A Framework for Antecedents to Health Information Systems Uptake by Healthcare Professionals: An Exploratory Study of Electronic Medical Records
Abstract
1. Introduction
- Research Question. What are the factors that impact healthcare professionals’ uptake of EMR?
2. Materials and Methods
2.1. Method
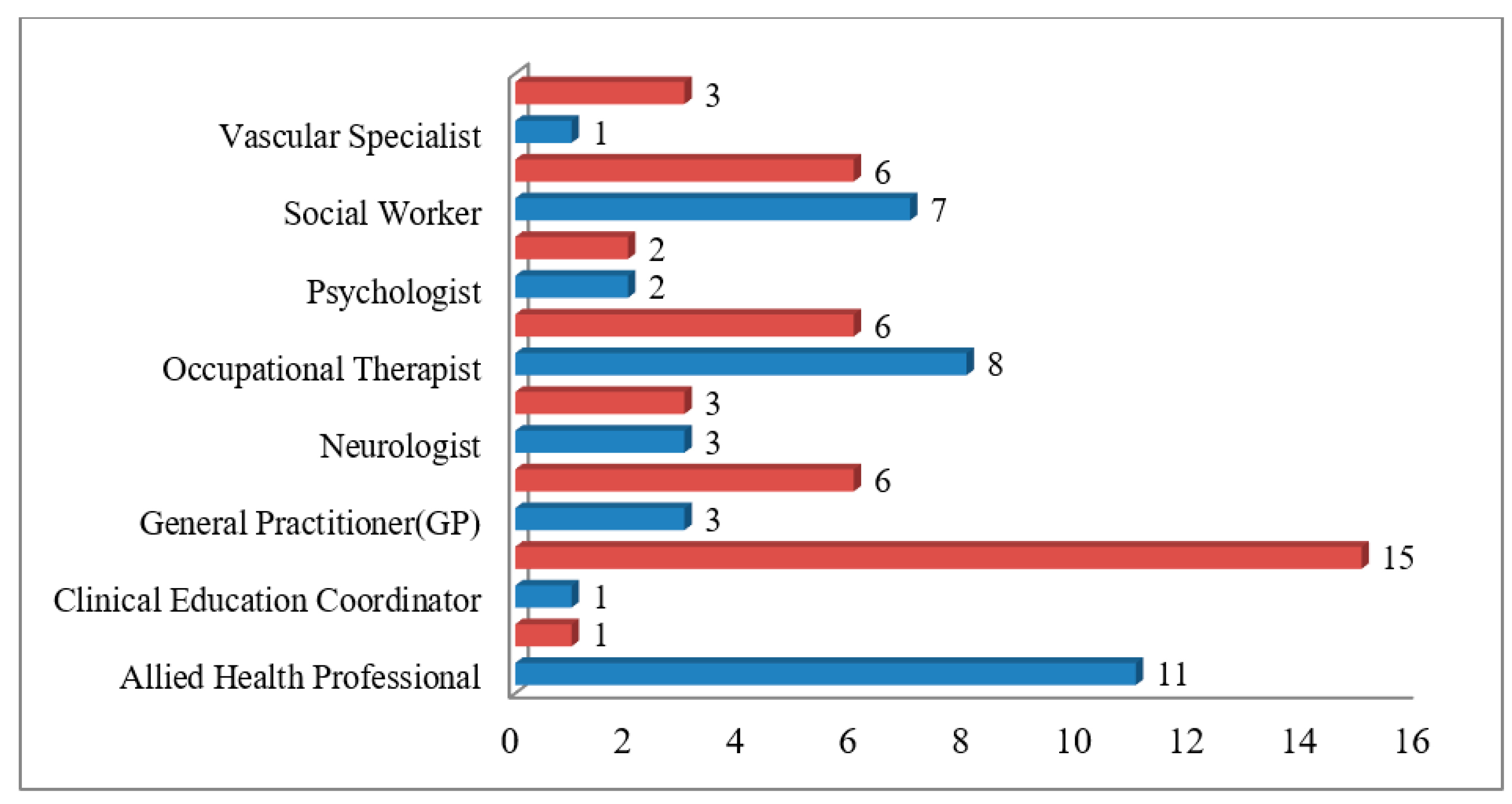
2.1.1. Data Collection
2.1.2. Data Analysis
2.1.3. Ethics Approval
3. Results
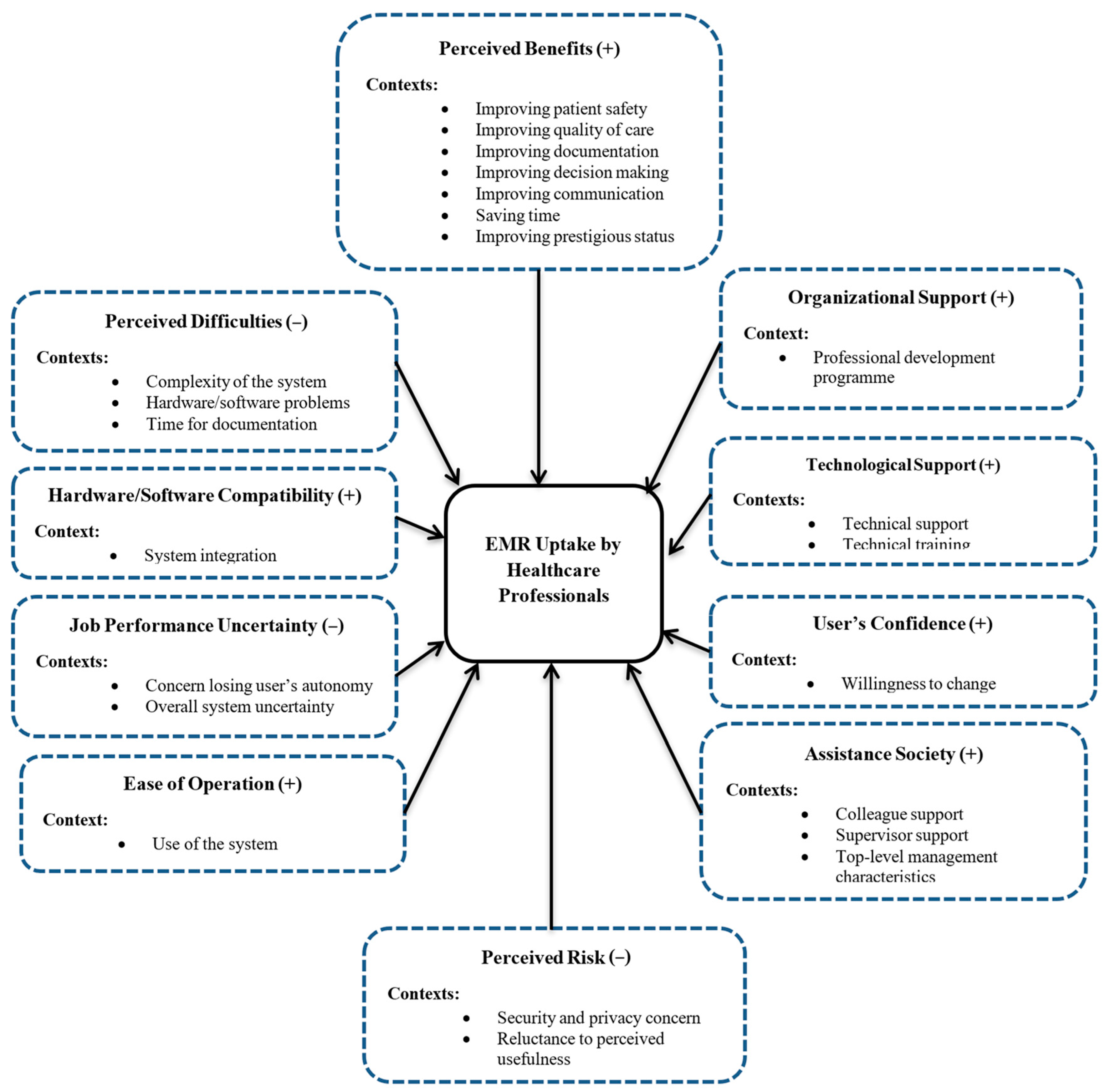
3.1. Perceived Benefits
3.2. Perceived Difficulties
3.3. Hardware/Software Compatibility
3.4. Job Performance Uncertainty
3.5. Ease of Operation
3.6. Perceived Risk
3.7. Assistance Society
3.8. User Confidence
3.9. Organisational Support
3.10. Technological Support
4. Discussion
4.1. Comparison with Previous Studies
4.2. Implications for Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| 1. Select age group 20–29 30–39 40–49 50–59 60 and above 2. Gender Male Female 3. What is your highest level of education? Associate’s degree Bachelor’s degree Master’s degree Doctorate Other 4. How long have you used the EMR system? 5. How often do you use EMR? 6. How do you feel about using an EMR system? 7. Please describe the advantages of the EMR system in the hospital. 8. Please describe the disadvantages of the EMR system in the hospital. 9. Have you faced any problems using the EMR system? Please clarify. 10. If any problem occurs, what steps do you take to identify and resolve the problem? 11. What do you expect most from your hospital to improve the existing EMR system? 12. Do you have any other thoughts about your experience with EMR? |
References
- Al-Dossary, H.; Alumran, A.; Al-Rayes, S.; Althumairi, A.; Aljanoubai, H.; Alhuseini, M.; Alkhaldi, O.; Al-Fayez, A.; Alanzi, T. An overview of health information management education in Saudi Arabia. Inform. Med. Unlocked 2021, 23, 100530. [Google Scholar] [CrossRef]
- Holden, R.J.; Karsh, B.-T. A theoretical model of health information technology usage behaviour with implications for patient safety. Behav. Inf. Technol. 2009, 28, 21–38. [Google Scholar] [CrossRef]
- Li, J.-S.; Zhang, X.-G.; Chu, J.; Suzuki, M.; Araki, K. Design and development of EMR supporting medical process management. J. Med. Syst. 2012, 36, 1193–1203. [Google Scholar] [CrossRef]
- Park, S.Y.; Lee, S.Y.; Chen, Y. The effects of EMR deployment on doctors’ work practices: A qualitative study in the emergency department of a teaching hospital. Int. J. Med. Inform. 2012, 81, 204–217. [Google Scholar] [CrossRef]
- Weihua, C.; Akay, M. Developing EMRs in Developing Countries. Information Technology in Biomedicine. IEEE Trans. Inf. Technol. Biomed. 2011, 15, 62–65. [Google Scholar] [CrossRef]
