Proposal for a Standard Architecture for the Integration of Clinical Information Systems in a Complex Hospital Environment
Abstract
1. Introduction
- Efficiency. Response times in a clinical environment are often essential, therefore the generation of deadlocks and waits are unacceptable.
- Robustness. In order to guarantee the operability of critical systems, redundancy and a design that contemplates contingencies and optimization in the management of resources are required.
- Scalability. It is necessary to assume the possibility of growth, both in the systems involved and in the volume of information handled.
- Normalization and standardization. The use of open standards is key to guarantee present and future interoperability with other information systems.
- Reuse. The model does not intend to be a unique solution for a particular problem, but to constitute a generic reference.
- Functionality. In addition to complying with the above principles, it must be considered that the information systems to be integrated into the model cover real needs, and the orientation of the information systems must always be to cover those needs of the end users and the organization sponsoring these systems.
2. Materials and Methods
2.1. Methodology
- Phase I: Analysis of functional requirements.A detailed analysis of the information system needs in a clinical environment was performed. To this end, the different clinical blocks were broken down into each disciplinary area and these were broken down into the main information systems they require. The different information flows that are communicated between the different systems are reviewed below.
- Phase II: Analysis of technical requirements.The identification of the technical requirements to be met by the proposed integration model was carried out in order to define a viable platform that can be implemented in a real environment.
- Phase III: Study of technical solutions.An assessment was made of the different information exchange mechanisms for executing the integration processes. Based on the analyzed mechanisms, the comparative review of the different implementations of each mechanism was deepened.
- Phase IV: Model design.An integration platform model that covers the functional and technical requirements defined was proposed, using the technical solutions analyzed in phase III.
- Phase V: Implementation proposal, maintenance approach.The implementation of the integration model was proposed, as well as the considerations for the operability and maintenance of the platform.
- Phase VI: Evolution of the model and future possibilities.Future improvements and evolutions of the platform were contemplated, considering the forecast of the evolution of the technology market in the health field, as well as estimates of future functional needs.
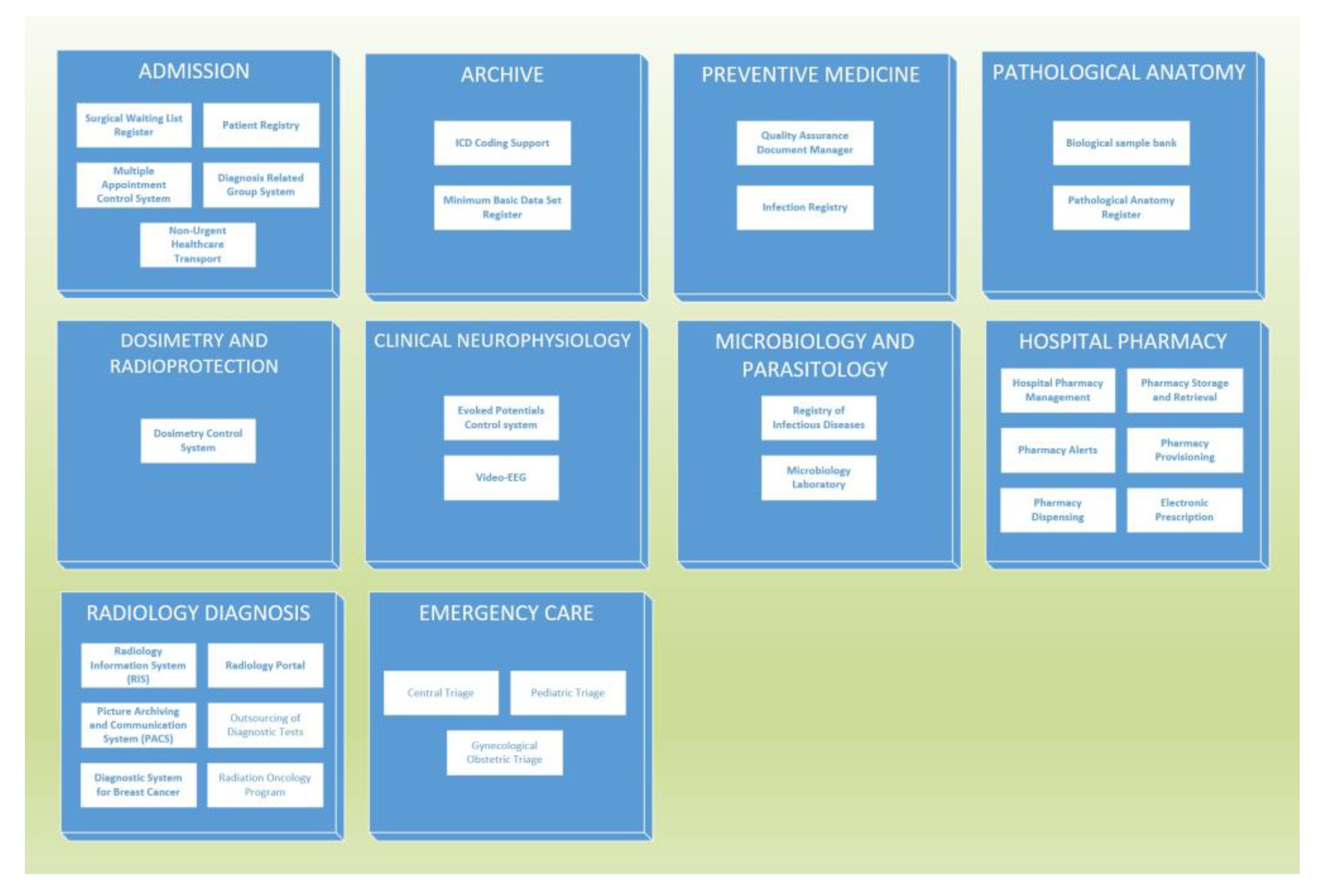
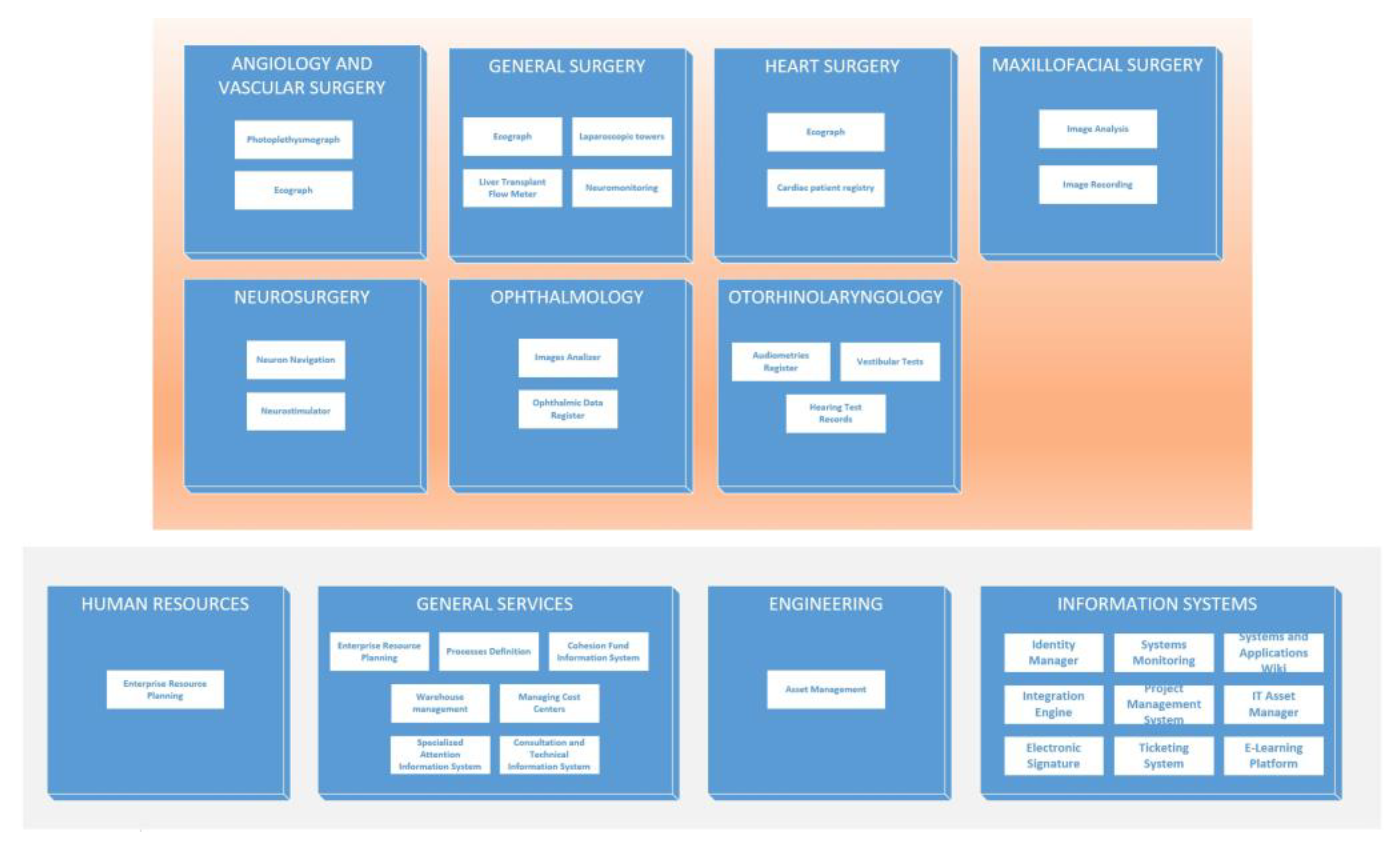
2.2. Functional Requirements
- Medical services;
- Central services;
- Surgical services;
- Obstetric, gynecological and pediatric services;
- Multidisciplinary units;
- Non-assistance services.
- ○
- Master data;
- ○
- Patient administrative information;
- ○
- Clinical data queries;
- ○
- Alert management;
- ○
- Management of patient movements;
- ○
- Management of patient activity in the practice;
- ○
- Activity management in operating theaters;
- ○
- Surgical waiting list;
- ○
- Clinical trials;
- ○
- Medical orders and prescriptions;
- ○
- Day hospital treatments.
