Balancing Layout Space and Risk Comprehension in Health Communication: A Comparison of Separated and Integrated Icon Arrays
Abstract
1. Introduction
- (1)
- Under space-constrained conditions, which visual layout—separated or integrated—more effectively enhances users’ comprehension of medical risk information?
- (2)
- Do individual differences in health literacy, graph literacy, and numeracy moderate the effects of these layout strategies?
2. Materials and Methods
2.1. Experimental Design
2.2. Participants
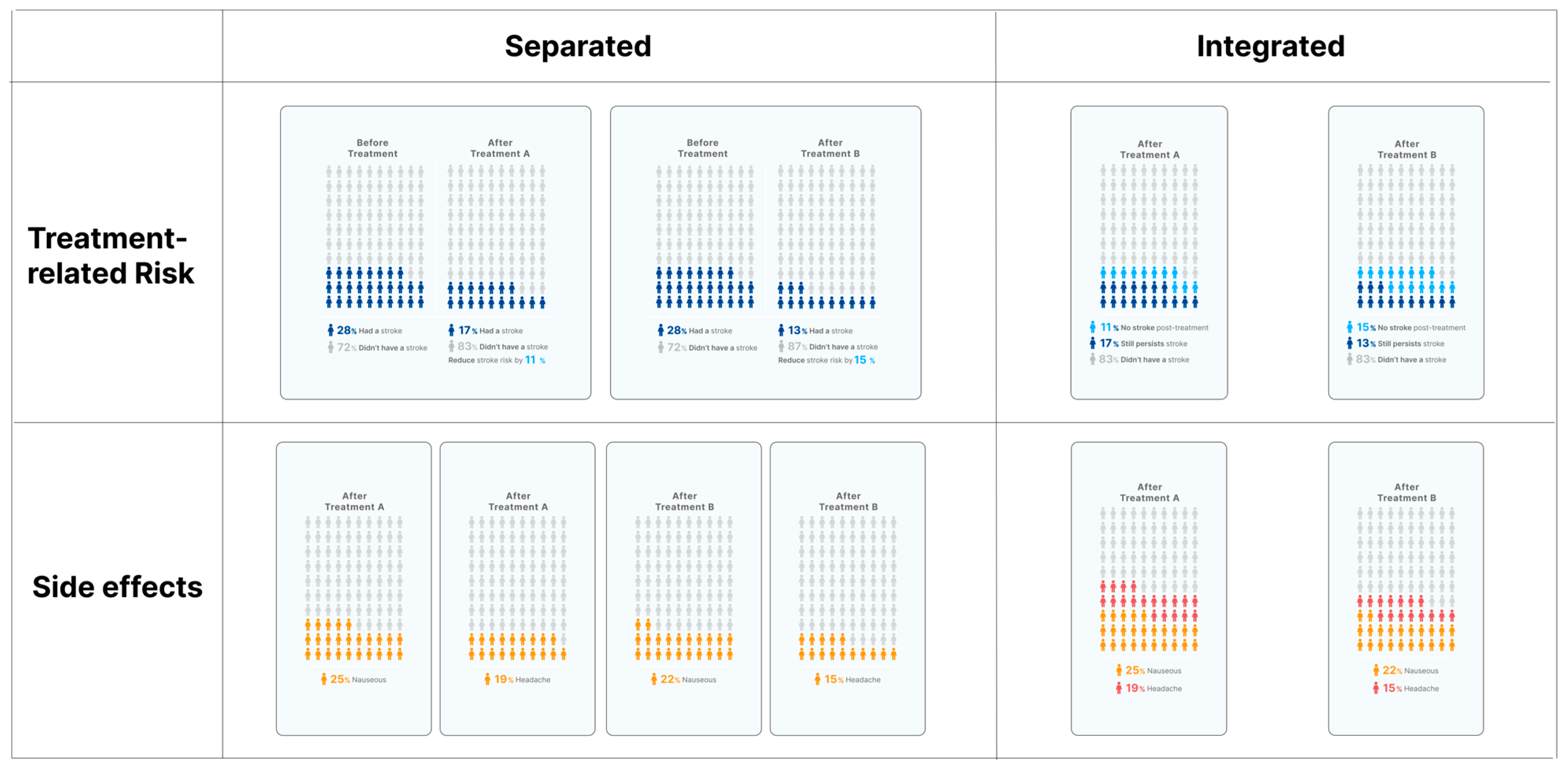
2.3. Stimuli
- Separated: Risks before and after treatment were shown in two distinct arrays.
