Abstract
Nowadays, according to the intention of many hospitals and medical centers to computerize their processes and medical treatments, including data forms and medical images, which are generating a considerable amount of data, IT specialists and data scientists who are oriented to eHealth and related issues know the importance of data integration and its benefits. This study indicates the significance of data integration, especially in medical information systems. It means that the medical subsystems in the HIS (hospital information system) must be integrated, and it is also necessary to unify with the MIS (management information system). In this paper, the accuracy level of the extracted reports from the information system (to evaluate the staff’s performance) will be measured in two ways: (1) At first, the performance of the clinic reception staff will be evaluated. In this way, the personnel attendance system is an independent and separate software, and the mentioned evaluation has been performed by its report. (2) The following year, in the same location, the same evaluation has been performed based on the data extracted from the personnel attendance subsystem, which has been added to the medical information system as an integrated information system. After comparing the accuracy level of both ways, this paper concludes that when the personnel attendance subsystem as a part of the MIS has been unified with the HIS, the reports and, consequently, management decisions will be more accurate; therefore, the managers and decision-makers will perceive the importance of data integration more than in the past.
1. Introduction
Undoubtedly in recent years, almost everybody himself/herself or one of his/her family has dealt with medical information systems and their facilities, even in the format of an Internet lab answer, and all of them know the advantages of these systems compared to medical data on paper [1]. Several eHealth systems are used during the complete healthcare process. Starting from systems for managing patient documentation (e.g., an electronic health record (EHR)), managing organizational issues in a healthcare site (such as patient admission), and ending with financial systems. The basic concept of the EHR is that it is a virtual container for health-related documentation for a subject of care [2]. Data are continuously generated in medical scenarios, making data management a convoluted responsibility. In fact, not only several data sources can be involved, but also different data structures [1]. eHealth technologies, including electronic medical records (EMRs), computerized provider order entry (CPOE), e-Prescribing, and computerized decision support systems (CDSS), are promoted for their financial and clinical benefits. eHealth has become central to many government agendas worldwide [3]. The management information system (MIS) uses information technology, people, and business processes to record, store, and process data to produce information decision-makers can use to make day-to-day decisions [4]. Martin also notes that the complete form of MIS is management information systems. The purpose of a MIS is to extract data from varied sources and derive insights that drive business growth, including financials, inventory, personnel, project timelines, manufacturing, real estate, marketing, raw materials, and R&D. The MIS collects the data, stores it, and makes it accessible to managers who want to analyze the data by running reports. Conversely, the hospital/health information system (HIS) is an integrated information system that provides hospital information requirements for daily operations such as planning and patient care [5]. Regarding the medical processes, many HISs have their subsystems, including reception, sonography, radiology, patient queuing system, inpatients, etc. At the same time, it is prevalent among some hospitals to utilize a MIS as a separate software to manage their personnel and administrative processes whose subsystems consist of inventory, calculating salary, accounting, personnel attendance system, etc.
eHealth technologies today require not so many financial advantages as clinical advantages. In the 21st century, it has become more important for people (and hopefully for healthcare as well) to personify medical care, which can overcome the problem of doctors’ erroneous decisions [6,7].
There is a need for healthcare architecture for eHealth due to the failure of ICT (information and communication technology) and HIS investments in healthcare. Integration and interoperability play a significant role in this failure. The eHealth architectural model researchers propose that the demands of the healthcare system, the implementer, and the hardware must be considered [8]. Data integrity remains one of the most critical concerns for healthcare industries also. Data integrity breaches in healthcare institutions may have serious consequences [9]. They have pointed out that preserving data integrity in healthcare industries has become a challenging problem because of the healthcare institutions’ organizational structure that entails high-end point complexity and regulatory pressures.
In recent years, many companies, industries, and hospitals have tended to computerize their processes and interactions, but many senior managers are unaware of the importance of data integration and having unified information systems. Indeed, they mistakenly believe that even having separate and independent subsystems is enough. In contrast, we will indicate that although it is prevalent among hospitals to do so when we integrate them as integrated medical information (HIS + MIS), the extracted reports and subsequent decision-making will be more accurate and reliable. In this regard, through bolding the avails of data integration, especially in the medical information system, top managers and other decision-makers in this field will be encouraged to pay attention and dedicate an adequate budget to implement integrated medical information systems.
