Adopting Business Intelligence Techniques in Healthcare Practice
Abstract
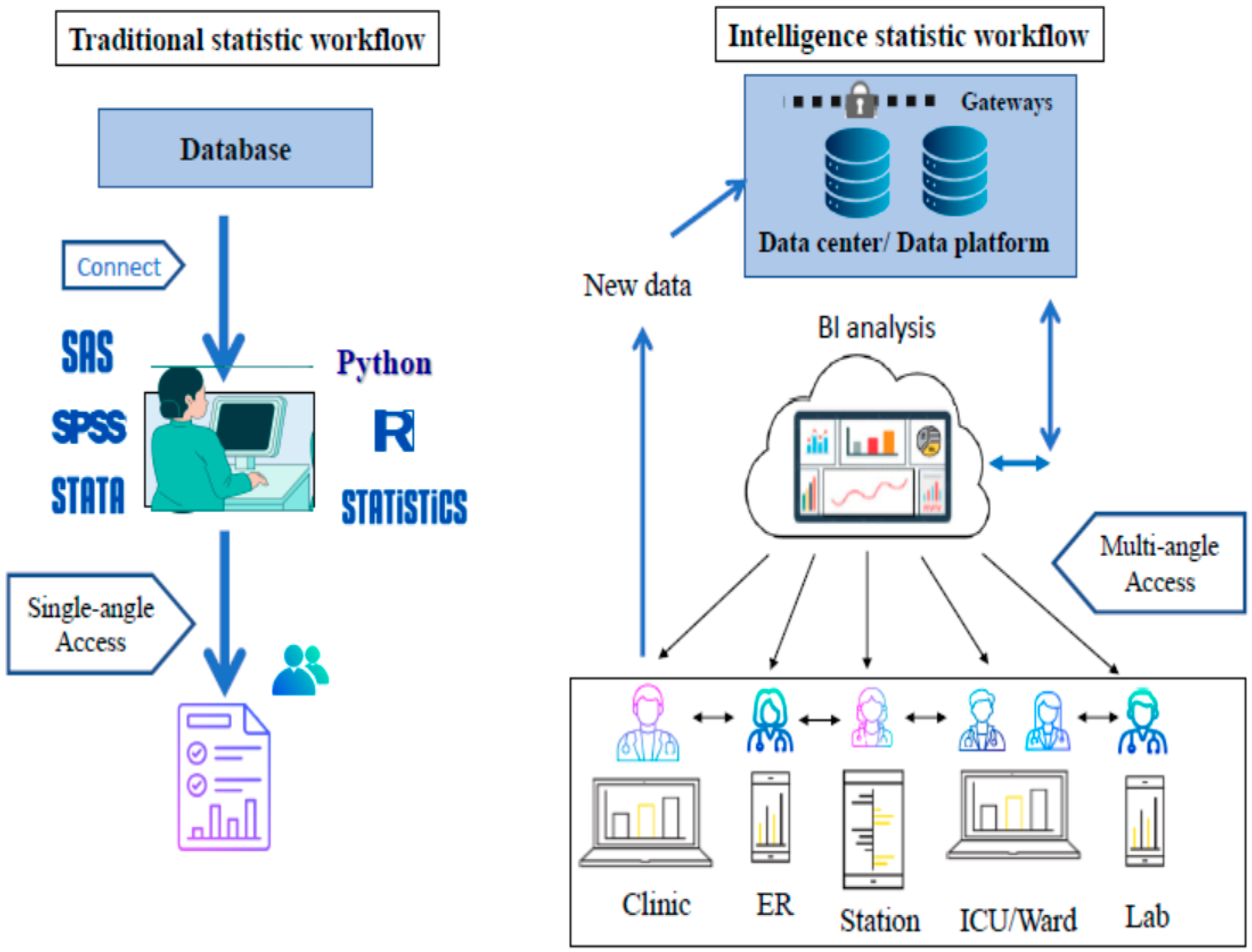
1. Introduction
2. Methods
2.1. Empirical Data Sources
2.2. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hung, M.; Bounsanga, J.; Voss, M.W. Interpretation of correlations in clinical research. Postgrad. Med. 2017, 129, 902–906. [Google Scholar] [CrossRef] [PubMed]
- Šendelj, R. Information Technology and Information Management in Healthcare. Stud. Health Technol. Inform. 2020, 274, 139–158. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Park, J. Identifying the Knowledge Structure and Trends of Nursing Informatics: A Text Network Analysis. Comput. Inform. Nurs. CIN 2023, 41, 8–17. [Google Scholar] [CrossRef]
- Loh, K.P.; McHugh, C.; Mohile, S.G.; Mustian, K.; Flannery, M.; Klepin, H.; Schnall, R.; Culakova, E.; Ramsdale, E. Using Information Technology in the Assessment and Monitoring of Geriatric Oncology Patients. Curr. Oncol. Rep. 2018, 20, 25. [Google Scholar] [CrossRef]
- Dehnavi, Z.; Ayatollahi, H.; Hemmat, M.; Abbasi, R. Health Information Technology and Diabetes Management: A Review of Motivational and Inhibitory Factors. Curr. Diabetes Rev. 2021, 17, 268–279. [Google Scholar] [CrossRef]
- Naseer Qureshi, K.; Din, S.; Jeon, G.; Piccialli, F. An accurate and dynamic predictive model for a smart M-Health system using machine learning. Inf. Sci. 2020, 538, 486–502. [Google Scholar] [CrossRef]
- Mintz, Y.; Brodie, R. Introduction to artificial intelligence in medicine. Minim. Invasive Ther. Allied. Technol. 2019, 28, 73–81. [Google Scholar] [CrossRef]
- Robert, N. How artificial intelligence is changing nursing. Nurs. Manag. 2019, 50, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Loewen, L.; Roudsari, A. Evidence for Busines Intelligence in Health Care: A Literature Review. Stud. Health Technol. Inform. 2017, 235, 579–583. [Google Scholar]
- Weng, S.S.; Yang, M.H.; Koo, T.L.; Hsiao, P.I. Modeling the prediction of business intelligence system effectiveness. SpringerPlus 2016, 5, 737. [Google Scholar] [CrossRef]
- Andrade, J.R.M.; Blomberg, L.C. Business intelligence applied to the consumption of iodinated contrast agents in computed tomography scans. BMC Med. Inform. Decis. Mak. 2022, 22, 76. [Google Scholar] [CrossRef] [PubMed]
- González-Pérez, C.; Llorente-Sanz, L.; Torrego-Ellacuría, M.; Molinero-Muñoz, M.; Liras-Medina, Á.; García-Sacristán, A.A.; Luaces, M.; Martínez-Sesmero, J.M. Business intelligence for the visualization and data analysis of Telepharmacy activity indicators in a hospital pharmacy service scorecard. Farm. Hosp. Organo Expr. Cient. Soc. Esp. Farm. Hosp. 2022, 46, 24–30. [Google Scholar]
