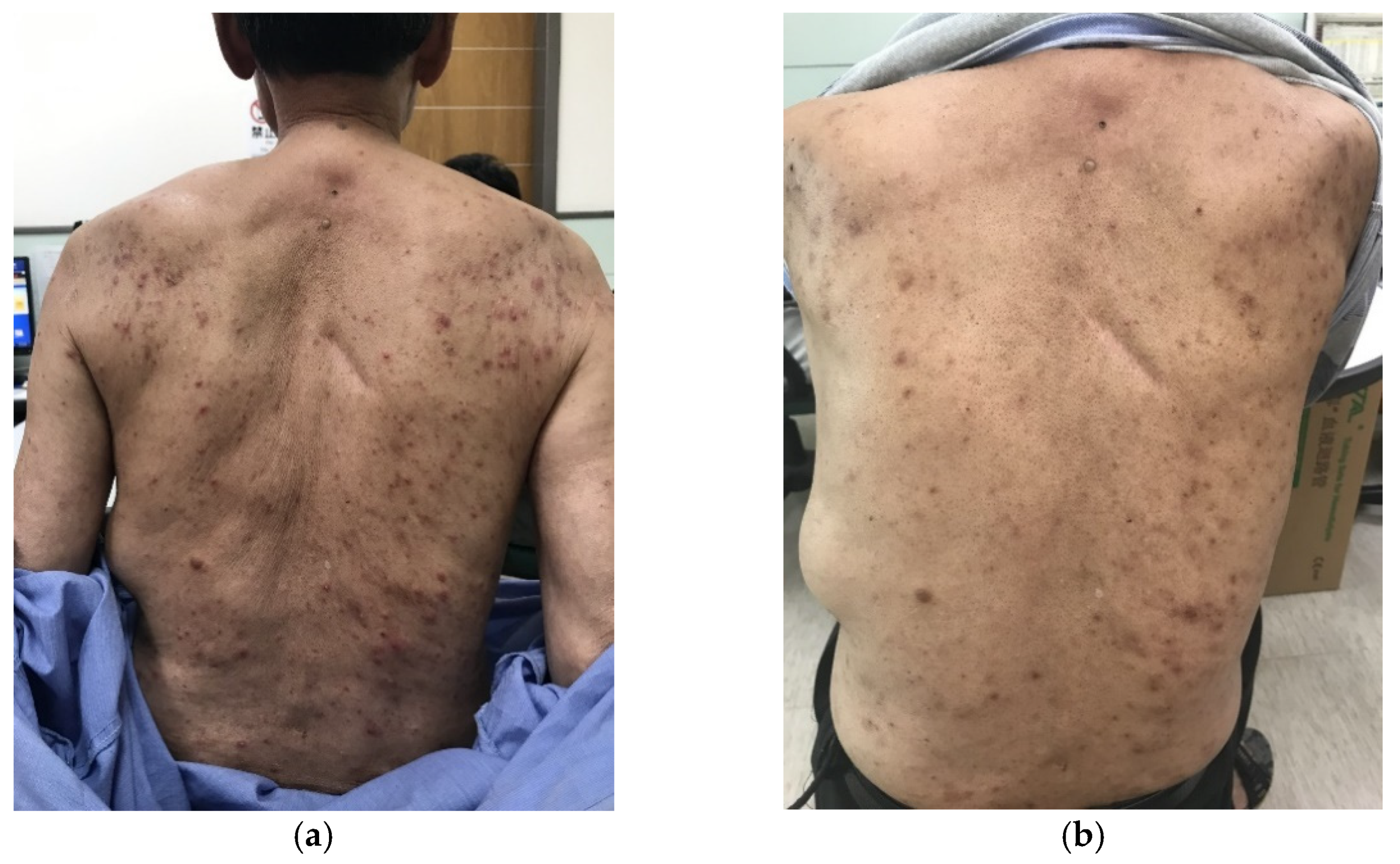
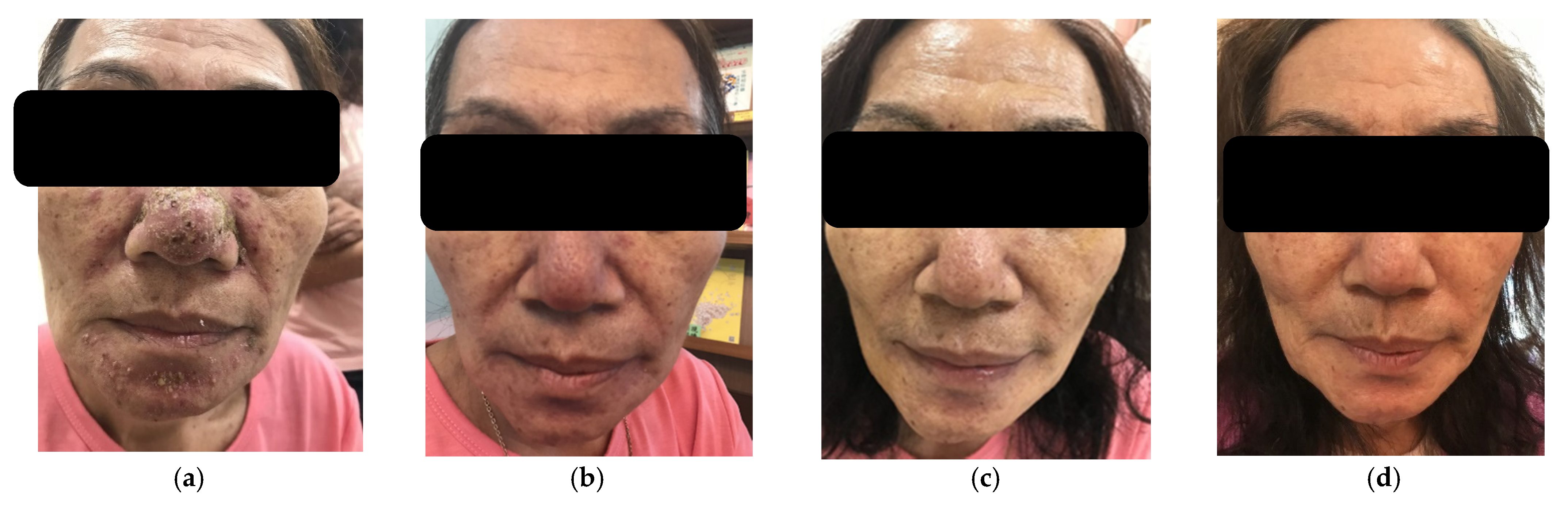
3.2. mHLJD Decoction Cream Significantly Decreased the Grades of Rash Acneiform
3.3. mHLJD Decoction Cream Significantly Decreased the Grades of Dry Skin
3.4. Safety of mHLJD Decoction Cream in This Trial
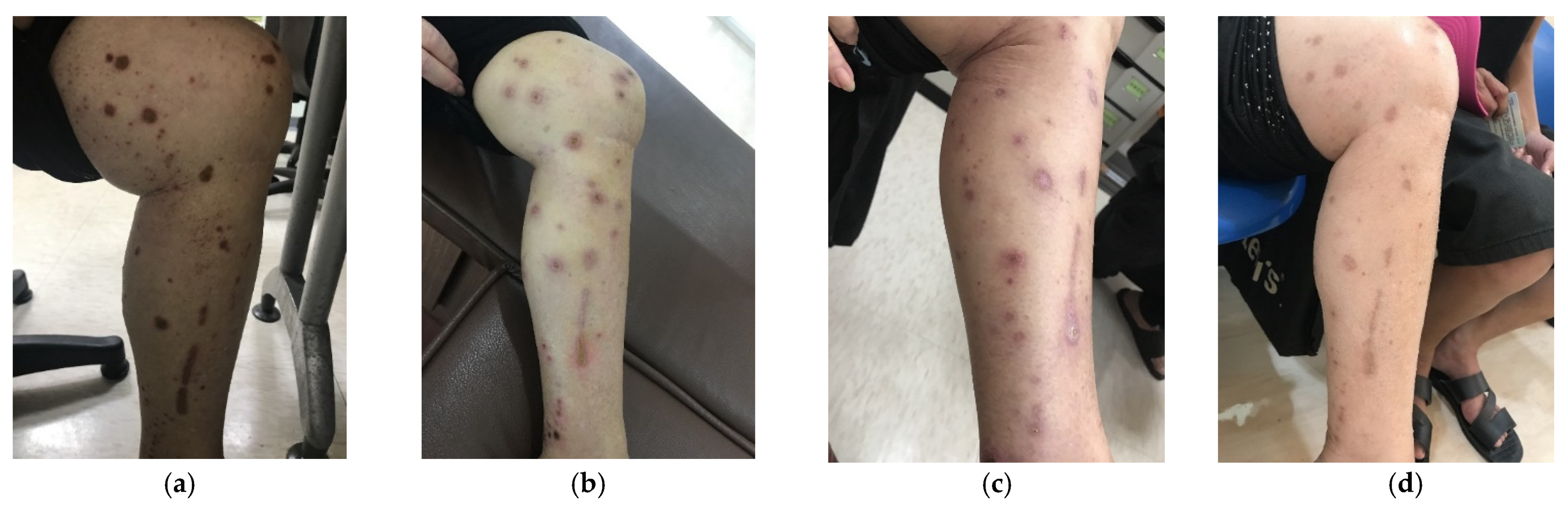
3.5. mHLJD Decoction Cream Significantly Decreased the Grades of Rash Acneiform in Three Cases
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fabbrocini, G.; Panariello, L.; Caro, G.; Cacciapuoti, S. Acneiform Rash Induced by EGFR Inhibitors: Review of the Literature and New Insights. Skin Appendage Disord 2015, 1, 31–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lacouture, M.E.; Anadkat, M.J.; Bensadoun, R.J.; Bryce, J.; Chan, A.; Epstein, J.B.; Eaby-Sandy, B.; Murphy, B.A.; Group, M.S.T.S. Clinical practice guidelines for the prevention and treatment of EGFR inhibitor-associated dermatologic toxicities. Support Care Cancer 2011, 19, 1079–1095. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kozuki, T. Skin problems and EGFR-tyrosine kinase inhibitor. Jpn. J. Clin. Oncol. 2016, 46, 291–298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, Z.; Dee, E.C.; Bach, D.Q.; Mostaghimi, A.; LeBoeuf, N.R. Evaluation of a Comprehensive Skin Toxicity Program for Patients Treated With Epidermal Growth Factor Receptor Inhibitors at a Cancer Treatment Center. JAMA Dermatol. 2020, 156, 1079–1085. [Google Scholar] [CrossRef]
- Chanprapaph, K.; Vachiramon, V.; Rattanakaemakorn, P. Epidermal growth factor receptor inhibitors: A review of cutaneous adverse events and management. Dermatol. Res. Pract. 2014, 2014, 734249. [Google Scholar] [CrossRef] [Green Version]