Few articles have addressed the integration of medical information systems and its effect on the accuracy of reports, which is a severe concern for data scientists, especially in medical information systems. Therefore, we have investigated the information system of Avicenna Infertility Center, including the HIS and the MIS, to assess the impact of this integration on the quality and accuracy of reports and the evaluation of staff performance. To this end, we have evaluated the performance of reception unit personnel in two different years: before and after the integration of the MIS and HIS (HIS + MIS). Therefore, in this paper, we investigate the impact on the accuracy level of information when the HIS and MIS, along with their subsystems, are merged to create a more integrated information system. Specifically, we aim to determine how much the reports and decisions will become more accurate.
We will illustrate that although the existence of a HIS and MIS may be a positive point for any hospital and medical center, it is not enough to achieve accurate reports and, consequently, perfect human evaluation. If we decide to reach reliable reports and accurate human evaluation, we must move forward the integrated information systems.
To achieve the goals outlined in this article, we will review the relevant literature on data integration and its importance in medical information systems. Next, we will describe the deployment of a HIS and MIS in medical centers and how they can be integrated. Following the integration, we will analyze the benefits that can be realized, particularly regarding the accuracy of information (through data analysis and the reception rate concept). Finally, we will summarize our findings and conclusions.
2. Related Works
Managing data integrity is a challenging task for any expert or researcher. Technological ecosystems applied to eHealth means an evolution of information systems to cover the heterogeneity of data flows and the evolution of the specific component that is integrated into the technological ecosystems. Data integrity techniques postulate that blockchain is the most prioritized data integrity technique [9]. This paper [10] presents a data integrity mechanism for an eHealth telemonitoring system that operates in a smart home and facilitates the transmission of medical data from the patient’s home to the healthcare center. The mechanism employs cryptographic smart cards and agent technology to ensure data integrity.
Andrea et al. [11] have clarified the relationship between data integration and integrity. This research has indicated that the processing of queries becomes more challenging when the global schema has integrity restrictions, even for primary forms. Similar to the source-centric approach to data integration, the issues mainly occur because it is necessary to cope with insufficient information.
Fabian et al. [12] have explained that predictive, preventative, customized, interactive, and digital healthcare will be the norm in the future. They have also claimed that for research and at the point of care, full data and information must be accessible as a foundation for specialized diagnosis and treatment. This paper has concluded that data exchange and integration will be crucial to accomplish these aims.
Temporal granularity will be one of the most significant technological problems in integrating consumer healthcare data with electronic medical records for chronic illness management [13]. In another paper, data integrity in medical information systems has been investigated: poor EHR system design and improper use can cause EHR-related errors that jeopardize the integrity of the information in the EHR, leading to errors that endanger patient safety or decrease the quality of care. This paper expresses that these unintended consequences may also increase fraud and abuse and have serious legal implications [14]. Using tools to automate the process ensures its validity and minimizes the risk of bias [15]. Another study aims to outline the threat landscape for data integrity in healthcare through a review of attack statistics from around the world and Saudi Arabia, focusing on the criticality of these threats in Saudi Arabia [16]. The findings of this systematic literature review suggest that the healthcare sector requires a more robust approach to data integrity.
Unfortunately, there are times when this massive volume of data’s privacy and integrity are not guaranteed. Many threats can change or even delete part of these logs [17]. This paper has proposed considering some of these threats and preventing their consequences in some eHealth systems. The increasing number of information sources and services in some domains, such as healthcare, increases the amount of information available. Therefore, there is a need to transform that information into knowledge [18].
