Controlled Drug Delivery Vehicles in Veterinary Oncology: State-of-the-Art and Future Directions
Abstract
1. Introduction
2. Paclitaxel
3. Doxorubicin
4. Cisplatin
5. Small-Molecule Inhibitors and Monoclonal Antibodies
6. Tumor Microenvironment and Drug-Delivered Systems
7. Development of Controlled Drug Delivery Systems and Future Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Dos Anjos, D.S.; Vital, A.F.; Lainetti, P.F.; Leis-Filho, A.F.; Dalmolin, F.; Elias, F.; Calazans, S.G.; Fonseca-Alves, C.E. Deregulation of VEGFR-2 and PDGFR Expression and Microvascular Density in a Triple-Negative Model of Canine Malignant Mammary Tumors with Lymph Node or Lung Metastasis. Vet. Sci. 2019, 6, 3. [Google Scholar] [CrossRef] [PubMed]
- Boston, S.; Henderson, R.A., Jr. Role of surgery in multimodal cancer therapy for small animals. Vet. Clin. Small Anim. Pract. 2014, 44, 855–870. [Google Scholar] [CrossRef] [PubMed]
- Meier, V.S.; Beatrice, L.; Turek, M.; Poirier, V.J.; Cancedda, S.; Stiborova, K.; Körner, M.; Marconato, L.; Weyland, M.S.; Rohrer Bley, C. Outcome and failure patterns of localized sinonasal lymphoma in cats treated with first-line single-modality radiation therapy: A retrospective study. Vet. Comp. Oncol. 2019, 17, 528–536. [Google Scholar] [CrossRef] [PubMed]
- Kent, M.S. Cats and chemotherapy: Treat as ‘small dogs’ at your peril. J. Feline Med. Surg. 2013, 15, 419–424. [Google Scholar] [CrossRef]
- Prado, M.C.M.; Macedo, S.A.L.; Guiraldelli, G.G.; de Faria Lainetti, P.; Leis-Filho, A.F.; Kobayashi, P.E.; Laufer-Amorim, R.; Fonseca-Alves, C.E. Investigation of the Prognostic Significance of Vasculogenic Mimicry and Its Inhibition by Sorafenib in Canine Mammary Gland Tumors. Front. Oncol. 2019, 9, 1445. [Google Scholar] [CrossRef]
- Dos Anjos, D.S.; Bueno, C.; Magalhães, L.F.; Magalhães, G.M.; Mattos-Junior, E.; Pinto, M.M.R.; De Nardi, A.B.; Brunner, C.H.M.; Leis-Filho, A.F.; Calazans, S.G.; et al. Electrochemotherapy induces tumor regression and decreases the proliferative index in canine cutaneous squamous cell carcinoma. Sci. Rep. 2019, 9, 15819. [Google Scholar] [CrossRef]
- Fonseca-Alves, C.E.; Kobayashi, P.E.; Leis-Filho, A.F.; Lainetti, P.F.; Grieco, V.; Kuasne, H.; Rogatto, S.R.; Laufer-Amorim, R. E-Cadherin Downregulation is Mediated by Promoter Methylation in Canine Prostate Cancer. Front. Genet. 2019, 10, 1242. [Google Scholar] [CrossRef]
- Hohenhaus, A.E.; Kelsey, J.L.; Haddad, J.; Barber, L.; Palmisano, M.; Farrelly, J.; Soucy, A. Canine Cutaneous and Subcutaneous Soft Tissue Sarcoma: An Evidence-Based Review of Case Management. J. Am. Anim. Hosp. Assoc. 2016, 52, 77–89. [Google Scholar] [CrossRef]
- Turner, H.; Séguin, B.; Worley, D.R.; Ehrhart, N.P.; Lafferty, M.H.; Withrow, S.J.; Selmic, L.E. Prognosis for dogs with stage III osteosarcoma following treatment with amputation and chemotherapy with and without metastasectomy. J. Am. Vet. Med. Assoc. 2017, 251, 1293–1305. [Google Scholar] [CrossRef]
- Wendelburg, K.M.; Price, L.L.; Burgess, K.E.; Lyons, J.A.; Lew, F.H.; Berg, J. Survival time of dogs with splenic hemangiosarcoma treated by splenectomy with or without adjuvant chemotherapy: 208 cases (2001–2012). J. Am. Vet. Med. Assoc. 2015, 247, 393–403. [Google Scholar] [CrossRef]
- Axiak, S.M.; Selting, K.A.; Decedue, C.J.; Henry, C.J.; Tate, D.; Howell, J.; Bilof, K.J.; Kim, D.Y. Phase I dose escalation safety study of nanoparticulate paclitaxel (CTI 52010) in normal dogs. Int. J. Nanomed. 2011, 6, 2205–2212. [Google Scholar] [CrossRef] [PubMed]
- Bredlau, A.L.; Motamarry, A.; Chen, C.; McCrackin, M.A.; Helke, K.; Armeson, K.E.; Bynum, K.; Broome, A.M.; Haemmerich, D. Localized delivery of therapeutic doxorubicin dose across the canine blood-brain barrier with hyperthermia and temperature sensitive liposomes. Drug Deliv. 2018, 25, 973–984. [Google Scholar] [CrossRef] [PubMed]
- Kesisoglou, F.; Wang, M.; Galipeau, K.; Harmon, P.; Okoh, G.; Xu, W. Effect of Amorphous Nanoparticle Size on Bioavailability of Anacetrapib in Dogs. J. Pharm. Sci. 2019, 108, 2917–2925. [Google Scholar] [CrossRef] [PubMed]
- Marr, A.K.; Kurzman, I.D.; Vail, D.M. Preclinical evaluation of a liposome-encapsulated formulation of cisplatin in clinically normal dogs. Am. J. Vet. Res. 2004, 65, 1474–1478. [Google Scholar] [CrossRef]
- Prélaud, A.R.; Fuchs, S.; Weber, K.; Winter, G.; Coester, C.; Mueller, R.S. In vitro effects of CpG oligodeoxynucleotides delivered by gelatin nanoparticles on canine peripheral blood mononuclear cells of atopic and healthy dogs—a pilot study. Vet. Dermatol. 2013, 24, 494-e117. [Google Scholar] [CrossRef]
- Arami, H.; Patel, C.B.; Madsen, S.J.; Dickinson, P.J.; Davis, R.M.; Zeng, Y.; Sturges, B.K.; Woolard, K.D.; Habte, F.G.; Akin, D.; et al. Nanomedicine for Spontaneous Brain Tumors: A Companion Clinical Trial. ACS Nano 2019, 13, 2858–2869. [Google Scholar] [CrossRef]