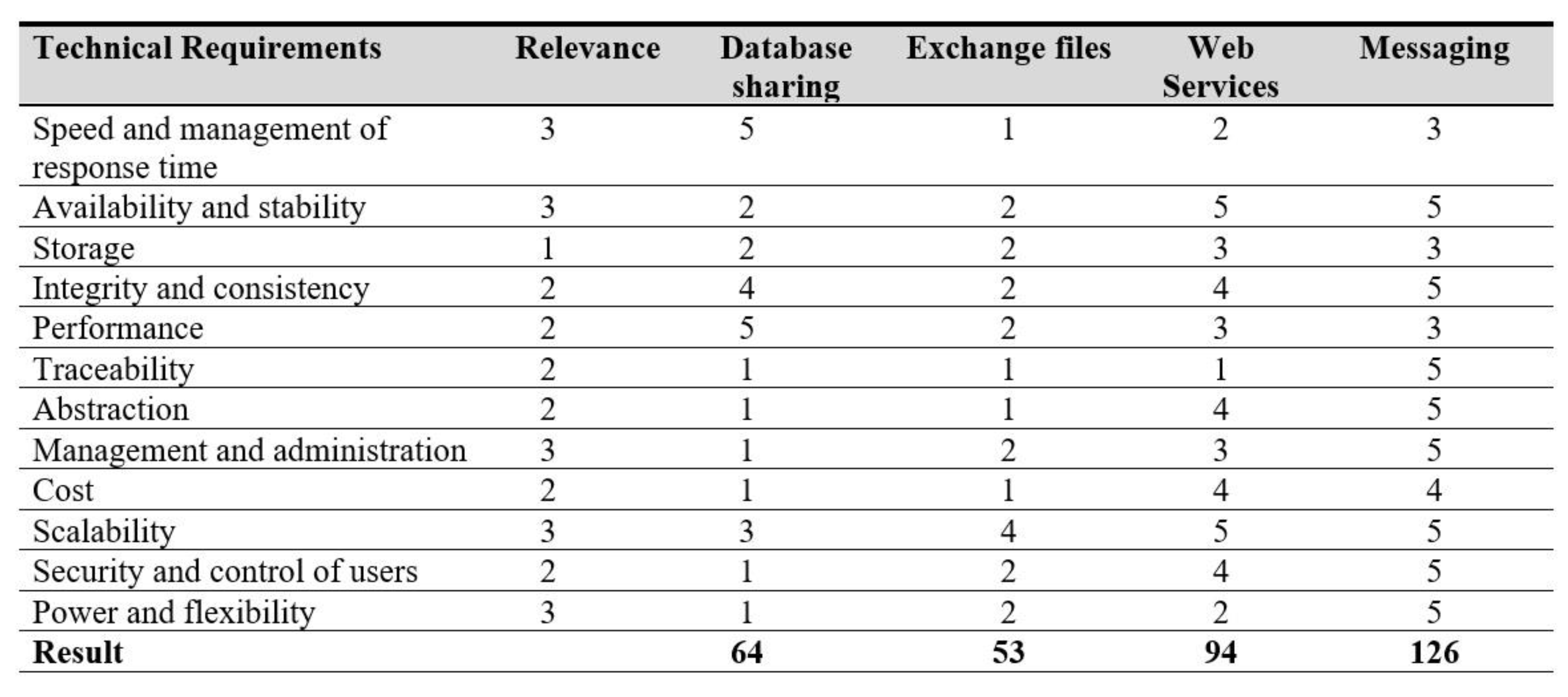
2.3. Technical Requirements
- Speed and management of response time. In a complex clinical environment, the information exchanged is time sensitive. For example information related to real-time care (in a consultation, in the emergency room or to care for a hospitalized patient) does not have the same priority as the retrieval of laboratory tests or the updating of appointment agendas. For this reason, a solution was sought that allows different levels of priority to be established in communication, and guarantees response times to be adjusted to functional needs for information that needs to be notified urgently. This way, urgent data, normal priority data and low priority data must be differentiated.
- Availability and stability. The power provided by information technologies has a major drawback associated with it: the dependence that they generate. The lack of operability of an integration system can block hospital operations. In order to avoid it, contingency plans are prepared for disasters, but the first measure is to minimize the possibility of failure and denial of service. Therefore, the solution must allow the use of a replicated model, which reduces as much as possible the possibility of general failure of the system, and paralyzes the exchange of information.
- Storage. Final information, consisting of clinical and management data, reports, test results, etc., should be stored in the HIS and departmental applications. However, the information processed in a certain time window, usually several days, must be stored persistently. The purpose of this is to ensure that this information can be retrieved in case of the failure of any of the other information systems, and to be able to follow up if a failure or error has occurred. Although a few days of persistence may suggest that the volume of storage required will not be high, the large amount of information flow that includes multimedia information from diagnostic tests requires the provision of a large volume of storage space. This high volume of information, along with the needs of information exploitation and security measures to be taken (traceability, redundancy, backups) make it necessary to have a stable storage system that allows the handling of information, therefore a database management system was used for this purpose.