- Welton, J.M. Business intelligence and nursing administration. J. Nurs. Adm. 2014, 44, 245–246. [Google Scholar] [CrossRef]
- Chu, H.Y.; Huang, H.C.; Huang, C.Y.; Chu, C.C.; Su, C.T.; Tsai, I.L.; Hu, H.L.S.; Guo, S.L. A predictive model for identifying low medication adherence among older adults with hypertension: A classification and regression tree model. Geriatr. Nurs. 2021, 42, 1309–1315. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.Y.; Yu, M.Y. Reliability and validity of the mammography screening beliefs questionnaire among Chinese American women. Cancer Nurs. 2003, 26, 131–142. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, S.; Chaplin, W.; Schoenthaler, A.M.; Ogedegbe, G. Revision and validation of the medication adherence self-efficacy scale (MASES) in hypertensive African Americans. J. Behav. Med. 2008, 31, 453–462. [Google Scholar] [CrossRef]
- Ho, C.; Yu, J.; Liu, T.; Lee, J.T. Factors Involved in the Medication Adherence of Hypertensive Patients. J. Nurs. Healthc. Res. 2014, 11, 23–32. [Google Scholar]
- Nguyen, N.T.T.; Vu, H.T.T.; Hu, H.L.; Lin, K.C.; Nguyen, T.X.; Huang, H.C. Applying classification and regression tree analysis to identify risks of developing sarcopenia in the older population. Int. J. Older People Nurs. 2022, 17, e12488. [Google Scholar] [CrossRef]
- Kuo, Y.T.; Kuo, L.K.; Chen, C.W.; Yuan, K.C.; Fu, C.H.; Chiu, C.T.; Yeh, Y.C.; Liu, J.H.; Shih, M.C. Score-based prediction model for severe vitamin D deficiency in patients with critical illness: Development and validation. Crit. Care 2022, 26, 394. [Google Scholar] [CrossRef]
- Al-Arkee, S.; Mason, J.; Lane, D.A.; Fabritz, L.; Chua, W.; Haque, M.S.; Jalal, Z. Mobile Apps to Improve Medication Adherence in Cardiovascular Disease: Systematic Review and Meta-analysis. J. Med. Internet Res. 2021, 23, e24190. [Google Scholar] [CrossRef]
- Alhussein, G.; Hadjileontiadis, L. Digital Health Technologies for Long-term Self-management of Osteoporosis: Systematic Review and Meta-analysis. JMIR mHealth uHealth 2022, 10, e32557. [Google Scholar] [CrossRef] [PubMed]
- Chin-Jung, L.; Hsiao-Yean, C.; Yeu-Hui, C.; Kuan-Chia, L.; Hui-Chuan, H. Effects of mobile health interventions on improving glycemic stability and quality of life in patients with type 1 diabetes: A meta-analysis. Res. Nurs. Health 2021, 44, 187–200. [Google Scholar] [CrossRef]