- Lee, J.; Cho, H.R.; Cha, G.D.; Seo, H.; Lee, S.; Park, C.K.; Kim, J.W.; Qiao, S.; Wang, L.; Kang, D.; et al. Flexible, sticky, and biodegradable wireless device for drug delivery to brain tumors. Nat. Commun. 2019, 10, 5205. [Google Scholar] [CrossRef]
- Young, J.S.; Bernal, G.; Polster, S.P.; Nunez, L.; Larsen, G.F.; Mansour, N.; Podell, M.; Yamini, B. Convection-Enhanced Delivery of Polymeric Nanoparticles Encapsulating Chemotherapy in Canines with Spontaneous Supratentorial Tumors. World Neurosurg. 2018, 117, e698–e704. [Google Scholar] [CrossRef]
- Freeman, A.C.; Platt, S.R.; Holmes, S.; Kent, M.; Robinson, K.; Howerth, E.; Eagleson, J.; Bouras, A.; Kaluzova, M.; Hadjipanayis, C.G. Convection-enhanced delivery of cetuximab conjugated iron-oxide nanoparticles for treatment of spontaneous canine intracranial gliomas. J. Neurooncol. 2018, 137, 653–663. [Google Scholar] [CrossRef]
- Rossmeisl, J. Maximizing Local Access to Therapeutic Deliveries in Glioblastoma. Part V: Clinically Relevant Model for Testing New Therapeutic Approaches. In Glioblastoma [Internet]; De Vleeschouwer, S., Ed.; Codon Publications: Brisbane, Australia, 2017. Available online: http://www.ncbi.nlm.nih.gov/books/NBK470000 (accessed on 20 April 2020).
- Park, S.Y.; Kang, Z.; Thapa, P.; Jin, Y.S.; Park, J.W.; Lim, H.J.; Lee, J.Y.; Lee, S.W.; Seo, M.H.; Kim, M.S.; et al. Development of sorafenib loaded nanoparticles to improve oral bioavailability using a quality by design approach. Int. J. Pharm. 2019, 566, 229–238. [Google Scholar] [CrossRef]
- Grabtchak, S.; Montgomery, L.G.; Whelan, W.M. Feasibility of interstitial near-infrared radiance spectroscopy platform for ex vivo canine prostate studies: Optical properties extraction, hemoglobin and water concentration, and gold nanoparticles detection. J. Biomed. Opt. 2014, 19, 057003. [Google Scholar] [CrossRef] [PubMed]
- Feldhaeusser, B.; Platt, S.R.; Marrache, S.; Kolishetti, N.; Pathak, R.K.; Montgomery, D.J.; Reno, L.R.; Howerth, E.; Dhar, S. Evaluation of nanoparticle delivered cisplatin in beagles. Nanoscale 2015, 7, 13822–13830. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Shao, N.; Jin, Y.; Zhang, L.; Jiang, H.; Xiong, N.; Su, F.; Xu, H. Determination of non-liposomal and liposomal doxorubicin in plasma by LC-MS/MS coupled with an effective solid phase extraction: In comparison with ultrafiltration technique and application to a pharmacokinetic study. J. Chromatogr. B 2018, 1072, 149–160. [Google Scholar] [CrossRef] [PubMed]
- Aktas, B.Y.; Taban, H.; Aksoy, S. Atezolizumab and Nab-Paclitaxel in Advanced Triple-Negative Breast Cancer. N. Engl. J. Med. 2019, 380, 985–986. [Google Scholar] [CrossRef]
- Wardhani, B.W.; Puteri, M.U.; Watanabe, Y.; Louisa, M.; Setiabudy, R.; Kato, M. TGF-β-Induced TMEPAI Attenuates the Response of Triple-Negative Breast Cancer Cells to Doxorubicin and Paclitaxel. J. Exp. Pharmacol. 2020, 12, 17–26. [Google Scholar] [CrossRef]
- Poirier, V.J.; Hershey, A.E.; Burgess, K.E.; Phillips, B.; Turek, M.M.; Forrest, L.J.; Beaver, L.; Vail, D.M. Efficacy and toxicity of paclitaxel (Taxol) for the treatment of canine malignant tumors. J. Vet. Intern. Med. 2004, 18, 219–222. [Google Scholar] [CrossRef]
- Silva, D.M.; Franciosi, A.I.; Pezzini, P.C.; Guérios, S.D. Subcutaneous administration of paclitaxel in dogs with cancer: A preliminary study. Can. Vet. J. 2015, 56, 823–830. [Google Scholar]
- Selting, K.A.; Bechtel, S.M.; Espinosa, J.; Henry, C.J.; Tate, D.; Bryan, J.N.; Rajewski, L.; Flesner, B.K.; Decedue, C.; Baltezor, M. Evaluation of intravenous and subcutaneous administration of a novel, excipient-free, nanoparticulate formulation of paclitaxel in dogs with spontaneously occurring neoplasia. Vet. Comp. Oncol. 2018, 16, 650–657. [Google Scholar] [CrossRef]
- Zhao, L.; Ye, Y.; Li, J.; Wei, Y.M. Preparation and the in-vivo evaluation of paclitaxel liposomes for lung targeting delivery in dogs. J. Pharm. Pharmacol. 2011, 63, 80–86. [Google Scholar] [CrossRef]
- Axiak-Bechtel, S.M.; Kumar, S.R.; Dank, K.K.; Clarkson, N.A.; Selting, K.A.; Bryan, J.N.; Rosol, T.J.; Espinosa, J.; Decedue, C.J. Nanoparticulate paclitaxel demonstrates antitumor activity in PC3 and Ace-1 aggressive prostate cancer cell lines. Invest. New Drugs 2013, 31, 1609–1615. [Google Scholar] [CrossRef]
- Young, R.C.; Ozols, R.F.; Myers, C.E. The anthracycline antineoplastic drugs. N. Engl. J. Med. 1981, 305, 139–153. [Google Scholar] [CrossRef] [PubMed]
- Ogilvie, G.K.; Fettman, M.J.; Mallinckrodt, C.H.; Walton, J.A.; Hansen, R.A.; Davenport, D.J.; Gross, K.L.; Richardson, K.L.; Rogers, Q.; Hand, M.S. Effect of fish oil, arginine, and doxorubicin chemotherapy on remission and survival time for dogs with lymphoma: A double-blind, randomized placebo-controlled study. Cancer 2000, 88, 1916–1928. [Google Scholar] [CrossRef]