- Integrated: Risks were combined in one array using two shades of blue.
- Separated: Each side effect was displayed in a separate icon array.
- Integrated: Multiple side effects were combined in a single array using different colors.
2.4. Statistical Analysis
2.5. Measures
2.5.1. Comprehension
2.5.2. Health Literacy
2.5.3. Graph Literacy
2.5.4. Numeracy Skill
3. Results
3.1. Participant Characteristics
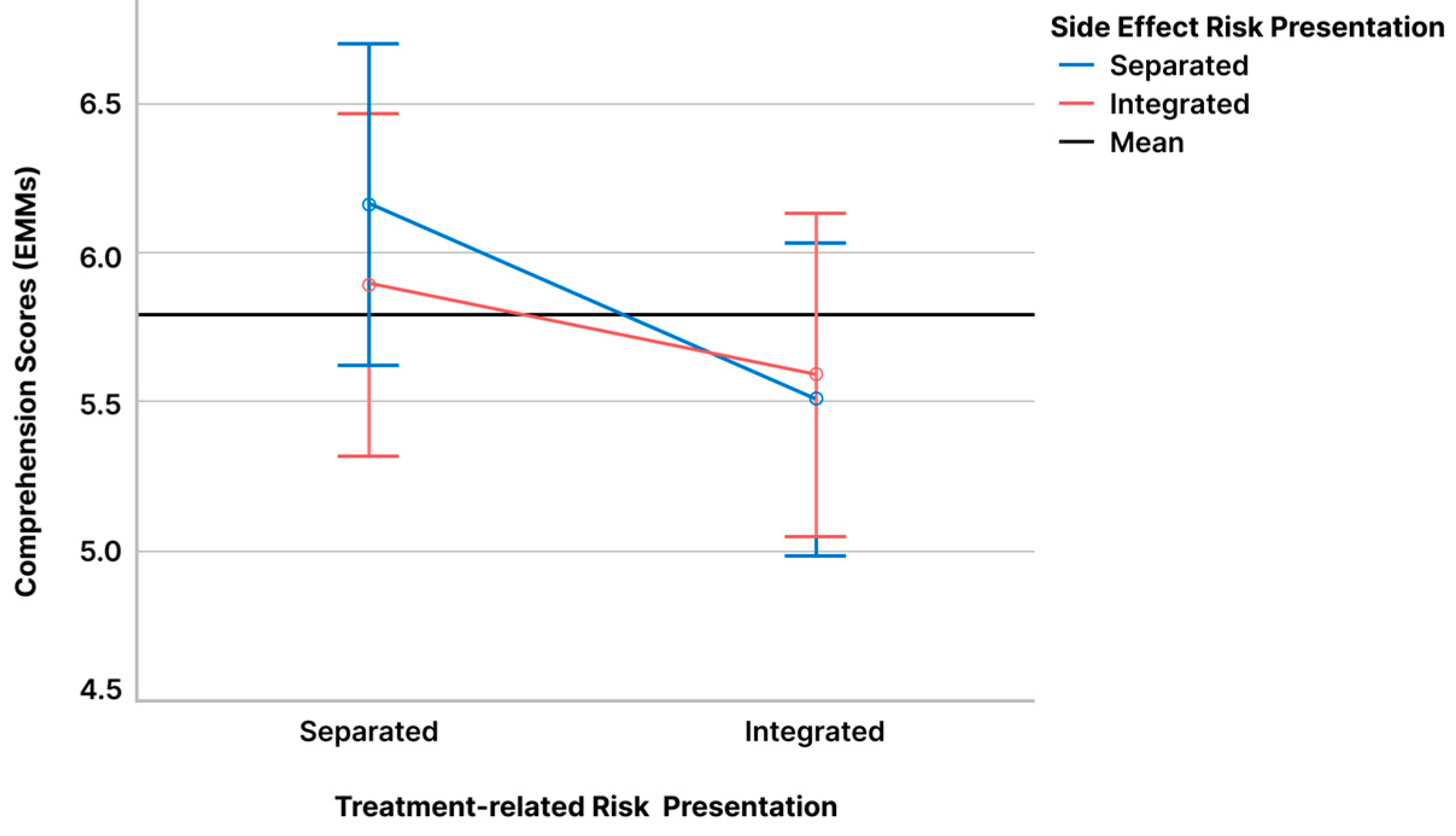
3.2. Effects of Presentation Layout on Comprehension
3.3. Moderating Effects of Cognitive Abilities
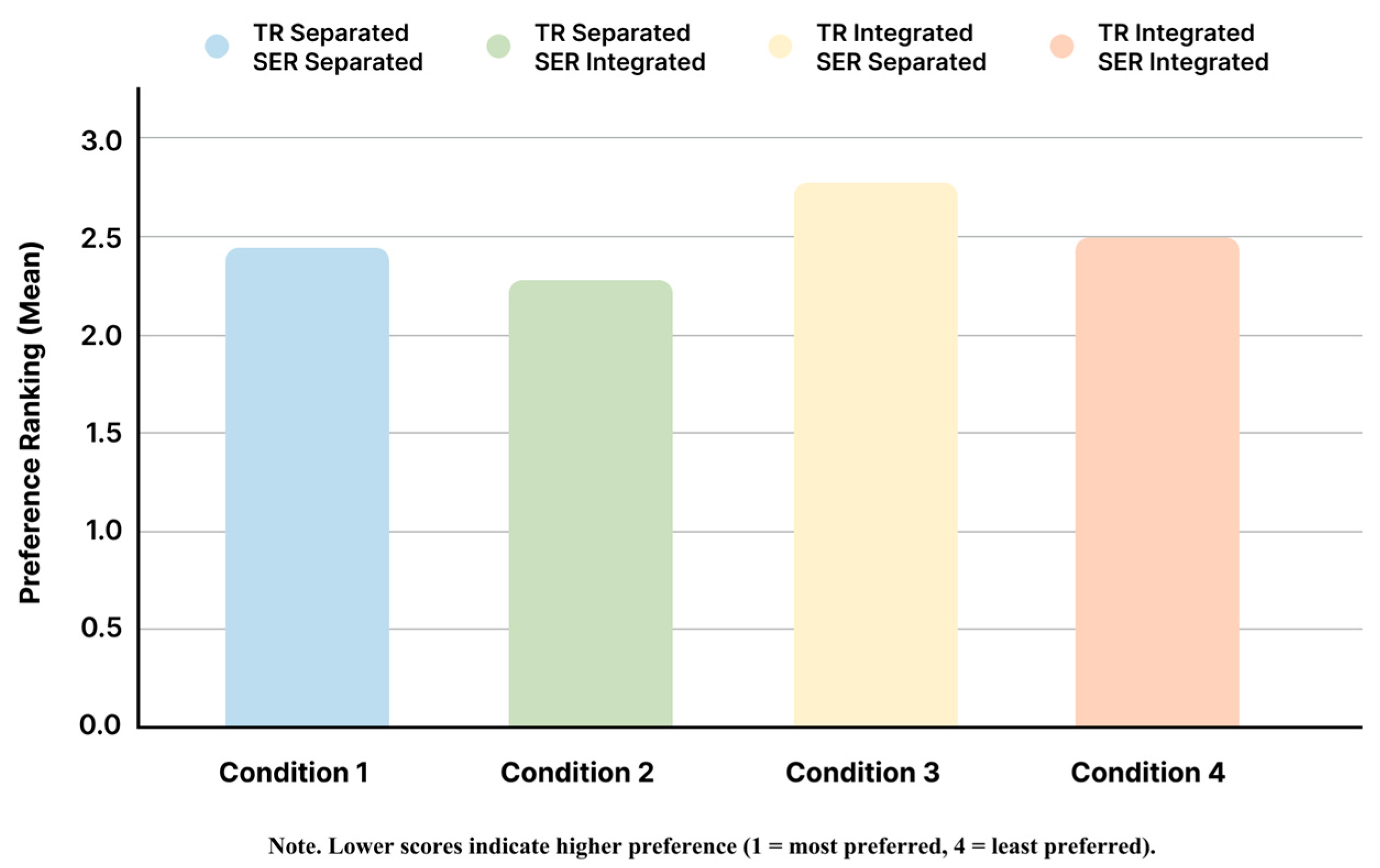
3.4. Preferences for Visual Layouts
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| SDM | Shared Decision Making |
| PDAs | Patient Decision Aids |
| BNT | Berlin Numeracy Test |
| TR | Treatment-Related Risk |
| SER | Side Effect Risk |
References
- Stacey, D.; Volk, R.J. The International Patient Decision Aid Standards (IPDAS) Collaboration: Evidence Update 2.0. Med. Decis. Mak. 2021, 41, 729–733. [Google Scholar] [CrossRef]
- Morgan, D.J.; Scherer, L.D.; Korenstein, D. Improving Physician Communication About Treatment Decisions. JAMA 2020, 324, 937–938. [Google Scholar] [CrossRef]
- Elwyn, G.; Durand, M.A.; Song, J.; Aarts, J.; Barr, P.J.; Berger, Z.; Cochran, N.; Frosch, D.; Galasiński, D.; Gulbrandsen, P.; et al. A three-talk model for shared decision making: Multistage consultation process. BMJ 2017, 359, j4891. [Google Scholar] [CrossRef] [PubMed]
- Hanson, J.L. Shared decision making: Have we missed the obvious? Arch. Intern. Med. 2008, 168, 1368–1370. [Google Scholar] [CrossRef]
- Hawley, S.T.; Zikmund-Fisher, B.; Ubel, P.; Jancovic, A.; Lucas, T.; Fagerlin, A. The impact of the format of graphical presentation on health-related knowledge and treatment choices. Patient Educ. Couns. 2008, 73, 448–455. [Google Scholar] [CrossRef]
- Richter, R.; Jansen, J.; Bongaerts, I.; Damman, O.; Rademakers, J.; Van Der Weijden, T. Communication of benefits and harms in shared decision making with patients with limited health literacy: A systematic review of risk communication strategies. Patient Educ. Couns. 2023, 116, 107944. [Google Scholar] [CrossRef]
