Abstract
Purpose: The purpose of this in vivo study was to investigate whether the less invasive approach (reduced thickness of the restoration) will result in a comparable risk of failure and similar aesthetic results, compared to conventional layered full porcelain crowns, and can, therefore, be used as a good alternative. Material and Methods: The tested ceramic was lithium-disilicate ceramic (IPS e.max). Forty-four patients with endodontically treated premolars or molars were randomized into two groups and provided with single crowns. One group received conventional all-ceramic crowns made from a lithium-disilicate core and hand-veneered aesthetic ceramic, while another group received full-contoured lithium-disilicate ceramic crowns with reduced wall thickness than manufactures recommendations. The teeth for conventional crowns were prepared with 1 mm rounded shoulder and 2 mm occlusal reduction, while teeth for monolithic crowns were prepared with 0.6 mm wide rounded shoulder and 1 mm occlusal reduction. All crowns were prepared by the same clinician and manufactured in the same laboratory by the same technician. The survival and aesthetics of the crowns were assessed by the independent clinician. Apart from this, patients’ aesthetic satisfaction was evaluated. The assessment was double blind as both the examiner and the patients did not know which type of crown was provided. The observation period was 36 months. Survival of the crowns was assessed using the modified United States Public Health Service (USPHS) criteria and aesthetics and participants’ aesthetic satisfaction with the crowns was evaluated using a visual analogue scale. Results: The one-year survival rate for layered crowns was 100% and for monolithic crowns 95.5%. The median patients’ aesthetic satisfaction with both crowns was 100%. Conclusions: The results indicate similar one-year survival rate of reduced-thickness monolithic lithium-disilicate crowns and conventional veneered crowns. Differences with patients’ satisfaction with the aesthetics of both crowns were not statistically significant and it can be said that the patients’ aesthetic satisfaction was the same for both crowns.
Keywords:
lithium-disilicate ceramic; IPS e.max; monolithic; veneered; CAD/CAM; reduced-thickness; survival; aesthetics 1. Introduction
Endodontic treatment causes weakening of the tooth. As most of these teeth have already lost some tooth structure due to caries, fractures or previous restorations, restoring of these teeth should ensure functional stability and long-term survival. This is particularly the situation with posterior teeth, which must be able to withstand great occlusal forces during mastication.
Crown coverage increases survival of root canal treated (RCT) teeth for six times [1,2,3]. Eckerbom et al. [4] showed that crowned RCT teeth have a similar risk of failure as the vital ones. Besides only cuspal coverage, good occlusal design of the restoration is very important to ensure axial force distribution and minimize the amount of non-axial forces [5]. As the remaining tooth structure plays the major role in structural integrity and survival of pulpless teeth, sufficient tooth structure excludes the need for post placement [6].
In cases where we have severe destruction of clinical crown, lack of enamel or cervical defect, the crowning of these teeth would be the best option. Apart from this, when the majority of clinical crown is intact and we have enough enamel, minimally invasive onlay, overlay or endocrown restoration can also be the choice of therapy.
Lithium-disilicate ceramic was introduced in 1998 as IPS Empress 2 (Ivoclar, Vivadent). It consisted of a glass matrix filled with micron-sized lithium-disilicate crystals and submicron lithium orthophosphate crystals dispersed between them [7]. Lithium-disilicate crystals constituted about 70% of the volume. Empress 2 had good aesthetic and mechanical characteristics but due to low translucency, it was only used as a core material on which the veneering ceramic was applied. Later on, IPS e.max lithium-disilicate ceramic was introduced. It has the same chemical base of Empress 2 but better mechanical properties and translucency due to a different firing procedure during laboratory processing [7]. Besides its use as a core material, excellent optical properties allow its use for monolithic, full-contoured restorations.