- Mauldin, G.N.; Matus, R.E.; Withrow, S.J.; Patnaik, A.K. Canine osteosarcoma. Treatment by amputation versus amputation and adjuvant chemotherapy using doxorubicin and cisplatin. J. Vet. Intern. Med. 1988, 2, 177–180. [Google Scholar] [CrossRef] [PubMed]
- Sorenmo, K.U.; Jeglum, K.A.; Helfand, S.C. Chemotherapy of canine hemangiosarcoma with doxorubicin and cyclophosphamide. J. Vet. Intern. Med. 1993, 7, 370–376. [Google Scholar] [CrossRef]
- Withers, S.S.; Kass, P.H.; Rodriguez, C.O., Jr.; Skorupski, K.A.; O’Brien, D.; Guerrero, T.A.; Sein, K.D.; Rebhun, R.B. Fasting reduces the incidence of delayed-type vomiting associated with doxorubicin treatment in dogs with lymphoma. Transl. Oncol. 2014, 7, 377–383. [Google Scholar] [CrossRef]
- O’Keefe, D.A.; Sisson, D.D.; Gelberg, H.B.; Schaeffer, D.J.; Krawiec, D.R. Systemic toxicity associated with doxorubicin administration in cats. J. Vet. Intern. Med. 1993, 7, 309–317. [Google Scholar] [CrossRef]
- Vail, D.M.; Kravis, L.D.; Cooley, A.J.; Chun, R.; MacEwen, E.G. Preclinical trial of doxorubicin entrapped in sterically stabilized liposomes in dogs with spontaneously arising malignant tumors. Cancer Chemother. Pharmacol. 1997, 39, 410–416. [Google Scholar] [CrossRef]
- Gyöngyösi, M.; Lukovic, D.; Zlabinger, K.; Spannbauer, A.; Gugerell, A.; Pavo, N.; Traxler, D.; Pils, D.; Maurer, G.; Jakab, A.; et al. Liposomal doxorubicin attenuates cardiotoxicity via induction of interferon-related DNA damage resistance. Cardiovasc. Res. 2019, 116, cvz192. [Google Scholar] [CrossRef]
- Working, P.K.; Newman, M.S.; Sullivan, T.; Yarrington, J. Reduction of the cardiotoxicity of doxorubicin in rabbits and dogs by encapsulation in long-circulating, pegylated liposomes. J. Pharmacol. Exp. Ther. 1999, 289, 1128–1133. [Google Scholar]
- Sorenmo, K.; Samluk, M.; Clifford, C.; Baez, J.; Barrett, J.S.; Poppenga, R.; Overley, B.; Skorupski, K.; Oberthaler, K.; Van Winkle, T.; et al. Clinical and pharmacokinetic characteristics of intracavitary administration of pegylated liposomal encapsulated doxorubicin in dogs with splenic hemangiosarcoma. J. Vet. Intern. Med. 2007, 21, 1347–1354. [Google Scholar] [CrossRef]
- Teske, E.; Rutteman, G.R.; Kirpenstein, J.; Hirschberger, J. A randomized controlled study into the efficacy and toxicity of pegylated liposome encapsulated doxorubicin as an adjuvant therapy in dogs with splenic haemangiosarcoma. Vet. Comp. Oncol. 2011, 9, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Wójcik, M.; Lewandowski, W.; Król, M.; Pawłowski, K.; Mieczkowski, J.; Lechowski, R.; Zabielska, K. Enhancing anti-tumor efficacy of Doxorubicin by non-covalent conjugation to gold nanoparticles—in vitro studies on feline fibrosarcoma cell lines. PLoS ONE 2015, 10, e0124955. [Google Scholar] [CrossRef] [PubMed]
- Yin, Q.; Tang, L.; Cai, K.; Tong, R.; Sternberg, R.; Yang, X.; Dobrucki, L.W.; Borst, L.B.; Kamstock, D.; Song, Z.; et al. Pamidronate functionalized nanoconjugates for targeted therapy of focal skeletal malignant osteolysis. Proc. Natl. Acad. Sci. USA 2016, 113, E4601–E4609. [Google Scholar] [CrossRef] [PubMed]
- Hauck, M.L.; LaRue, S.M.; Petros, W.P.; Poulson, J.M.; Yu, D.; Spasojevic, I.; Pruitt, A.F.; Klein, A.; Case, B.; Thrall, D.E.; et al. Phase I trial of doxorubicin-containing low temperature sensitive liposomes in spontaneous canine tumors. Clin. Cancer Res. 2006, 12, 4004–4010. [Google Scholar] [CrossRef] [PubMed]
- Kisseberth, W.C.; MacEwen, E.G.; Helfand, S.C.; Vail, D.M.; London, C.L.; Keller, E. Response to liposome-encapsulated doxorubicin (TLC D-99) in a dog with myeloma. J. Vet. Intern. Med. 1995, 9, 425–428. [Google Scholar] [CrossRef] [PubMed]
- Kleiter, M.; Tichy, A.; Willmann, M.; Pagitz, M.; Wolfesberger, B. Concomitant liposomal doxorubicin and daily palliative radiotherapy in advanced feline soft tissue sarcomas. Vet. Radiol. Ultrasound 2010, 51, 349–355. [Google Scholar] [CrossRef]
- Griffin, L.; Frank, C.B.; Seguin, B. Pilot study to evaluate the efficacy of lymphotropic nanoparticle enhanced MRI for diagnosis of metastatic disease in canine head and neck tumours. Vet. Comp. Oncol. 2019. [Google Scholar] [CrossRef]
- Dasari, S.; Tchounwou, P.B. Cisplatin in cancer therapy: Molecular mechanisms of action. Eur. J. Pharmacol. 2014, 740, 364–378. [Google Scholar] [CrossRef]
- Sousa, G.F.; Wlodarczyk, S.R.; Monteiro, G. Carboplatin: Molecular mechanisms of action associated with chemoresistance. Braz. J. Pharm. Sci. 2014, 50, 693–701. [Google Scholar] [CrossRef]
- Food and Drug Administration—FDA. PARAPLATIN®. 2004. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2004/20452scs001_paraplatin_lbl.pdf (accessed on 20 April 2020).
