Lean Six Sigma in Healthcare: A Systematic Literature Review on Motivations and Benefits
Abstract
:1. Introduction
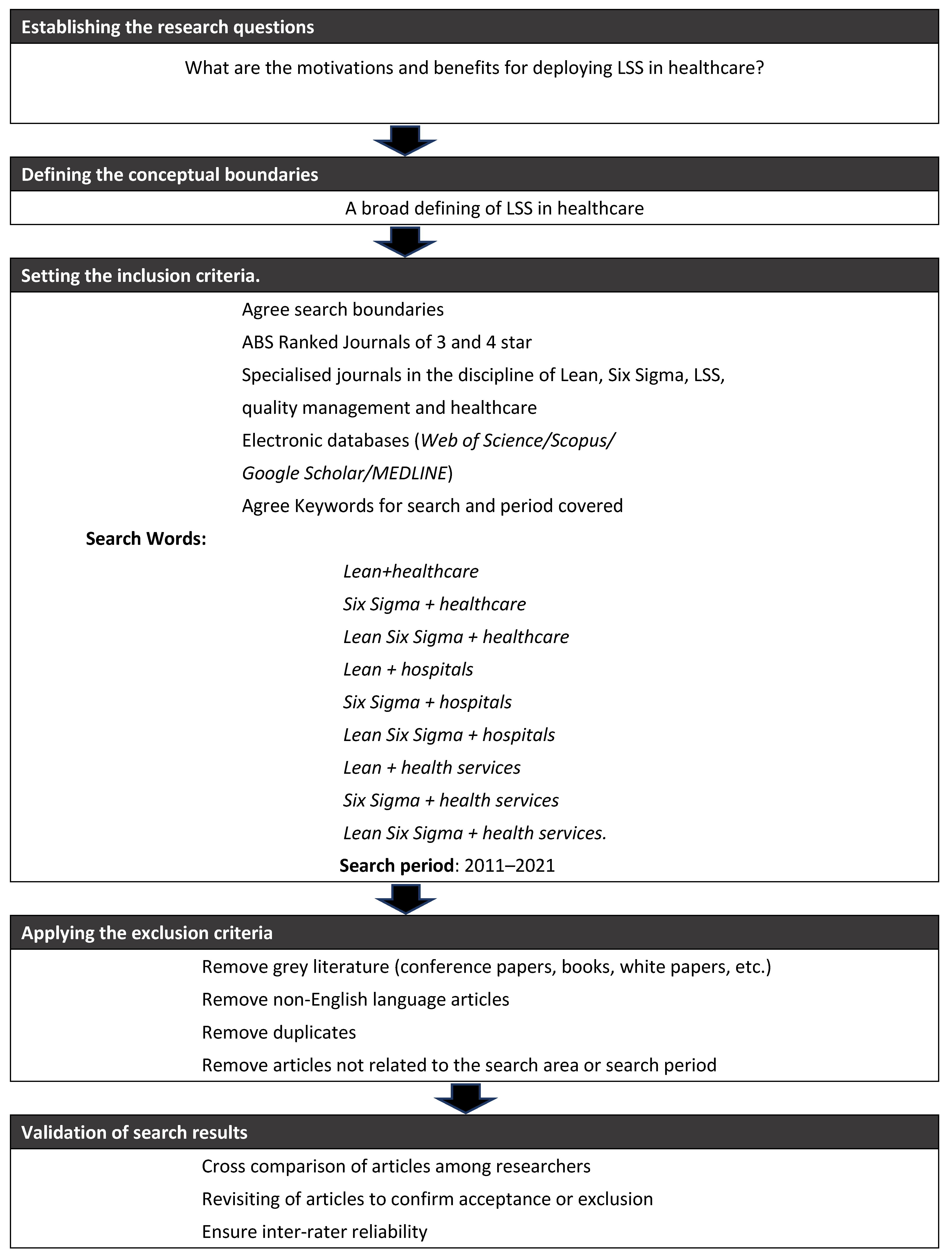
2. Research Methodology
3. Results
3.1. Publications Timeline
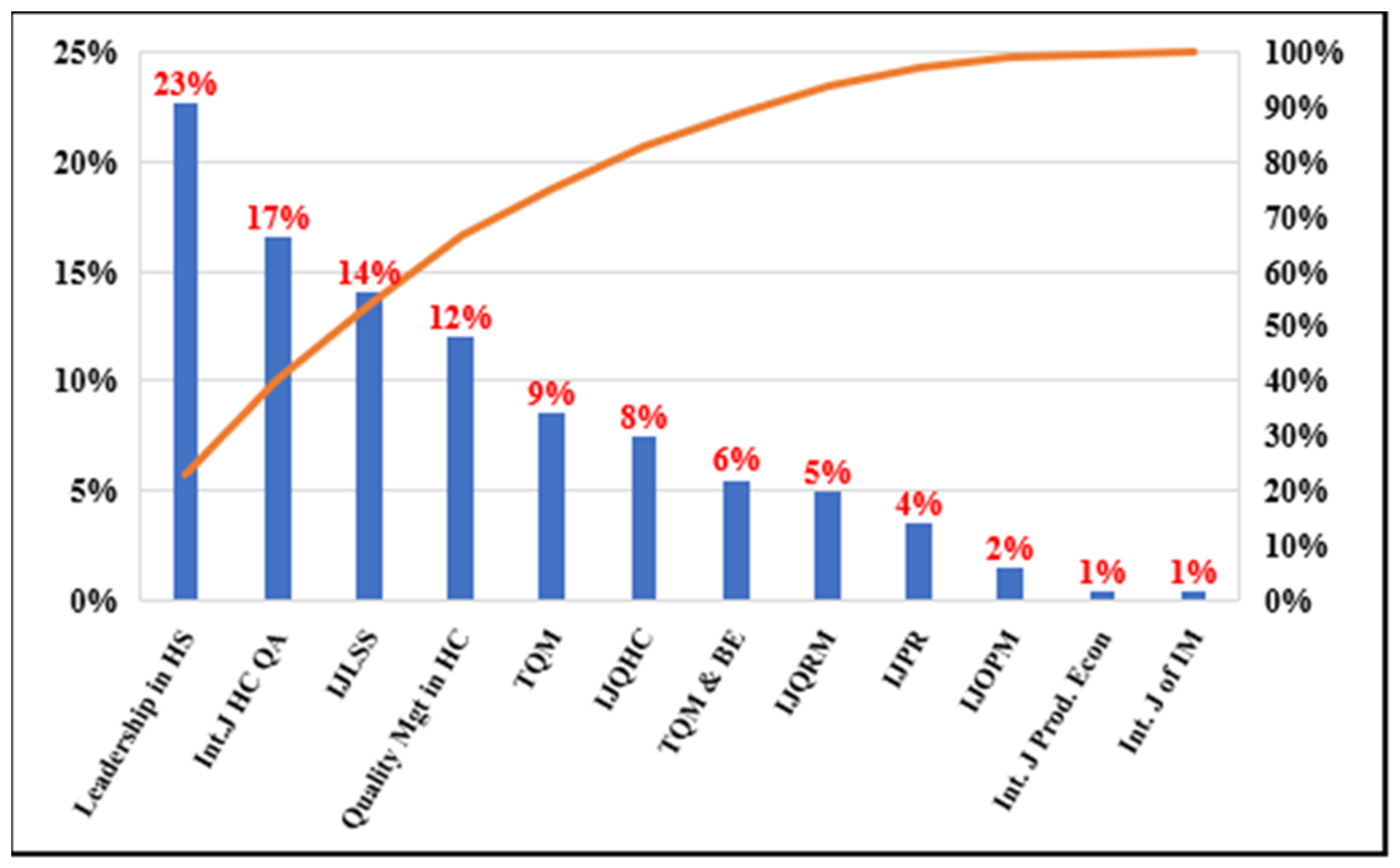
3.1.1. Publications by Journal
3.1.2. The Motivational Factors
| Authors | Motivating Factors to Adopt LSS |
|---|---|
| Holden and Hackbart (2012) [34] | Manage the implementation of I.T. solutions and new technologies. Understand customer needs. Will need the leadership to improve process. |
| Feng and Manuel (2008) [37] | Six Sigma is a ready-to-implement choice if an organisation is trying to adopt a data-driven, systematic approach to process improvement. High return on investment (ROI) is the most relevant motivation for organisations committed to implementing Lean Six Sigma with a top-down approach. |
| Gowen, et al. (2006) [38] | The authors discuss qualitative and quantitative motivations. Quantitative motivations are quality improvement, increased customer satisfaction, net cost savings, decreased error frequency and reduced severity. Qualitative motivation is increased understanding of errors, heightened awareness of errors and reduced impact of errors. |
| Taner (2013) [39] | Staff had complained about the hospital cataract unit’s image as perceived by Turkish society. |
| Bowerman, et al. (2007) [51] | Embrace opportunities for process and organisational improvement. |
| Ballé and Régnier (2007) [52] | Build a learning environment for staff and management. |
| Schattenkirk (2012) [53] | Guide the organisation toward continuous improvement. Create the internal dynamic capacity to deal with continuous improvement. |
| Taner, et al. (2012) [39] | Hospital administration considered the application of Six Sigma to improve clinical process performance. |
| Niemeijer, et al. (2012) [54] | Improve clinical process quality and reduce cost. Senior management decided to use the LSS methodology because there were positive experiences in the hospital. |
| Niemeijer, et al. (2011) [55] | Reduce costs, increase revenues and improve the quality and safety of clinical pathways. |
| Laureani, et al. (2013) [45] | Evaluate the learning outcomes of organisation members who participated in a Master’s program, funded by the organisation, focused on continuous improvement. |
| Nayar, et al. (2016) [56] | Assess the compliance with the hospitals dual care policy. Provide high-quality care and facilitate medication co-management for dual care veterans. |
| Elbireer, et al. (2013) [25] | Effectively address the increased demand challenge because it has increased data entry and triage errors. |
| Ulhassan, et al. (2013) [31] | Effectively adopt Swedish National guidelines of cardiac emergency pathways. Improve patient satisfaction. Managers believe that Lean is a practical approach to improving the organisation’s ability to deal with change. |
| Dannapfel, et al. (2014) [26] | The Lean improvement programme was introduced to tackle challenges such as an ageing society, rising care expectations and budgetary and economic constraints. |
| McIntosh, et al. (2014) [48] | Comply with U.K. National Health Service (NHS) efficiency savings guidelines. Improve patient value. |
| Bowerman, et al. (2007) [50] | Improvement in financial and operational performance. |
| Fillingham (2007) [57] | Productivity improvement, mortality reduction, fast recovery, length of stay |
| Kumar and Steinebach (2008) [58] | Minimised clinical errors in surgical activities, increased the hospital’s profitability overall, and ensured patient safety. |
| Taner, et al. (2012) [59] | Improve high patient safety and diagnostic efficiency. |
| DelliFraine, et al. (2013) [60] | Organisations’ motivations for implementing the methodology are unclear and must be deduced from the methodological implementation choices, the tools used and the stated objectives. Moreover, in many cases, motivations are confused with objectives. |
| Chiarini, et al. (2013) [61] | Improved lead time from the emergency department to hospitalisation or discharge. |
| Hicks, et al. (2015) [62] | Develop a new endoscopy facility on an existing site that fully complied with the Joint Advisory Group requirements (JAG, 2011) and would likely score highly in the global rating scale (GRS) standards. |
| Crema and Verbano (2015) [46] | Improve the effectiveness of clinical risk management. |
| Jayasinha (2016) [47] | Increase the quality provided to the patients. |
| Dobrzykowski, et al. (2016) [32] | Reach internal processes integration. Cost reduction. |
| Matthias and Brown (2016) [40] | Lean projects are motivated to improve performance and comply with national regulations and guidelines. |
| Deblois and Lepanto (2016) [35] | Process improvement tends to emerge as the primary purpose justifying the implementation of Lean in the healthcare sector. |
| Roemeling, et al. (2017) [27] | Address the challenges of increasing demands for excellent performance. |
| Crema and Verbano (2017) [44] | Lean healthcare management (LHM) can support Choosing Wisely implementation. |
| Polanski, et al. (2018) [63] | Define a standardised and validated outcome analysis method. |
| Trakulsunti and Antony (2018) [3] | Top management vision. Leaders realise the opportunities arising from business process re-engineering and the culture of continuous change. |
| Isack, et al. (2018) [42] | Effectively respond to the pressure from national authorities. Two categories of reasons co-exist: proactive (i.e., self-desire by the company) and reactive (response to customer requirements and threats, whereby failure to comply may result in adverse effects). Internal motivators (i.e., safe working conditions, reasonable salary and job rotation) are used more than external motivators (rewards and performance review) to motivate employees. |
| Woodnutt (2018) [24] | NHS hospitals adopt several quality improvement ideologies, often originally described or discovered outside the health sector, to address the crisis in funding and efficiency. |
| Hallam and Contreras (2018) [64] | Address the demands for higher quality standards associated with the increased demand. |
| Ahmed, et al. (2018) [39] | Private hospital staff are more motivated than public hospital staff to implement Lean management initiatives, Six Sigma initiatives, patient safety and teamwork because staff perceive these paradigms and tools as more favourable. |