- Gigerenzer, G.; Hoffrage, U. How to improve Bayesian reasoning without instruction: Frequency formats. Psychol. Rev. 1995, 102, 684–704. [Google Scholar] [CrossRef]
- Garcia-Retamero, R.; Cokely, E.T. Designing Visual Aids That Promote Risk Literacy: A Systematic Review of Health Research and Evidence-Based Design Heuristics. Hum. Factors 2017, 59, 582–627. [Google Scholar] [CrossRef] [PubMed]
- Galesic, M.; Garcia-Retamero, R.; Gigerenzer, G. Using icon arrays to communicate medical risks: Overcoming low numeracy. Health Psychol. 2009, 28, 210. [Google Scholar] [CrossRef]
- Garcia-Retamero, R.; Galesic, M. Who proficts from visual aids: Overcoming challenges in people’s understanding of risks. Soc. Sci. Med. 2010, 70, 1019–1025. [Google Scholar] [CrossRef]
- Tait, A.R.; Voepel-Lewis, T.; Zikmund-Fisher, B.J.; Fagerlin, A. Presenting Research Risks and Benefits to Parents. Anesth. Analg. 2010, 111, 718–723. [Google Scholar] [CrossRef]
- Trevena, L.J.; Bonner, C.; Okan, Y.; Peters, E.; Gaissmaier, W.; Han, P.K.J.; Ozanne, E.; Timmermans, D.; Zikmund-Fisher, B.J. Current Challenges When Using Numbers in Patient Decision Aids: Advanced Concepts. Med. Decis. Mak. 2021, 41, 834–847. [Google Scholar] [CrossRef]
- O’Neill, E.S.; Grande, S.W.; Sherman, A.; Elwyn, G.; Coylewright, M. Availability of patient decision aids for stroke prevention in atrial fibrillation: A systematic review. Am. Heart J. 2017, 191, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Zikmund-Fisher, B.J.; Ubel, P.A.; Smith, D.M.; Derry, H.A.; McClure, J.B.; Stark, A.; Pitsch, R.K.; Fagerlin, A. Communicating side effect risks in a tamoxifen prophylaxis decision aid: The debiasing influence of pictographs. Patient Educ. Couns. 2008, 73, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Zikmund-Fisher, B.J.; Fagerlin, A.; Roberts, T.R.; Derry, H.A.; Ubel, P.A. Alternate Methods of Framing Information About Medication Side Effects: Incremental Risk Versus Total Risk of Occurrence. J. Health Commun. 2008, 13, 107–124. [Google Scholar] [CrossRef]