One of the best articles in this field strongly emphasizes the importance of data integrity, particularly in healthcare systems. It explains that one of the significant issues with relying on networked data is the presence of ‘dirty data’ [19]. Dirty data may include incomplete, missing, or inaccurate information. Vimalachandran et al. [19] have also explained that the concern is particularly significant in health care, where dirty data represents the dark side of the great potential of adopting health-related IT systems. They have continued that, first and foremost, dirty data can lead to medical errors, which can kill or cause long-term damage to patients’ health. Data should be an accurate representation of its source, and it should be reliable. Another study [20] was conducted to evaluate the quality of operational data in an emergency department (ED) before and after the implementation of an electronic health record (EHR). It found that systematic errors and inaccuracies are common in EHR operational data in the immediate period after a typical EHR implementation. Ward et al. [20] described that administrators and policymakers should be aware of such possibilities during EHR implementation and should attempt to minimize the deleterious effects of EHR implementation on data integrity. There is a maintained trend regarding using of available web platforms as the core technology for information exchange and actors’ interaction in health ecosystems [21].
In addition, other authors have claimed that, undoubtedly, data has become one of the company’s most valuable assets [22]. The more appropriate data an organization has, the more successful it is likely to become. This is where data integrity becomes key. Data integrity has become a serious issue over recent years and is a core focus of many industries. Agrawal et al. [22] have expressed that integrity ensures that the data is original, correct, and safeguarded from unauthorized modification. There is also some academic review prepared by [23] which investigated integrating fundamental concepts, such as PHRs, EMRs, and EHRs, and related challenges. However, it has not pointed directly to integrating MIS and HIS; integrated data from EMRs, EHRs, and PHRs can create huge databases suitable for big data analysis methods and tools. Heart et al. [23] have added that this type of data analysis has great promise for driving personalized care and improving public health decision-making and health policy crafting.
Hsiao et al. [24] have discussed the need for integrated medical information systems. They state that as the structure and format of electronic patient records and prescriptions mature, it is essential to implement a comprehensive medical information system that integrates various electronic information systems. These authors stress the importance of making such a system applicable to the current medical environment, allowing for the integration of electronic patient records from all levels of medical centers and clinics, the secure transmission of these integrated records between them, the combined use of electronic prescriptions with patients’ medications, and the anonymous or confidential transmission of patients’ private data. Wang et al. [25] focus on the integration issues in eHealth that have been scientifically addressed and have concluded that different disciplines have different knowledge functions in the eHealth field. For example, medical and health-related disciplines supplied more knowledge of research subjects, entities, and research methodology, while information technology-related disciplines played a more prominent role in providing technology- and data-related knowledge. These authors have argued that the integration pattern of different knowledge types became stable along with the maturity of the eHealth field, which could reveal that the proportion of knowledge amount, references, and source disciplines, as well as citation interval of different knowledge types, were becoming stable in recent years.
Wu and Trigo [26] have examined the impact of information system integration on healthcare management and medical service. They highlight the importance of medical care combined with information technology as a new trend and note that the completeness and consistency of information directly affect the efficiency, quality, and safety of healthcare services. These authors also argue that the level of internet information technology is reflected in the degree to which data and applications are shared and accessed across different communication networks, a concept known as information systems integration.
In this regard, Raji’s dissertation on the regional integration of electronic medical records [27] has identified significant challenges to the regional integration of EMRs. Raji notes that despite the expansion of regional integration initiatives such as Clinical Connect, a regional EMR clinical viewer, physicians face challenges with implementation, support, and advanced use of electronic records. He concludes that physicians use EMRs fundamentally and do not fully utilize advanced, integrated features.
Franček et al. [28] have noted that integrated care and a comprehensive view of a patient’s care are highly sought in today’s healthcare systems. Medical information collected from various sources and accessed through EHRs by authorized users is the enabling technology behind this approach. This study provides an overview of different interoperability aspects related to data exchange and maps them to standard healthcare business processes. Additionally, Heart et al. [23] have researched the integration of EHRs, EMRs, and PHRs and argue that this integration of medical information, including demographic, lifestyle, and behavioral data with health records, leads to a more patient-centered approach to care. They also suggest that this can result in improved health and wellness but pose serious challenges and threats to security and privacy.
