The Role of Academia in Reorientation Models of Care—Insights on eHealth
Abstract
:1. Introduction
2. Innovation 2.0 Collaborating for Shared Purpose
2.1. Organisational Stakeholder Engagement
2.2. Post Stakeholder Engagement Technology Infrastructure Development
- (a)
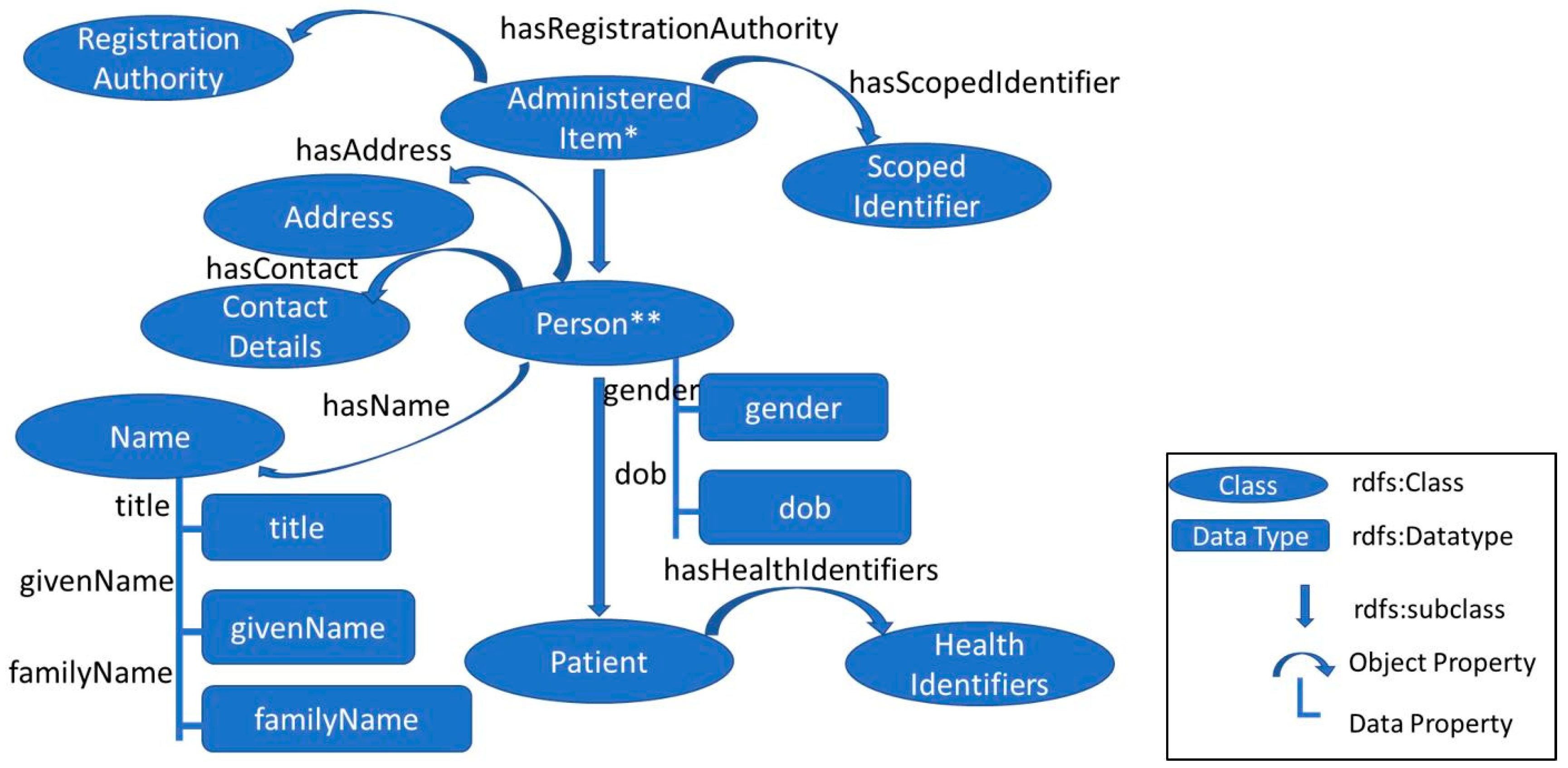
- A framework to represent core information for reporting and statistical data analysis purposes.
