Lean Six Sigma in Healthcare: A Systematic Literature Review on Challenges, Organisational Readiness and Critical Success Factors
Abstract
:1. Introduction
- RQ1:What are the challenges/limitations in deploying LSS in the healthcare sector, as noted in the literature?
- RQ2: What are the organisational readiness factors for deploying LSS in healthcare?
- RQ3: What are the critical success factors (CSFs) for LSS to succeed in healthcare?
- RQ4: What are the key LSS tools utilised in healthcare?
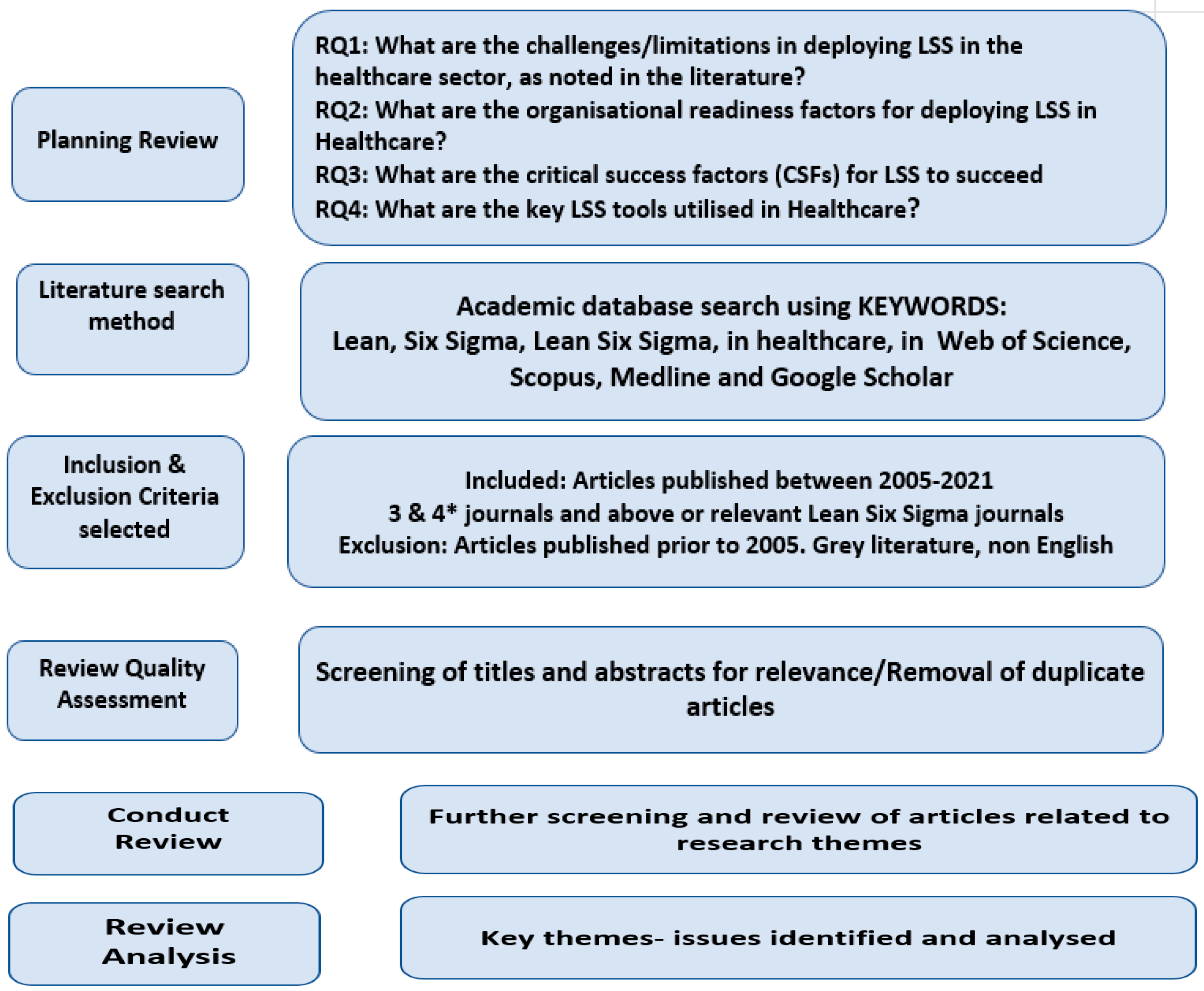
2. Research Methodology
3. Results
3.1. Readiness Factors
| Authors | Readiness Factors |
|---|---|
| Bhat et al. [2] | Effective leadership; statistical and non-statistical Lean tools knowledge; knowledge management (manage lessons learned, maturity); management of multidisciplinary teams; physicians and nurses’ specialised training. |
| Trakulsunti and Antony [4] | Transformational style of leadership. |
| Vaishnavi and Suresh [24] | Management commitment and leadership; effective communication; customer-oriented; financial capabilities; supplier management; LSS tools and technique; coordinate improvement procedure; teamwork and execution technique; training and learning; effective use of technology; organisational strategy; accessibility of information; goal management culture; organisation infrastructure; employee trust and culture; recognition and reward system. |
| Hilton et al. [26] | Transformational leadership; employee commitment; training and coaching activities; maturity in quality initiatives; and effective management of multidisciplinary teams. |
| Ajmera and Jain [29] | Financial capability; patient involvement; time constraint; leadership; professional organisational culture; goal specificity; clarity of organisational vision; competency and expertise; training; and employee engagement. |
| Bowerman et al. [30] | Effective leadership and organisational culture. |
| Feng and Manuel [31] | Management commitment. |
| De Lima et al. [34] | Top management’s vision should add value to the patient and embrace employee motivation. |
| Kahm and Ingelsson [32] | Managers must have time, support from the entire organisation, and clear and disseminated goals. |
| De Lima et al. [34] | Top management’s vision should add value to the patient and embrace employee motivation. |
| Roemeling et al. [33] | Management motivation; alignment between strategy and operational goals; clear and effective communication within the organisation; implementation and dissemination strategy based on organisational maturity; and staff participation and widespread consensus. |
| Roemeling et al. [33] | Maturity in continuous improvement tools; and previous experience in process re-engineering projects. |
| Meyer [35] | Transformational style of leadership; pervasive communication across all organisational levels; widespread knowledge of project management; and training in data analysis and applied performance improvement methods. |
| Ahmed et al. [36] | Effective leadership; training programmes and continuing education; employee suggestion and feedback to improve their Lean implementation skills. |
| Ahmed et al. [36] | Good perception of LSS process improvement tools; trust in structural approach to managing quality improvement activities and planning to decide the major quality improvement projects; employees dedicated and motivated to improve the hospital’s quality performance. |
| Ahmed et al. [36] | Transformational leadership; Lean implementation has to be aligned to organisational strategy; maturity in project management activities; and investment in ongoing training. |
| Hallam and Contreras [37] | Knowledge symmetry; clear communication; and multidisciplinary team management. |
| Holden and Hackbart [38] | Widespread consensus in the organisation; teamwork skills and coaching activities; and widespread and clear communication. |
| Dannapfel et al. [39] | Transformational style of leadership; LSS training; Lean dissemination strategies and organisational culture; and spreading positive results achieved in other departments. |
| Deblois and Lepanto [40] | Changes in the culture of a healthcare setting involving long-term organisational policies and strategic planning; implementation of multidisciplinary and multiskilled teams with decentralised decision making; clinical leaders and managers’ commitment as well as the front-line commitment; recognition of a need for change; and implementation of a quality culture fostering continuous improvement. |
| Honda et al. [41] | Organisation structure and political hierarchy; infrastructure of the hospitals; multidisciplinary team approach coupled with Six Sigma training. |
| Niemeijer et al. [42] | Effective leadership; management commitment; project management skills; and change-oriented organisational culture. |
| McIntosh et al. [43] | Effective leadership; organisational culture; and training. |
| Ulhassan et al. [44] | Effective leadership and management commitment; continuous improvement of organisational culture; and teamwork. |
| Leite et al. [45] | Transformational leadership; staff motivational element (i.e., feeling of working in a constant emergency); and widespread consensus in the organisation. |
| Swarnakar et al. [46] | Top management participation; manager sponsorship and commitment; staff motivation; multidisciplinary team management; and social and organisational approval factors. |
| Abdallah [47] | Transformational leadership; project management skills; introduction strategy; employees’ general understanding; empowering the Lean implementation team; and quality and learning culture |
| Hung et al. [48] | Leadership commitment; sensitivity to professional values and the culture of medicine; and perceived adequacy of organisational resources to fully support the change efforts. |
| Gowen et al. [49] | Employee commitment. |