- Hung, Y.C.; Chin, C.Y.; Lee, Y.C.; Chen, Y.H.; Tsai, M.Y. Clinical experience of chinese herbal medicine ameliorates dermatologic events from epidermal growth factor receptor inhibitors for lung cancer: A case series. Explore 2019, 15, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.J.; Zhang, H.B.; Liu, L.R.; Liu, Y.H.; Zhang, F.L.; Bai, J.P.; Li, Y.; Qu, Y.C.; Qu, X.; Chen, X.; et al. Yin-Cold or Yang-Heat Syndrome Type of Traditional Chinese Medicine Was Associated with the Epidermal Growth Factor Receptor Gene Status in Non-Small Cell Lung Cancer Patients: Confirmation of a TCM Concept. Evid.-Based Complement. Altern. Med. 2017, 2017, 7063859. [Google Scholar] [CrossRef] [Green Version]
- Hu, Y.; Hu, Z.; Wang, S.; Dong, X.; Xiao, C.; Jiang, M.; Lv, A.; Zhang, W.; Liu, R. Protective effects of Huang-Lian-Jie-Du-Tang and its component group on collagen-induced arthritis in rats. J. Ethnopharmacol. 2013, 150, 1137–1144. [Google Scholar] [CrossRef]
- Wu, Y.H.; Chuang, S.Y.; Hong, W.C.; Lai, Y.J.; Chang, Y.L.; Pang, J.H. In vivo and in vitro inhibitory effects of a traditional Chinese formulation on LPS-stimulated leukocyte-endothelial cell adhesion and VCAM-1 gene expression. J. Ethnopharmacol. 2012, 140, 55–63. [Google Scholar] [CrossRef]
- Yue, G.H.; Zhuo, S.Y.; Xia, M.; Zhang, Z.; Gao, Y.W.; Luo, Y. Effect of huanglian jiedu decoction on thoracic aorta gene expression in spontaneous hypertensive rats. Evid. Based Complement. Alterna. Med. 2014, 2014, 565784. [Google Scholar] [CrossRef]
- Lu, Z.; Xiong, W.; Xiao, S.; Lin, Y.; Yu, K.; Yue, G.; Liu, Q.; Li, F.; Liang, J. Huanglian Jiedu Decoction ameliorates DSS-induced colitis in mice via the JAK2/STAT3 signalling pathway. Chin. Med. 2020, 15, 45. [Google Scholar] [CrossRef]
- Fan, H.J.; Zhao, X.S.; Tan, Z.B.; Liu, B.; Xu, H.L.; Wu, Y.T.; Xie, L.P.; Bi, Y.M.; Lai, Y.G.; Liang, H.F.; et al. Effects and mechanism of action of Huang-Lian-Jie-Du-Tang in atopic dermatitis-like skin dysfunction in vivo and in vitro. J. Ethnopharmacol. 2019, 240, 111937. [Google Scholar] [CrossRef]
- Chen, Y.; Xian, Y.; Lai, Z.; Loo, S.; Chan, W.Y.; Lin, Z.X. Anti-inflammatory and anti-allergic effects and underlying mechanisms of Huang-Lian-Jie-Du extract: Implication for atopic dermatitis treatment. J. Ethnopharmacol. 2016, 185, 41–52. [Google Scholar] [CrossRef]