- Integrity and consistency. The information communicated in an integration process must be consistent at all points in it, whether in the source system, the integration platform or the target systems. This information does not only cover the data to be sent, but also the transaction metadata.
- Performance. The volume of data to be processed is very high, and some of them with critical priority. In addition, processing will be continuous but uneven: in a complex clinical center, activity is uninterrupted 24 h a day, every day of the year. In certain periods of time and on certain days the workload will be greater than others. Therefore, it is necessary to guarantee that the processing will be efficient enough so as not to generate a queuing that blocks the operation of the systems.
- Traceability. The architecture is required to allow detailed tracking of any transaction, and to know all steps that have been carried out from the system of origin to the destination systems. This information must be very detailed, including the timestamps of each transaction.
- Abstraction. The integration platform must be separated from the logic of the rest of the clinical applications, allowing to add, remove or replace applications with minimal adjustments, without dependence on the internal logic of each system.
- Management and administration. As far as possible, ease of maintenance and parameterization is sought. Maintaining a model that is as simple and consistent as possible reduces the risk of errors and failures, and therefore indirect costs.
- Cost. The total cost of ownership is considered to be a relevant factor, which should be kept as low as possible, provided all other requirements are met. The total cost of ownership includes the cost of hardware devices, software licenses, the cost of personnel for implementation and maintenance and the cost of risk management.
- Scalability. The possibility of extending the integration architecture to cover future needs, either by incorporating new systems, contemplating the management of new information flows or increasing the volume of data to be processed.
- Security and control of users. The model will be performing a critical function in the hospital, and using very sensitive information. It is necessary to comply with the legal requirements of security and data protection, so the possibility of controlling failures, redundancy and contingency plans must be considered, as well as a solid system for controlling access to information.
- Power and flexibility. In a real environment, in order to adapt to changes, it must be possible to make adjustments at each of the points (information source systems, information flows, information destination systems). The system must have a sufficient level of adaptability to be able to integrate with any modern information system that meets any communications standard, even if the complexity of the integration increases. This is not the ideal scenario, but the need to cover functional requirements may require some partial compromise of the technical requirements.
2.4. Technical Solutions
- Database sharing. In this mechanism, the system that wants to share information (master system) allows access in query mode to part of its data repository system that should receive the information (slave system).This solution has many drawbacks, two of which stand out: On the one hand, it generates a very high dependence on the operation of the master system: in the event of changes in the data model, the integration is affected. On the other hand, the performance of the master system may be compromised by the access of the slave system, especially in the case where both systems must access the information of the other, where the problems would multiply. There is no homogeneous interface for access to information by several systems, preventing the solution from being scalable. There is also the problem of the difficulty in actively requesting information from the slave system, making it necessary to have processes in the master system that prepare, adapt or process information.
- Exchange files. The master system generates certain files with exchange information, which can be queried by several slave systems. This mechanism has several similarities with the previous one. Although it avoids the impact on the performance of the master system, the problems raised remain: no standardized form of communication is offered, so each client would be forced to make a custom adaptation for a non-homogeneous solution. There is no simple way for the slave system to make requests for information, necessitating tailor-made processes in the master system that conduct surveys in the client system to prepare the information it requires.
- Web Services. The service-oriented model (SOA) using web services as an interchange mechanism, unlike the previous mechanisms, offers a complete separation of the business layer of the master application from the integration layer. It allows a scalable and homogeneous solution for slave systems to query master systems, and for the role of the master or slave system to be combined according to the business needs of each application. This solution model is already feasible and applicable, however it has several drawbacks when used on a large scale. In scenarios such as information systems in large clinical environments, with hundreds of systems sharing information between them, the main stumbling block to overcome is a lack of control. Multiple queries are performed redundantly, generating inefficiencies, and the need arises to control priority in the exchange of information between systems (some require faster response times than others), and changes in production systems and the implementation of new ones make it necessary to modify the operation of integrations, being necessary in this case to modify the logic of each system individually, with the cost, delay and risk that this entails.
- Messaging. Alternatively, there is the possibility of using an Enterprise Serial Bus (ESB) model, a control system that allows for communication between systems and transactions between them. In the health field, there are implementations of ESBs focused on the problems of health systems, called integration engines. The use of integration engines as a mechanism for exchanging information offers the advantages of the web services model presented above, with the addition that they offer a higher level of abstraction, providing a single point of control of the integrations. In this way, through the use of the engine, each integration can be parameterized, defining multiple sources and destinations of information between the integrated systems, making changes in them when necessary, and prioritizing and defining different policies for each integration in each situation (message saturation, errors in the master system, errors in the slave system, processing failures). It also offers the possibility of adding logic to specific integrations in a transparent way for the integrated systems.