| Robbins et al. [50] | High-performance work systems (engaging staff, aligning leaders, acquiring and developing talent, and empowering the front line). |
| Steed [51] | Shared reason to change; effective leadership determined by personal characteristics; behaviours and actions, and knowledge; and defining the key leadership strategy to successfully implement LSS in a hospital environment. |
| Dobrzykowski et al. [52] | Top-level management support; transformational leadership; staff dynamic capability; and comprehensive Lean orientation. |
| Walley et al. [53] | Organisation’s orientation to patient values. |
| Peimbert-García [54] | Management support; staff commitment; customer focus; training; continuous improvement vision; cultural readiness; data; external support; and communication. |
| Dobrzykowski and McFadden [55] | Trust and physicians’ commitment; and staff directly employed by the organisation. |
| Eamranond et al. [56] | Effective redistribution of time for hospital staff; cross-fertilisation; employees’ commitment; long-term plans for successful process improvements; mutual commitment of managerial and clinical leaders; effective leadership; continuous improvement culture. |
| Henrique et al. [57] | Effective communication; managerial support; employee commitment; and organisational culture. |
| Henrique et al. [57] | Top management involvement; involvement of health professionals; IT support; dedicated implementation team; and effective leadership. |
| Khorasani et al. [58] | Importance of Lean in supply chain management in Healthcare |
| Hutton et al. [59] | Workplace violence prevention using Lean principles |
| Isack et al. [60] | Adoption of Lean principles in a medical lab; improved efficiencies |
| Narayanamurthy et al. [61] | Transformational leadership; staff commitment; staff have a comprehensive understanding of processes and operational and economic performance. |
3.2. Critical Success Factors (CSFs)
| Authors | CSFs |
|---|---|
| McDermott et al. [1] | Robust data; use of technology; supply chain optimisation; IT support systems; statistical process control techniques; risk management; and workplace management. |
| Bhat et al. [2] | Effective leadership; availability of data; involvement of cross-functional team; effective communication. |
| Ricciardi et al. [3] | Multidisciplinary team. |
| Trakulsunti et al. [4] | Improvement culture; structured deployment plan; sustainability plan; top management commitment; project selection; team formation; and training. |
| Trakulsunti et al. [4] | Understanding tools and techniques; understanding Lean philosophy; top management support; training; staff engagement; leadership capability; appropriate team formation; implementation infrastructure; and cultural change. |
| Trakulsunti and Antony [4] | Clear vision and support from top management; quality improvement culture; and adoption of information technology. |
| Gijo et al. [5] | Effective utilisation of statistical tools and techniques; project management; and cross-functional team. |
| Gonzalez-Aleu et al. [10] | Management support; goal clarity and alignment; commitment to change; team member time management; communication; and availability and reliable data. |
| Burgess and Radnor [19] | Leadership; management commitment; motivational strategies; system maturity; trust; knowledge management; training, Lean project results; project management; organisational culture; training; coaching; team management; and bottom-up approach. |
| Vaishnavi and Suresh [24] | Information about methodology; trust among employees; quality improvement culture; acceptance of change; organisational structure, availability of resources; employee empowerment; employee spirit and cooperation; working environment; and waste audit. |
| Vaishnavi and Suresh [24] | Voice of customers; aligning project goals with organisation vision; management commitment; leadership; effective communication; supplier management; understanding tools and technique; effective use of technology; organizational strategy; organisational infrastructure; continuous performance measurement; employee commitment and trust; recognition and reward system; project selection; time and cost management. |
| Hilton et al. [26] | Training; top management commitment; multidisciplinary team; maturity in the process; improvement initiatives; and project management. |
| Ajmera and Jain [29] | Lean leadership; professional organisational culture; teamwork; and interdepartmental cooperation. |
| Bowerman et al. [30] | Commitment and support from top management; infrastructure; training; effective communication; and effective leadership. |
| Feng and Manuel [31] | Top management leadership. |
| Kahm and Ingelsson [32] | Employee involvement; improvement culture; supportive and participative executive management; and effective communication. |
| Roemeling et al. [33] | Knowledge management; rigorous follow-up; and waste audit. |
| Roemeling et al. [33] | Employees’ involvement in sustainment; standardisation; and maturity in methodology. |
| Meyer [35] | Stakeholder engagement; project management; action plans; effective communications; improvement culture; policy and procedures; and accreditation. |
| Ahmed et al. [36] | Continuous quality improvement; operational excellence initiatives; patient safety; and teamwork. |
| Hallam and Contreras [37] | Establishing clear definitions of Lean healthcare; implementing control plans; training; stakeholder involvement and support; multidisciplinary teams; concurrent involvement by all departments; executive commitment; and clear vision. |
| Holden and Hackbart [38] | Work standardisation; connections between people; seamless flow; problem solving; acceptance of new standard work; and teams in one work cell. |