- Campion, T.R.; Waitman, L.R.; Lorenzi, N.M.; May, A.K.; Gadd, C.S. Barriers and facilitators to the use of computer-based intensive insulin therapy. Int. J. Med. Inform. 2011, 80, 863–871. [Google Scholar] [CrossRef]
- Carayon, P.; Smith, P.; Hundt, A.S.; Kuruchittham, V.; Li, Q. Implementation of an electronic health records system in a small clinic: The viewpoint of clinic staff. Behav. Inf. Technol. 2009, 28, 5–20. [Google Scholar] [CrossRef]
- Najaftorkaman, M.; Ghapanchi, A.H.; Talaei-Khoei, A.; Ray, P. A Taxonomy of Antecedents to User Adoption of Health Information Systems: A Synthesis of Thirty Years of Research. J. Am. Soc. Inf. Sci. Technol. 2013, 66, 576–598. [Google Scholar] [CrossRef]
- Hailegebreal, S.; Dileba, T.; Haile, Y.; Abebe, S. Health professionals’ readiness to implement electronic medical record system in Gamo zone public hospitals, southern Ethiopia: An institution based cross-sectional study. BMC Health Serv. Res. 2023, 23, 773. [Google Scholar] [CrossRef] [PubMed]
- Akwaowo, C.D.; Sabi, H.M.; Ekpenyong, N.; Isiguzo, C.M.; Andem, N.F.; Maduka, O.; Dan, E.; Umoh, E.; Ekpin, V.; Uzoka, F.-M. Adoption of electronic medical records in developing countries—A multi-state study of the Nigerian healthcare system. Front. Digit. Health 2022, 4, 1017231. [Google Scholar] [CrossRef]
- Cucciniello, M.; Lapsley, I.; Nasi, G.; Pagliari, C. Understanding key factors affecting electronic medical record implementation: A sociotechnical approach. BMC Health Serv. Res. 2015, 15, 268. [Google Scholar] [CrossRef]
- Ngugi, P.N.; Were, M.C.; Babic, A. Users’ perception on factors contributing to electronic medical records systems use: A focus group discussion study in healthcare facilities setting in Kenya. BMC Med. Inform. Decis. Mak. 2021, 21, 362. [Google Scholar] [CrossRef] [PubMed]
- Alanazi, B.; Butler-Henderson, K.; Alanazi, M.R. Factors influencing healthcare professionals’ perception towards EHR/EMR systems in gulf cooperation council countries: A systematic review. Oman Med. J. 2020, 35, e192. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Parpia, C.; Sriharan, A.; Keefe, D.T. Electronic medical record-related burnout in healthcare providers: A scoping review of outcomes and interventions. BMJ Open 2022, 12, e060865. [Google Scholar] [CrossRef]
- Tavares, J.; Goulão, A.; Oliveira, T. Electronic Health Record Portals adoption: Empirical model based on UTAUT2. Inform. Health Soc. Care 2018, 43, 109–125. [Google Scholar] [CrossRef] [PubMed]