- Kim, S.; Kim, Y.; Kim, J.E.; Cho, K.H.; Chung, J.H. Berberine inhibits TPA-induced MMP-9 and IL-6 expression in normal human keratinocytes. Phytomedicine 2008, 15, 340–347. [Google Scholar] [CrossRef]
- Lee, J.W.; Kang, Y.J.; Choi, H.K.; Yoon, Y.G. Fractionated Coptis chinensis Extract and Its Bioactive Component Suppress Propionibacterium acnes-Stimulated Inflammation in Human Keratinocytes. J. Microbiol. Biotechnol. 2018, 28, 839–848. [Google Scholar] [CrossRef] [Green Version]
- Jung, M.A.; Jang, S.E.; Hong, S.W.; Hana, M.J.; Kim, D.H. The role of intestinal microflora in anti-inflammatory effect of baicalin in mice. Biomol. Ther. 2012, 20, 36–42. [Google Scholar] [CrossRef] [Green Version]
- Ma, G.Z.; Liu, C.H.; Wei, B.; Qiao, J.; Lu, T.; Wei, H.C.; Chen, H.D.; He, C.D. Baicalein inhibits DMBA/TPA-induced skin tumorigenesis in mice by modulating proliferation, apoptosis, and inflammation. Inflammation 2013, 36, 457–467. [Google Scholar] [CrossRef]
- Chi, Y.S.; Kim, H.P. Suppression of cyclooxygenase-2 expression of skin fibroblasts by wogonin, a plant flavone from Scutellaria radix. Prostaglandins Leukot. Essent. Fatty Acids 2005, 72, 59–66. [Google Scholar] [CrossRef]
- Deng, R.; Li, F.; Wu, H.; Wang, W.Y.; Dai, L.; Zhang, Z.R.; Fu, J. Anti-inflammatory Mechanism of Geniposide: Inhibiting the Hyperpermeability of Fibroblast-Like Synoviocytes via the RhoA/p38MAPK/NF-kappaB/F-Actin Signal Pathway. Front. Pharmacol. 2018, 9, 105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, X.; Zhang, W.; Wang, T.; Jiang, H.; Zhang, Z.; Fu, Y.; Yang, Z.; Cao, Y.; Zhang, N. Geniposide plays an anti-inflammatory role via regulating TLR4 and downstream signaling pathways in lipopolysaccharide-induced mastitis in mice. Inflammation 2014, 37, 1588–1598. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Li, L.; Li, H.; Zhu, Z.; Hua, L.; Lei, F.; Kheir, M.M.; Du, L. Transdermal permeation of geniposide in the herbal complex liniment in vivo and in vitro. Int. J. Pharm. 2010, 392, 72–77. [Google Scholar] [CrossRef]