- (b)
- A format to process data and required information in a common standardised way to support integrated care and timely access to information.
- (c)
2.3. The Political Process Considering the Academic Role in Implementation Research
3. Summary of Progress Phase One
3.1. Individual Stakeholder Engagement
3.2. Technology Infrastructure Development
3.3. The Political Process Considering the Academic Role in Implementation Research
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Centre for Eintegrated Care. Available online: https://www.ceic.ie (accessed on 15 May 2019).
- World Health Organisation. Framework for People Centered Integrated Care Services (Sixty Ninth World Health Assembly). 2016. Available online: http://www.who.int/servicedeliverysafety/areas/people-centred-care/en/ (accessed on 15 May 2019).
- Sustainable Development Goals. 13 March 2019. Available online: https://sustainabledevelopment.un.org/ (accessed on 15 May 2019).
- Greenhalgh, T.; Wherton, J.; Papoutsi, C.; Lynch, J.; Hughes, G.; A’Court, C.; Shaw, S. Beyond Adoption: A New Framework for Theorizing and Evaluating Non Adoption, Abandonment, and Challenges to the Scale-Up, Spread, and Sustainability of Health and Care Technologies. J. Med. Int. Res. 2017, 19, 367. [Google Scholar] [CrossRef] [PubMed]
- Slainte Implementation Strategy (National Strategy Report); Government of Ireland: Dublin, Ireland, 2018. Available online: https://health.gov.ie/blog/publications/slaintecare-Implementation-Strategy/ (accessed on 15 May 2019).
- Wilson, M.R. Scholarly Activity Redefined: Balancing the Three-LegSged Stool. Ochsner J. 2006, 6, 12–14. [Google Scholar] [PubMed]
- Stenberg, K.; Hanssen, O.; Tan Torres, T.; Bertram, M.; Brindley, C.; Soucat, A. Financing transformative health systems towards achievement of the health Sustainable Development Goals: A model for projected resource needs in 67 low-Income and middle-Income countries. Lancet Glob. Health. 2017, 5, 875–887. [Google Scholar] [CrossRef]
- McEvoy, P. Chronic Disease Management: A New Paradigm for Care, 1st ed.; CRC Press: London, UK, 2017. [Google Scholar]
- Pawson, R. The Science of Evaluation. A Realist Manifesto; Sage: London, UK, 2013. [Google Scholar]
- Curley, M.; Salmelin, B. Open Innovation 2.0; Springer: Cham, Switzerland, 2018. [Google Scholar]
- The World Wide Web Consortium W3C. Available online: https://www.w3.org (accessed on 12 May 2019).
- Hussey, P.; Tully, M. National Data Dictionary Metadata Registry Framework Briefing Paper Health Service Executive. (2015, June). eHealth Ireland. 2017. Available online: https://www.ehealthireland.ie/Our-Team/Enterprise-Architecture/HSE-National-Data-Dictionary-Briefing-Paper.pdf (accessed on 12 May 2019).
- McGlinn, K.; Hussey, P. An analysis of healthcare standards to support the development of the Slaintecare ontology for integrated care in Ireland. 2019; under review. [Google Scholar]
- European Internet Foundation. Digital World in 2025 [European Parliament]. 2009. Available online: https://www.eifonline.org/the-digital-world-in-2025.html (accessed on 12 February 2019).