- McDowell, M.; Gigerenzer, G.; Wegwarth, O.; Rebitschek, F.G. Effect of Tabular and Icon Fact Box Formats on Comprehension of Benefits and Harms of Prostate Cancer Screening: A Randomized Trial. Med. Decis. Mak. 2019, 39, 41–56. [Google Scholar] [CrossRef]
- Wallace, M.J.; Weissler, E.H.; Yang, J.-C.; Brotzman, L.; Corriere, M.A.; Secemsky, E.A.; Sutphin, J.; Johnson, F.R.; Marcos Gonzalez, J.; Tarver, M.E.; et al. Using Separate Single-Outcome Risk Presentations Instead of Integrated Multioutcome Formats Improves Comprehension in Discrete Choice Experiments. Med. Decis. Mak. 2024, 44, 649–660. [Google Scholar] [CrossRef]
- Zikmund-Fisher, B.J.; Fagerlin, A.; Ubel, P.A. Improving understanding of adjuvant therapy options by using simpler risk graphics. Cancer 2008, 113, 3382–3390. [Google Scholar] [CrossRef] [PubMed]
- Zikmund-Fisher, B.J.; Fagerlin, A.; Ubel, P.A. A Demonstration of ‘Less Can Be More’ in Risk Graphics. Med. Decis. Mak. 2010, 30, 661–671. [Google Scholar] [CrossRef] [PubMed]
- Tiede, K.E.; Ripke, F.; Degen, N.; Gaissmaier, W. When Does the Incremental Risk Format Aid Informed Medical Decisions? The Role of Learning, Feedback, and Number of Treatment Options. Med. Decis. Mak. 2020, 40, 212–221. [Google Scholar] [CrossRef]
- Congelosi, P.D.; Carroll, M.C.; Wong, S.L. Numeracy levels influence shared decision-making and surgical outcomes: A scoping review of the literature. Am. J. Surg. 2023, 225, 967–974. [Google Scholar] [CrossRef]
- Okan, Y.; Garcia-Retamero, R.; Cokely, E.T.; Maldonado, A. Individual Differences in Graph Literacy: Overcoming Denominator Neglect in Risk Comprehension. J. Behav. Decis. Mak. 2012, 25, 390–401. [Google Scholar] [CrossRef]
- Barrouillet, P.; Camos, V. Developmental Increase in Working Memory Span: Resource Sharing or Temporal Decay? J. Mem. Lang. 2001, 45, 1–20. [Google Scholar] [CrossRef]
- Barrouillet, P.; Bernardin, S.; Camos, V. Time Constraints and Resource Sharing in Adults’ Working Memory Spans. J. Exp. Psychol. Gen. 2004, 133, 83–100. [Google Scholar] [CrossRef]