- Chu, M.; Zhang, M.B.; Liu, Y.C.; Kang, J.R.; Chu, Z.Y.; Yin, K.L.; Ding, L.Y.; Ding, R.; Xiao, R.X.; Yin, Y.N.; et al. Role of Berberine in the Treatment of Methicillin-Resistant Staphylococcus aureus Infections. Sci. Rep. 2016, 6, 24748. [Google Scholar] [CrossRef] [Green Version]
- More, N.V.; Kharat, K.R.; Kharat, A.S. Berberine from Argemone mexicana L exhibits a broadspectrum antibacterial activity. Acta Biochim. Pol. 2017, 64, 653–660. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cury-Martins, J.; Eris, A.P.M.; Abdalla, C.M.Z.; Silva, G.B.; de Moura, V.P.T.; Sanches, J.A. Management of dermatologic adverse events from cancer therapies: Recommendations of an expert panel. An. Bras. Dermatol. 2020, 95, 221–237. [Google Scholar] [CrossRef]
- Shmueli, E.S.; Geva, R.; Yarom, N.; Hubert, A.; Keynan, R.; Kedem, T.H.; Eini, M.; Tamarkin, D.; Shirvan, M. Topical doxycycline foam 4% for prophylactic management of epidermal growth factor receptor inhibitor skin toxicity: An exploratory phase 2, randomized, double-blind clinical study. Support. Care Cancer 2019, 27, 3027–3033. [Google Scholar] [CrossRef] [PubMed]
- Vaccaro, M.; Guarneri, F.; Borgia, F.; Pollicino, A.; Altavilla, G.; Cannavò, S.P. Efficacy, tolerability and impact on quality of life of clindamycin phosphate and benzoyl peroxide for the treatment of cetuximab-associated acneiform eruption in patients with metastatic colorectal cancer. J. Dermatol. Treat. 2016, 27, 148–152. [Google Scholar] [CrossRef] [PubMed]
- Holcmann, M.; Sibilia, M. Mechanisms underlying skin disorders induced by EGFR inhibitors. Mol. Cell Oncol. 2015, 2, e1004969. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shafritz, A.B.; Coppage, J.M. Acute and chronic paronychia of the hand. J. Am. Acad. Orthop. Surg. 2014, 22, 165–174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, J.; Wang, J.; Yang, C.; Zhu, C.; Guo, G.; Tang, J.; Shen, H. Antimicrobial characteristics of Berberine against prosthetic joint infection-related Staphylococcus aureus of different multi-locus sequence types. BMC Complement. Altern. Med. 2019, 19, 218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whitehead, S.M.; Eykyn, S.J.; Phillips, I. Anaerobic paronychia. Br. J. Surg. 1981, 68, 420–422. [Google Scholar] [CrossRef]
- Rockwell, P.G. Acute and chronic paronychia. Am. Fam. Physician 2001, 63, 1113–1116. [Google Scholar]
| No. | Ingredients | % (w/w) | Manufacturer | City | Country |
|---|---|---|---|---|---|
| 1 | Pure water | 25.345 | (not applicable) | (not applicable) | (not applicable) |
| 2 | Glycerin | 2.00 | P&G Chemicals | Cincinnati | USA |
| 3 | Butylene glycol | 2.00 | Oxea Chemical | Dallas | USA |
| 4 | Sodium alginate | 1.00 | Bright Moon Seaweed | Qingdao | China |
| 5 | Acetamidoethoxyethanol | 2.00 | Spiga Nord | Carasco | Italy |
| 6 | Methylparaben | 0.20 | Clariant Produkte GmbH | Frankfurt am Main | Germany |
| 7 | Sclerotium gum | 0.60 | Even Biochemical | Guangzhou | China |
| 8 | Polyglyceryl-3 stearate | 3.00 | Oleon | Evergem | Belgium |
| 9 | Glyceryl stearate citrate | 2.00 | Oleon | Evergem | Belgium |
| 10 | Potassium cetyl phosphate | 1.00 | DSM Fine Chemicals | Heerlen | Netherlands |
| 11 | Behenyl alcohol | 2.00 | Cognis Japan Ltd. | Tokyo | Japan |
| 12 | Stearyl alcohol | 2.00 | Cognis Oleochemicals (M) Sdn Bhd | Teluk Panglima Garang | Malaysia |
| 13 | Stearic acid | 1.00 | Pacific Oleochemicals | Pasir Gudang | Malaysia |
| 14 | Isopropyl isostearate | 6.00 | Oleon | Evergem | Belgium |
| 15 | Isostearic acid | 3.00 | Oleon | Evergem | Belgium |
| 16 | Octyldodecanol | 1.00 | BASF SE | Ludwigshafen | Germany |
| 17 | Caprylic/Capric triglyceride | 2.00 | Paim-OLEO/Selangor | Selangor | Malaysia |
| 18 | Jojoba oil | 3.00 | Eco Oil Argentina S.A. | Buenos Aires | Argentina |