Another study has emphasized the importance of integrating EHRs into the national healthcare systems of low- and middle-income countries (LMICs) to meet the United Nations Sustainable Development Goal of promoting healthy lives and well-being for all people [29]. The authors also note that national EHR systems are on the rise, but mostly in developed countries.
Integrating patient-reported outcomes (PROs) into EHRs has been studied from a new perspective, highlighting the potential for improved patient–provider communication and care delivery. However, it has also been noted that new system implementations in healthcare institutions often involve changes to clinical workflow and organizational culture [30]. Specifically, this study [31] examines the ecosystem surrounding EHR-integrated PRO systems, including user needs and organizational factors. Dalal et al. [32] investigate whether an EHR-integrated patient portal is associated with an increased understanding of the care plan, including the critical recovery goal, among patients and clinicians in an acute care setting. They note that patient–clinician communication during acute care is suboptimal and that patient portals connected to the EHR have the potential to improve communication and mutual understanding about the care plan for seriously ill hospitalized patients. This is particularly important for facilitating goal-concordant care. There is also a study that has processed the other aspect of integrated EHRs and behavioral health in which it has been quoted that integrating behavioral health into primary care can improve care quality; however, most electronic health records are not designed to meet the needs of integrated teams [32]. Moreover, it has been concluded that health information technology tools designed for behavioral health integration must fit the needs of clinics for the successful uptake and improvement in patient experiences.
3. Deployment of HIS and MIS
As previously mentioned, IT professionals and other groups may use the terms HIS and MIS with different definitions. Many medical centers and hospitals use HIS for medical and treatment processes. In this more common usage, medical information systems, including various subsystems, are referred to as eHealth and consist of all medical images and data related to patients, as well as possibly some information about doctors and nurses, with a data structure as shown in Figure 1.
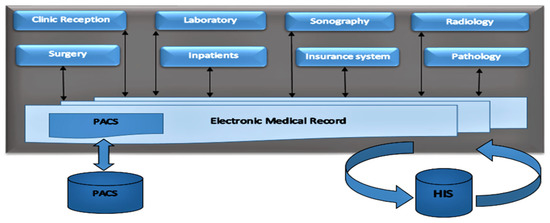
Figure 1.
The data structure in HIS.
3.1. Hospital Information System
A HIS is an information system that generally employs medical and industrial centers and enterprises to manage and perform administrative and official processes, including human resources, accounting, storage management, and a personnel attendance system. It is typically considered an independent and separate software consisting of several subsystems, as shown in Figure 2.
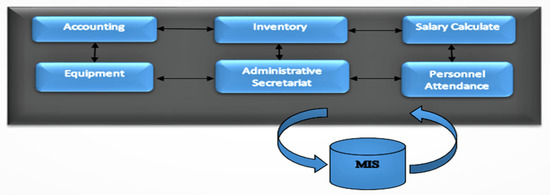
Figure 2.
Prevalent subsystems of MIS.
3.2. Management Information System
This often leads to using two different types of information systems, which are generally believed to be fundamentally different in terms of the nature and type of information they contain, and should therefore be kept separate. In this scenario, the MIS typically handles personnel salary calculations and evaluations, while the HIS manages the medical process of patients.
4. Transferring One Subsystem from MIS to HMIS
As we have pointed out in Figure 2, one of the subsystems of the management information system is the personnel attendance system. In Avicenna Clinic Infertility, this subsystem was typically placed within the MIS. However, at the end of 2019, IT specialists decided to move the subsystem from the MIS to a healthcare management information system (HMIS) to implement a more integrated information system. To facilitate this transition, the necessary technical confirmations were carried out as follows:
- o
- Performing fundamental definitions and professional expressions in the destination subsystem.
- o
- Connecting the attendance devices to the new subsystem.
- o
- Customizing the destination subsystem to prepare some features available in the MIS.
- o
- Carrying out the essential data entry such as identities, work shifts, leave, and mission authorizing also permitted delay and haste.
- o
- Building the necessary reports in the second personnel attendance subsystem.
In early 2020, the personnel attendance system that had been developed in the healthcare management information system (HMIS) was put into use. This meant that the staff presence, work time shifts, and all related processes were managed through the subsystem available in the HMIS. Calculating the active time, salaries, and even evaluating staff performance will now be more integrated.