| Peimbert-García, et al. (2019) [28] | Lean implementation is motivated by the desire to increase the safety and quality of patient care (the financial motivation is also present, but it has less effect on adopting the methodology). |
| Kahm and Ingelsson (2019) [65] | Drive quality and safety process improvements. |
| Ahmed, et al. (2019) [21] | Improve the quality performance of hospitals. |
| Ryan, et al. (2019) [66] | Design new processes that incorporate innovative solutions for remote patient monitoring. |
| Ahmed, et al. (2019) [21] | Ensure compliance with national regulations and guidelines, i.e., The Care Quality Commission (CQC) and NHS Foundation Trust (F.T.). Benchmarking. Address financial difficulty or crisis. |
| Walley, et al. (2019) [29] | Reduce primary care system costs, overproduction and errors in managing patient flow. |
| Antony, et al. (2019) [67] | Explore opportunities to improve the quality of clinical pathways. |
| Slade, et al. (2020) [68] | Adopt best practices provided by national agency guidelines. |
| Gao, et al. (2020) [22] | Address the request of the Chinese government that creates significant demands for improving efficiency and effectiveness. |
| Eamranond, et al. (2020) [69] | Improve clinical process safety using the implementation of interprofessional, multitiered Lean daily management (LDM). |
| Bhat, et al. (2020) [1] | The desire to experiment with models for process optimisation was the key motivation. Subsequently, successful pilots, processes, and organisation-wide benefits prompted the organisation to commit to implementing the LSS model at the macro level. |
| Leite, et al. (2021) [70] | Adopt models that provide organisations with the tools to deal with emergencies effectively. |
| Swarnakar, et al. (2021) [23] | The hospital management was motivated to improve the service quality and reduce the harmful wastes that impact society and the environment. In addition, hospital managers were highly motivated to adopt effective techniques to overcome patient waiting time and waste disposal problems. |
| Narayanamurthy, et al. (2018a) [30] | The adoption of Lean is motivated by the quantum of benefits harvested by several hospitals in developed countries. |
| Lima, et al. (2021) [20] | Lean is considered a key factor in driving business strategies, reducing costs, improving patient value, and enhancing the quality and safety of business processes. |
| Ramori, et al. (2021) [34] | Reduce waste and costs and improve overall patient care and satisfaction. Sustain competitive advantage for accountable care organisations. |
| Hundal, et al. (2021) [71] | The key motivation is personal safety, followed by process redesign and effective implementation of telemedicine. |
3.1.3. Benefits of Deploying LSS in Healthcare
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Bhat, S.; Antony, J.; Gijo, E.V.; Cudney, E.A. Lean Six Sigma for the Healthcare Sector: A Multiple Case Study Analysis from the Indian Context. Int. J. Qual. Reliab. Manag. 2019, 37, 90–111. [Google Scholar] [CrossRef]
- McDermott, O.; Antony, J.; Douglas, J. Exploring the Use of Operational Excellence Methodologies in the Era of COVID-19: Perspectives from Leading Academics and Practitioners. TQM J. 2021, 33, 1647–1665. [Google Scholar] [CrossRef]
- Trakulsunti, Y.; Antony, J.; Edgeman, R.; Cudney, B.; Dempsey, M.; Brennan, A. Reducing Pharmacy Medication Errors Using Lean Six Sigma: A Thai Hospital Case Study. Int. J. Qual. Reliab. Manag. 2021, 33, 1–19. [Google Scholar] [CrossRef]
- Ricciardi, C.; Balato, G.; Romano, M.; Santalucia, I.; Cesarelli, M.; Improta, G. Fast Track Surgery for Knee Replacement Surgery: A Lean Six Sigma Approach. TQM J. 2020, 32, 461–474. [Google Scholar] [CrossRef]
- Antony, J.; Palsuk, P.; Gupta, S.; Mishra, D.; Barach, P. Six Sigma in Healthcare: A Systematic Review of the Literature. Int. J. Qual. Reliab. Manag. 2018, 35, 1075–1092. [Google Scholar] [CrossRef]
- Gijo, E.V.; Antony, J.; Hernandez, J.; Scaria, J. Reducing Patient Waiting Time in a Pathology Department Using the Six Sigma Methodology. Leadersh. Health Serv. 2013, 26, 253–267. [Google Scholar] [CrossRef]
- Byrne, A.; Womack, J.P. Lean Turnaround; McGraw-Hill: New York, NY, USA, 2012. [Google Scholar]
- George, M.L. Lean Six Sigma: Combining Six Sigma Quality with Lean Production Speed; McGraw-Hill: New York, NY, USA, 2002. [Google Scholar]
- Bhat, S.; Gijo, E.V.; Antony, J.; Cross, J. Strategies for successful deployment and sustainment of Lean Six Sigma in the healthcare sector in India: A multi-level perspective. TQM J. 2022. ahead-of-print. [Google Scholar] [CrossRef]
- Sloan, T.; Fitzgerald, A.; Hayes, K.J.; Radnor, Z.; Robinson, S.; Sohal, A. Lean in healthcare–history and recent developments. J. Health Organ. Manag. 2014, 28, 2. [Google Scholar] [CrossRef]
- Gonzalez-Aleu, F.; Van Aken, E.M.; Cross, J.; Glover, W.J. Continuous Improvement Project within Kaizen: Critical Success Factors in Hospitals. TQM J. 2018, 30, 335–355. [Google Scholar] [CrossRef]
- Antony, J.; Lancastle, J.; McDermott, O.; Bhat, S.; Parida, R.; Cudney, E. An Evaluation of Lean and Six Sigma Methodologies in the U.K. National Health Services. Int. J. Qual. Reliab. Manag. 2021. ahead-of-print. [Google Scholar] [CrossRef]
- Burgess, K.; Singh, P.J.; Koroglu, R. Supply Chain Management: A Structured Literature Review and Implications for Future Research. Int. J. Oper. Prod. Manag. 2006, 26, 703–729. [Google Scholar] [CrossRef]
- Garza-Reyes, J.A. Lean and Green—A Systematic Review of the State of the Art Literature. J. Clean. Prod. 2015, 102, 18–29. [Google Scholar] [CrossRef]
- Alcaide-Munoz, C.; Gutierrez-Gutierrez, L. Six Sigma and Organisational Ambidexterity: A Systematic Review and Conceptual Framework. Int. J. Lean Six Sigma 2017, 8, 436–456. [Google Scholar] [CrossRef]
- Tranfield, D.; Denyer, D.; Smart, P. Towards a Methodology for Developing Evidence-Informed Management Knowledge by Means of Systematic Review. Br. J. Manag. 2003, 14, 207–222. [Google Scholar] [CrossRef]
- Yang, E.C.L.; Khoo-Lattimore, C.; Arcodia, C. A Systematic Literature Review of Risk and Gender Research in Tourism. Tour. Manag. 2017, 58, 89–100. [Google Scholar] [CrossRef]
- Petticrew, M. Systematic Reviews from Astronomy to Zoology: Myths and Misconceptions. BMJ 2001, 322, 98–101. [Google Scholar] [CrossRef]
- Parameswaran, U.D.; Ozawa-Kirk, J.L.; Latendresse, G. To live (code) or to not: A new method for coding in qualitative research. Qual. Soc. Work. 2020, 19, 630–644. [Google Scholar] [CrossRef]