- Zikmund-Fisher, B.J.; Witteman, H.O.; Dickson, M.; Fuhrel-Forbis, A.; Kahn, V.C.; Exe, N.L.; Valerio, M.; Holtzman, L.G.; Scherer, L.D.; Fagerlin, A. Blocks, ovals, or people? Icon type affects risk perceptions and recall of pictographs. Med. Decis. Mak. 2014, 34, 443–453. [Google Scholar] [CrossRef]
- Zikmund-Fisher, B.J.; Witteman, H.O.; Fuhrel-Forbis, A.; Exe, N.L.; Kahn, V.C.; Dickson, M. Animated graphics for comparing two risks: A cautionary tale. J. Med. Internet Res. 2012, 14, e106. [Google Scholar] [CrossRef]
- Price, M.; Cameron, R.; Butow, P. Communicating risk information: The influence of graphical display format on quantitative information perception—Accuracy, comprehension and preferences. Patient Educ. Couns. 2007, 69, 121–128. [Google Scholar] [CrossRef]
- Trevena, L.J.; Zikmund-Fisher, B.J.; Edwards, A.; Gaissmaier, W.; Galesic, M.; Han, P.K.; King, J.; Lawson, M.L.; Linder, S.K.; Lipkus, I.; et al. Presenting quantitative information about decision outcomes: A risk communication primer for patient decision aid developers. BMC Med. Inf. Decis. Mak. 2013, 13 (Suppl. 2), S7. [Google Scholar] [CrossRef]
- Chew, L.D.; Griffin, J.M.; Partin, M.R.; Noorbaloochi, S.; Grill, J.P.; Snyder, A.; Bradley, K.A.; Nugent, S.M.; Baines, A.D.; Vanryn, M. Validation of Screening Questions for Limited Health Literacy in a Large VA Outpatient Population. J. Gen. Intern. Med. 2008, 23, 561–566. [Google Scholar] [CrossRef] [PubMed]
- Okan, Y.; Janssen, E.; Galesic, M.; Waters, E.A. Using the Short Graph Literacy Scale to Predict Precursors of Health Behavior Change. Med. Decis. Mak. 2019, 39, 183–195. [Google Scholar] [CrossRef]
- Cokely, E.T.; Galesic, M.; Schulz, E.; Ghazal, S.; Garcia-Retamero, R. Measuring Risk Literacy: The Berlin Numeracy Test. Judgm. Decis. Mak. 2012, 7, 25–47. [Google Scholar] [CrossRef]
- Sørensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, J. User Satisfaction vs. Performance Metrics. 2012. Available online: https://www.nngroup.com/articles/satisfaction-vs-performance-metrics/ (accessed on 20 March 2025).