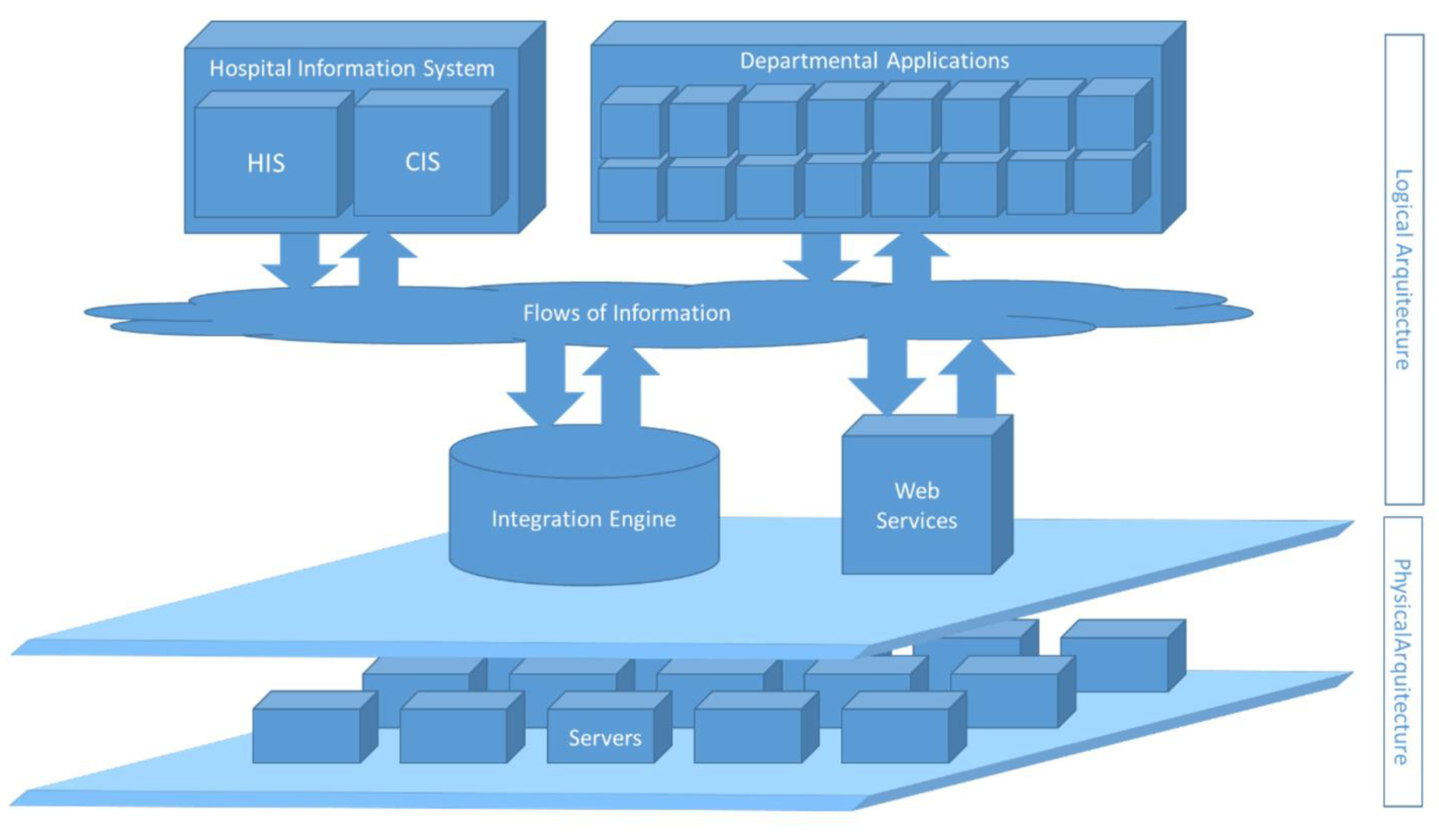
3. Results
3.1. Target Architecture Proposal
- Information systems, formed by the HIS/CIS, and by the departmental applications corresponding to the different units and clinical services.
- The information flows corresponding to the data to be shared between systems.
- The integration engine, which will house all the logic and control of the system.The physical architecture shall consist of the following elements:
- Servers, where the different system applications are hosted (HIS/CIS, departmental applications, integration engine, web services). Data, which are the criticality of the system; the servers will be redundant and in high availability, monitored and with defined backup policies, although the detail of the system model of each application exceeds the scope of this article.
- Communications that guarantee sufficient quality of service for the different applications to provide the service for which they are implemented, and also cover the operational requirements of information exchange of the integration system. As indicated in the previous point, messaging is chosen as the most efficient exchange mechanism.
- Security management: control of engine users, roles and permissions.
- Configuration of the connection points of each of the departments (IP address and port).
- Creation of input and output channels for each of the applications that will communicate with the engine.
- Configuration of each channel: type of information received, method and time of polling new messages, analysis of messages, recovery of specific data, transformation of the message if appropriate, forwarding to other channels or systems, traceability of messages, level of persistence of messages. This is the most delicate process and requires the most testing.
- Configuration of communication security measures. In certain situations (excessive glued messaging, for example) measures can be taken. These can be internal engine management, such as stopping a channel to avoid excessive consumption of resources, or notifying an administrator.
3.2. Implementation and Deployment
- Exhaustive pre-tests for all integrations in certification environments, covering the following typology: unit tests, integration tests, functional validation tests, performance tests.
- Preparation of a contingency plan to cover the operation of the clinical center in the event of partial or total failures, either by designing non-IT circuits, using alternative tools in the event of failure of the defined applications or working with the defined applications but in isolation, not integrated with the entire system.