- Qi, W.; Wang, Y.; Li, C.; He, K.; Wang, Y.; Huang, S.; Li, C.; Guo, Q.; Hu, J. Predictive models for predicting the risk of maternal postpartum depression: A systematic review and evaluation. J. Affect. Disord. 2023, 333, 107–120. [Google Scholar] [CrossRef]
- Kernbach, J.M.; Staartjes, V.E. Foundations of Machine Learning-Based Clinical Prediction Modeling: Part II-Generalization and Overfitting. Acta Neurochir. Suppl. 2022, 134, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Godinho, T.M.; Lebre, R.; Almeida, J.R.; Costa, C. ETL Framework for Real-Time Business Intelligence over Medical Imaging Repositories. J. Digit. Imaging 2019, 32, 870–879. [Google Scholar] [CrossRef]
- Yuan, S.; Kroon, B.; Kramer, A. Building prediction models with grouped data: A case study on the prediction of turnover intention. Hum. Resour. Manag. J. 2023, 34, 20–38. [Google Scholar] [CrossRef]
- Fette, G.; Kaspar, M.; Liman, L.; Dietrich, G.; Ertl, M.; Krebs, J.; Störk, S.; Puppe, F. Exporting Data from a Clinical Data Warehouse. Stud. Health Technol. Inform. 2018, 248, 88–93. [Google Scholar] [PubMed]
- Wyllie, D.; Davies, J. Role of data warehousing in healthcare epidemiology. J. Hosp. Infect. 2015, 89, 267–270. [Google Scholar] [CrossRef]
- Afshartous, D.; de Leeuw, J. Prediction in Multilevel Models. J. Educ. Behav. Stat. 2005, 30, 109–139. [Google Scholar] [CrossRef]
- Handelman, G.S.; Kok, H.K.; Chandra, R.V.; Razavi, A.H.; Lee, M.J.; Asadi, H. eDoctor: Machine learning and the future of medicine. J. Intern. Med. 2018, 284, 603–619. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, H.-C.; Wang, H.-K.; Chen, H.-L.; Wei, J.; Yin, W.-H.; Lin, K.-C. Adopting Business Intelligence Techniques in Healthcare Practice. Informatics 2024, 11, 65. https://doi.org/10.3390/informatics11030065
Huang H-C, Wang H-K, Chen H-L, Wei J, Yin W-H, Lin K-C. Adopting Business Intelligence Techniques in Healthcare Practice. Informatics. 2024; 11(3):65. https://doi.org/10.3390/informatics11030065
Chicago/Turabian StyleHuang, Hui-Chuan, Hui-Kuan Wang, Hwei-Ling Chen, Jeng Wei, Wei-Hsian Yin, and Kuan-Chia Lin. 2024. "Adopting Business Intelligence Techniques in Healthcare Practice" Informatics 11, no. 3: 65. https://doi.org/10.3390/informatics11030065
APA StyleHuang, H.-C., Wang, H.-K., Chen, H.-L., Wei, J., Yin, W.-H., & Lin, K.-C. (2024). Adopting Business Intelligence Techniques in Healthcare Practice. Informatics, 11(3), 65. https://doi.org/10.3390/informatics11030065