IPS e.max lithium-disilicate ceramic is available in two forms: e.max Press for the lost-wax hot pressing technique; and e.max CAD for the CAD/CAM milling technique. Pressable e.max comes in the form of fully crystalized ingots containing approximately 70% lithium-disilicate crystals and flexural strength of about 400 MPa. Machinable (CAD/CAM) e.max comes in blocks that are partially crystalized. It consists of approximately 40% lithium-metasilicate crystals in a glassy phase and has flexural strength of 130 MPa. Blocks like this are blue and quite soft, which allows easy milling without excessive wear of bur and possible damage of the material. After try-in procedure, the blue restorations are fired to get full crystallization with transformation of lithium-metasilicate to lithium-disilicate, and final strength and shade of ceramic. Fully crystalized e.max CAD also consists of 70% lithium-disilicate crystals in a glassy matrix, with flexural strength of 360 MPa [8,9].
Both systems, press and CAD/CAM, can be used for conventional veneered or fully anatomic crowns. In addition, both ingots and CAD blocks are industrially produced in a reproducible manner, which prevents formation of defects, possible in hand mixing veneering ceramic, and leads to dense, high-quality material free of pores [8,10,11].
Veneered crowns are made from the lithium-disilicate as a base (core) on which the aesthetic, but weak, veneering ceramic is applied. The technique is called the layering technique. Due to the multi-layering technique, the unique combination of opalescence, brightness and translucency ensures the superb aesthetic, and a natural-looking appearance can be achieved. On the other hand, a monolithic crown is fully anatomic and is fully made from the same material. As the whole crown is made from lithium-disilicate ceramic, the use of weaker veneer ceramic is excluded, thus minimizing the possibility of chipping or delamination. This was confirmed in different laboratory studies where a monolithic IPS e.max lithium-disilicate crown showed superior fracture resistance behavior and reliability compared to a veneered IPS e.max lithium-disilicate crown [12] and a veneered zirconia all-ceramic crown [11,13]. This high reliability was also confirmed in clinical studies where monolithic IPS e.max lithium-disilicate crowns achieved a success rate of more than 96% after two and four years [9,14,15].
Monolithic e.max lithium-disilicate restorations can be produced with either the press or CAD/CAM technique. If the press technique is used, the crown becomes fully crystallized after firing, and if needed, it can be stained to get a better aesthetic. If the milling technique is used, partially crystallized blue blocks are milled and tried in the mouth, and, if needed, adjustments made. The restoration is stained and then finally fired to fully crystallize the restoration. The advantage of e.max CAD over press is the possibility for chairside production. It allows fitting of the final restoration at the same appointment the teeth are prepared.
As RCT teeth already have impaired structural integrity due to access preparation, it is desirable that any further preparation preserves as much remaining tooth as possible. Conventional veneered all-ceramic crowns require an occlusal reduction of 1.5–2 mm and axial reduction of 1.2–1.5 mm with addition of 0.8–1 mm heavy chamfer of shoulder [16,17,18]. Preparation like this removes the majority of hard tooth structure leaving structurally weakened tooth, with residual dentine thickness of less than 1.5 mm [19].
This study was planned as a prospective, randomized, controlled clinical trial. The aim of this study is to examine whether a thinner porcelain crown (full-contoured lithium-disilicate ceramic crown) can provide a satisfactory aesthetic result, assessed by the patient, together with a good survival rate compared to conventional all-ceramic crowns made from a lithium-disilicate core and hand-veneered aesthetic ceramic. The null hypothesis for this study was that there is significant difference in the aesthetics and survival rate between thinner monolithic IPS e.max CAD and veneered IPS e-max CAD single posterior crowns.
2. Materials and Methods
The research protocol was approved by the Ethical Committee of the School of Dentistry, University of Zagreb, Croatia. Conventional all-ceramic crowns made from hand-veneered IPS e.max PRESS (Ivoclar Vivadent, Schaan, Lichtenstein) lithium-disilicate core were compared to reduced-thickness full-contoured monolithic IPS e.max CAD (Ivoclar Vivadent, Schaan, Lichtenstein) lithium-disilicate crowns. Participants for the study were selected among patients attending general dental practice (GDP) in Bjelovar and Zagreb, Croatia. The screening and examination processes were performed by the same clinician (operator) who provided treatment for selected patients. The operator was well trained for providing the determined treatment and experienced in all kinds of prosthodontics procedures. All patients attending the named GDP were screened according to determined inclusion and exclusion criteria (Table 1 and Table 2). Apart from this, patients’ dental history was examined. The duration of the study was 36 months (three years) with regular recalls every six months. The patients were recruited and treated as soon as they were identified and did not wait until the full sample was identified.