- Involvement of the management of the clinical center, and preparation and dissemination of a communication plan describing the start-up process.
- Execution of previous simulations of the process, including the possibility of reversing in case of critical failure.
- Planning and management of the post-implantation support necessary to cover the incidents and problems once the start-up has been carried out.
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Appendix A
- Master data management
- ○
- Maintaining physician data
- ○
- Updating bed data
- Administrative management of patients
- ○
- New patient registration
- ○
- Modification of patient status
- ○
- Patient mergers
- ○
- Reversal of merger
- ○
- Reassigning episodes
- ○
- Updating patient identification
- ○
- Diagnostic or procedure update
- Consultation of clinical data
- ○
- Search for patient demographics
- ○
- Demographic response
- ○
- Patient search
- ○
- Patient list response
- ○
- Episode search
- ○
- Episode listing response
- Alert management
- ○
- Alert assignment
- ○
- Cancellation or deactivation of alert
- Management of patient movements
- ○
- Pre-Admission
- ○
- Admission
- ○
- High
- ○
- Unconfirmed discharge
- ○
- Temporary Discharge
- ○
- Transfer
- ○
- Application for admission
- ○
- Transfer request
- ○
- Registration of movements
- ○
- Updating Information
- ○
- Temporary Entry
- ○
- Patient Exchange
- ○
- Cancellation of admission
- ○
- Cancellation of registration
- ○
- Cancellation of stock transfer
- ○
- Unconfirmed discharge cancellation
- ○
- Cancellation of transfer request
- ○
- Cancellation of unconfirmed admission
- ○
- Cancellation of pre-admission
- ○
- Cancellation of Temporary Acquisition
- ○
- Cancellation of temporary admission
- In-office patient activity management
- ○
- New appointment
- ○
- Scheduled appointment modification
- ○
- Cancellation of appointment
- ○
- Appointment start
- ○
- Patient reception
- ○
- Call for consultation
- ○
- End of quotation
- ○
- Cancellation of reception
- ○
- Cancellation of the end of the appointment
- ○
- Appointment rescheduling
- ○
- Record of not going to an appointment
- ○
- New appointment request
- ○
- Change request
- ○
- Delete request
- Activity management in operating theatres
- ○
- Programming intervention
- ○
- Changing scheduling
- ○
- Canceling scheduling
- ○
- Intervention capture
- ○
- Capture modification
- ○
- Capture Cancellation
- ○
- Closure of intervention
- ○
- Reversal of closing
- ○
- Admission for major outpatient surgery
- ○
- Reversal of revenue
- ○
- Surgery discharge
- ○
- Discharge cancellation
- ○
- Patient admission
- ○
- Transfer to the operating room
- ○
- Transfer to plant
- ○
- Cancellation of stock transfer
- ○
- Intervention reprogramming
- ○
- Suspension of intervention
- Surgical waiting list
- ○
- Waiting list inclusion
- ○
- Waiting list output
- ○
- Cancellation of waiting listing
- ○
- Canceling waiting list output
- ○
- Insertion in medical waiting list
- ○
- Exit from medical waiting list
- ○
- Patient admission
- ○
- Patient discharge
- ○
- Cancellation of inclusion
- ○
- Canceling scheduling
- ○
- Cancellation of admission
- ○
- Discharge cancellation
- ○
- Modification of registration
- ○
- Waiting list output
- ○
- Change of status and waiting list situation
- Clinical tests
- ○
- New order
- ○
- Acceptance of the order
- ○
- Order completion
- ○
- Order scheduling
- ○
- Order completion
- ○
- Order rejection
- ○
- Order scheduling
- ○
- New petition
- ○
- Partial acceptance of requests
- ○
- Partial scheduling of future change records
- ○
- Partial resolution of petitions
- ○
- Full resolution of petitions
- ○
- Validation, modification or cancellation of the result obtained
- Medical orders and prescriptions
- ○
- New prescription
- ○
- Modification of prescription
- ○
- Cancellation of prescription
- ○
- Prescription interruption
- ○
- End of prescription
- ○
- Pharmaceutical validation
- ○
- Management confirmation
- ○
- New dispensation
- ○
- Dispensing cancellation
- Day Hospital Treatments
- ○
- Activity scheduling
- ○
- Patient reception
- ○
- Start of activity
- ○
- End of activity
- ○
- Canceling scheduling
- ○
- Cancellation of receipt
- ○
- Reversal of activity end
- ○
- New appointment request
- ○
- Change request
- ○
- Deleting flag
References