- Cai, S.; Zhang, T.; Forrest, W.C.; Yang, Q.; Groer, C.; Mohr, E.; Aires, D.J.; Axiak-Bechtel, S.M.; Flesner, B.K.; Henry, C.J.; et al. Phase I-II clinical trial of hyaluronan-cisplatin nanoconjugate in dogs with naturally occurring malignant tumors. Am. J. Vet. Res. 2016, 77, 1005–1016. [Google Scholar] [CrossRef]
- Vail, D.M.; Kurzman, I.D.; Glawe, P.C.; O’Brien, M.G.; Chun, R.; Garrett, L.D.; Obradovich, J.E.; Fred, R.M., 3rd; Khanna, C.; Colbern, G.T.; et al. STEALTH liposome-encapsulated cisplatin (SPI-77) versus carboplatin as adjuvant therapy for spontaneously arising osteosarcoma (OSA) in the dog: A randomized multicenter clinical trial. Cancer Chemother. Pharmacol. 2002, 50, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Venable, R.O.; Worley, D.R.; Gustafson, D.L.; Hansen, R.J.; Ehrhart, E.J., 3rd; Cai, S.; Cohen, M.S.; Forrest, M.L. Effects of intratumoral administration of a hyaluronan-cisplatin nanoconjugate to five dogs with soft tissue sarcomas. Am. J. Vet. Res. 2012, 73, 1969–1976. [Google Scholar] [CrossRef] [PubMed]
- Fonseca-Alves, C.E.; Calazans, S.G. Metronomic Chemotherapy in Small Animal Practice: An Update. Asian J. Anim. Vet. Adv. 2016, 11, 17–23. [Google Scholar] [CrossRef][Green Version]
- Holtermann, N.; Kiupel, M.; Kessler, M.; Teske, E.; Betz, D.; Hirschberger, J. Masitinib monotherapy in canine epitheliotropic lymphoma. Vet. Comp. Oncol. 2016, 14 (Suppl. 1), 127–135. [Google Scholar] [CrossRef] [PubMed]
- Giuliano, A.; Dobson, J. Prospective clinical trial of masitinib mesylate treatment for advanced stage III and IV canine malignant melanoma. J. Small Anim. Pract. 2020, 61, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Berger, E.P.; Johannes, C.M.; Jergens, A.E.; Allenspach, K.; Powers, B.E.; Du, Y.; Mochel, J.P.; Fox, L.E.; Musser, M.L. Retrospective evaluation of toceranib phosphate (Palladia®) use in the treatment of gastrointestinal stromal tumors of dogs. J. Vet. Intern. Med. 2018, 32, 2045–2053. [Google Scholar] [CrossRef]
- Piscoya, S.L.; Hume, K.R.; Balkman, C.E. A retrospective study of proteinuria in dogs receiving toceranib phosphate. Can. Vet. J. 2018, 59, 611–616. [Google Scholar]
- Foskett, A.; Manley, C.; Naramore, R.; Gordon, I.K.; Stewart, B.M.; Khanna, C. Tolerability of oral sorafenib in pet dogs with a diagnosis of cancer. Vet. Med. 2017, 8, 97–102. [Google Scholar] [CrossRef]
- Mazzarella, L.; Guida, A.; Curigliano, G. Cetuximab for treating non-small cell lung cancer. Expert Opin. Biol. Ther. 2018, 18, 483–493. [Google Scholar] [CrossRef]
- Singer, J.; Weichselbaumer, M.; Stockner, T.; Mechtcheriakova, D.; Sobanov, Y.; Bajna, E.; Wrba, F.; Horvat, R.; Thalhammer, J.G.; Willmann, M.; et al. Comparative oncology: ErbB-1 and ErbB-2 homologues in canine cancer are susceptible to cetuximab and trastuzumab targeting. Mol. Immunol. 2012, 50, 200–209. [Google Scholar] [CrossRef]
- Baghban, R.; Roshangar, L.; Jahanban-Esfahlan, R.; Seidi, K.; Ebrahimi-Kalan, A.; Jaymand, M.; Kolahian, S.; Javaheri, T.; Zare, P. Tumor microenvironment complexity and therapeutic implications at a glance. Cell Commun. Signal. 2020, 18, 59. [Google Scholar] [CrossRef] [PubMed]
- Pi Castro, D.; José-López, R.; Fernández Flores, F.; Rabanal Prados, R.M.; Mandara, M.T.; Arús, C.; Pumarola Batlle, M. Expression of FOXP3 in Canine Gliomas: Immunohistochemical Study of Tumor-Infiltrating Regulatory Lymphocytes. J. Neuropathol. Exp. Neurol. 2020, 79, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Fonseca-Alves, C.E.; Rodrigues, M.M.; de Moura, V.M.; Rogatto, S.R.; Laufer-Amorim, R. Alterations of C-MYC, NKX3.1, and E-cadherin expression in canine prostate carcinogenesis. Microsc. Res Tech. 2013, 76, 1250–1256. [Google Scholar] [CrossRef] [PubMed]
- Franzoni, M.S.; Brandi, A.; de Oliveira Matos Prado, J.K.; Elias, F.; Dalmolin, F.; de Faria Lainetti, P.; Prado, M.C.M.; Leis-Filho, A.F.; Fonseca-Alves, C.E. Tumor-infiltrating CD4(+) and CD8(+) lymphocytes and macrophages are associated with prognostic factors in triple-negative canine mammary complex type carcinoma. Res. Vet. Sci. 2019, 126, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Calderón, L.G.R.; Kobayashi, P.E.; Vasconcelos, R.O.; Fonseca-Alves, C.E.; Laufer-Amorim, R. Characterization of Collagen Fibers (I, III, IV) and Elastin of Normal and Neoplastic Canine Prostatic Tissues. Vet. Sci. 2019, 6, 22. [Google Scholar] [CrossRef] [PubMed]
- De Souza, T.A.; de Campos, C.B.; De Biasi Bassani Gonçalves, A.; Nunes, F.C.; Monteiro, L.N.; de Oliveira Vasconcelos, R.; Cassali, G.D. Relationship between the inflammatory tumor microenvironment and different histologic types of canine mammary tumors. Res. Vet. Sci. 2018, 119, 209–214. [Google Scholar] [CrossRef]
- Guo, J.; Zeng, H.; Chen, Y. Emerging Nano Drug Delivery Systems Targeting Cancer-Associated Fibroblasts for Improved Antitumor Effect and Tumor Drug Penetration. Mol. Pharm. 2020, 17, 1028–1048. [Google Scholar] [CrossRef]