| Dannapfel et al. [39] | Understanding adopter’s perspective; effective communications; clear vision and objectives; patient participation; and multiple communication channels. |
| Deblois and Lepanto [40] | Empowerment of the front-line workers; continuous improvement; and leadership. |
| Honda et al. [41] | Multidisciplinary team approach; training; presence of an internal project leader and internal project champion; senior leadership involvement as champions; availability of Black Belts and Green Belts in the system; commitment from clinical management and steering committees; involving co-workers and physicians; and continuous communication. |
| Niemeijer et al. [42] | Training for doctors, nurses and support staff; and leadership. |
| Niemeijer et al. [42] | Project management skills; matrix organisational structure; staff and management commitment; directorate sponsorship; successful pilot projects; and continuous training. |
| McIntosh et al. [43] | Leadership; empowerment; teamwork; information sharing; quality programme meetings; employee recognition; results sharing; training, financial rewards, promotion opportunity; and learning ecosystem. |
| Leite et al. [45] | Clear communication; careful planning; visual management; standard operating procedures; and use of technology. |
| Swarnakar et al. [46] | Awareness of statutory policy; comprehensive information; qualified team for deployment; training; multidisciplinary team; and understanding of tools and techniques. |
| Abdallah [47] | Leadership; top management involvement and continuous support; prioritising quality initiative; training and education; empowerment; understanding of tools and techniques; teamwork; and quality and learning culture. |
| Hung et al. [48] | Front-line engagement; visual management; metric of measurement; professional values and culture; culture of innovation, collaboration, creativity; continuous improvement; organisational resources; training; and follow-up. |
| Gowen et al. [49] | Employee commitment; control initiatives; training; communication; performance evaluation; job redesign; and empowerment. |
| Robbins et al. [50] | Rigorous evaluation of improvement strategies in the context. |
| Dobrzykowski et al. [52] | Internal integration; clinical coordination and communication; comprehensive understanding of methodology; waste elimination; and voice of the customer. |
| Walley et al. [53] | Waste audit; and understanding tools and techniques. |
| Peimbert-García et al. [54] | Employee and management commitment. |
| Dobrzykowski and McFadden [55] | Trust between doctors and hospitals. |
| Eamranond et al. [56] | Quality improvement culture; strong leadership team; training; stakeholders’ involvement; organisational stability; deployment strategy; metric of measurement; and reward systems. |
| Henrique et al. [57] | Audit process; competition programs; work standards; A3 method; KPIs; Kaizen event; visual management; Gemba walks; VSM; structured approach; deployment strategy; training; follow-up; effective communication; continuous improvement culture; data-based decisions; aligning project goals with strategic objectives; risk analysis and piloting; information; involvement of physicians; top management involvement; involvement of health professionals; IT support; dedicated implementation team; and effective leadership. |
| Khorasani et al. [58] | Supply chain management; leadership; top management involvement; and organisational culture. |
| Hutton et al. [59] | Top management support; availability of data; voice of the customer; technology; human availability; and education. |
| Isack et al. [60] | Top management involvement; adequate training and proper planning; learning organisation; effective change management; internal and external customer satisfaction; and dissemination of Lean thinking culture in the organisation. |
| Narayanamurthy et al. [61] | A well-defined framework; dedicated team; training and education; value stream analysis; waste audit; and rigorous follow-up. |
| Polanski et al. [62] | Continuous improvement; and process optimisation. |
| McGrath et al. [63] | Involvement of patient and all relevant stakeholders; and sustainment strategies. |
| Ryan et al. [64] | Teamwork; and involvement of patients. |
| Al-Hinai and Shamsuzzoha [65] | Working environment; HR management, supply chain management; and sustainment plans. |
| Chang et al. [66] | Training; technology application; quality of service; and understanding process. |
| Gao et al. [67] | Strong leadership, training, time management, and teamwork. |
| Slade et al. [68] | Organisational culture; leadership; teamwork; staff involvement; effective communication; and HR policies. |
| Hundal et al. [69] | VSM, data analytics; and FMEA. |
| Lee et al. [70] | Multidimensional cultural orientations; patient involvement; and a structured approach. |
| Ramori et al. [71] | Business strategy; organisational design and structure; quality culture; understanding entire value stream; trust; mindfulness; needfulness; respectful, interaction, diverse team: social and task relatedness; effective communication; data availability; and leadership. |
| Taner et al. [72] | Lack of respect among the employees working in the sector; lack of teamwork; and lack of education (awareness of the methodology and the application of Lean tools). High workload and operational improvement are not a priority. |
| Laureani et al. [73] | Top management support; commitment of staff; regular communication with stakeholders; involvement of physicians; and clear project objectives. |
| Taner [74] | Education and training; organisational commitment; and tracking and reporting. |
| Taner et al. [74] | Extensive training of professionals; specialised training; and qualified professionals. |
| Ker et al. [75] | Use of digital technology; design of prescription system and workflow; and managing waste in the workflow. |
| Lorden et al. [76] | Communication; leadership; and workload. |