- Academic Journal Guide. Chartered Association of Business Schools 2018. Available online: https://charteredabs.org/academic-journal-guide-2018/ (accessed on 1 September 2022).
- de Lima, F.R.P.; Da Silva, A.L.; Godinho Filho, M.; Dias, E.M. Systematic Review: Resilience Enablers to Combat Counterfeit Medicines. Supply Chain Manag. Int. J. 2018, 12, 117–135. [Google Scholar] [CrossRef]
- Ahmed, E.S.; Ahmad, M.N.; Othman, S.H. Business Process Improvement Methods in Healthcare: A Comparative Study. Int. J. Health Care Qual. Assur. 2019, 32, 887–908. [Google Scholar] [CrossRef]
- Gao, T.; Zhang, X.; Gurd, B.; Liu, Z. From self-management to a systemised process: The implementation of lean management in a Chinese hospital’s pharmacy intravenous admixture services center. Leadersh. Health Serv. 2020, 33, 325–337. [Google Scholar] [CrossRef]
- Swarnakar, V.; Bagherian, A.; Singh, A.R. Modeling Critical Success Factors for Sustainable LSS Implementation in Hospitals: An Empirical Study. Int. J. Qual. Reliab. Manag. 2021. ahead-of-print. [Google Scholar] [CrossRef]
- Woodnutt, S. Is Lean sustainable in today’s NHS hospitals? A systematic literature review using the meta-narrative and integrative methods. Int. J. Qual. Health Care 2018, 30, 578–586. [Google Scholar] [CrossRef] [PubMed]
- Elbireer, A.; le Chasseur, J.; Jackson, B. Improving laboratory data entry quality using Six Sigma. Int. J. Health Care Qual. Assur. 2013, 26, 496–509. [Google Scholar] [CrossRef] [PubMed]
- Dannapfel, P.; Poksinska, B.; Thomas, K. Dissemination strategy for Lean thinking in health care. Int. J. Health Care Qual. Assur. 2014, 27, 391–404. [Google Scholar] [CrossRef]
- Roemeling, O.; Land, M.; Ahaus, K. Does lean cure variability in health care? Int. J. Oper. Prod. Manag. 2017, 37, 1229–1245. [Google Scholar] [CrossRef]
- Peimbert-García, R.E. Analysis and Evaluation of Reviews on Lean and Six Sigma in Health Care. Qual. Manag. Health Care 2019, 28, 229–236. [Google Scholar] [CrossRef]
- Walley, P.; Found, P.; Williams, S. Failure demand: A concept evaluation in U.K. primary care. Int. J. Health Care Qual. Assur. 2019, 32, 21–33. [Google Scholar] [CrossRef]
- Narayanamurthy, G.; Gurumurthy, A.; Subramanian, N.; Moser, R. Assessing the readiness to implement lean in healthcare institutions—A case study. Int. J. Prod. Econ. 2018, 197, 123–142. [Google Scholar] [CrossRef]
- Ulhassan, W.; Sandahl, C.; Westerlund, H.; Henriksson, P.; Bennermo, M.; Von Thiele Schwarz, U.; Thor, J. Antecedents and characteristics of lean thinking implementation in a Swedish hospital: A case study. Qual. Manag. Health Care 2013, 22, 48–61. [Google Scholar] [CrossRef]
- Dobrzykowski, D.D.; McFadden, K.L.; Vonderembse, M.A. Examining pathways to safety and financial performance in hospitals: A study of lean in professional service operations. J. Oper. Manag. 2016, 43, 39–51. [Google Scholar] [CrossRef]
- Holden, R.J.; Hackbart, G. From group work to teamwork: A case study of ‘Lean’ rapid process improvement in the ThedaCare Information Technology Department. IIE Trans. Healthc. Syst. Eng. 2012, 2, 190–201. [Google Scholar] [CrossRef]
- Ramori, K.A.; Cudney, E.A.; Elrod, C.C.; Antony, J. Lean business models in Healthcare: A systematic review. Total Qual. Manag. Bus. Excell. 2021, 32, 558–573. [Google Scholar] [CrossRef]
- Deblois, S.; Lepanto, L. Lean and Six Sigma in acute care: A systematic review of reviews. Int. J. Health Care Qual. Assur. 2016, 29, 192–208. [Google Scholar] [CrossRef] [PubMed]
- Feng, Q.; Manuel, C.M. Under the knife: A national survey of six sigma programs in U.S. healthcare organisations. Int. J. Health Care Qual. Assur. 2008, 21, 535–547. [Google Scholar] [CrossRef]
- Gowen, C.R.; Mcfadden, K.L.; Hoobler, J.M.; Tallon, W.J. Exploring the efficacy of healthcare quality practices, employee commitment, and employee control. J. Oper. Manag. 2006, 24, 765–778. [Google Scholar] [CrossRef]
- Taner, M.T. Application of Six Sigma methodology to a cataract surgery unit. Int. J. Health Care Qual. Assur. 2013, 26, 768–785. [Google Scholar] [CrossRef]
- Ahmed, S.; Abd Manaf, N.H.; Islam, R. Measuring Lean Six Sigma and quality performance for healthcare organisations. Int. J. Qual. Serv. Sci. 2018, 10, 267–278. [Google Scholar]
- Matthias, O.; Brown, S. Implementing operations strategy through Lean processes within health care: The example of NHS in the U.K. Int. J. Oper. Prod. Manag. 2016, 36, 1435–1457. [Google Scholar] [CrossRef]
- Elamir, H. Improving patient flow through applying lean concepts to emergency department. Leadersh. Health Serv. 2018, 31, 293–309. [Google Scholar] [CrossRef]
- Isack, H.D.; Mutingi, M.; Kandjeke, H.; Vashishth, A.; Chakraborty, A. Exploring the adoption of Lean principles in medical laboratory industry: Empirical evidences from Namibia. Int. J. Lean Six Sigma 2018, 9, 133–155. [Google Scholar] [CrossRef]
- Rosa, A.; Marolla, G.; Lega, F.; Manfredi, F. Lean adoption in hospitals: The role of contextual factors and introduction strategy. BMC Health Serv. Res. 2021, 21, 889. [Google Scholar]
- Crema, M.; Verbano, C. Lean Management to support Choosing Wisely in Healthcare: The first evidence from a systematic literature review. Int. J. Qual. Health Care 2017, 29, 889–895. [Google Scholar] [CrossRef] [PubMed]
- Laureani, A.; Brady, M.; Antony, J. Applications of Lean Six Sigma in an Irish hospital. Leadersh. Health Serv. 2013, 26, 322–337. [Google Scholar] [CrossRef]
- Crema, M.; Verbano, C. Investigating the connections between health lean management and clinical risk management. Int. J. Health Care Qual. Assur. 2015, 28, 791–811. [Google Scholar] [CrossRef] [PubMed]
- Jayasinha, Y. Decreasing turnaround time and increasing patient satisfaction in a safety net hospital-based pediatrics clinic using lean six sigma methodologies. Qual. Manag. Health Care 2016, 25, 38–43. [Google Scholar] [CrossRef] [PubMed]
- McIntosh, B.; Sheppy, B.; Ivan, C. Illusion or delusion—Lean management in the health sector. Int. J. Health Care Qual. Assur. 2014, 27, 482–492. [Google Scholar] [CrossRef]
- Honda, A.C.; Bernardo, V.Z.; Gerolamo, M.C.; Davis, M.M. How lean six sigma principles improve hospital performance. Qual. Manag. J. 2018, 25, 70–82. [Google Scholar] [CrossRef]
- Bowerman, J.; Antony, J.; Downey-Ennis, K.; Antony, F.; Seow, C. Can Six Sigma be the ‘cure’ for our ‘ailing’ NHS? Leadersh. Health Serv. 2007, 20, 242–253. [Google Scholar]
- Ballé, M.; Régnier, A. Lean as a learning system in a hospital ward. Leadersh. Health Serv. 2007, 20, 33–41. [Google Scholar] [CrossRef]