- Matiz, O.R.S.; Santili, J.; Almeida, M.A.M.; Magalhaes, L.F.; Magalhaes, G.M.; Fonseca-Alves, C.E.; Nardi, A.B.; Calazans, S.G. Loss of Tumor-Associated Macrophages and Vascular Endothelial Growth Factor Immunoexpression in Solid Mammary Carcinoma in Dogs. Pak. Vet. J. 2019, 40. [Google Scholar] [CrossRef]
- Ettlin, J.; Clementi, E.; Amini, P.; Malbon, A.; Markkanen, E. Analysis of gene expression signatures in cancer-associated stroma from canine mammary tumours reveals molecular homology to human breast carcinomas. Int. J. Mol. Sci. 2017, 18, 1101. [Google Scholar] [CrossRef]
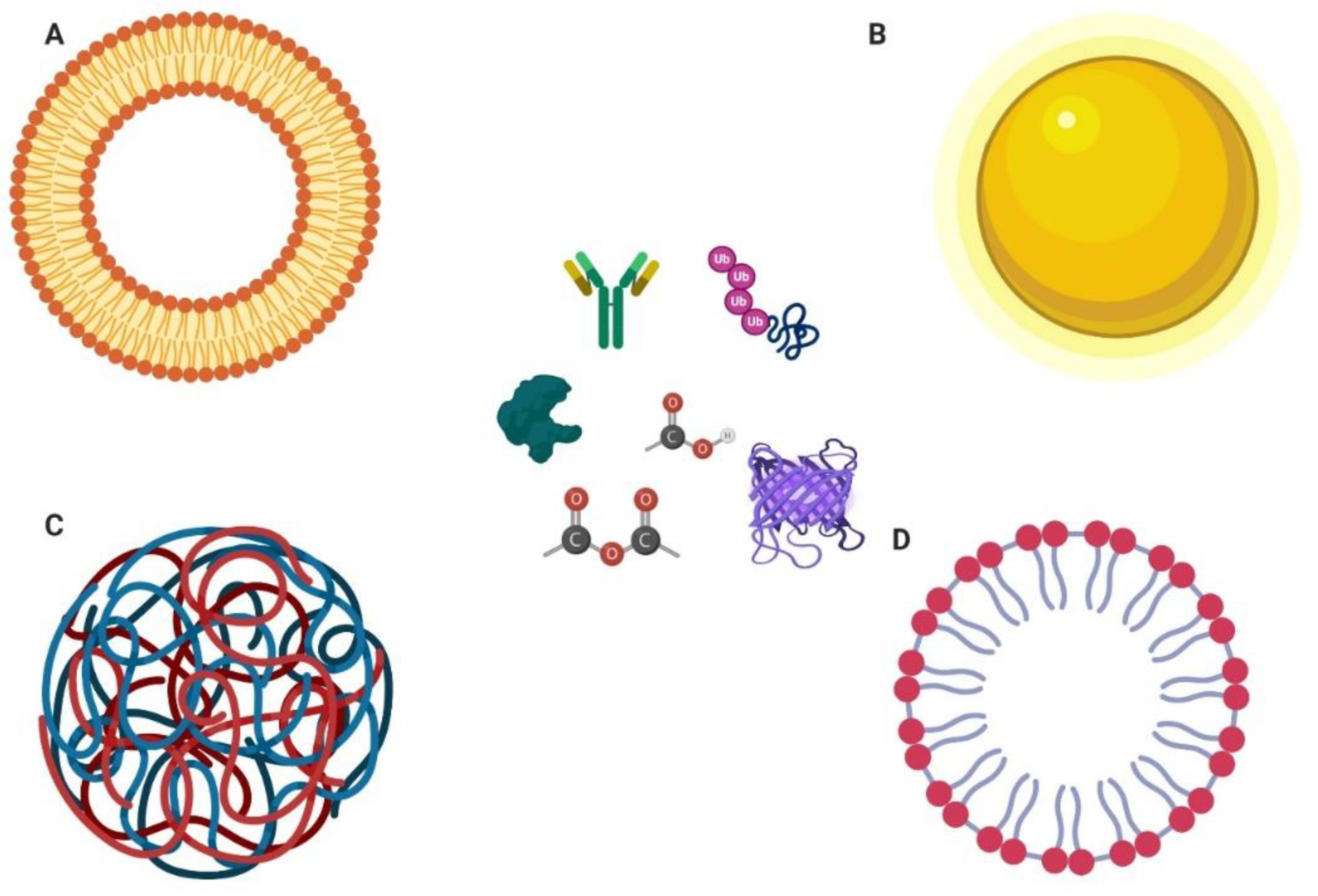
- Zabielska-Koczywąs, K.; Lechowski, R. The Use of Liposomes and Nanoparticles as Drug Delivery Systems to Improve Cancer Treatment in Dogs and Cats. Molecules 2017, 22, 2167. [Google Scholar] [CrossRef]
- Akbarzadeh, A.; Rezaei-Sadabady, R.; Davaran, S.; Joo, S.W.; Zarghami, N.; Hanifehpour, Y.; Samiei, M.; Kouhi, M.; Nejati-Koshki, K. Liposome: Classification, preparation, and applications. Nanoscale Res. Lett. 2013, 8, 102. [Google Scholar] [CrossRef] [PubMed]
- Hoopes, P.J.; Wagner, R.J.; Duval, K.; Kang, K.; Gladstone, D.J.; Moodie, K.L.; Crary-Burney, M.; Ariaspulido, H.; Veliz, F.A.; Steinmetz, N.F.; et al. Treatment of Canine Oral Melanoma with Nanotechnology-Based Immunotherapy and Radiation. Mol. Pharm. 2018, 15, 3717–3722. [Google Scholar] [CrossRef] [PubMed]
- Lucas, S.R.; Maranhão, R.C.; Guerra, J.L.; Coelho, B.M.; Barboza, R.; Pozzi, D.H. Pilot clinical study of carmustine associated with a lipid nanoemulsion in combination with vincristine and prednisone for the treatment of canine lymphoma. Vet. Comp. Oncol. 2015, 13, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Raposo, L.R.; Roma-Rodrigues, C.; Jesus, J.; Martins, L.M.D.R.S.; Pombeiro, A.J.; Baptista, P.V.; Fernandes, A.R. Targeting canine mammary tumours via gold nanoparticles functionalized with promising Co(II) and Zn(II) compounds. Vet. Comp. Oncol. 2017, 15, 1537–1542. [Google Scholar] [CrossRef]
- Hansen, A.E.; Petersen, A.L.; Henriksen, J.R.; Boerresen, B.; Rasmussen, P.; Elema, D.R.; af Rosenschöld, P.M.; Kristensen, A.T.; Kjær, A.; Andresen, T.L. Positron Emission Tomography Based Elucidation of the Enhanced Permeability and Retention Effect in Dogs with Cancer Using Copper-64 Liposomes. ACS Nano 2015, 9, 6985–6995. [Google Scholar] [CrossRef]
- Axiak-Bechtel, S.M.; Upendran, A.; Lattimer, J.C.; Kelsey, J.; Cutler, C.S.; Selting, K.A.; Bryan, J.N.; Henry, C.J.; Boote, E.; Tate, D.J.; et al. Gum arabic-coated radioactive gold nanoparticles cause no short-term local or systemic toxicity in the clinically relevant canine model of prostate cancer. Int. J. Nanomed. 2014, 9, 5001–5011. [Google Scholar] [CrossRef]
- Benhabbour, S.R.; Luft, J.C.; Kim, D.; Jain, A.; Wadhwa, S.; Parrott, M.C.; Liu, R.; DeSimone, J.M.; Mumper, R.J. In vitro and in vivo assessment of targeting lipid-based nanoparticles to the epidermal growth factor-receptor (EGFR) using a novel Heptameric ZEGFR domain. J. Control. Release 2012, 158, 63–71. [Google Scholar] [CrossRef]
- Mili, B.; Das, K.; Kumar, A.; Saxena, A.C.; Singh, P.; Ghosh, S.; Bag, S. Preparation of NGF encapsulated chitosan nanoparticles and its evaluation on neuronal differentiation potentiality of canine mesenchymal stem cells. J. Mater. Sci. Mater. Med. 2017, 29, 4. [Google Scholar] [CrossRef]
- Zhong, J.; Mao, W.; Shi, R.; Jiang, P.; Wang, Q.; Zhu, R.; Wang, T.; Ma, Y. Pharmacokinetics of liposomal-encapsulated and un-encapsulated vincristine after injection of liposomal vincristine sulfate in beagle dogs. Cancer Chemother. Pharmacol. 2014, 73, 459–466. [Google Scholar] [CrossRef]
| Substance | Nanomaterial | Tumour Subtype | Study Results | Outcome | Reference |
|---|---|---|---|---|---|
| - | Silica- coated gold nanoparticles (GNPs) | Brain tumors | GNPs were more frequently found in tissue areas closer to blood vessel walls and had heterogeneous extravasation into spontaneous brain tumors. | Nanoparticles’ EPR and its variations foreshadow clinical applications of nanomedicine in management of brain tumors | Arami et al. [16] |
| - | Colloidal solution of Gold nanorods (Nanopartz) | Prostate | Optical detection of Au NPs via the proportional absorption of the product (NP concentration and the individual absorption cross-section). | Gold nanoparticles can be used for ex vivo systematic study of canine and, potentially, human prostate; comprehensive diagnostic markers in determining the state of the prostate health | Grabtchak et al. [22] |
| Plant-based virus-like nanoparticle (VLP) | Magnetic iron oxide nanoparticle (mNPH) | Oral melanoma | Immunological reaction in the tumor correlated with the clinical response and significant increase in immune cell infiltration of tumors receiving radiotherapy with VLP treatment. | The study successfully demonstrates the feasibility, safety and promising efficacy of VLP + radiotherapy treatment in a highly translatable spontaneous preclinical model | Hoopes et al. [74] |