- McCaffery, K.J.; Dixon, A.; Hayen, A.; Jansen, J.; Smith, S.; Simpson, J.M. The Influence of Graphic Display Format on the Interpretations of Quantitative Risk Information among Adults with Lower Education and Literacy. Med. Decis. Mak. 2012, 32, 532–544. [Google Scholar] [CrossRef]
- Micallef, L.; Dragicevic, P.; Fekete, J.-D. Assessing the Effect of Visualizations on Bayesian Reasoning through Crowdsourcing. IEEE Trans. Vis. Comput. Graph. 2012, 18, 2536–2545. [Google Scholar] [CrossRef]
- Feldman-Stewart, D.; Kocovski, N.; McConnell, B.A.; Brundage, M.D.; Mackillop, W.J. Perception of Quantitative Information for Treatment Decisions. Med. Decis. Mak. 2000, 20, 228–238. [Google Scholar] [CrossRef] [PubMed]


| Variable | Category/Range | Mean (SD) | n (%) |
|---|---|---|---|
| Gender | Male | – | 52 (43.0%) |
| Female | – | 69 (57.0%) | |
| Age | 22–65 years | 36.64 (8.03) | – |
| Education | High school | – | 25 (20.7%) |
| University | – | 84 (69.4%) | |
| Graduate or above | – | 12 (9.9%) | |
| Health Literacy | 3–15 | 10.42 (1.80) | – |
| Graph Literacy | 0–4 | 1.55 (1.19) | – |
| Numeracy (BNT) | 0–3 | 1.71 (1.14) | – |
| Layout Factor | Presentation Type | Mean (M) | Standard Deviation (SD) |
|---|---|---|---|
| Treatment-Related Risk Presentation | Separated | 6.03 | 3.23 |
| Integrated | 5.55 | 3.15 | |
| Side Effect Risk Presentation | Separated | 5.83 | 3.09 |
| Integrated | 5.74 | 3.28 |
| Effect | F | df | p | Partial η2 |
|---|---|---|---|---|
| Treatment-Related Risk Presentation | 12.456 | 1, 120 | <0.001 | 0.094 |
| Side Effect Risk Presentation | 0.536 | 1, 120 | 0.465 | 0.004 |
| Treatment × Side Effect Interaction | 1.717 | 1, 120 | 0.193 | 0.014 |
| Source | F | df | p-Value | Partial η2 |
|---|---|---|---|---|
| Within-Subjects Effects | ||||
| Treatment-related risk Format | 1.381 | 1 | 0.242 | 0.012 |
| Side Effect risk Format | 0.226 | 1 | 0.635 | 0.002 |
| Treatment × Side Effect | 1.650 | 1 | 0.201 | 0.014 |
| Between-Subjects (Covariates) | ||||
| Health Literacy | 0.380 | 1 | 0.540 | 0.003 |
| Graph Literacy | 14.870 | 1 | <0.001 | 0.113 |
| Numeracy (BNT) | 6.290 | 1 | 0.014 | 0.051 |
| Interactions (Moderation Effects) | ||||
| Treatment × Health Literacy | 0.214 | 1 | 0.644 | 0.002 |
| Treatment × Graph Literacy | 3.378 | 1 | 0.069 | 0.028 † |
| Treatment × Numeracy (BNT) | 7.119 | 1 | 0.009 | 0.057 |
| Side Effect × Health Literacy | 0.008 | 1 | 0.929 | <0.001 |
| Side Effect × Graph Literacy | 0.351 | 1 | 0.554 | 0.003 |
| Side Effect × Numeracy (BNT) | 0.220 | 1 | 0.640 | 0.002 |
| Treatment × Side Effect × Health Literacy | 0.869 | 1 | 0.353 | 0.007 |
| Treatment × Side Effect × Graph Literacy | 1.980 | 1 | 0.162 | 0.017 |