- Benson, T.; Grieve, G. Principles of Health Interoperability SNOMED CT, HL7 and FHIR, 3rd ed.; Springer: London, UK, 2016. [Google Scholar]
- Appleton, B. Patterns Introduction. [Academic]. 2000. Available online: http://www.sci.brooklyn.cuny.edu/~sklar/teaching/s08/cis20.2/papers/appleton-patterns-intro.pdf (accessed on 12 May 2019).
- OECD. Recommendations to OECD Ministers of Health from the High Level Reflection Group on the Future of Health Statistics; OECD: Paris, France, 2017. [Google Scholar]
- ISO. International Standards Organisation Information Technology—Metadata registries (MDR)—Part 3: Registry Metamodel and Basic Attributes ISO 11179_3. Available online: http://metadata-standards.org/11179/ (accessed on 12 May 2019).
- ISO TC 215/26 Healthcare Informatics Metadata Repository Requirements (MetaRep) Working. Available online: https://login.cen.eu/portal/ CEN TC 251 2017 (accessed on 12 May 2019).
- Agency for Clinical Innovation. 2019. Available online: https://www.aci.health.nsw.gov.au/resources/integrated-care/aci/integrated-care (accessed on 12 May 2019).
- Smith, B.; Varzi, A.C. The formal ontology of boundaries. Electron. J. Anal. Philos. 1997, 5, 1–23. [Google Scholar]
- Smith, B. The Structures of the Common Sense World. Acta Philos. Fenn. 1995, 58, 290–317. [Google Scholar]
- European Commission Horizon Europe Fact Sheet. Available online: https://ec.europa.eu/commission/sites/beta-political/files/budget-may2018-research-innovation_en.pdf (accessed on 12 May 2019).
- Department of Health Research Services and Policy Unit 2019 July 17th Towards a Model of Integrated Person-centerd Care. Available online: https://health.gov.ie/wp-content/uploads/2019/07/Towards-a-Model-of-Integrated-Person-Centred-Care.pdf (accessed on 26 July 2019).
- eHealth Ireland Ecosystem. Ecosystem Network [Council of Clinical Information Officers]. June 2015. Available online: http://www.ehealthireland.ie/StakeholderEngagement/eHealth%20Ireland%20EcoSystem (accessed on 12 May 2019).
- Adapt Research Team. The Adapt Center [Research Centre]. 2019. Available online: https://www.adaptcentre.ie/ (accessed on 12 May 2019).
- Oughtibridge, N. A System of Concepts for the Continuity of Care. 2015. Available online: https://contsys.org/ (accessed on 12 May 2019).
- Art Decor Open Tools. [Open Source Development Tool for HL7]. 2017. Available online: https://art-decor.org/mediawiki/index.php?title=Main_Page (accessed on 7 February 2019).

| Active Design Patterns | Original Phase One |
|---|---|
| Platform |
|
| Ecosystem |
|
| Planning for adoption |
|
| Agile production |
|
| Industrialising innovation |
|
| Data driven innovation |
|
| Links to Emerging Work on Models of Meaning |
|---|
| http://theme-e.adaptcentre.ie/metarep/index-en.html |
| http://build.fhir.org/fhir.ttl |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hussey, P.; McGlinn, K. The Role of Academia in Reorientation Models of Care—Insights on eHealth. Informatics 2019, 6, 37. https://doi.org/10.3390/informatics6030037
Hussey P, McGlinn K. The Role of Academia in Reorientation Models of Care—Insights on eHealth. Informatics. 2019; 6(3):37. https://doi.org/10.3390/informatics6030037
Chicago/Turabian StyleHussey, Pamela, and Kris McGlinn. 2019. "The Role of Academia in Reorientation Models of Care—Insights on eHealth" Informatics 6, no. 3: 37. https://doi.org/10.3390/informatics6030037
APA StyleHussey, P., & McGlinn, K. (2019). The Role of Academia in Reorientation Models of Care—Insights on eHealth. Informatics, 6(3), 37. https://doi.org/10.3390/informatics6030037