| Carmustine | Lipid nanoemulsion (LDE) | Lymphoma | LDE-carmustine showed non-hematologic toxicity or hepatic function commitment; LDE- carmustine and commercial carmustine were equivalent in terms of toxicity, tumor remission and survival time. | LDE- carmustine is safe for administration in a combined chemotherapeutic protocol with vincristine and prednisone | Lucas et al. [75] |
| Cetuximab | Iron-oxide nanoparticles (cetuximab-IONPs) | Spontaneous intracranial gliomas | Volume of distribution was proportional to infusion volume and dispersion of the cetuximab-IONPs and infusion can be delivered in awake dogs safely and effectively over 3 days. | Cetuximab-IONP CED is a safe and effective adjuvant therapy for spontaneous canine glioma patients at the time of their initial tumor surgery. | Freeman et al. [19] |
| Cisplatin | Hyaluronan-cisplatin nanoconjugate (HA-Pt) | Spontaneous cancers | Cisplatin and HA-Pt inhibited cell growth over 80% compared to control and cisplatin treatment showed similar levels of creatinine excretion. HA-Pt did not cause nephrotoxicity. | The HA-Pt formulation demonstrated positive response in spontaneous canine squamous cell carcinomas | Cai et al. [52] |
| Cisplatin | Platin-M nano- particles (T-Platin-M-NPs) | Canine J3TBG glioma and SDT3G glioblastoma cell lines | T-Platin-M-NPs can be effective in glial cell canine tumors and its activity is better than cisplatin and carboplatin which are currently used as chemotherapeutic agents. | There is potential to use T-Platin-M-NPs as an effective injectable chemotherapeutic agent in dogs | Feldhaeusser et al. [23] |
| Cisplatin | Liposome-encapsulated | Healthy animals | Toxic effects commonly associated with unencapsulated cisplatin, were not observed in dogs treated with liposome-encapsulated cisplatin at dosages equivalent to twice the known maximally tolerated dose of unencapsulated cisplatin. | Liposome- encapsulated cisplatin can be safely administered to clinically normal dogs at dosages of up to 150 mg/m2 without the need for concurrent hydration protocols | Marr et al. [14] |
| Cisplatin | STEALH Liposome-encapsulated cisplatin (SPI-77) | Osteosarcoma | The 11-month overall median survival found for SPI-77-treated dogs was nearly identical to that reported using native cisplatin. The systemic delivery of these escalated doses did not translate into enhanced efficacy. | Liposome encapsulation of cisplatin allows the safe and repeated delivery of doses up to five times the maximally tolerated dose of native cisplatin in tumor bearing dogs | Vail et al. [53] |
| Cisplatin | Hyaluronan nanocarrier | Soft tissue sarcomas | No tissue reactions were detected after hyaluronan-cisplatin injection; intratumoral administration of hyaluronan-cisplatin resulted in higher concentrations in the tumor and sentinel lymph nodes than in plasma or serum. | Intratumoral injection of the hyaluronan-cisplatin nanoconjugate was well tolerated in treated dogs and may be a safe and effective method for the administration of maintenance chemotherapy | Venable et al. [54] |
| Co(II)-NanoTS265 and Zn(II)-NanoTS262 compounds | Gold nanoparticles (AuNPs) | Mammary tumours (FR37-CMT) cells | Both compounds induced a reduction of viable cell. AuNPs can act as promising carriers for drug delivery; increased cytotoxic activity; metal compounds displayed lower IC50 than cisplatin and doxorubicin against cells. | NanoTS262 and NanoTS265 are promising chemotherapeutic formulations for mammary carcinomas and targeting anti-bodies or peptides, may further improve efficacy | Raposo et al. [76] |
| Cu-64 | PEGylated liposomes with copper-64 | Spontaneous solid tumors | New and highly efficient method for loading copper-64 PET isotopes into liposomes; moderate to high nanocarrier tumor accumulation levels were achieved in spontaneous carcinomas based on the EPR-effect. | Radiolabeled liposomes may serve as theragnostic imaging agent guiding both diagnostic and therapeutic intervention for several malignancies in future clinical practice | Hansen et al. [77] |
| Doxorrubicin | PEGylated liposomes with Copper-64 | Splenic Haemangiosarcoma | Intraperitoneal treated dogs had fewer serosal, mesenteric, and omental metastases than historical controls treated with systemic doxorubicin. Pegylated liposomal doxorubicin was absorbed relatively quickly from the abdominal cavity. | Intraperitoneal pegylated liposomal encapsulated doxorubicin administration did not prevent intraabdominal recurrence of HSA in dogs | Sorenmo et al. [41] |