| 19 | Macadamia nut oil | 3.00 | Arista | Wilton | USA |
| 20 | Vitamin E | 0.50 | DSM Nutritional Products | Kaiseraugst | Switzerland |
| 21 | Isododecane | 1.00 | LANXESS GmbH | Cologne | Germany |
| 22 | Dimethicone | 1.00 | Dow Corning | Midland | USA |
| 23 | Phenoxyethanol | 0.25 | Clariant Produkte GmbH | Frankfurt am Main | Germany |
| 24 | Octopirox | 0.005 | Hoechst Aktiengesellschaft | Frankfurt am Main | Germany |
| 25 | Proprylene paraben | 0.10 | Clariant Produkte GmbH | Frankfurt am Main | Germany |
| 26 | mHLJD decoction | 35.0 | (not applicable) | (not applicable) | (not applicable) |
| Total | 100 | ||||
| Grading of Skin Side Effect | EGFRI/TKI Drugs | mHLJD Decoction Cream |
|---|---|---|
| Grade 1 | Original dose | Keep treatment |
| Grade 2 | Original dose | Keep treatment |
| Grade 3, tolerable side effect | Original dose | Keep treatment, stop if no improvement within 7 days |
| Grade 3, intolerable side effect | Stop for one week or reduce dose | Keep treatment, stop if no improvement within 7 days |
| Grade 4 | Stop treatment | Keep treatment, stop if no improvement within 3 days |
| Characteristic, n (%) | Total Number (n = 27) | Previous Use of Medications for Skin Side Effects | p Value | |
|---|---|---|---|---|
| No (n = 16) | Yes (n = 11) | |||
| Sex | ||||
| Male | 12 (44.4%) | 8 (50.0%) | 4 (36.4%) | 0.696 |
| Female | 15 (55.6%) | 8 (50.0%) | 7 (63.6%) | |
| Age, mean (SD) | 59.1 (10.7) | 58.4 (10.8) | 60.1 (11.1) | 0.716 |
| <65 | 19 | 12 (75.0%) | 7 (63.6%) | 0.675 |
| >/=65 | 8 | 4 (25.0%) | 4 (36.4%) | |
| Period, medium (IQR) | 71 (195) | 18.5 (21.8) | 222 (932) | <0.001 |
| Drugs | ||||
| EGFRIs (cetuximab/panitumumab) | 7 (25.9%) (6/1) | 6 (37.5%) | 1 (9.1%) | 0.183 |
| TKIs (gefitinib/erlotinib/afatinib) | 20 (74.1%) (4/9/7) | 10 (62.5%) | 10 (90.9%) | |
| Rash Acneiform | Dry Skin | Scalp Pain | Pain of Skin | Pruritus | Palmar-Plantar Erythrodysestheisa | Skin Hyperpigmentation | |
|---|---|---|---|---|---|---|---|