Table 1.
Inclusion criteria.

Table 2.
Exclusion Criteria.
Using OpenEpi statistical software, the number of participants needed for each group was determined to be 22. Using computer software, the participants were randomized into two groups and each participant was assigned an identification number. Each patient was provided with only one crown. If a participant had more than one eligible tooth, the operator chose the tooth that fitted the inclusion criteria the best. With only one crown provided per participant, the possibility to compare two or more provided crowns and judge the aesthetics based on other ones was excluded. All crowns were prepared by the same clinician.
Before preparation, two silicon impressions were taken using putty material (EXA’lence®; GC, Tokyo, Japan). The first one was vertically sectioned and used as a silicon key to guide optimum axial and occlusal tooth preparation. The other impression was used for making direct temporary crowns. The teeth for veneered crowns were prepared with gingival finish line equigingival or supragingival, 1 mm wide rounded shoulder, 2 mm occlusal reduction, axial inclination approximately 10° and all angles rounded. The teeth for monolithic crowns were prepared the same way as for the veneered ones, except that for monolithic crowns, 0.6 mm wide rounded shoulder and 1 mm occlusal reduction was done.
Tooth preparation started with making depth-orientation groves on occlusal and buccal/lingual surfaces [18]. For veneered crowns, a rough 1.8 mm wide round-end fissure bur (Komet 6881.314.018; Brasseler, Lemgo, Germany) was used. For the monolithic crowns, rough 1.8 mm wide round-end fissure bur for occlusal surface and 1.2 mm wide round-end fissure bur (Komet 6881.314.012; Brasseler, Lemgo, Germany) for buccal/lingual surfaces was used. The amount of reduced tooth tissue was regularly controlled with the silicon key. According to the sulcus width, the appropriate cord size (000, 00, 0, 1) was selected (Ultrapak®; Ultradent Products, Inc., South Jordan, UT, USA), applying the single-cord technique. The teeth were polished using fine 1.8 mm wide round-end fissure bur (Komet 8881.314.018; Brasseler, Lemgo, Germany) for teeth crowned with veneered crown, and 1.2 mm wide round-end fissure bur (Komet 8881.314.012; Brasseler, Lemgo, Germany) for teeth provided with monolithic crown. With the cord in the sulcus, the impression was taken using vinyl polyether silicone material (EXA’lence®; GC, Tokyo, Japan), and two-phase technique. Bite registration was taken using thermoplastic material (Bite Compound®; GC, Tokyo, Japan). After tooth preparation, temporary crowns were made (Protemp 4®; 3M ESPE, Seefeld, Germany) and placed using eugenol-free temporary cement (Freegenol®; GC, Tokyo, Japan). Finally, the occlusion was checked and adjusted if needed.
The tooth shade was determined using VITA Easyshade Advance 4.0 (VITA Zahnfabrik, Bad Säckingen, Germany). In addition, the photography with Vita Linearguide 3D-MASTER (VITA Zahnfabrik, Bad Säckingen, Germany) was taken. The first adjacent tooth was used as a base for color determination. If the first adjacent tooth was not appropriate for shade determination, due to multiple fillings, heavy destruction or severe discoloration, the operator chose the tooth for color determination. The color of prepared tooth was also recorded.