| Hicks et al. [77] | Engagement with stakeholders; and simulation. |
| Sanders and Karr [78] | Manager commitment; physician leadership; staff commitment; motivation; and training. |
| Chiarini and Baccarani [79] | Top management commitment; and investment and infrastructure. |
| Jayasinha [80] | Better communications; stakeholder engagement; and waste audit. |
| Jorma et al. [81] | Robust data; management and employee commitment; resource allocation; workload management; training; and communication. |
| Matthias and Brown [82] | Structured approach; cultural transformation; and deployment strategies. |
| Nayar et al. [83] | Innovative culture; education; redesign the process; and outreach to community providers. |
| Doğan and Unutulmaz [84] | Standardisation of operations; learning organisation; and training. |
| Ramadan et al. [85] | Top management support; people involvement; operational awareness; improvement culture; quality focus; and accreditation. |
| Barnabè and Giorgino [86] | A systemic approach to knowledge sharing; group decision making; and policy deployment strategies. |
| Kuwaiti and Subbarayalu [87] | Understanding of tools and techniques. |
| Nabelsi and Gagnon [88] | Managing the supply chain; project management; simulation and piloting; structured risk analysis; and measurable performance metrics. |
| Stelson et al. [89] | Managerial decisions; communication; and project management. |
| Deara et al. [90] | Use of proven methods; supportive organisations; stakeholders’ involvement; setting clear goals and objectives; financial support; project management; effective governance; competent project teams; commitment to success; aligned supply chains; appropriate standards; and capable sponsors. |
| Elamir [91] | Leadership; nurse and physician’ involvement; multidisciplinary team; and training. |
| Ingelsson et al [92] | Adapting a Lean leadership-training program within a health care organisation |
| Swarnaker al [93] | Importance of prioritization of critical success factors for sustainable Lean Six Sigma implementation in Indian healthcare organisations |
| Rad [94] | Leadership and management; strategic planning; focus on customer and market; focus on employees; focus on suppliers, material resources, process management; and performance results. |
| Almutairi et al. [95] | Teamwork; patient orientation; organisational culture; consumer relationship; supplier relationship; hospital supply chain processes; and human resources. |
| Almutairi et al. [95] | Hospital leadership; organisational vision and strategic goals; organisational culture; streamlining business process; customer relationship; and supplier relationship. |
| Davies et al. [96] | Teamwork, organisational culture, and understanding of tools and techniques. |
| Isfahani et al. [97] | Teamwork; structured methodology; and management commitment. |
| Kaswan et al. [98] | Involvement of everyone in the organisation; top management support; relationship between supplier and hospital; quality circle; and teamwork. |
3.3. Challenges
| Authors | Challenges |
|---|---|
| McDermott et al. [1] | Clinical staff are not trained in Lean thinking. |
| Trakulsunti and Antony [4] | Effective coaching and mentoring of Lean projects due to a lack of or no project champions in place. |
| Burgess and Radnor [19] | Implementation tends to be isolated rather than system-wide; Lean focuses on tools but fails to address its less-visible strategic elements and enabling factors relating to leadership and organisational readiness. |
| Woodnut [28] | Ambiguity in definition and implementation has contributed to the erosion of system-wide Lean implementation in many healthcare units. |
| Bowerman et al. [30] | Absence of baseline data for process improvement; psychology of the workforce towards change (receptiveness to change). |
| Lima et al. [32] | Excess of bureaucracy in the hospital field because of regulations, protocols, etc.; resistance to work standardisation by physicians. |
| Kahm and Ingelsson [32] | Insecurity about implementation in practice; lack of understanding of the underlying principles of Lean. |
| Roemeling et al. [33] | No standard definition of Lean across the workforce, and implementation becomes a big challenge. |
| Niemeijer et al. [41] | Lack of project management skills; silo mentality across the organisation. |
| Swarnakar et al. [45] | Lack of reward and recognition system, which leads to poor motivation to pursue Lean. |
| Abdallah [46] | Low employee morale is a challenge in the healthcare sector; as physicians have more power than many employees in a hospital sector, managers struggle to persuade the use of process improvement initiatives such as Lean. |
| Peimbert-García et al. [54] | Lack of resources (workforce, financial, time, etc.). |
| Peimbert-García et al. [54] | Lack of training or inadequate training. |
| Peimbert-García et al. [54] | Resistance to cultural change with new initiatives (being complacent with the current culture). |
| Peimbert-García et al. [54] | Lack of employee commitment. |
| Narayanamurthy et al. [61] | Absence of a lean readiness framework and lack of organisational readiness culture. |
| Mcgrath et al. [63] | Lack of or no sustainability component considered in the initiative (i.e., the sustainability of improvement). |
| Taner et al. [72] | Lack of respect among the employees working in the sector; lack of teamwork; and lack of education (awareness of the methodology and the application of Lean tools). High workload and operational improvement are not a priority. |
| Laureani et al. [73] | Budget constraints. |
| Jorma et al. [81] | Understanding process metrics (what to measure and how to measure accurately) has been challenging in many hospitals. |
| Sanders and Karr [84] | Low level of initial trust among employees to adopt Lean across the organisation. |