- Schattenkirk, D. Building sustainable internal capacity for quality within a healthcare environment. TQM J. 2012, 24, 374–382. [Google Scholar] [CrossRef]
- Robbins, J.; Garman, A.N.; Song, P.H.; McAlearney, A.S. How high-performance work systems drive health care value: An examination of leading process improvement strategies. Qual. Manag. Health Care 2012, 21, 188–202. [Google Scholar] [CrossRef]
- Niemeijer, G.C.; Does, R.J.; de Mast, J.; Trip, A.; van den Heuvel, J. Generic project definitions for improvement of health care delivery: A case-based approach. Qual. Manag. Health Care 2011, 20, 152–164. [Google Scholar] [CrossRef]
- Nayar, P.; Ojha, D.; Fetrick, A.; Nguyen, A.T. Applying Lean Six Sigma to improve medication management. Int. J. Health Care Qual. Assur. 2016, 29, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Fillingham, D. Can lean save lives? Leadersh. Health Serv. 2007, 20, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Steinebach, M. Eliminating U.S. hospital medical errors. Int. J. Health Care Qual. Assur. 2008, 21, 444–471. [Google Scholar] [CrossRef]
- Taner, M.T.; Sezen, B.; Atwat, K.M. Application of Six Sigma methodology to a diagnostic imaging process. Int. J. Health Care Qual. Assur. 2012, 25, 274–290. [Google Scholar] [CrossRef] [PubMed]
- DelliFraine, J.L.; Wang, Z.; McCaughey, D.; Langabeer, J.R.; Erwin, C.O. The use of six Sigma in health care management: Are we using it to its full potential? Qual. Manag. Health Care 2013, 22, 210–223. [Google Scholar] [CrossRef]
- Chiarini, A. Waste savings in patient transportation inside large hospitals using lean thinking tools and logistic solutions. Leadersh. Health Serv. 2013, 26, 356–367. [Google Scholar] [CrossRef]
- Hicks, S.; McGovern, T.; Prior, G.; Smith, I. Applying lean principles to the design of healthcare facilities. Int. J. Prod. Econ. 2015, 170, 677–686. [Google Scholar] [CrossRef]
- Polanski, W.H.K.; Martin, D.; Günther, S.; Schackert, S.; Klingelhoefer, L.; Fauser, M.; Storch, A.; Sobottka, S.B. Application of the Six Sigma concept for quality assessment of different strategies in DBS surgery. Int. J. Qual. Health Care 2018, 30, 760–768. [Google Scholar] [CrossRef]
- Hallam, C.R.A.; Contreras, C. Lean healthcare: Scale, scope and sustainability. Int. J. Health Care Qual. Assur. 2018, 31, 684–696. [Google Scholar] [CrossRef]
- Kahm, T.; Ingelsson, P. Creating a development force in Swedish healthcare: A focus on the first-line managers’ perspective when applying Lean. Int. J. Health Care Qual. Assur. 2019, 32, 1132–1144. [Google Scholar] [CrossRef]
- Ryan, P.; McGrath, C.; Lawrie, I.; Fitzsimons, C.; O’Shea, J.; De BrÚn, A. Enhancing efficiency in a cardiac investigations department by increasing remote patient monitoring. Int. J. Qual. Health Care 2019, 31, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Antony, J.; Forthun, S.C.; Trakulsunti, Y.; Farrington, T.; McFarlane, J.; Brennan, A.; Dempsey, M. An exploratory study into the use of Lean Six Sigma to reduce medication errors in the Norwegian public healthcare context. Leadersh. Health Serv. 2019, 32, 509–524. [Google Scholar] [CrossRef] [PubMed]
- Slade, J.J.; Wrzesniewski, C.E.; Hunter, O.O.; Allaudeen, N. Complementing Root Cause Analysis with Improvement Strategies to Optimise Venous Thromboembolism Prophylaxis in Patients with Epidural Catheters. Qual. Manag. Health Care 2020, 29, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Eamranond, P.P.; Bhukhen, A.; DiPalma, D.; Kunuakaphun, S.; Burke, T.; Rodis, J.; Grey, M. Interprofessional, multitiered daily rounding management in a high-acuity hospital. Int. J. Health Care Qual. Assur. 2020, 33, 447–461. [Google Scholar] [CrossRef] [PubMed]
- Leite, H.; Lindsay, C.; Kumar, M. COVID-19 outbreak: Implications on healthcare operations. TQM J. 2021, 33, 247–256. [Google Scholar] [CrossRef]
- Narayanamurthy, G.; Gurumurthy, A.; Lankayil, A.A. Experience of implementing lean thinking in an Indian healthcare institution. Int. J. Lean Six Sigma 2018, 12, 23–60. [Google Scholar] [CrossRef]
- Gupta, S.; Kapil, S.; Sharma, M. Improvement of laboratory turnaround time using lean methodology. Int. J. Health Care Qual. Assur. 2018, 31, 295–308. [Google Scholar] [CrossRef]
- Hundal, G.S.; Thiyagarajan, S.; Alduraibi, M.; Laux, C.M.; Furterer, S.L.; Cudney, E.A.; Antony, J. Lean Six Sigma as an organisational resilience mechanism in health care during the era of COVID-19. Int. J. Lean Six Sigma 2021, 12, 762–783. [Google Scholar] [CrossRef]
- Farrokhi, F.R.; Gunther, M.; Williams, B.; Blackmore, C.C. Application of Lean Methodology for Improved Quality and Efficiency in Operating Room Instrument Availability. J. Healthc. Qual. 2015, 37, 277–286. [Google Scholar] [CrossRef] [PubMed]
- Setijono, D.; Naraghi, M.A.; Ravipati, P.U. Decision support system and the adoption of lean in a Swedish emergency ward: Balancing supply and demand towards improved value stream. Int. J. Lean Six Sigma 2010, 1, 234–248. [Google Scholar] [CrossRef]
- Yamamoto, J.J.; Malatestinic, B.; Lehman, A.; Juneja, R. Facilitating process changes in meal delivery and radiological testing to improve inpatient insulin timing using six sigma method. Qual. Manag. Health Care 2010, 19, 189–200. [Google Scholar] [CrossRef]
- Al-Araidah, O.; Momani, A.; Khasawneh, M.; Momani, M. Lead-time reduction utilising lean tools applied to Healthcare: The inpatient pharmacy at a local hospital. J. Healthc. Qual. 2010, 32, 59–66. [Google Scholar] [CrossRef] [PubMed]
- LaGanga, L.R. Lean service operations: Reflections and new directions for capacity expansion in outpatient clinics. J. Oper. Manag. 2011, 29, 422–433. [Google Scholar] [CrossRef]
- Kuo, A.M.; Borycki, E.; Kushniruk, A.; Lee, T.S. A healthcare Lean Six Sigma System for postanesthesia care unit workflow improvement. Qual. Manag. Health Care 2011, 20, 4–14. [Google Scholar] [CrossRef]
- Soriano-Meier, H.; Forrester, P.L.; Markose, S.; Arturo Garza-Reyes, J. The role of the physical layout in the implementation of lean management initiatives. Int. J. Lean Six Sigma 2011, 2, 254–269. [Google Scholar] [CrossRef]
- Sanders, J.H.; Karr, T. Improving E.D. specimen TAT using Lean Six Sigma. Int. J. Health Care Qual. Assur. 2015, 28, 428–440. [Google Scholar] [CrossRef]
- Wang, T.-K.; Yang, T.; Yang, C.-Y.; Chan, F.T.S. Lean principles and simulation optimisation for emergency department layout design. Ind. Manag. Data Syst. 2015, 115, 678–699. [Google Scholar] [CrossRef]