- Adetoyi, O.E.; Raji, O.A. Electronic health record design for inclusion in sub-Saharan Africa medical record informatics. Sci. Afr. 2020, 7, e00304. [Google Scholar] [CrossRef]
- Liu, S. The impact of forced use on customer adoption of self-service technologies. Comput. Hum. Behav. 2012, 28, 1194–1201. [Google Scholar] [CrossRef]
- Jha, A.K.; DesRoches, C.M.; Campbell, E.G.; Donelan, K.; Rao, S.R.; Ferris, T.G.; Shields, A.; Rosenbaum, S.; Blumenthal, D. Use of electronic health records in U.S. hospitals. N. Engl. J. Med. 2009, 360, 1628–1638. [Google Scholar] [CrossRef]
- Schoen, C.; Osborn, R.; Squires, D.; Doty, M.; Rasmussen, P.; Pierson, R.; Applebaum, S. A survey of primary care doctors in ten countries shows progress in use of health information technology, less in other areas. Health Aff. 2012, 31, 2805–2816. [Google Scholar] [CrossRef]
- Boonstra, A.; Broekhuis, M. Barriers to the acceptance of electronic medical records by physicians from systematic review to taxonomy and interventions. BMC Health Serv. Res. 2010, 10, 231. [Google Scholar] [CrossRef]
- Kruse, C.S.; Kristof, C.; Jones, B.; Mitchell, E.; Martinez, A. Barriers to electronic health record adoption: A systematic literature review. J. Med. Syst. 2016, 40, 252. [Google Scholar] [CrossRef]
- Blumenthal, D.; Tavenner, M. The “meaningful use” regulation for electronic health records. N. Engl. J. Med. 2010, 363, 501–504. [Google Scholar] [CrossRef] [PubMed]
- Campanella, P.; Lovato, E.; Marone, C.; Fallacara, L.; Mancuso, A.; Ricciardi, W.; Specchia, M.L. The impact of electronic health records on healthcare quality: A systematic review and meta-analysis. Eur. J. Public Health 2016, 26, 60–64. [Google Scholar] [CrossRef]
- Black, A.D.; Car, J.; Pagliari, C.; Anandan, C.; Cresswell, K.; Bokun, T.; McKinstry, B.; Procter, R.; Majeed, A.; Sheikh, A. The impact of ehealth on the quality and safety of health care: A systematic overview. PLoS Med. 2011, 8, e1000387. [Google Scholar] [CrossRef]
- Alharthi, H.; Youssef, A.; Radwan, S.; Al-Muallim, S.; Zainab, A.-T. Physician satisfaction with electronic medical records in a major Saudi Government hospital. J. Taibah Univ. Med Sci. 2014, 9, 213–218. [Google Scholar] [CrossRef]
- Kaipio, J.; Lääveri, T.; Hyppönen, H.; Vainiomäki, S.; Reponen, J.; Kushniruk, A.; Borycki, E.; Vänskä, J. Usability problems do not heal by themselves: National survey on physicians’ experiences with EHRs in Finland. Int. J. Med. Inform. 2017, 97, 266–281. [Google Scholar] [CrossRef]
- Asan, O.; Montague, E. Technology-mediated information sharing between patients and clinicians in primary care encounters. Behav. Inf. Technol. 2014, 33, 259–270. [Google Scholar] [CrossRef]