All crowns were produced in the same laboratory by the same technician. The restorations were produced using the CAD/CAM system (Sirona Dental System GmbH, Bensheim, Germany). The impressions were casted using type 4 dental stone (Fujirock EP®; GC, Tokyo, Japan), and the die was prepared. The abutment teeth were scanned using an inEos X5 scanner (Sirona Dental System GmbH, Bensheim, Germany). With computer software (inLab SW 4.4; Sirona Dental System GmbH, Bensheim, Germany), the cores for the veneered crowns were designed on uniform thickness of 0.6 mm. Using the same software, the full monolithic crowns were designed with 0.6 marginal and 1 mm occlusal thickness. Partially crystallized lithium-disilicate blocks were milled using a CAD/CAM milling unit (inLab MC XL; Sirona Dental System GmbH, Bensheim, Germany).
Partially crystallized ceramic cores and monolithic crowns were tried in the mouth. The cores were evaluated regarding marginal seating. As the monolithic crowns were full-contoured, the marginal seating was checked as well as the occlusal and approximal contacts. The marginal seating of cores and monolithic crowns were assessed using a sharp dental probe under 3× magnification. Any necessary adjustments regarding occlusal or approximate contacts were made using a fine diamond bur.
After try-in, the crowns were sent back to the laboratory and finished. Monolithic crowns were manually stained and fired to achieve full crystallization. The cores were fired to achieve full crystallization and veneered with nano-fluorapatite ceramic (IPS e.max Ceram®; Ivoclar Vivadent, Schaan, Lichtenstein). The VITA Easyshade Advance 4.0 and Vita Linearguide 3D-MASTER (VITA Zahnfabrik, Bad Säckingen, Germany) were also used in the laboratory to check the color.
The final crowns were tried in the mouth. The occlusal contacts were checked in centric occlusion and lateral excursive movements using 8µm articulation foil (Articulating foil®; Interdent, Celje, Slovenia). Final adjustments regarding occlusion or approximal contacts were made. Both the clinician and technician evaluated the color and, if needed, recorded changes that should be made. The crowns that were adjusted were sent back to the laboratory and finished.
The final crowns were cemented using transparent dual-cure self-adhesive resin cement Variolink Esthetic DC (Ivoclar Vivadent, Schaan, Lichtenstein).
The baseline assessment was carried out one week after cementation. After baseline examination, regular follow-up appointments were conducted every six months. On each appointment, the same assessment protocol regarding technical performance of the crowns was done. The aesthetic evaluation was performed at the baseline assessment and patients’ satisfaction with the aesthetics at the baseline assessment and after one year.
Participants’ aesthetic satisfaction with the crowns was evaluated using a visual analogue scale. This assessment tool is simple to use. All participants receive the same questionnaire with 100 mm straight line and left and right end points. The left endpoint is rated as “Unsatisfied” and the right end point is rated as “Fully satisfied”. Participants are asked to mark the point on the line at the place they feel represents their aesthetic satisfaction with provided crowns. By measuring the distance from left to right the numeric value of patients’ satisfaction is obtained.
Survival of the crowns was assessed using the Modified United States Public Health Service (USPHS) criteria [20,21]. Restorations rated with Alfa or Beta in both categories are defined as a success, while restorations rated Charlie or Delta, in either category, are defined as a failure, and a replacement is needed.
The assessment was double blind as both the participants and the examiner did not know which type of crown was provided. As the intervention was the same for all participants (tooth preparation), they could not see any differences among them. The crowns were clinically examined using standardized diagnostic dental instruments under 3× magnification and all the findings were recorded.
Differences between study groups in clinical characteristics of crowns immediately after the cementation and after 12 months were performed by Fisher–Freeman–Halton’s exact test. The Mann–Whitney U test was used to analyze differences in patients’ aesthetic satisfaction in each time point, while the Wilcoxon test was used to analyze differences between two time points in each study group. The survival rate was calculated as the total percentage of success after 12 months for each study group with corresponding 95% confidence intervals (95% CI). All P values below 0.05 were considered significant. MedCalc® Statistical Software version 19.8 (MedCalc Software Ltd., Oostende, Belgium) was used for all statistical procedures.