- Moraros, J.; Lemstra, M.; Nwankwo, C. Lean interventions in Healthcare: Do they actually work? A systematic literature review. Int. J. Qual. Health Care 2016, 28, 150–165. [Google Scholar] [CrossRef]
- Jorma, T.; Tiirinki, H.; Bloigu, R.; Turkki, L. Lean thinking in Finnish Healthcare. Leadersh. Health Serv. 2016, 29, 9–36. [Google Scholar] [CrossRef]
- Sánchez, M.; Suárez, M.; Asenjo, M.; Bragulat, E. Improvement of emergency department patient flow using lean thinking. Int. J. Qual. Health Care 2018, 30, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Bancroft, J.; Saha, K.; Li, D.; Lukacs, G.; Pierron, X. Lean Six-Sigma: The means to healing an ailing NHS? Int. J. Qual. Reliab. Manag. 2018, 35, 1976–1988. [Google Scholar] [CrossRef]
- Dobrzykowski, D.D.; McFadden, K.L. Examining Governance in Hospital Operations: The Effects of Trust and Physician Employment in Achieving Efficiency and Patient Satisfaction. Decis. Sci. 2020, 51, 74–109. [Google Scholar] [CrossRef]
- Regattieri, A.; Bartolini, A.; Cima, M.; Fanti, M.G.; Lauritano, D. An innovative procedure for introducing the lean concept into the internal drug supply chain of a hospital. TQM J. 2018, 30, 717–731. [Google Scholar] [CrossRef]
- Hutton, S.A.; Vance, K.; Burgard, J.; Grace, S.; Van Male, L. Workplace violence prevention standardisation using lean principles across a healthcare network. Int. J. Health Care Qual. Assur. 2018, 31, 464–473. [Google Scholar] [CrossRef]
- Almutairi, A.M.; Salonitis, K.; Al-Ashaab, A. Assessing the leanness of a supply chain using multi-grade fuzzy logic: A healthcare case study. Int. J. Lean Six Sigma 2019, 10, 81–105. [Google Scholar] [CrossRef]
- Vaishnavi, V.; Suresh, M. Modelling of readiness factors for the implementation of Lean Six Sigma in healthcare organisations. Int. J. Lean Six Sigma 2020, 11, 597–633. [Google Scholar] [CrossRef]
- Vaishnavi, V.; Suresh, M. Assessment of readiness level for implementing lean six Sigma in healthcare organisation using fuzzy logic approach. Int. J. Lean Six Sigma 2021, 12, 175–209. [Google Scholar] [CrossRef]
- Al-Hinai, N.; Shamsuzzoha, A. Developing a practical methodology to improve the healthcare services: Studying a neonatal intensive care unit case in Oman. Int. J. Qual. Reliab. Manag. 2021, 38, 1425–1442. [Google Scholar] [CrossRef]
- Ricciardi, C.; Sorrentino, A.; Improta, G.; Abbate, V.; Latessa, I.; Perrone, A.; Triassi, M.; Dell'aversana Orabona, G. A health technology assessment between two pharmacological therapies through Six Sigma: The case study of bone cancer. TQM J. 2020, 32, 1507–1524. [Google Scholar] [CrossRef]
- Chang, D.; Leu, J.; Wang, W.; Chen, Y. Improving waiting time for surgical rooms using workflow and the six-sigma method. Total Qual. Manag. Bus. Excell. 2020, 31, 869–886. [Google Scholar] [CrossRef]
- Souza, T.A.; Roehe Vaccaro, G.L.; Lima, R.M. Operating room effectiveness: A lean healthcare performance indicator. Int. J. Lean Six Sigma 2020, 11, 973–988. [Google Scholar] [CrossRef]
- Henrique, D.B.; Filho, M.G.; Marodin, G.; de Sousa Jabbour, A.B.L.; Jabbour, C.J.C. A framework to assess sustaining continuous improvement in lean Healthcare. Int. J. Prod. Res. 2021, 59, 2885–2904. [Google Scholar] [CrossRef]
- Rocha, Í.J.A.; Vasconcelos, C.R.D. Lean healthcare implications in an occupational medicine clinic. Int. J. Lean Six Sigma 2021, 12, 973–991. [Google Scholar] [CrossRef]
- Lee, J.Y.; McFadden, K.L.; Lee, M.K.; Gowen, C.R.U.S. hospital culture profiles for better performance in patient safety, patient satisfaction, Six Sigma, and lean implementation. Int. J. Prod. Econ. 2021, 234, 108047. [Google Scholar] [CrossRef]
- Khorasani, S.T.; Cross, J.; Maghazei, O. Lean supply chain management in Healthcare: A systematic review and meta-study. Int. J. Lean Six Sigma 2020, 11, 1–34. [Google Scholar] [CrossRef]
- Davies, C.; Lyons, C.; Whyte, R. Optimising nursing time in a day care unit: Quality improvement using Lean Six Sigma methodology. Int. J. Qual. Health Care 2019, 31, 22–28. [Google Scholar]
- Improta, G.; Balato, G.; Ricciardi, C.; Russo, M.A.; Santalucia, I.; Triassi, M.; Cesarelli, M. Lean Six Sigma in Healthcare: Fast track surgery for patients undergoing prosthetic hip replacement surgery. TQM J. 2019, 31, 526–540. [Google Scholar] [CrossRef]
- Meyer, M.A. Competencies required for healthcare improvement positions. Int. J. Health Care Qual. Assur. 2019, 32, 281–295. [Google Scholar] [CrossRef]
- Feibert, D.C.; Andersen, B.; Jacobsen, P. Benchmarking healthcare logistics processes—A comparative case study of Danish and U.S. hospitals. Total Qual. Manag. Bus. Excell. 2019, 30, 108–134. [Google Scholar] [CrossRef]
- Al-Zain, Y.; Al-Fandi, L.; Arafeh, M.; Salim, S.; Al-Quraini, S.; Al-Yaseen, A.; Abu Taleb, D. Implementing Lean Six Sigma in a Kuwaiti private hospital. Int. J. Health Care Qual. Assur. 2019, 32, 431–446. [Google Scholar] [CrossRef]
- Isfahani, M.; Tourani, H.S.; Seyedin, H. Lean management approach in hospitals: A systematic review. Int. J. Lean Six Sigma 2019, 10, 161–188. [Google Scholar] [CrossRef]
- Crane, J.; Crane, F.G. Preventing Medication Errors in Hospitals through a Systems Approach and Technological Innovation: A Prescription for 2010. Hosp. Top. 2006, 84, 3–8. [Google Scholar] [CrossRef]


| Authors | Benefits (Real Benefit or Potential Benefits) |
|---|---|
| Gowen, et al. (2006) [37] | Quality improvement, customer satisfaction increase, net cost savings, reduced error frequency, reduced error severity, increased understanding of errors, heightened awareness of errors, and reduced the impact of errors. |
| Fillingham (2007) [57] | Reduced staff dissatisfaction and frustration, productivity improvement, mortality reduction, fast recovery, length of stay, paperwork reduction, and better teamwork. |
| Bowerman, et al. (2007) [50] | Improvement in financial and operational performance. |
| Kumar and Steinebach (2008) [58] | Minimised clinical errors in surgical activities, increased the hospital’s profitability overall, and ensured patient safety. |
| Feng and Manuel (2008) [37] | Reduced cycle time, streamlined process flow and reduced medical errors. |
| Hundal, et al. (2021) [73] | VSM, data analytics; and Failure Mode Effect Analysis (FMEA). |
| Farrokhi, et al. (2015) [74] | Adopt best practices of operating room management. |
| Gupta, et al. (2018) [72] | Reduction of the average TAT from 180 to 95 min in the haematology lab, and from 268 to 208 min in the biochemistry lab. |
| Setijono, et al. (2010) [75] | Reduction in resource utilisation, reducing the cost of care, reduction in patient waiting time. |