- Popela, I.; Zuva, T.; Appiah, M. Factors That Influence the Adoption of Electronic Patients Records Management Systems in South Africa. In Proceedings of the 2019 International Multidisciplinary Information Technology and Engineering Conference, IMITEC 2019, Vanderbijlpark, South Africa, 21–22 November 2019. [Google Scholar]
- Gastaldi, L.; Radaelli, G.; Lettieri, E.; Luzzini, D.; Corso, M. Professionals’ use of ICT in hospitals: The interplay between institutional and rational factors. Int. J. Technol. Manag. 2019, 80, 85–106. [Google Scholar] [CrossRef]
- Alshahrani, A.; Stewart, D.; MacLure, K. A systematic review of the adoption and acceptance of eHealth in Saudi Arabia: Views of multiple stakeholders. Int. J. Med. Inform. 2019, 128, 7–17. [Google Scholar] [CrossRef]
- Vathanophas, V.; Pacharapha, T. Information Technology Acceptance in healthcare service: The study of Electronic Medical Record (EMR) in Thailand. In Proceedings of the Technology Management for Global Economic Growth (PICMET), 2010 Proceedings of PICMET’10 2010, Phuket, Thailand, 18–22 July 2010; IEEE: New York, NY, USA; pp. 1–5. [Google Scholar]
- Jawhari, B.; Ludwick, D.; Keenan, L.; Zakus, D.; Hayward, R. Benefits and challenges of EMR implementations in low resource settings: A state-of-the-art review. BMC Med. Inform. Decis. Mak. 2016, 16, 116. [Google Scholar] [CrossRef]
- Rowley, J. Using case studies in research. Manag. Res. News 2002, 25, 16–27. [Google Scholar] [CrossRef]
- Yin, R.K. Case Study Research: Design and Methods; Sage: Newcastle upon Tyne, UK, 2009; Volume 5. [Google Scholar]
- Biernacki, P.; Waldorf, D. Snowball sampling: Problems and techniques of chain referral sampling. Sociol. Methods Res. 1981, 10, 141–163. [Google Scholar] [CrossRef]
- Gibbs, G.R. Qualitative Data Analysis: Explorations with NVivo; Open University: Milton Keynes, UK, 2002. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Boyatzis, R.E. Transforming Qualitative Information: Thematic Analysis and Code Development; Sage: Newcastle upon Tyne, UK, 1998. [Google Scholar]

| Underlying factors | Improving patient safety Improving the quality of care Improving documentation Improving decision-making Improving communication Saving time Improving prestigious status |
| Example of data extracts | R18_improving patient safety: “EMR has key functions that can improve patient safety because data is entered electronically. It means that written errors and typos are eliminated in this computer-based system”. R26_improving quality of care: “patients’ records in the EMR are more comprehensive than paper records, and specialists can access these records and collaborate together to have better care”. |