3. Results
Differences between study groups in clinical characteristics of crowns immediately after the cementation are shown in Table 3. The only significance was noted in color where monolithic crowns showed more discoloration compared to the layered crowns (P < 0.001). After 12 months, initial difference in color remained—a significantly better result was in the layered crowns group (P < 0.001); B classification in the monolithic group was in 10 (47.6%), while in the layered crowns group, all samples were classified as A. In addition, the monolithic crowns group had more marginal discoloration after 12 months compared to the layered crowns group (Table 4). There were no significant differences in patients’ satisfaction with aesthetics of the crowns between study groups immediately and 12 months after the cementation. Median values of patients’ aesthetic satisfaction were 100.0% in both study groups (Table 5). Significant improvement was shown in both groups after 12 months with P values P = 0.020 and P = 0.019 respectively (Figure 1). Survival rate after 12 months for the layered crowns group was 100.0% (95% CI 84.6% to 100.0%), while in the monolithic group, it was 95.5% (95% CI 77.2% to 99.9%).

Table 3.
Differences between study groups in clinical characteristics of crowns immediately after the cementation.

Table 4.
Differences in clinical characteristics of crowns between study groups 12 months after cementation: Fisher–Freeman–Halton’s exact test.

Table 5.
Differences in patients’ aesthetic satisfaction between groups immediately and 12 months after the cementation: Mann–Whitney U test.
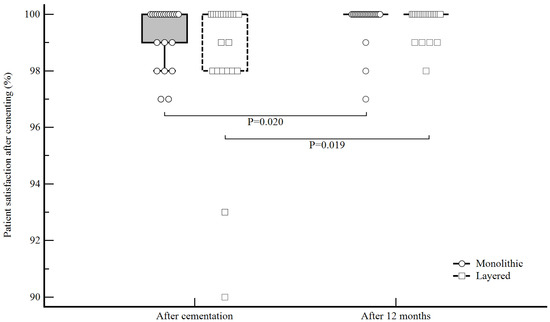
Figure 1.
Differences in patients’ aesthetic satisfaction score before and after 12 months for each group: Wilcoxon test.
4. Discussion
The results of this study support the rejection of null hypothesis. First, there is no significant difference in aesthetics between thinner monolithic IPS e.max and veneered IPS e.max crowns as median values of patients’ satisfaction with aesthetics of both groups were the same. Second, the difference in survival rate between thinner monolithic crowns and veneered crowns is not statistically significant and, therefore, survival of monolithic crowns is comparable to veneered ones.
Up to date, there are no reported studies about clinical survival of monolithic lithium-disilicate crowns with a reduced thickness to the manufacturers’ recommendations, nor that compare the reliability of reduced-thickness monolithic with veneered lithium-disilicate crowns. Previous laboratory studies have shown great fracture resistance of reduced-thickness monolithic IPS e.max lithium-disilicate crowns [13,22]. The results of the study show high values of single-load-to-fracture (SLF) for monolithic crowns with 1 mm occlusal thickness and fracture resistance higher than those of veneered zirconia-based crowns and comparable to those of metal-ceramic [13]. In another laboratory study, fracture resistance of monolithic IPS e.max CAD crowns with 1 mm wall thickness show similar results for crowns with wall thickness of 1 and 1.5 mm, and the differences in loads to failure were not significant. Ageing also did not significantly influence the fracture resistance [22]. Unlike these two studies that show high fracture resistance of monolithic IPS e.max crowns, a laboratory study by Noor et al. shows a significant decrease in fracture resistance for reduced-thickness e.max CAD crowns [23].
Apart from this, two in vitro studies tested the influence of ceramic thickness on the fracture resistance of ultrathin occlusal lithium-disilicate veneers. The results show that occlusal thickness of 0.7–1 mm is suggested and survived cyclic loading without damage [24], while another study shows high fracture strength under cyclic loading for even thinner occlusal IPS e.max CAD veneers with only 0.3/0.5 mm fissure/cusp thickness [25].