| Yamamoto, et al. (2010) [76] | Increased communication and restricted the scheduling of inpatient procedures during mealtimes reduced disruptions to insulin administration. On-time meal delivery and increased the proportion of patients taking insulin scheduled for radiology tests during appropriate times. Optimised insulin delivery and patient safety. |
| Al-Araidah et al. (2010) [77] | A thorough investigation of the drug dispensing process revealed unnecessary complexities contributing to delays in delivering medications to patients. As a result, the average cycle time was reduced from 158 to 82 min, a time saving of 76 min, or 448% of the original cycle time. |
| LaGanga (2011) [78] | Increased capacity to admit new patients into a healthcare service operation system. Analysis of 1726 intake appointments for the year preceding and the full year following the Lean project showed a 27% increase in the service capacity to intake new patients and a 12% reduction in the no-show rate due to the transformation of service processes the Lean project. |
| Kuo, et al. (2011) [79] | Reduced waiting time for patients waiting for orthopaedic surgery. |
| Soriano-Meier, et al. (2011) [80] | Improved non-clinical service operations in the U.K.’s NHS. |
| Taner, et al. (2012) [59] | Reduction in delays, reduction in repeats, achieving targets, high patient safety, low bias, high efficiency, high diagnostic efficiency. |
| Schattenkirk (2012) [53] | Reduced time in process improvement, high return on investment. |
| Holden and Hackbart (2012) [34] | Improved mean first call resolution; improvement of timely completion performance for high-urgency calls and timely completion performance for medium- and low-urgency (follow-up six months). Improved teamwork: communication, coordination, workload distribution. |
| Robbins, et al. (2012) [54] | Strengthened communication within departments, aligning mission, goals and tactics, generated a culture of change and improved working conditions. |
| Niemeijer, et al. (2012) [55] | Reduced cost and improved quality. LSS aided the organisation’s transition from purely problem-oriented to more process-oriented. |
| Taner (2013) [39] | Improved patient access to care, lowered complication rate, and increased skills transfer. |
| Laureani, et al. (2013) [46] | Reduction in in-hospital falls, more complete medical records and reduction in prescription lead times. |
| Burgess and Radnor (2013) [13] | 45% reduction in turnaround time; 60% increase in productivity; 53% increase in efficiency; 98% reduction in errors. |
| Elbireer, et al. (2013) [26] | After initiating the Six Sigma project, there was a 60.5% reduction in data entry errors from 423 errors a month (i.e., 4.34 Six Sigma) in the first month to 166 errors/month (i.e., 4.65 Six Sigma) over 12 months. The team estimated the average cost of identifying and fixing a data entry error to be USD 16.25 per error. Thus, reducing errors by an average of 257 errors per month over one year has saved the laboratory USD 50,115. In addition, the project developed awareness among the laboratory staff about continuously improving their work processes. |
| Gijo, et al. (2013) [6] | Reduced patient waiting time in a pathology department of a super-speciality hospital attached to a manufacturing company. |
| Ulhassan, et al. (2013) [32] | Enhanced staff and resource utilisation; improved workflow for patient discharge process, enhanced communication, as well as better coordination. |
| Farrokhi, et al. (2015) [74] | Potential institutional annual cost savings of USD 2.8 million. Reduction in unnecessary instruments delivered to the operating room; reduced the number of instruments for minimally invasive spine surgery by 70%; setup time decreased by 37%. |
| DelliFraine, et al. (2013) [60] | Patient satisfaction and improved organisational performances. |
| Chiarini, et al. (2013) [61] | Reduce costs related to patient transportation and other kinds of waste. The results have reduced the patient’s average lead time from the emergency department to hospitalisation or discharge. |
| Dannapfel, et al. (2014) [27] | Improving staff experience and working environment, increasing job satisfaction and creating development time. |
| McIntosh, et al. (2014) [49] | Waste and cost reduction, increasing care quality and applying techniques to reduce turnaround time in critical services. |
| Hicks, et al. (2015) [62] | Improved patient flow, increased number of beds and toilets, reduced distance travelled, reduced process steps and accommodated the increase in demand. |
| Sanders and Karr (2015) [81] | Reduction of turnaround times for E.D. specimens. Indirect results: The project results included: a 50% decrease in vials used for testing, a 50% decrease in unused or extra specimens, a 90% decrease in E.D. specimens without orders, a 30% decrease in complete blood count analysis (CBCA) median turnaround time (TAT) a 50% decrease in CBCA TAT variation, a 10% decrease in troponin TAT variation, an 18.2% decrease in URPN TAT variation, and a 2–5-min decrease in E.D. registered nurses rainbow draw time. |
| Crema and Verbano (2015) [47] | Safety improvements. |
| Wang, et al. (2015) [82] | The patients’ average waiting time was reduced from 78 to 38 min. The service level increased from 54.86 to 88.55%. Moreover, the number of nurses was reduced from nine to six. |
| Nayar, et al. (2016) [56] | Reduced clinic waiting time for veterans, reduced the time taken to fill non-VA prescriptions, reduced veterans’ clinic visits for unnecessary/non-urgent non-VA prescriptions, improved veterans’ satisfaction, improved provider satisfaction and improved compliance. |
| Jayasinha (2016) [48] | Improved discharge process efficiency, reduced number of steps in the process, less interruption for the physician, fewer order entry errors/corrections, and improved patient satisfaction. |
| Dobrzykowski, et al. (2016) [33] | Direct and positive impact on patient safety; it impacts financial performance through internal integration—improving operations (internal coordination; increased teamwork; knowledge management, waste reduction). |
| Deblois and Lepanto (2016) [36] | Health outcomes, processes, quality and economic aspects. |
| Moraros, et al. (2016) [83] | Patient flow and safety. |
| Jorma, et al. (2016) [84] | Cost reduction. |
| Roemeling, et al. (2017) [28] | Reduced direct waste (most projects) (preventive and proactive intervention). |