| Underlying factors | The complexity of the system Hardware/software problems Time for documentation |
| Example of data extracts | R5_complexity of the system: “We lose documentation sometimes if it has not been saved. It’s not easy to cut and paste from each program. You need to paste into a Word document from meta-vision (specific program in the hospital) and then into EMR”. Z14_time for documentation: “Data entry takes a long time because we have to convert all charts and images, and I think that this should be improved to save nurses’ time”. |
| Underlying factors | System Integration |
| Example of data extracts | R44_system integration: “The benefit of the EMR system is connection with decision support systems so that managers can monitor workflow in the whole hospital. We don’t need anyone to enter data into the decision support system so it cuts down time taken on documentation”. |
| Underlying factors | Concern about losing user’s autonomy Overall system uncertainty |
| Example of data extracts | R15_concern about losing user’s autonomy: “I think that by using EMR we lose control over medical information, because data is shared with others and they can evaluate and modify that information”. R37_overall system uncertainty: “On a few occasions my data has been deleted by EMR. If it cannot be retrieved, this puts me under risk of litigation if evidence of my encounter with a patient is not input into patient charts”. |
| Underlying factors | Use of the system |
| Example of data extracts | R25_use of the system: “I can easily sort notes by date or type or profession. It can save my time and documentation, so that I can focus on my career”. |
| Underlying factors | Security and privacy concern Reluctance to perceive usefulness |
| Example of data extracts | R18_security and privacy concerns: “Paper-based medical records are much more secure than computer-based systems. Hackers can attack the system and destroy everything”. R48_psychological risk: “As a department supervisor, I know nurses who are reluctant to see the benefits of the system, so they are likely to do more paper work in the department. The nurses think that they have to spend more time in data entry processes”. |
| Underlying factors | Colleague support Supervisor support Top-level management characteristics |