| Ramadan and Arafeh [85] | Senior managers do not dedicate resources to quality improvement, and quality improvement practices are primitive and superficial; lack of communication or poor communication between Lean professionals and staff in the hospital setting (nurses, doctors, clinicians, etc.). |
| Jayasinha [86] | Lack of automation. |
| Almutairi et al. [95] | Lack of commitment from senior management; poor leadership. |
| Elbireer et al. [99] | Processes are human-driven with some automation, which results in high-output variability. |
3.4. Tools Used
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McDermott, O.; Antony, J.; Douglas, J. Exploring the Use of Operational Excellence Methodologies in the Era of COVID-19: Perspectives from Leading Academics and Practitioners. TQM J. 2021. ahead-of-print. [Google Scholar] [CrossRef]
- Bhat, S.; Antony, J.; Gijo, E.V.; Cudney, E.A. Lean Six Sigma for the Healthcare Sector: A Multiple Case Study Analysis from the Indian Context. Int. J. Qual. Reliab. Manag. 2019, 37, 90–111. [Google Scholar] [CrossRef]
- Ricciardi, C.; Balato, G.; Romano, M.; Santalucia, I.; Cesarelli, M.; Improta, G. Fast Track Surgery for Knee Replacement Surgery: A Lean Six Sigma Approach. TQM J. 2020, 32, 461–474. [Google Scholar] [CrossRef]
- Trakulsunti, Y.; Antony, J.; Edgeman, R.; Cudney, B.; Dempsey, M.; Brennan, A. Reducing Pharmacy Medication Errors Using Lean Six Sigma: A Thai Hospital Case Study. TQM J. 2021, 33, 664–682. [Google Scholar] [CrossRef]
- Gijo, E.V.; Antony, J.; Hernandez, J.; Scaria, J. Reducing Patient Waiting Time in a Pathology Department Using the Six Sigma Methodology. Leadersh. Health Serv. 2013, 26, 253–267. [Google Scholar] [CrossRef]
- Byrne, A.; Womack, J.P. Lean Turnaround; McGraw-Hill: New York, NY, USA, 2012. [Google Scholar]
- George, M.L. Lean Six Sigma: Combining Six Sigma Quality with Lean Production Speed; McGraw-Hill: New York, NY, USA, 2002. [Google Scholar]
- Bhat, S.; Gijo, E.V.; Jnanesh, N.A. Application of Lean Six Sigma methodology in the registration process of a hospital. Int. J. Product. Perform. Manag. 2014, 63, 613–643. [Google Scholar] [CrossRef]
- Antony, J.; Palsuk, P.; Gupta, S.; Mishra, D.; Barach, P. Six Sigma in Healthcare: A Systematic Review of the Literature. Int. J. Qual. Reliab. Manag. 2018, 35, 1075–1092. [Google Scholar] [CrossRef]
- Gonzalez-Aleu, F.; Van Aken, E.M.; Cross, J.; Glover, W.J. Continuous Improvement Project within Kaizen: Critical Success Factors in Hospitals. TQM J. 2018, 30, 335–355. [Google Scholar] [CrossRef]
- Antony, J.; Lancastle, J.; McDermott, O.; Bhat, S.; Parida, R.; Cudney, E. An Evaluation of Lean and Six Sigma Methodologies in the UK National Health Services. Int. J. Qual. Reliab. Manag. 2021. ahead-of-print. [Google Scholar] [CrossRef]
- Albliwi, S.; Antony, J.; Abdul Halim Lim, S.; van der Wiele, T. Critical failure factors of Lean Six Sigma: A systematic literature review. Int. J. Qual. Reliab. Manag. 2014, 31, 1012–1030. [Google Scholar] [CrossRef]
- Noronha, A.; Bhat, S.; Gijo, E.V.; Antony, J.; Laureani, A.; Laux, C. Performance and service quality enhancement in a healthcare setting through lean six sigma strategy. Int. J. Qual. Reliab. Manag. 2021. ahead-of-print. [Google Scholar] [CrossRef]
- McDermott, O.; Antony, J.; Bhat, S.; Jayaraman, R.; Rosa, A.; Marolla, G.; Parida, R. Lean Six Sigma in Healthcare: A Systematic Literature Review on Motivations and Benefits. Processes 2022, 10, 1910. [Google Scholar] [CrossRef]
- Radnor, Z. Transferring Lean into government. J. Manuf. Technol. Manag. 2010, 21, 411–428. [Google Scholar] [CrossRef]
- McDermott, O.; Ronan, L.; Butler, M. A Comparison of Assisted Human Reproduction (AHR) in Ireland with other developed countries. Reprod. Health 2020. preprint. [Google Scholar] [CrossRef]
- Yang, E.C.L.; Khoo-Lattimore, C.; Arcodia, C. A Systematic Literature Review of Risk and Gender Research in Tourism. Tour. Manag. 2017, 58, 89–100. [Google Scholar] [CrossRef]
- Alcaide-Munoz, C.; Gutierrez-Gutierrez, L. Six Sigma and Organisational Ambidexterity: A Systematic Review and Conceptual Framework. Int. J. Lean Six Sigma 2017, 8, 436–456. [Google Scholar] [CrossRef]
- Tranfield, D.; Denyer, D.; Smart, P. Towards a Methodology for Developing Evidence-Informed Management Knowledge by Means of Systematic Review. Br. J. Manag. 2003, 14, 207–222. [Google Scholar] [CrossRef]
- Burgess, K.; Singh, P.J.; Koroglu, R. Supply Chain Management: A Structured Literature Review and Implications for Future Research. Int. J. Oper. Prod. Manag. 2006, 26, 703–729. [Google Scholar] [CrossRef]
- Petticrew, M. Systematic Reviews from Astronomy to Zoology: Myths and Misconceptions. BMJ 2001, 322, 98–101. [Google Scholar] [CrossRef] [PubMed]
- Parameswaran, U.D.; Ozawa-Kirk, J.L.; Latendresse, G. To live (code) or to not: A new method for coding in qualitative research. Qual. Soc. Work 2020, 19, 630–644. [Google Scholar] [CrossRef]
- Chartered Association of Business Schools. Academic Journal Guide. 2018. Available online: https://charteredabs.org/academic-journal-guide-2018/ (accessed on 16 September 2021).
- Vaishnavi, V.; Suresh, M. Modelling of readiness factors for the implementation of Lean Six Sigma in healthcare organisations. Int. J. Lean Six Sigma 2020, 11, 597–633. [Google Scholar] [CrossRef]
- Marolla, G.; Rosa, A.; Giuliani, F. Addressing critical failure factors and barriers in implementing Lean Six Sigma in Italian public hospitals. Int. J. Lean Six Sigma 2021. ahead-of-print. [Google Scholar] [CrossRef]
- Hilton, R.; Balla, M.; Sohal, A.S. Factors critical to the success of a Six-Sigma quality program in an Australian hospital. Total Qual. Manag. Bus. Excell. 2008, 19, 887–902. [Google Scholar] [CrossRef]
- Al Khamisi, Y.N.; Khan, M.K.; Munive-Hernandez, J.E. Knowledge-based lean six sigma system for enhancing quality management performance in healthcare environment. Int. J. Lean Six Sigma 2019, 10, 211–233. [Google Scholar] [CrossRef]