The results of this study are in correlation with the results of previous laboratory studies where monolithic crowns with wall thickness of 1 mm or smaller show great fracture resistance. After one year, one monolithic crown fractured, while all others showed no ceramic fracture or ceramic chipping. The fracture line was noticed on the occlusal surface and the crown was replaced with the new crown, and the patient was excluded from the study.
Regarding the survival rate of classic monolithic crowns, the current results are in correspondence with previous clinical studies regarding clinical performance of monolithic IPS e.max lithium-disilicate crowns. Two to ten years survival rate ranged from 96% to 100% [7,9,14,15,26,27]. Laboratory studies regarding fracture resistance of both monolithic and veneered lithium-disilicate crowns also showed high probability of survival [28,29]. On the other hand, the survival rate of tested veneered crowns is also comparable to those of previous clinical studies [26,30].
Furthermore, as the thickness of ceramic is directly related to aesthetics, it was the second thing that was tested. Unlike most other studies we wanted to see patients’ satisfaction with provided crowns. In many cases, patients’ expectations are lower than dentists’, especially in the lateral region, and often the teeth are even overprepared to get enough space for aesthetic material. That was also seen in this study where patients’ satisfaction with the aesthetics of monolithic crowns was much higher than those of the trained clinician. While the clinician scored color for half of the monolithic crowns A and half B, the patients’ average aesthetic satisfaction after cementation was 99%. The difference is probably a result of thinner ceramic and a difference in translucency, which the clinician noticed, but in most cases, the patients did not. When speaking about veneered crowns, the difference was not so big, as the clinician scored all the crowns A, while patients’ average satisfaction was 98%. It is interesting that despite the fact that the clinician scored all veneered crowns A, patients’ average aesthetic satisfaction with veneered crowns was almost the same as for monolithic crowns. These results are in correspondence with study assumption that patients do not notice minor details that can affect the aesthetics and color so much, and that the patients’ expectations are often lower than the clinician, leading to much higher satisfaction. After one year, patients’ average aesthetic satisfaction even increased, which lead us to conclude that only aesthetics is not as important to patients as we think, and if there are some minor imperfections or the material of choice, it doesn’t enable perfect aesthetics; after some time, most of the patients would not notice any difference.
Development in ceramic materials and adhesive bonding agents led to modification of classic preparation principles in fixed prosthodontics with a trend shifting to preservation of as much tooth structure as possible. Increasing demands for metal-free restorations and superb aesthetics have also led to the development of many new all-ceramic systems that allow all-ceramic restorations to be made wholly from strong material without compromising the aesthetics. Therefore, the primary objective of this study was to see whether the thinner lithium-disilicate crown can achieve satisfactory clinical survival rate and aesthetics, and thus lead to additional tooth preservation.
The limitation of current results, regarding survival of the crowns, is the time of the study. As these are one-year follow-up results, further assessment is planned to see the clinical performance of reduced-thickness monolithic crowns.
5. Conclusions
Within the limitation of this study, it can be said that the one-year survival rate of reduced-thickness IPS e.max lithium-disilicate posterior crowns is similar to those of veneered IPS e.max lithium-disilicate crowns. Furthermore, patients’ satisfaction with the aesthetics of both crowns is almost the same.
Author Contributions
Conceptualization, D.Š. and M.J.; Methodology, D.Š.; Investigation, D.Š.; Writing-original draft preparation, D.Š.; Writing-review and editing, M.J.; Supervision, M.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external founding.
Institutional Review Board Statement
The research protocol was approved by the Ethical Committee of the School of Dentistry, University of Zagreb, Croatia (date of approval 13 January 2017).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Due to confidentiality all the data are secured and available to the investigator.