| Example of data extracts | Z11_colleague support: “I do not have such good computer skills as my supervisor and colleagues. They are really helpful in solving my problems”. R12_supervisor support: “I think that the supervisor of each department should not only focus on managing line tasks, but should support their staff in other ways such as with technology-based issues. They should have regular contact with the EMR team to keep up to date with the latest EMR functionalities and changes”. |
| Underlying factors | Willingness to change |
| Example of data extracts | R43_willingness to change: “I believe that the EMR system can improve quality of care by organising medical information. By using the EMR system, doctors can interact with their patients in a timely manner. I am completely happy to use the computer system instead of paper documents”. |
| Underlying factors | Professional development program |
| Example of data extracts | R28_professional development program: “performance development modules in the hospital can be useful to develop users’ skills with the technology. Training is the first phase of performance development and we should encourage different department to set training sessions”. |
| Underlying factors | Technical support Technical training |
| Example of data extracts | R10_technical support: “When I faced any problems related to the EMR system, IT staff members were available by phone to help me to solve that issue. They are on the phone until I am OK with the system”. Participant R49 expressed “Formal technical training can help nurses to boost their computer skills to use EMR and I think that it’s essential for new staff”. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Torkman, R.; Ghapanchi, A.H.; Ghanbarzadeh, R. A Framework for Antecedents to Health Information Systems Uptake by Healthcare Professionals: An Exploratory Study of Electronic Medical Records. Informatics 2024, 11, 44. https://doi.org/10.3390/informatics11030044
Torkman R, Ghapanchi AH, Ghanbarzadeh R. A Framework for Antecedents to Health Information Systems Uptake by Healthcare Professionals: An Exploratory Study of Electronic Medical Records. Informatics. 2024; 11(3):44. https://doi.org/10.3390/informatics11030044
Chicago/Turabian StyleTorkman, Reza, Amir Hossein Ghapanchi, and Reza Ghanbarzadeh. 2024. "A Framework for Antecedents to Health Information Systems Uptake by Healthcare Professionals: An Exploratory Study of Electronic Medical Records" Informatics 11, no. 3: 44. https://doi.org/10.3390/informatics11030044
APA StyleTorkman, R., Ghapanchi, A. H., & Ghanbarzadeh, R. (2024). A Framework for Antecedents to Health Information Systems Uptake by Healthcare Professionals: An Exploratory Study of Electronic Medical Records. Informatics, 11(3), 44. https://doi.org/10.3390/informatics11030044