| Doxorrubicin | PL-DOX (Doxil®, Sequus Pharmaceuticals, Menlo Park, CA, USA) | Splenic Haemangiosarcoma | The median disease-free period for dogs treated with PL-DOX and free doxorubicin was equivalent. No significant differences in toxicity between PL-DOX and free doxorubicin were noticed. | PL-DOX was easily administered to dogs and did not lead to significant toxicities and significant difference in survival was not observed | Teske et al. [42] |
| Doxorrubicin | PL-DOX (Doxil®, Sequus Pharmaceuticals, Menlo Park, CA, USA) | Different tumors type | The dose-limiting toxicities are different for Doxil when compared to free doxorubicin and o significant myelosuppression or cardiotoxicity was noted in Doxil treatment. | Although the results of this study must be evaluated with care owing to the small number in each tumor group, it appears that Doxil as a single agent may have a broad spectrum of activity | Vail et al. [38] |
| Doxorrubicin | Colloid gold nanoparticles | Feline fibrossarcoma | A higher cytotoxic effect of Au-GSH-Dox than that of free doxorubicin has been observed. GSH coated Au NPs are good doxorubicin nanocarriers for feline fibrosarcoma cell lines with high P-gp activity. | Au-GSH-Dox may be a potent new therapeutic agent to increase the efficacy of the drug by overcoming the resistance to doxorubicin in feline fibrosarcoma cell lines | Wójcik et al. [43] |
| Doxorrubicin | Polylactide nanoparticles (NPs) loaded with doxorubicin (Doxo) and coated with bone-seeking pamidronate (Pam) Pam-Doxo-NPs | Osteosarcoma | Enhanced bone tumor accumulation and prolonged retention compared with nontargeted NPs. The therapeutic was well tolerated without toxicities and attenuated localized osteosarcoma progression compared with nontargeted Doxo-NPs. | Pam-Doxo-NPs were capable of minimizing systemic off target toxicities and enhance localized antitumor activities in a preclinical murine tumor model and canine model | Yin et al. [44] |
| Doxorubicin | Temperature sensitive liposomes (TSL) | High-grade gliomas | Higher temperatures resulted in increased area of cerebral damage and TSL combined with hyperthermia allows potentially therapeutic doses of Dox across the blood–brain barrier. | The study demonstrates that localized doxorubicin delivery to the brain can be facilitated by TSL-Dox with localized hyperthermia with no significant neurological deficits | Bredlau et al. [12] |
| Doxorubicin | Low temperature sensitive liposome (LTSL-doxorubicin) | Solid tumors (carcinomas or sarcomas) | The dose of LTSL doxorubicin was suboptimal in many patients and had a 30% response rate and cutaneous toxicity typically observed with LTSL-doxorubicin. | LTSL-doxorubicin offers a novel approach to improving drug delivery to solid tumors; it was well tolerated and resulted in favorable response profiles in these patients | Hauck et al. [45] |
| Doxorubicin | Liposome-encapsulated Doxorubicin (L-DOX) | Multiple Myeloma | Liposome encapsulation of doxorubicin decreases its cardiotoxicity; the remission induced with L-DOX was complete and durable; L-DOX has a decreased toxicity compared with free doxorubicin even with a high dose | L-DOX has greater efficacy in the treatment of some tumors and decreased toxicity compared with free doxorubicin, without cardiotoxicity | Kisseberth et al. [46] |
| Doxorubicin | Pegylated Liposomal Doxorubicin | Feline soft tissues sarcomas | Median overall survival was 324 days and all cats developed some degree of leukotrichia. The liposomal doxorubicin and daily fractionated palliative radiotherapy were well tolerated by the cats. | The administration of pegylated liposomal doxorubicin in combination with daily palliative radiotherapy was feasible, generally well tolerate | Kleiter et al. [47] |
| Ferumoxytol | Ultra-small superparamagnetic iron oxide nanoparticle (USPIOs) lymphotropic nanoparticle enhanced MRI (LNMRI) | Metastatic lymph nodes in Canine Head and Neck Tumors | There were no negative side effects to the USPIOs noted and LNMRI was successful in identifying metastatic lymph nodes with 100% sensitivity and an 88% specificity. | LNMRI has the potential to be a sensitive and specific method of diagnosing lymph node metastasis | Griffin et al. [48] |
| Gold | Gum arabic-coated 198AuNP (GA-198AuNP) | Prostate cancer | GA-198AuNPs have more homogenous dose distribution and higher emission of energy compared to current brachytherapy seeds used to treat prostate cancer and the gum arabic glycoprotein provided a nontoxic coating on NPs and is highly stable in vivo | This study provides evidence that intralesional injection of GA-198AuNP is safe with minimal short-term systemic toxicity in the naturally occurring large animal model of prostatic cancer | Axiak-Bechte et al. [78] |