| Treatment × Side Effect × Numeracy (BNT) | 0.898 | 1 | 0.345 | 0.008 |
| Numeracy Group | Treatment-Related Risk Format | Mean (EMM) | SE | 95% CI | p-Value |
|---|---|---|---|---|---|
| Low | Separated | 5.15 | 0.415 | [4.33, 5.97] | <0.001 |
| Integrated | 4.46 | 0.396 | [3.67, 5.24] | ||
| High | Separated | 6.81 | 0.392 | [6.04, 7.59] | 0.116 |
| Integrated | 6.52 | 0.374 | [5.78, 7.26] |
| Condition | Layout Type | Unadjusted Mean | SE | 95% CI | EMM (Adjusted) | SE | 95% CI |
|---|---|---|---|---|---|---|---|
| 1 | Treatment Separated + Side Effect Separated | 6.17 | 0.29 | [5.61, 6.79] | 6.17 | 0.28 | [5.62, 6.71] |
| 2 | Treatment Separated + Side Effect Integrated | 5.89 | 0.31 | [5.33, 6.55] | 5.89 | 0.29 | [5.31, 6.47] |
| 3 | Treatment Integrated + Side Effect Separated | 5.50 | 0.30 | [4.96, 6.16] | 5.50 | 0.27 | [4.97, 6.04] |
| 4 | Treatment Integrated + Side Effect Integrated | 5.59 | 0.30 | [5.00, 6.26] | 5.59 | 0.28 | [5.04, 6.13] |
| Condition (I) | Condition (J) | Mean Difference (I–J) | SE | p-Value | 95% CI |
|---|---|---|---|---|---|
| 1 | 2 | 0.273 | 0.195 | 0.987 | [−0.251, 0.796] |
| 1 | 3 | 0.661 | 0.191 | 0.005 | [0.148, 1.174] |
| 1 | 4 | 0.579 | 0.178 | 0.009 | [0.101, 1.056] |
| 2 | 3 | 0.388 | 0.196 | 0.301 | [−0.138, 0.915] |
| 2 | 4 | 0.306 | 0.190 | 0.661 | [−0.204, 0.816] |
| 3 | 4 | 0.083 | 0.182 | 1.000 | [−0.405, 0.570] |
| Condition (I) | Condition (J) | Z Statistic | Asymptotic Sig. (2-Tailed) | Adjusted p-Value (Bonferroni) |
|---|---|---|---|---|
| 1 | 2 | −1.008 | 0.313 | 1.0 |
| 1 | 3 | −2.105 | 0.035 | 0.21 |
| 1 | 4 | −0.924 | 0.356 | 1.0 |
| 2 | 3 | −2.733 | 0.006 | 0.036 |
| 2 | 4 | −0.612 | 0.541 | 1.0 |
| 3 | 4 | −2.028 | 0.043 | 0.258 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, L.-J.; Zheng, M.-C. Balancing Layout Space and Risk Comprehension in Health Communication: A Comparison of Separated and Integrated Icon Arrays. Informatics 2025, 12, 105. https://doi.org/10.3390/informatics12040105
Wang L-J, Zheng M-C. Balancing Layout Space and Risk Comprehension in Health Communication: A Comparison of Separated and Integrated Icon Arrays. Informatics. 2025; 12(4):105. https://doi.org/10.3390/informatics12040105
Chicago/Turabian StyleWang, Li-Jen, and Meng-Cong Zheng. 2025. "Balancing Layout Space and Risk Comprehension in Health Communication: A Comparison of Separated and Integrated Icon Arrays" Informatics 12, no. 4: 105. https://doi.org/10.3390/informatics12040105
APA StyleWang, L.-J., & Zheng, M.-C. (2025). Balancing Layout Space and Risk Comprehension in Health Communication: A Comparison of Separated and Integrated Icon Arrays. Informatics, 12(4), 105. https://doi.org/10.3390/informatics12040105