- Woodnutt, S. Is Lean sustainable in today’s NHS hospitals? A systematic literature review using the meta-narrative and integrative methods. Int. J. Qual. Health Care 2018, 30, 578–586. [Google Scholar] [CrossRef] [PubMed]
- Ajmera, P.; Jain, V. A fuzzy interpretive structural modelling approach for evaluating the factors affecting lean implementation in Indian healthcare industry. Int. J. Lean Six Sigma 2020, 11, 376–397. [Google Scholar] [CrossRef]
- Bowerman, J.; Antony, J.; Downey-Ennis, K.; Antony, F.; Seow, C. Can Six Sigma be the ‘cure’ for our ‘ailing’ NHS? Leadersh. Health Serv. 2007, 20, 242–253. [Google Scholar] [CrossRef]
- Feng, Q.; Manuel, C.M. Under the knife: A national survey of six sigma programs in US healthcare organisations. Int. J. Health Care Qual. Assur. 2008, 21, 535–547. [Google Scholar] [CrossRef]
- Kahm, T.; Ingelsson, P. Creating a development force in Swedish healthcare: A focus on the first-line managers’ perspective when applying Lean. Int. J. Health Care Qual. Assur. 2019, 32, 1132–1144. [Google Scholar] [CrossRef]
- Roemeling, O.; Land, M.; Ahaus, K. Does lean cure variability in health care? Int. J. Oper. Prod. Manag. 2017, 37, 1229–1245. [Google Scholar] [CrossRef]
- De Lima, F.R.P.; Da Silva, A.L.; Godinho Filho, M.; Dias, E.M. Systematic Review: Resilience Enablers to Combat Counterfeit Medicines. Supply Chain Manag. Int. J. 2018, 12, 117–135. [Google Scholar] [CrossRef]
- Meyer, M.A. Competencies required for healthcare improvement positions. Int. J. Health Care Qual. Assur. 2019, 32, 281–295. [Google Scholar] [CrossRef]
- Ahmed, S.; Abd Manaf, N.H.; Islam, R. Measuring Lean Six Sigma and quality performance for healthcare organisations. Int. J. Health Care Qual. Serv. Sci. 2018, 10, 267–278. [Google Scholar]
- Hallam, C.R.A.; Contreras, C. Lean healthcare: Scale, scope and sustainability. Int. J. Health Care Qual. 2018, 31, 684–696. [Google Scholar] [CrossRef]
- Holden, R.J.; Hackbart, G. From group work to teamwork: A case study of ‘Lean’ rapid process improvement in the ThedaCare Information Technology Department. IIE Trans. Healthcare Syst. Eng. 2012, 2, 190–201. [Google Scholar] [CrossRef]
- Dannapfel, P.; Poksinska, B.; Thomas, K. Dissemination strategy for Lean thinking in health care. Int. J. Health Care Qual. 2014, 27, 391–404. [Google Scholar] [CrossRef]
- Deblois, S.; Lepanto, L. Lean and Six Sigma in acute care: A systematic review of reviews. Int. J. Health Care Qual. Assur. 2016, 29, 192–208. [Google Scholar] [CrossRef]
- Honda, A.C.; Bernardo, V.Z.; Gerolamo, M.C.; Davis, M.M. How lean six sigma principles improve hospital performance. Qual. Manag. J. 2018, 25, 70–82. [Google Scholar] [CrossRef]
- Niemeijer, G.C.; Does, R.J.; de Mast, J.; Trip, A.; van den Heuvel, J. Generic project definitions for improvement of health care delivery: A case-based approach. Qual. Manag. Health Care 2011, 20, 152–164. [Google Scholar] [CrossRef]
- McIntosh, B.; Sheppy, B.; Ivan, C. Illusion or delusion—Lean management in the health sector. Int. J. Health Care Qual. Assur. 2014, 27, 482–492. [Google Scholar] [CrossRef]
- Ulhassan, W.; Sandahl, C.; Westerlund, H.; Henriksson, P.; Bennermo, M.; Von Thiele Schwarz, U.; Thor, J. Antecedents and characteristics of lean thinking implementation in a Swedish hospital: A case study. Qual. Manag. Health Care 2013, 22, 48–61. [Google Scholar] [CrossRef]
- Leite, H.; Lindsay, C.; Kumar, M. COVID-19 outbreak: Implications on healthcare operations. TQM J. 2021, 33, 247–256. [Google Scholar] [CrossRef]
- Swarnakar, V.; Bagherian, A.; Singh, A.R. Modeling Critical Success Factors for Sustainable LSS Implementation in Hospitals: An Empirical Study. Int. J. Qual. Reliab. Manag. 2021. ahead-of-print. [Google Scholar] [CrossRef]
- Abdallah, A. Implementing quality initiatives in healthcare organisations: Drivers and challenges. Int. J. Health Care Qual. Assur. 2014, 27, 166–181. [Google Scholar] [CrossRef]
- Hung, D.; Martinez, M.; Yakir, M.; Gray, C. Implementing a Lean Management System in Primary Care: Facilitators and Barriers from the Front Lines. Qual. Manag. Health Care 2015, 24, 103–108. [Google Scholar] [CrossRef]
- Gowen, C.R.; Mcfadden, K.L.; Hoobler, J.M.; Tallon, W.J. Exploring the efficacy of healthcare quality practices, employee commitment, and employee control. J. Oper. Manag. 2006, 24, 765–778. [Google Scholar] [CrossRef]
- Robbins, J.; Garman, A.N.; Song, P.H.; McAlearney, A.S. How high-performance work systems drive health care value: An examination of leading process improvement strategies. Qual. Manag. Health Care 2012, 21, 188–202. [Google Scholar] [CrossRef]
- Steed, A. An exploration of the leadership attributes and methods associated with successful lean system deployments in acute care hospitals. Qual. Manag. Health Care 2012, 21, 48–58. [Google Scholar] [CrossRef]
- Dobrzykowski, D.D.; McFadden, K.L.; Vonderembse, M.A. Examining pathways to safety and financial performance in hospitals: A study of lean in professional service operations. J. Oper. Manag. 2016, 42, 39–51. [Google Scholar] [CrossRef]
- Walley, P.; Found, P.; Williams, S. Failure demand: A concept evaluation in UK primary care. Int. J. Health Care Qual. Assur. 2019, 32, 21–33. [Google Scholar] [CrossRef]
- Peimbert-García, R.E. Analysis and Evaluation of Reviews on Lean and Six Sigma in Health Care. Qual. Manag. Health Care 2019, 28, 229–236. [Google Scholar] [CrossRef]
- Dobrzykowski, D.D.; McFadden, K.L. Examining Governance in Hospital Operations: The Effects of Trust and Physician Employment in Achieving Efficiency and Patient Satisfaction. Decis. Sci. 2020, 51, 74–109. [Google Scholar] [CrossRef]
- Eamranond, P.P.; Bhukhen, A.; DiPalma, D.; Kunuakaphun, S.; Burke, T.; Rodis, J.; Grey, M. Interprofessional, multitiered daily rounding management in a high-acuity hospital. Int. J. Health Care Qual. Assur. 2020, 33, 447–461. [Google Scholar] [CrossRef]