| Polanski, et al. (2018) [63] | Evidence-based therapeutic success rates in terms of quality of earnings. |
| Narayanamurthy, et al. (2018a) [31] | Appropriate delivery model, matching patient and organisational expectations, smoothed the flow of patients, medicines, information, equipment, etc. |
| Trakulsunti and Antony (2018) [3] | Patient safety, improved internal and external customer satisfaction, effective communication, improved team dynamics, enhanced employee morale and quantifiable cost savings. |
| Gonzalez-Aleu, et al. (2018) [11] | Achieved continuous improvement projects in hospitals. |
| Narayanamurthy, et al. (2018b) [71] | Improvement in total lead time, average value-added time, the total waiting time of a patient, the average turnaround time for reports, physical space usage, worker absenteeism, walking distances of staff, percentage of cases rescheduled due to late starts and number of reports with errors. |
| Isack, et al. (2018) [43] | Positive impact on operational performance, shortened turnaround time (TAT), employee motivation and cost reduction. |
| Honda, et al. (2018) [50] | Improved process performance, including waiting for time reduction and patient flow with the subsequent impact of increasing patient satisfaction. Reduced operating costs and inventories. |
| Sánchez, et al. (2018) [85] | Significant reductions in process time of discharges, length of stay (389 vs. 329 min, p < 0.001), and waiting time (71 vs. 48 min, p < 0.001) were achieved after Lean implementation, improving workplace well-being. |
| Hallam and Contreras (2018) [64] | Lean tools resulted in reducing Ohno’s seven wastes. |
| Bancroft, et al. (2018) [86] | Significant improvements in productivity, patient care and cost reduction. |
| Ahmed, et al. (2018) [40] | Patient safety, teamwork and quality performance of the hospitals are based on demographics such as gender, types of hospital and working experience. |
| Dobrzykowski and McFadden (2020) [87] | Increase the competitiveness of organisations. |
| Dobrzykowski and McFadden (2020) [87] | Trust between doctors and hospitals. |
| Dobrzykowski and McFadden (2020) [87] | Lean improved process integration, and process integration impacted on operational efficiency and patient satisfaction. |
| Regattieri, et al. (2018) [88] | Space optimisation (reduction of space dedicated to material stock); time reduction for the material handling process (check of inventory level, place in stock, picking and procurement); immediate reduction of the average material inventory level. |
| Hutton, et al. (2018) [89] | Standardisation in threat assessment and education of workplace violence streamlines and standardises processes to free up clinician time for other responsibilities, while simultaneously improving internal and external customer satisfaction. |
| Almutairi, et al. (2019) [90] | Patient safety, patient care, improved quality and reduced cost. |
| Peimbert-García, et al. (2019) [29] | Financial saving, increased productivity, a better quality of care, few errors and better patient safety. |
| Almutairi, et al. (2019) [90] | Improved supply chain framework. |
| Vaishnavi and Suresh (2020) [91] | Reduced the medical error, waiting time, delivery of medical reports, unnecessary medical cost and continuous improvement. |
| Vaishnavi and Suresh (2020b) [92] | Voice of customers; aligning project goals with organisation vision; management commitment; leadership, effective communication, supplier management, understanding tools and technique; effective use of technology; organisational strategy; organisational infrastructure; continuous performance measurement; employee commitment and trust; recognition and reward system; project selection; time and cost management. |
| Al-Hinai and Shamsuzzoha (2021) [93] | Improved the efficiency of the staff flow and storage management and reduced the noise level. |
| Ricciardi, et al. (2020b) [94] | Identified which antibiotic treatment influences the outcome of LOS. |
| Chang, et al. (2020) [95] | Reduced the total waiting time and reduced variations in the surgical room process. Reduced the average time from 22.8 min to 15.6 min, and increased the satisfaction level of surgical patients, surgeons and staff in the surgical room. |
| Souza, et al. (2020) [96] | Operational wastes can be identified. |
| Henrique, et al. (2021) [97] | Patient rescheduling rate, reduction of 50% in total inventory, reduction of 66% in medication delivery delays, reduction in general costs, increased billing rate, reduction in the stock of materials and medicines. |
| Rocha and Vasconcelos (2021) [98] | Reduction of time wasted in the patient’s journey, increased employee productivity and efficiency in patient care during the work shift are considered. |
| Lee, et al. (2021) [99] | A strong multidimensional culture with more Lean and Six Sigma implementation in hospitals. Better patient safety and satisfaction level for better quality performance of U.S. hospitals. |
| Khorasani, et al. (2020) [100] | Supply chain management; leadership; top management involvement; and organisational culture. |
| Davies, et al. (2019) [101] | Significant improvements in service performance and patient and staff satisfaction. Significant added value includes a reduction in PTTs, an increase in nursing care time and an improvement in the nurse–patient ratio. |
| Improta, et al. (2019) [102] | The average LOS was reduced from 10.66 to 7.8 days (−26.8%). |
| Meyer (2019) [103] | Process improvement, competency-based job posting. |
| Feibert, et al. (2019) [104] | Traceability, degree of automation, security of supply. |
| Kahm and Ingelsson P. (2019) [65] | Decreased dissatisfaction at work, stress and poor or insufficient health. |
| Ryan, et al. (2019) [66] | Reduced the number of unscheduled attendances to the clinic, safer, more timely responses to cardiac events and enhanced care quality. |
| Walley, et al. (2019) [30] | Reduced the pressure on other health services, acted promptly and increased patient safety. |
| Al-Zain, et al. (2019) [105] | Reduction in waiting time. A cost–benefit analysis estimated the present project value at USD 656,459, leading to USD 5,820,319 in savings by 2025. |
| Isfahani, et al. (2019) [106] | The rate of providing care and services at the right time significantly increased, intervals between the reception and getting the service were also significantly reduced, and patients’ length of stay in all studies was considerably reduced. |