| Number * | 26 | 7 | 2 | 2 | 2 | 1 | 1 |
| Percentage | 96.30% | 25.93% | 7.41% | 7.41% | 7.41% | 3.70% | 3.70% |
| Most Severe Grade | 3 | 2 | 3 | 2 | 2 | 1 | 1 |
| Number | Mean | SD | Medium | IQR | p Value | |
|---|---|---|---|---|---|---|
| Week 0 | 26 | 2.19 | 0.69 | 2.00 | 1.00 | -- |
| Week 2 | 26 | 1.27 | 0.83 | 1.00 | 1.00 | <0.001 |
| Week 4 | 26 | 0.88 | 0.65 | 1.00 | 1.00 | <0.001 |
| Week 6 | 22 | 0.68 | 0.65 | 1.00 | 1.00 | <0.001 |
| Week 8 | 20 | 0.55 | 0.69 | 0.00 | 1.00 | <0.001 |
| Week 10 | 19 | 0.37 | 0.50 | 0.00 | 1.00 | <0.001 |
| Number | Mean | SD | Medium | IQR | p Value | |
|---|---|---|---|---|---|---|
| Week 0 | 16 | 2.25 | 0.68 | 2.00 | 1.00 | -- |
| Week 2 | 16 | 1.31 | 0.79 | 1.00 | 1.00 | 0.002 |
| Week 4 | 16 | 0.81 | 0.66 | 1.00 | 1.00 | <0.001 |
| Week 6 | 12 | 0.67 | 0.78 | 0.50 | 1.00 | 0.002 |
| Week 8 | 11 | 0.55 | 0.82 | 0.00 | 1.00 | 0.003 |
| Week 10 | 11 | 0.27 | 0.45 | 0.00 | 1.00 | 0.002 |
| Number | Mean | SD | Medium | IQR | p Value | |
|---|---|---|---|---|---|---|
| Week 0 | 10 | 2.10 | 0.74 | 2.00 | 1.25 | -- |
| Week 2 | 10 | 1.20 | 0.92 | 1.00 | 1.25 | 0.014 |
| Week 4 | 10 | 1.00 | 0.67 | 1.00 | 0.50 | 0.005 |
| Week 6 | 10 | 0.70 | 0.48 | 1.00 | 1.00 | 0.006 |
| Week 8 | 9 | 0.56 | 0.53 | 1.00 | 1.00 | 0.006 |
| Week 10 | 8 | 0.50 | 0.54 | 0.50 | 1.00 | 0.010 |
| Number | Mean | SD | Medium | IQR | p Value | |
|---|---|---|---|---|---|---|
| Week 0 | 7 | 1.57 | 0.54 | 2.00 | 1.00 | -- |
| Week 2 | 7 | 1.14 | 0.69 | 1.00 | 1.00 | 0.180 |
| Week 4 | 7 | 0.71 | 0.49 | 1.00 | 1.00 | 0.034 |
| Week 6 | 6 | 0.67 | 0.52 | 1.00 | 1.00 | 0.034 |
| Week 8 | 5 | 0.80 | 0.45 | 1.00 | 0.50 | 0.059 |
| Week 10 | 5 | 0.80 | 0.45 | 1.00 | 0.50 | 0.059 |
| Number | Mean | SD | Medium | IQR | p Value | |
|---|---|---|---|---|---|---|
| Week 0 | 4 | 1.57 | 0.50 | 2.00 | 0.75 | -- |
| Week 2 | 4 | 1.00 | 0.82 | 1.00 | 1.50 | 0.180 |
| Week 4 | 4 | 0.75 | 0.50 | 1.00 | 0.75 | 0.102 |
| Week 6 | 3 | 0.67 | 0.58 | 1.00 | -- | 0.102 |