- Ebadollahi, S.; Coden, A.; Tanenblatt, M.; Chang, S.; Syeda-Mahmood, T.; Amir, A. Concept-Based Electronic Health Records: Opportunities and Challenges. In Proceedings of the 14th ACM International Conference on Multimedia, Santa Barbara, CA, USA, 23–27 October 2006; p. 1006. [Google Scholar] [CrossRef]
- Azami, I.E.; Malki, M.O.C.; Tahon, C. Integrating Hospital Information Systems in Healthcare Institutions: A Mediation Architecture. J. Med. Syst. 2011, 36, 3123–3134. [Google Scholar] [CrossRef]
- Yungton, J.; Sittig, D.; Reilly, P.; Pappas, J.; Flammini, S.; Chueh, H.; Teich, J. A Software Architecture to Support a Large-Scale, Multi-Tier Clinical Information System. In Proceedings of the Annual Symposium on Computer Application in Medical Care, Orlando, FL, USA, 7–11 November 1998; pp. 210–214. [Google Scholar]
- Ray, A.; Jetley, R.; Jones, P. Engineering High Confidence Medical Device Software. ACM SIGBED Rev. 2009, 6, 1–7. [Google Scholar] [CrossRef]
- Davis, A.M. Fifteen Principles of Software Engineering. IEEE Softw. 1994, 11, 94–96. [Google Scholar] [CrossRef]
- Callele, D.; Wnuk, K.; Penzenstadler, B. New Frontiers for Requirements Engineering. In Proceedings of the 2017 IEEE 25th International Requirements Engineering Conference (RE), Lisbon, Portugal, 4–8 September 2017; pp. 184–193. [Google Scholar]
- Jonnagaddala, J.; Guo, G.; Batongbacal, S.; Marcelo, A.; Liaw, S.-T. Adoption of Enterprise Architecture for Healthcare in AeHIN Member Countries. BMJ Health Care Inform. 2020, 27, e100136. [Google Scholar] [CrossRef] [PubMed]
- Higman, S.; Dwivedi, V.; Nsaghurwe, A.; Busiga, M.; Sotter Rulagirwa, H.; Smith, D.; Wright, C.; Nyinondi, S.; Nyella, E. Designing Interoperable Health Information Systems Using Enterprise Architecture Approach in Resource-Limited Countries: A Literature Review. Int. J. Health Plan. Manag. 2019, 34, e85–e99. [Google Scholar] [CrossRef] [PubMed]
- Ajer, A.K.; Hustad, E.; Vassilakopoulou, P. Enterprise Architecture in Hospitals: Resolving Incongruence Issues. Stud. Health Technol. Inform. 2019, 264, 659–663. [Google Scholar] [CrossRef]
- Winter, A.; Stäubert, S.; Ammon, D.; Aiche, S.; Beyan, O.; Bischoff, V.; Daumke, P.; Decker, S.; Funkat, G.; Gewehr, J.; et al. Smart Medical Information Technology for Healthcare (SMITH). Methods Inf. Med. 2018, 57, e92–e105. [Google Scholar] [CrossRef]
- Argüello, M.; Des, J.; Perez, R.; Fernandez-Prieto, M.J.; Paniagua, H. Electronic Health Records (EHRs) Standards and the Semantic Edge: A Case Study of Visualising Clinical Information from EHRs. In Proceedings of the 2009 11th International Conference on Computer Modelling and Simulation, Cambridge, UK, 25–27 March 2009; pp. 485–490. [Google Scholar] [CrossRef]
- Bortis, G. Experiences with Mirth: An Open Source Health Care Integration Engine. In Proceedings of the 30th International Conference on Software Engineering (ICSE 2008), ACM, Leipzig, Germany, 10–18 May 2008; pp. 649–652. [Google Scholar] [CrossRef]
- Health Level Seven International. HL7 Standards. Available online: www.hl7.org/implement/standards/product_section.cfm?section=1 (accessed on 12 December 2021).
- Beeler, G.W. HL7 Version 3—An Object-Oriented Methodology for Collaborative Standards Development. Int. J. Med. Inform. 1998, 48, 151–161. [Google Scholar] [CrossRef]
- Sibarani, E.M. Simulating an Integration Systems: Hospital Information System, Radiology Information System and Picture Archiving and Communication System. In Proceedings of the 2012 2nd International Conference on Uncertainty Reasoning and Knowledge Engineering, Jakarta, Indonesia, 14–15 August 2012; pp. 62–66. [Google Scholar] [CrossRef]
- Sánchez-Caro, A.; Soguero-Ruiz, C.; Mora-Jiménez, I.; Lechuga, L.; Ramos-López, J.; García-Alberola, A.; Serrano-Balazote, P.; Rojo-Álvarez, J.L. Towards Semantic Interoperability for Cardiovascular Risk Stratification into the Electronic Health Records Using Archetypes and SNOMED-CT. In Proceedings of the Computing in Cardiology 2014, Cambridge, MA, USA, 7–10 September 2014; pp. 497–500. [Google Scholar]
- Soteriades, H.; Neokleous, K.; Tsouloupas, G.; Jossif, A.; Schizas, C. Electronic Health Record: Facilitating the Coding Process. In Proceedings of the 13th IEEE International Conference on BioInformatics and BioEngineering, Chania, Greece, 10–13 November 2013; pp. 1–4. [Google Scholar] [CrossRef]
- Kopanitsa, G.; Taranik, M. Application of ISO 13606 Archetypes for an Integration of Hospital and Laboratory Information Systems; Springer: Copenhagen, Denmark, 2015; pp. 29–36. [Google Scholar] [CrossRef]