Acknowledgments
School of Dentistry, University of Zagreb, Croatia.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Aquilino, S.A.; Caplan, D.J. Relationship between crown placement and the survival of endodontically treated teeth. J. Prosthet. Dent. 2002, 87, 256–263. [Google Scholar] [CrossRef]
- Dammaschke, T.; Steven, D.; Kaup, M.; Ott, K.H.R. Long-term survival of root-canal-treated teeth: A retrospective study over 10 years. J. Endod. 2003, 29, 638–643. [Google Scholar] [CrossRef]
- Sorensen, J.A.; Martinoff, J.T. Intracoronal reinforcement and coronal coverage: A study of endodontically treated teeth. J. Prosthet. Dent. 1984, 5, 780–784. [Google Scholar] [CrossRef]
- Eckerbom, M.; Magnusson, T.; Martinsson, T. Reasons for and incidence of tooth mortality in a Swedish population. Endod. Dent. Traumatol. 1992, 8, 230–234. [Google Scholar] [CrossRef] [PubMed]
- Torbjörner, A.; Fransson, B. Biomechanical aspects of prosthetic treatment of structurally compromised teeth. Int. J. Prosthodont. 2004, 17, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Fokkinga, W.A.; Kreulen, C.M.; Bronkhorst, E.; Creugers, N.H. Up to 17-year controlled clinical study on post-and-cores and covering crowns. J. Dent. 2007, 35, 778–786. [Google Scholar] [CrossRef] [PubMed]
- Etman, M.K.; Woolford, M.J. Three-year clinical evaluation of two ceramic crown systems: A preliminary study. J. Prosthet. Dent. 2010, 103, 80–90. [Google Scholar] [CrossRef]
- Tysowsky, G.W. The science behind lithium disilicate: A metal-free alternative. Dent. Today 2009, 28, 112–113. [Google Scholar] [PubMed]
- Reich, S.; Schierz, O. Chair-side generated posterior lithium disilicate crowns after 4 years. Clin. Oral Investig. 2013, 17, 1765–1772. [Google Scholar] [CrossRef]
- Giordano, R. Materials for chairside CAD/CAM-produced restorations. J. Am. Dent. Assoc. 2006, 137, 14–21. [Google Scholar] [CrossRef]
- Guess, P.C.; Zavanelli, R.A.; Silva, N.R.; Bonfante, E.A.; Coelho, P.G.; Thompson, V.P. Monolithic CAD/CAM lithium disilicate versus veneered Y-TZP crowns: Comparison of failure modes and reliability after fatigue. Int. J. Prosthodont. 2010, 23, 434–442. [Google Scholar] [PubMed]
- Zhao, K.; Pan, Y.; Guess, P.C.; Zhang, X.-P.; Swain, M.V. Influence of veneer application on fracture behavior of lithium-disilicate-based ceramic crowns. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2012, 28, 653–660. [Google Scholar] [CrossRef] [PubMed]
- Silva, N.; Bonfante, E.; Martins, L.; Valverde, G.; Thompson, V.; Ferencz, J.; Coelho, P. Reliability of reduced-thickness and thinly veneered lithium disilicate crowns. J. Dent. Res. 2012, 91, 305–310. [Google Scholar] [CrossRef] [Green Version]
- Fasbinder, D.J.; Dennison, J.B.; Heys, D.; Neiva, G. A clinical evaluation of chairside lithium disilicate CAD/CAM crowns: A two-year report. J. Am. Dent. Assoc. Sup. 2010, 141, 10–14. [Google Scholar] [CrossRef]
- Reich, S.; Fischer, S.; Sobotta, B.; Klapper, H.U.; Gozdowski, S. A preliminary study on the short-term efficacy of chairside computer-aided design/computer-assisted manufacturing-generated posterior lithium disilicate crowns. Int. J. Prosthodont. 2010, 23, 214–216. [Google Scholar]
- Etemadi, S.; Smales, R.J.; Drummond, P.W.; Goodhart, J.R. Assessment of tooth preparation designs for posterior resin-bonded porcelain restorations. J. Oral Rehabil. 1999, 26, 691–697. [Google Scholar] [CrossRef]