| Week 8 | 3 | 0.67 | 0.58 | 1.00 | -- | 0.102 |
| Week 10 | 3 | 0.67 | 0.58 | 1.00 | -- | 0.102 |
| Number | Mean | SD | Medium | IQR | p Value | |
|---|---|---|---|---|---|---|
| Week 0 | 3 | 1.33 | 0.58 | 1.00 | -- | -- |
| Week 2 | 3 | 1.33 | 0.58 | 1.00 | -- | >0.999 |
| Week 4 | 3 | 0.67 | 0.58 | 1.00 | -- | 0.157 |
| Week 6 | 3 | 0.67 | 0.58 | 1.00 | -- | 0.157 |
| Week 8 | 2 | 1.00 | 0.00 | 1.00 | -- | 0.317 |
| Week 10 | 2 | 1.00 | 0.00 | 1.00 | -- | 0.317 |
| Chinese Name | Latin Name | Major Ingredients |
|---|---|---|
| Huanglian | Coptidis Rhizoma | berberine |
| Huangbo | Phellodendri chinensis Cortex | berberine |
| Huangqin | Scutellariae Radix | baicalin, baicalein, wogonin |
| Zhizi | Gardenia jasminoides Ellis | geniposide |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, M.-Y.; Lin, M.-Y.; Chang, Y.-J.; Tseng, Y.-T.; Huang, I.-A.; Huang, W.-T.; Liu, Y.-W. Efficacy and Safety of Modified Huang-Lian-Jie-Du Decoction Cream on Cancer Patients with Skin Side Effects Caused by EGFR Inhibition. Processes 2021, 9, 1081. https://doi.org/10.3390/pr9071081
Lee M-Y, Lin M-Y, Chang Y-J, Tseng Y-T, Huang I-A, Huang W-T, Liu Y-W. Efficacy and Safety of Modified Huang-Lian-Jie-Du Decoction Cream on Cancer Patients with Skin Side Effects Caused by EGFR Inhibition. Processes. 2021; 9(7):1081. https://doi.org/10.3390/pr9071081
Chicago/Turabian StyleLee, Ming-Yang, Mei-Yi Lin, Yu-Ju Chang, Yu-Ting Tseng, I-An Huang, Wan-Ting Huang, and Yi-Wen Liu. 2021. "Efficacy and Safety of Modified Huang-Lian-Jie-Du Decoction Cream on Cancer Patients with Skin Side Effects Caused by EGFR Inhibition" Processes 9, no. 7: 1081. https://doi.org/10.3390/pr9071081
APA StyleLee, M.-Y., Lin, M.-Y., Chang, Y.-J., Tseng, Y.-T., Huang, I.-A., Huang, W.-T., & Liu, Y.-W. (2021). Efficacy and Safety of Modified Huang-Lian-Jie-Du Decoction Cream on Cancer Patients with Skin Side Effects Caused by EGFR Inhibition. Processes, 9(7), 1081. https://doi.org/10.3390/pr9071081