- Henrique, D.B.; Filho, M.G.; Marodin, G.; de Sousa Jabbour, A.B.L.; Jabbour, C.J.C. A framework to assess sustaining continuous improvement in lean Healthcare. Int. J. Prod. Res. 2021, 59, 2885–2904. [Google Scholar] [CrossRef]
- Khorasani, S.T.; Cross, J.; Maghazei, O. Lean supply chain management in Healthcare: A systematic review and meta-study. Int. J. Lean Six Sigma 2020, 11, 1–34. [Google Scholar] [CrossRef]
- Hutton, S.A.; Vance, K.; Burgard, J.; Grace, S.; Van Male, L. Workplace violence prevention standardisation using lean principles across a healthcare network. Int. J. Health Care Qual. Assur. 2018, 31, 464–473. [Google Scholar] [CrossRef]
- Isack, H.D.; Mutingi, M.; Kandjeke, H.; Vashishth, A.; Chakraborty, A. Exploring the adoption of Lean principles in medical laboratory industry: Empirical evidences from Namibia. Int. J. Lean Six Sigma 2018, 9, 133–155. [Google Scholar] [CrossRef]
- Narayanamurthy, G.; Gurumurthy, A.; Lankayil, A.A. Experience of implementing lean thinking in an Indian healthcare institution. Int. J. Lean Six Sigma 2018, 12, 23–60. [Google Scholar] [CrossRef]
- Polanski, W.H.K.; Martin, D.; Günther, S.; Schackert, S.; Klingelhoefer, L.; Fauser, M.; Storch, A.; Sobottka, S.B. Application of the Six Sigma concept for quality assessment of different strategies in DBS surgery. Int. J. Qual. Health Care 2018, 30, 760–768. [Google Scholar] [CrossRef]
- McGrath, K.; Casserly, M.; O’mara, F.; Mulsow, J.; Shields, C.; Staunton, O.; Teeling, S.P.; Ward, M. Zap it track it: The application of Lean Six Sigma methods to improve the screening system of low-grade mucinous neoplasms of the appendix in an acute hospital setting. Int. J. Qual. Health Care 2019, 31, 35–44. [Google Scholar] [CrossRef]
- Ryan, P.; McGrath, C.; Lawrie, I.; Fitzsimons, C.; O’Shea, J.; De Brún, A. Enhancing efficiency in a cardiac investigations department by increasing remote patient monitoring. Int. J. Qual. Health Care 2019, 31, 29–34. [Google Scholar] [CrossRef]
- Al-Hinai, N.; Shamsuzzoha, A. Developing a practical methodology to improve the healthcare services: Studying a neonatal intensive care unit case in Oman. Int. J. Qual. Reliab. Manag. 2021, 38, 1425–1442. [Google Scholar] [CrossRef]
- Chang, D.; Leu, J.; Wang, W.; Chen, Y. Improving waiting time for surgical rooms using workflow and the six-sigma method. Total Qual. Manag. Bus. Excell. 2020, 31, 869–886. [Google Scholar] [CrossRef]
- Gao, T.; Zhang, X.; Gurd, B.; Liu, Z. From self-management to a systemised process: The implementation of lean management in a Chinese hospital’s pharmacy intravenous admixture services center. Leadersh. Health Serv. 2020, 33, 325–337. [Google Scholar] [CrossRef]
- Slade, J.J.; Wrzesniewski, C.E.; Hunter, O.O.; Allaudeen, N. Complementing Root Cause Analysis with Improvement Strategies to Optimise Venous Thromboembolism Prophylaxis in Patients with Epidural Catheters. Qual. Manag. Health Care 2020, 29, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Hundal, G.S.; Thiyagarajan, S.; Alduraibi, M.; Laux, C.M.; Furterer, S.L.; Cudney, E.A.; Antony, J. Lean Six Sigma as an organisational resilience mechanism in health care during the era of COVID-19. Int. J. Lean Six Sigma 2021, 12, 762–783. [Google Scholar] [CrossRef]
- Lee, J.Y.; McFadden, K.L.; Lee, M.K.; Gowen, C.R. US hospital culture profiles for better performance in patient safety, patient satisfaction, Six Sigma, and lean implementation. Int. J. Prod. Econ. 2021, 234, 108047. [Google Scholar] [CrossRef]
- Ramori, K.A.; Cudney, E.A.; Elrod, C.C.; Antony, J. Lean business models in Healthcare: A systematic review. Total Qual. Manag. Bus. Excell. 2021, 32, 558–573. [Google Scholar] [CrossRef]
- Taner, M.T.; Sezen, B.; Atwat, K.M. Application of Six Sigma methodology to a diagnostic imaging process. Int. J. Health Care Qual. Assur. 2012, 25, 274–290. [Google Scholar] [CrossRef]
- Laureani, A.; Brady, M.; Antony, J. Applications of Lean Six Sigma in an Irish hospital. Leadersh. Health Serv. 2013, 26, 322–337. [Google Scholar] [CrossRef]
- Taner, M.T. Application of Six Sigma methodology to a cataract surgery unit. Int. J. Health Care Qual. Assur. 2013, 26, 768–785. [Google Scholar] [CrossRef] [PubMed]
- Ker, J.; Wang, Y.; Hajli, M.N.; Song, J.; Ker, C.W. Deploying lean in Healthcare: Evaluating information technology effectiveness in US hospital pharmacies. Int. J. Inf. Manag. 2014, 34, 556–560. [Google Scholar] [CrossRef]
- Lorden, A.L.; Zhang, Y.; Lin, S.; Côté, M.J. Measures of Success: The Role of Human Factors in Lean Implementation in Healthcare. Qual. Manag. J. 2014, 21, 26–37. [Google Scholar] [CrossRef]
- Hicks, S.; McGovern, T.; Prior, G.; Smith, I. Applying lean principles to the design of healthcare facilities. Int. J. Prod. Econ. 2015, 170, 677–686. [Google Scholar] [CrossRef]
- Sanders, J.H.; Karr, T. Improving ED specimen TAT using Lean Six Sigma. Int. J. Health Care Qual. Assur. 2015, 28, 428–440. [Google Scholar] [CrossRef]
- Chiarini, A.; Baccarani, C. TQM and lean strategy deployment in Italian hospitals: Benefits related to patient satisfaction and encountered pitfalls. Leadersh. Health Serv. 2016, 29, 377–391. [Google Scholar] [CrossRef]
- Jayasinha, Y. Decreasing turnaround time and increasing patient satisfaction in a safety net hospital-based pediatrics clinic using lean six sigma methodologies. Qual. Manag. Health Care 2016, 25, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Jorma, T.; Tiirinki, H.; Bloigu, R.; Turkki, L. Lean thinking in Finnish Healthcare. Leadersh. Health Serv. 2016, 29, 9–36. [Google Scholar] [CrossRef]
- Matthias, O.; Brown, S. Implementing operations strategy through Lean processes within health care: The example of NHS in the UK. Int. J. Oper. Prod. Manag. 2016, 36, 1435–1457. [Google Scholar] [CrossRef]