- Blair, F.M.; Wassell, R.W.; Steele, J.G. Crowns and other extra-coronal restorations: Preparations for full veneer crowns. Br. Dent. J. 2002, 192, 567–571. [Google Scholar] [CrossRef]
- Shillingburg, H.T.; Hobo, S.; Whitsett, L.D.; Jacobi, R.; Brackett, S.E. Fundamentals of Fixed Prosthodontics, 3rd ed.; Carol Stream; Quintessence Publishing Co., Inc.: Carol Stream, IL, USA, 1997. [Google Scholar]
- Davis, G.R.; Tayeb, R.A.; Seymour, K.G.; Cherukara, G.P. Quantification of residual dentine thickness following crown preparation. J. Dent. 2012, 40, 571–576. [Google Scholar] [CrossRef] [PubMed]
- Bayne, S.; Schmalz, G. Reprinting the classic article on USPHS evaluation methods for measuring the clinical research performance of restorative materials. Clin. Oral Investig. 2005, 9, 209–214. [Google Scholar] [CrossRef]
- Krämer, N.; Ebert, J.; Petschelt, A.; Frankenberger, R. Ceramic inlays bonded with two adhesives after 4 years. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2006, 22, 13–21. [Google Scholar] [CrossRef]
- Seydler, B.; Rues, S.; Müller, D.; Schmitter, M. In vitro fracture load of monolithic lithium disilicate ceramic molar crowns with different wall thicknesses. Clin. Oral Investig. 2014, 18, 1165–1171. [Google Scholar] [CrossRef] [PubMed]
- Nawafleh, N.A.; Hatamleh, M.M.; Öchsner, A.; Mack, F. Fracture load and survival of anatomically representative monolithic lithium disilicate crowns with reduced tooth preparation and ceramic thickness. J. Adv. Prosthodont. 2017, 9, 416–422. [Google Scholar] [CrossRef] [Green Version]
- Sasse, M.; Krummel, A.; Klosa, K.; Kern, M. Influence of restoration thickness and dental bonding surface on the fracture resistance of full-coverage occlusal veneers made from lithium disilicate ceramic. Dent. Mater. 2015, 31, 907–915. [Google Scholar] [CrossRef] [PubMed]
- Heintze, S.D.; Reinhardt, M.; Peschke, A. Fatigue resistance of CAD/CAM all-ceramic molar crowns of reduced thickness. Dent. Mater. 2017, 33, e38. [Google Scholar] [CrossRef]
- Sulaiman, T.A.; Delgado, A.J.; Donovan, T.E. Survival rate of lithium disilicate restorations at 4 years: A retrospective study. J. Prosthet. Dent. 2015, 114, 364–366. [Google Scholar] [CrossRef] [PubMed]
- Malament, K.A.; Natto, Z.S.; Thompson, V.; Rekow, D.; Eckert, S.; Weber, H.P. Ten-year survival of pressed, acid-etched e.max lithium disilicate monolithic and bilayered complete-coverage restorations: Performance and outcomes as a function of tooth position and age. J. Prosthet. Dent. 2019, 121, 782–790. [Google Scholar] [CrossRef] [Green Version]
- Longhini, D.; Rocha, C.; de Oliveira, L.T.; Olenscki, N.G.; Bonfante, E.A.; Adabo, G.L. Mechanical behavior of ceramic monolithic systems with different thicknesses. Oper. Dent. 2019, 44, E244–E253. [Google Scholar] [CrossRef]
- de Paula, V.G.; Bonfante, G.; Lorenzoni, F.C.; Coelho, P.G.; Bonjardim, L.R.; Fardin, V.P.; Bonfante, E.A. Lifetime prediction of veneered versus monolithic lithium disilicate crowns loaded on marginal ridges. Dent. Mater. 2019, 35, 511–522. [Google Scholar] [CrossRef]
- Gehrt, M.A.; Wolfart, S.; Rafai, N.; Reich, S.M.; Edelhoff, D. Clinical results of lithium-disilicate crowns after up to 9 years of service. Clin. Oral Investig. 2013, 17, 275–284. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).