- Saas, A.; Hossain, M.; Lee, C.-P. Development of a Software Tool for Healthcare Data Interchange. In Proceedings of the 1st ACM International Health Informatics Symposium, Arlington, VA, USA, 11–12 November 2010; pp. 517–520. [Google Scholar] [CrossRef]
- Rejeb, O.; Bastide, R.; Lamine, E.; Marmier, F.; Pingaud, H. A Model Driven Engineering Approach for Business Continuity Management in E-Health Systems. In Proceedings of the IEEE International Conference on Digital Ecosystems and Technologies, Campione d’Italia, Italy, 18–20 June 2012; pp. 1–7. [Google Scholar] [CrossRef]
- Krey, M. Key Challenges to Enabling IT in Healthcare. In Proceedings of the 2016 IEEE International Conference on Healthcare Informatics (ICHI), Chicago, IL, USA, 4–7 October 2016; pp. 328–333. [Google Scholar] [CrossRef]
- Bastos, J.; Neto, P.A.M.S.; Almeida, E.S.; Meira, S. Adopting Software Product Lines: A Systematic Mapping Study. In Proceedings of the Evaluation and Assessment in Software Engineering—EASE 2011, Durham, UK, 11–12 April 2011; pp. 717–722. [Google Scholar]
- Stisen, A.; Verdezoto, N.; Blunck, H.; Kjærgaard, M.B.; Grønbæk, K. Accounting for the Invisible Work of Hospital Orderlies: Designing for Local and Global Coordination. In Proceedings of the CSCW ’16: 19th ACM Conference on Computer-Supported Cooperative Work & Social Computing, New York, NY, USA, 26 February–2 March 2016; Association for Computing Machinery: New York, NY, USA, 2016; pp. 980–992. [Google Scholar] [CrossRef]
- Beyer, M.; Kuhn, K.; Meiler, C.; Jablonski, S.; Lenz, R. Towards a Flexible, Process-Oriented IT Architecture for an Integrated Healthcare Network. In Proceedings of the ACM Symposium on Applied Computing, Nicosia, Cyprus, 14–17 March 2004; Volume 1, pp. 264–271. [Google Scholar] [CrossRef]
- Koutkias, V.; Bouaud, J. Contributions on Clinical Decision Support from the 2018 Literature. Yearb. Med. Inform. 2019, 28, 135–137. [Google Scholar] [CrossRef][Green Version]
- Kilsdonk, E.; Peute, L.; Jaspers, M. Factors Influencing Implementation Success of Guideline-Based Clinical Decision Support Systems: A Systematic Review and Gaps Analysis. Int. J. Med. Inform. 2016, 98, 56–64. [Google Scholar] [CrossRef]
- Kwan, J.L.; Lo, L.; Ferguson, J.; Goldberg, H.; Diaz-Martinez, J.P.; Tomlinson, G.; Grimshaw, J.M.; Shojania, K.G. Computerised Clinical Decision Support Systems and Absolute Improvements in Care: Meta-Analysis of Controlled Clinical Trials. BMJ 2020, 370, m3216. [Google Scholar] [CrossRef] [PubMed]
- Praveena, M.D.A.; Bharathi, B. A Survey Paper on Big Data Analytics. In Proceedings of the 2017 International Conference on Information Communication and Embedded Systems (ICICES), Chennai, India, 23 February 2017; pp. 1–9. [Google Scholar] [CrossRef]
- Sharma, N.; Sawai, D.; Surve, G. Big Data Analytics: Impacting Business in Big Way. In Proceedings of the 2017 International Conference on Data Management, Analytics and Innovation (ICDMAI), Pune, India, 24–26 February 2017; pp. 111–116. [Google Scholar] [CrossRef]
- Ahuja, S.; Angra, S. Machine Learning and Its Applications: A Review. In Proceedings of the 2017 International Conference on Big Data Analytics and Computational Intelligence (ICBDAC), Chirala, India, 23–25 March 2017. [Google Scholar] [CrossRef]





Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maldonado Belmonte, E.; Otón Tortosa, S.; Ruggia Frick, R.J. Proposal for a Standard Architecture for the Integration of Clinical Information Systems in a Complex Hospital Environment. Informatics 2021, 8, 87. https://doi.org/10.3390/informatics8040087
Maldonado Belmonte E, Otón Tortosa S, Ruggia Frick RJ. Proposal for a Standard Architecture for the Integration of Clinical Information Systems in a Complex Hospital Environment. Informatics. 2021; 8(4):87. https://doi.org/10.3390/informatics8040087
Chicago/Turabian StyleMaldonado Belmonte, Enrique, Salvador Otón Tortosa, and Raúl Julián Ruggia Frick. 2021. "Proposal for a Standard Architecture for the Integration of Clinical Information Systems in a Complex Hospital Environment" Informatics 8, no. 4: 87. https://doi.org/10.3390/informatics8040087
APA StyleMaldonado Belmonte, E., Otón Tortosa, S., & Ruggia Frick, R. J. (2021). Proposal for a Standard Architecture for the Integration of Clinical Information Systems in a Complex Hospital Environment. Informatics, 8(4), 87. https://doi.org/10.3390/informatics8040087