- Nayar, P.; Ojha, D.; Fetrick, A.; Nguyen, A.T. Applying Lean Six Sigma to improve medication management. Int. J. Health Care Qual. Assur. 2016, 29, 16–23. [Google Scholar] [CrossRef]
- Doğan, N.O.; Unutulmaz, O. Lean production in Healthcare: A simulation-based value stream mapping in the physical therapy and rehabilitation department of a public hospital. Total Qual. Manag. Bus. Excell. 2016, 27, 64–80. [Google Scholar] [CrossRef]
- Ramadan, N.; Arafeh, M. Healthcare quality maturity assessment model based on quality drivers. Int. J. Health Care Qual. Assur. 2016, 29, 337–350. [Google Scholar] [CrossRef]
- Barnabè, F.; Giorgino, M.C. Practicing Lean strategy: Hoshin Kanri and X-Matrix in a healthcare-centered simulation. TQM J. 2017, 29, 590–609. [Google Scholar] [CrossRef]
- Kuwaiti, A.A.; Subbarayalu, A.V. Reducing patients’ falls rate in an Academic Medical Center (AMC) using Six Sigma “DMAIC” approach. Int. J. Health Care Qual. Assur. 2017, 30, 373–384. [Google Scholar] [CrossRef]
- Nabelsi, V.; Gagnon, S. Information technology strategy for a patient-oriented, lean, and agile integration of hospital pharmacy and medical equipment supply chains. Int. J. Prod. Res. 2017, 55, 3929–3945. [Google Scholar] [CrossRef]
- Stelson, P.; Hille, J.; Eseonu, C.; Doolen, T. What drives continuous improvement project success in healthcare? Int. J. Health Care Qual. Assur. 2017, 30, 43–57. [Google Scholar] [CrossRef]
- Deara, A.; Deara, M.; Bamber, C.; Elezi, E. A comparative analysis of lean implementations in NHS England hospitals. Int. J. Lean Enterp. Res. 2018, 2, 218–239. [Google Scholar] [CrossRef]
- Elamir, H. Improving patient flow through applying lean concepts to emergency department. Leadersh. Health Serv. 2018, 31, 293–309. [Google Scholar] [CrossRef]
- Ingelsson, P.; Bäckström, I.; Snyder, K. Adapting a Lean leadership-training program within a health care organisation through co-creation. Int. J. Qual. Serv. Sci. 2020, 12, 15–28. [Google Scholar]
- Swarnakar, V.; Bagherian, A.; Singh, A.R. Prioritization of critical success factors for sustainable Lean Six Sigma implementation in Indian healthcare organisations using best-worst-method. TQM J. 2022. ahead-of-print. [Google Scholar] [CrossRef]
- Rad, M.M.A. A survey of total quality management in Iran: Barriers to successful implementation in health care organisations. Leadersh. Health Serv. 2005, 18, 12–34. [Google Scholar]
- Almutairi, A.M.; Salonitis, K.; Al-Ashaab, A. Assessing the leanness of a supply chain using multi-grade fuzzy logic: A healthcare case study. Int. J. Lean Six Sigma 2019, 10, 81–105. [Google Scholar] [CrossRef]
- Davies, C.; Lyons, C.; Whyte, R. Optimising nursing time in a day care unit: Quality improvement using Lean Six Sigma methodology. Int. J. Qual. Health Care 2019, 31, 22–28. [Google Scholar] [PubMed]
- Isfahani, M.; Tourani, H.S.; Seyedin, H. Lean management approach in hospitals: A systematic review. Int. J. Lean Six Sigma 2019, 10, 161–188. [Google Scholar] [CrossRef]
- Kaswan, M.S.; Rathi, R.; Singh, M. Just in the decision-making approach, extraction and prioritisation of the health care unit. Int. J. Qual. Reliab. Manag. 2019, 36, 1243–1263. [Google Scholar] [CrossRef]
- Elbireer, A.; le Chasseur, J.; Jackson, B. Improving laboratory data entry quality using Six Sigma. Int. J. Health Care Qual. Assur. 2013, 26, 496–509. [Google Scholar] [CrossRef]
- Yadav, N.; Shankar, R.; Singh, S.P. Hierarchy of Critical Success Factors (CSF) for Lean Six Sigma (LSS) in Quality 4.0. Int. J. Global Bus. Compet. 2021, 16, 1–14. [Google Scholar] [CrossRef]
| Tools/Techniques | Lean | Six Sigma | Lean Six Sigma |
|---|---|---|---|
| Process mapping | X | X | X |
| Value stream mapping | X | X | |
| Ishikawa/fishbone diagram | X | X | X |
| Checklist | X | ||
| Pareto chart | X | X | |
| Failure mode effect analysis | X | X | |
| Decision trees | X | X | |
| Hazard analysis | X | ||
| Balanced scorecard | X | X | |
| 5S (sort-set in order-shine-standardize-sustain) | X | X | |
| SIPOC (supplier, input, process, output, customer) | X | X | |
| PDCA/PDSA | X | ||
| Kaizen | X | ||
| DMAIC/DMADV | X | X | |
| Poke-yoke | X | X | |
| Spaghetti chart | X | X | X |
| A3 report | X | ||
| Quality function deployment | X | X | |
| Gemba walks | X | X | |
| Brainstorming | X | X | X |
| Runs chart | X | X | |
| Heijunka | X | ||
| Cycle time/Takt time/workload balance | X | X | |
| Hoshin Kanri | X | X | X |
| Kata | X | ||
| Voice of the customer | X | X | X |
| Process capability analysis | X | X | |
| Control charts | X | X | |
| Statistical process control | X | X | |
| Design of experiments | X | X |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McDermott, O.; Antony, J.; Bhat, S.; Jayaraman, R.; Rosa, A.; Marolla, G.; Parida, R. Lean Six Sigma in Healthcare: A Systematic Literature Review on Challenges, Organisational Readiness and Critical Success Factors. Processes 2022, 10, 1945. https://doi.org/10.3390/pr10101945
McDermott O, Antony J, Bhat S, Jayaraman R, Rosa A, Marolla G, Parida R. Lean Six Sigma in Healthcare: A Systematic Literature Review on Challenges, Organisational Readiness and Critical Success Factors. Processes. 2022; 10(10):1945. https://doi.org/10.3390/pr10101945
Chicago/Turabian StyleMcDermott, Olivia, Jiju Antony, Shreeranga Bhat, Raja Jayaraman, Angelo Rosa, Giuliano Marolla, and Ratri Parida. 2022. "Lean Six Sigma in Healthcare: A Systematic Literature Review on Challenges, Organisational Readiness and Critical Success Factors" Processes 10, no. 10: 1945. https://doi.org/10.3390/pr10101945
APA StyleMcDermott, O., Antony, J., Bhat, S., Jayaraman, R., Rosa, A., Marolla, G., & Parida, R. (2022). Lean Six Sigma in Healthcare: A Systematic Literature Review on Challenges, Organisational Readiness and Critical Success Factors. Processes, 10(10), 1945. https://doi.org/10.3390/pr10101945