| Slade, et al. (2020) [68] | Zero cases of delays, reduction of variability in standard work. |
| Leite, et al. (2021) [70] | Potential to reduce mental stress during the pandemic. |
| Ricciardi, et al. (2020a) [4] | The corrective action consisted of applying fast-track surgery and improving the care process’s effectiveness and efficiency. |
| Lima, et al. (2021) [21] | Time gains, reduction of lead time, reduction of patient waiting time, improvement of cycle time, improvement of hospitalisation time, reduction of waiting lists, reduction of errors, identification and reduction of waste, reduction of stocks, reorganisation of physical space and reduction of costs, improved organisational culture, increased team spirit and communication, employee and supplier satisfaction, improved workload for nurses and reduced overtime, efficiency and productivity gains, bottleneck identification, improved patient and information flow, capacity levelling, positive impact on quality and safety indicators, reduced number of complaints, increased customer satisfaction (patient). |
| Eamranond, et al. (2020) [69] | Decreased severe safety events (SSEs), with a lower observed to the expected length of stay (O/E LOS). |
| Trakulsunti, et al. (2021) [3] | Customised LSS tool kit for reducing medication errors. |
| Vaishnavi and Suresh (2020) [91] | Eliminated waste during the process and ensured quick delivery of service. |
| Trakulsunti, et al. (2020) [3] | Reduction of errors in the medication process, such as missing medication, expired medication errors and order entry errors; reduced the estimated labour cost of USD 550,000 in a mid-sized hospital; can save the hospital inpatient pharmacy USD 82,650 annually by reducing the number of errors and missing doses; improved staff working performance. |
| McDermott, et al. (2021) [2] | Minimised WIP, overproduction, medical error, and cycle time, effectively utilised the employee’s abilities through up-skilling and reskilling activities; minimised length-of-stay, quicker bed assignment and lab results. |
| Ramori, et al. (2021) [35] | A Lean change transfers knowledge and creates a learning organisation. Reduced waste and costs, and improved customer (patient) satisfaction. |
| Walley, et al. (2019) [30] | Waste audit; and understanding tools and techniques. |
| Al-Hinai and Shamsuzzoha (2021) [93] | Working environment; H.R. management, supply chain management; and sustainment plans |
| Bhat, et al. (2020) [1] | Effective leadership; availability of data; involvement of cross-functional team; effective communication. |
| Chang, et al. (2020) [95] | Training; technology application; quality of service; and understanding process. |
| Eamranond, et al. (2020) [69] | Quality improvement culture; strong leadership team; training; stakeholders’ involvement; organisational stability; deployment strategy; metric of measurement; and reward systems. |
| Gao, et al. (2020) [23] | Strong leadership; training, time management, and teamwork. |
| Henrique, et al. (2021) [97] | Audit process; competition programs; work standards; A3 method; KPIs; Kaizen event; visual management; Gemba walks; Value stream Mapping (VSM); structured approach; deployment strategy; training; follow-up; effective communication; continuous improvement culture; data-based decisions; aligning project goals with strategic objectives; risk analysis and piloting; information; involvement of physicians; top management involvement; involvement of health professionals; I.T. support; dedicated implementation team; and effective leadership. |
| Leite, et al. (2021) [70] | Clear communication; careful planning; visual management; standard operating procedures; and use of technology. |
| Ricciardi, et al. (2020a) [4] | Multidisciplinary team |
| Slade, et al. (2020) [68] | Organisational culture; leadership; teamwork; staff involvement; effective communication; and H.R. policies. |
| Swarnakar, et al. (2021) [24] | Awareness of statutory policy; comprehensive information; qualified team for deployment; training; multidisciplinary team; and understanding of tools and techniques. |
| Trakulsunti, et al. (2021) [3] | Improvement culture; structured deployment plan; sustainability plan; top management commitment; project selection; team formation; and training. |
| Trakulsunti, et al. (2020) [3] | Understanding tools and techniques; understanding Lean philosophy; top management support; training; staff engagement; leadership capability; appropriate team formation; implementation infrastructure; and cultural change. |
| Vaishnavi and Suresh (2020a) [91] | Information about methodology; trust among employees; quality improvement culture; acceptance of change; organisational structure, availability of resources; employee empowerment; employee spirit and cooperation; working environment; and waste audit. |
| Lee, et al. (2021) [99] | Multidimensional cultural orientations; patient involvement; and a structured approach. |
| McDermott, et al. (2021) [2] | Robust data; use of technology; supply chain optimisation; I.T. support systems; statistical process control techniques; risk management; and workplace management. |
| Ramori, et al. (2021) [35] | Business strategy; organisational design and structure; quality culture; understanding entire value stream; trust; mindfulness; needfulness; respectful, interaction, diverse team; social and task relatedness; effective communication; data availability; and leadership. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McDermott, O.; Antony, J.; Bhat, S.; Jayaraman, R.; Rosa, A.; Marolla, G.; Parida, R. Lean Six Sigma in Healthcare: A Systematic Literature Review on Motivations and Benefits. Processes 2022, 10, 1910. https://doi.org/10.3390/pr10101910
McDermott O, Antony J, Bhat S, Jayaraman R, Rosa A, Marolla G, Parida R. Lean Six Sigma in Healthcare: A Systematic Literature Review on Motivations and Benefits. Processes. 2022; 10(10):1910. https://doi.org/10.3390/pr10101910
Chicago/Turabian StyleMcDermott, Olivia, Jiju Antony, Shreeranga Bhat, Raja Jayaraman, Angelo Rosa, Giuliano Marolla, and Ratri Parida. 2022. "Lean Six Sigma in Healthcare: A Systematic Literature Review on Motivations and Benefits" Processes 10, no. 10: 1910. https://doi.org/10.3390/pr10101910
APA StyleMcDermott, O., Antony, J., Bhat, S., Jayaraman, R., Rosa, A., Marolla, G., & Parida, R. (2022). Lean Six Sigma in Healthcare: A Systematic Literature Review on Motivations and Benefits. Processes, 10(10), 1910. https://doi.org/10.3390/pr10101910