| High affinity histidine×6-tagged EGFR-binding Z domain (heptameric ZEGFR domain). | Lipid-based oil-filled nanoparticles (NPs) with a high concentration of surface-chelated nickel (Ni-NPs) | A431 epidermoid carcinoma cells | Superior cell uptake achieved in EGFR overexpressing cells with these Ni-NPs with ZEGFR target; successfully target EGFR overexpressing cancer cells; targeting efficiency of the novel heptameric ZEGFR domain was also demonstrated in vivo | Ni-NPs could be a very useful tool for targeting and drug delivery to a wide range of EGFR positive cancers | Benhabbour et al. [79] |
| Nerve growth factor (NGF) | Encapsulated chitosan nanoparticles (CNPs) | Mesenchymal Stem Cells | NGF had 61% efficiency in vitro and these nanoparticles were found to be cytocompatible to Mesenchymal Stem Cells; NGF- CNPs were able to transdifferentiate cBM-MSCs without any chemical based reinduction. | NGF-CNPs are capable of releasing bioactive NGF with the ability to transdifferentiate mesenchymal stem cells into neurons | Mili et al. [80] |
| Paclitaxel | Nanoparticule paclitaxel (CTI 52010) | Healthy animals. focused on spontaneously occurring tumors | No evidence of hypersensitivity or gastrointestinal toxicity. The dose-limiting toxicity was grade 4 neutropenia and the maximum tolerated dosage was 120 mg/m2. | CTI 52010 was well tolerated when administered intravenously to normal dogs | Axiak et al. [11] |
| Paclitaxel | Nanoparticulate paclitaxel (nPX) formulation (CTI52010, Crititax®) | Prostate cancer cell lines (human and dogs) | nPX was as effective as PX in decreasing cell viability, increasing apoptosis, inhibiting clonogenic potential, and modifying microtubule dynamics; it could be an effective alternate for PX | Nanoparticulate paclitaxel is as effective as paclitaxel in both human and canine castration-resistant prostate cancer | Axiak-Bechtel et al. [31] |
| Paclitaxel | Nanoparticulate, excipient-free formulation of paclitaxel (CTI52010) | Different tumors type | The lack of systemic absorption after subcutaneous administration; side effects were well tolerated at dosages up to 118 mg/m2; no unique toxicity or hypersensitivity was noted | CTI52010 was administered safely to tumor-bearing dogs and is an attractive chemotherapeutic to be considered in intratumoral administration | Selting et al. [29] |
| Paclitaxel | Liposomes composed of Tween-80/HSPC/cholesterol | Healthy animals | The paclitaxel liposomes showed excellent lung targeting properties in comparison with paclitaxel injection; liposome carrier was associated with a lung-targeting effect; didn’t cause hemolysis | The liposomes are a promising carrier for a lung-targeting drug delivery system for the treatment of lung diseases, such as lung cancer | Zhao et al. [30] |
| Sorafenib | Nanoparticulation using fat and supercritical fluid (NUFs) | Healthy animals | Encapsulated sorafenib exhibited higher blood drug profiles indicating better absorption; concentration of PVP should be kept at low level to achieve the maximum absorption of sorafenib | Nanoparticle formulation could enhance the bioavailability and therapeutic efficacy of sorafenib | Park et al. [21] |
| Temozolomide (TMZ) | Polymeric magnetite nanoparticles (PMNPs) | Intracranial tumors | In 70% of the cases, the infusion accurately targeted the tumor mass was determined by the presence of PMNP signal in the tumor on immediate postoperative MRI; PMNP was enough to induce an observable decrease in tumor volume | T convection-based drug delivery using PMNPs can be safely performed in a canine model of glioma | Young et al. [18] |
| Vincristine | Liposomes | Healthy animals | Encapsulated vincristine showed a higher plasmatic concentration then un-encapsulated vincristine after intravenous injection of both forms of vincristine; enhanced anti-tumor activity and lower toxicity of liposome | The increased therapeutic index of encapsulated vincristine is demonstrated by the pharmacokinetic features | Zhong et al. [81] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lainetti, P.d.F.; Zuliani, F.; Leis-Filho, A.F.; Fonseca Alves, R.H.; Fonseca-Alves, C.E. Controlled Drug Delivery Vehicles in Veterinary Oncology: State-of-the-Art and Future Directions. Processes 2020, 8, 541. https://doi.org/10.3390/pr8050541
Lainetti PdF, Zuliani F, Leis-Filho AF, Fonseca Alves RH, Fonseca-Alves CE. Controlled Drug Delivery Vehicles in Veterinary Oncology: State-of-the-Art and Future Directions. Processes. 2020; 8(5):541. https://doi.org/10.3390/pr8050541
Chicago/Turabian StyleLainetti, Patricia de Faria, Fernanda Zuliani, Antonio Fernando Leis-Filho, Ricardo Henrique Fonseca Alves, and Carlos Eduardo Fonseca-Alves. 2020. "Controlled Drug Delivery Vehicles in Veterinary Oncology: State-of-the-Art and Future Directions" Processes 8, no. 5: 541. https://doi.org/10.3390/pr8050541
APA StyleLainetti, P. d. F., Zuliani, F., Leis-Filho, A. F., Fonseca Alves, R. H., & Fonseca-Alves, C. E. (2020). Controlled Drug Delivery Vehicles in Veterinary Oncology: State-of-the-Art and Future Directions. Processes, 8(5), 541. https://doi.org/10.3390/pr8050541