Now that the previously-mentioned transfer of the personnel attendance system from the management information system to the healthcare management information system (HMIS) has taken place (as shown in Figure 3), it is possible to compare the accuracy level of the reports related to the evaluation of staff performance. To do this, we need to quantitatively evaluate the personnel using a measurable factor that can be calculated in both situations (before and after the subsystem was integrated). Therefore, we have utilized a professional term in the medical field called the reception rate (RR).
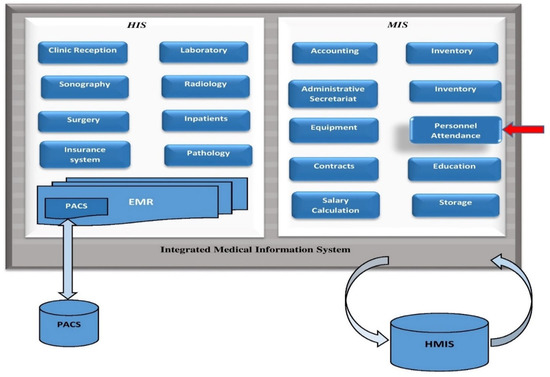
Figure 3.
HMIS (HIS + MIS). Red pointer highlights the recently inserted personnel attendance sub-system.
5. Reception Rate
When the personnel attendance system was placed in the separated software (MIS) and after its transmission to a HMIS, a measurable criterion was permanently used, known as the reception rate. This expression is used to evaluate reception personnel and calculates as follows:
Reception rate = number of admitted patients/number of useful working hours
The reception rate has been calculated for the reception personnel for 2019 and separately for 2020. In this study, the obtained reception rate related to 2019 is called abbreviated RR_19, and about 2020, it will be called RR_20.
For calculating RR_19, the number of admitted patients has been extracted from the HIS, whereas the number of working hours has been obtained from the MIS (independent software).
Undoubtedly, RR_20 has been obtained from both variables (the number of admitted patients and working hours) available in the HMIS.
In this step, we start rummaging into which RR_19 or RR_20 is more accurate and reliable. However, we know that RR_20 originated from an integrated information system and RR_19 from two separate ones.
6. Data Analysis
In this research, we will assess the accuracy level of the built reports by focusing on a measurable index to experiment with the consequences of integrating subsystems. Among the various available criteria, we have chosen the reception rate because no other intervention can affect the RR calculation over the two mentioned years. Therefore, it can be considered a symbol of the veracity of the built reports and, consequently, decision-making. The admission rate, as usual, will be calculated and used as a significant factor to evaluate the personnel’s annual (or, in some cases, monthly) performance, and this is why we have taken the annual calculation of this index in this study.
6.1. Data Extraction
During the study, we endeavor to determine what effect data integrity will have on calculating employee performance appraisal accuracy. For this purpose, we have compared the accuracy level of the admission rate calculation in two different circumstances:
- o
- Calculating the reception rate (RR_19) through two separate information systems: HIS and MIS.
- o
- Calculating the reception rate (RR_20) in an integrated information system: HMIS.
- o
- As we introduced before, to calculate the reception rate, we need both “the number of admitted patients” and the “number of working hours”. The necessary data has been extracted from the available reports, but in 2019, a part of the data (number of admitted patients) was in the HIS, and another part (number of working hours) was extracted from the MIS. In contrast, in 2020, both parts of the reception rate came from an integrated information system (HMIS). To clarify this issue, the extracted information and the sources used are given in Table 1.
 Table 1. Data extraction in 2019 and 2020.
Table 1. Data extraction in 2019 and 2020.
As indicated in Table 1, the sample consists of 21 reception personnel, including 15 females and 6 males. Their age is between 25 and 37 years. During 2019 and 2020, there has not been any change in the reception staff; consequently, some effective factors such as age, marital status, and education level have been controlled in this study. In addition, the work conditions and the type of tasks assigned to the mentioned individuals are the same (it is also worth mentioning that, although due to the issues related to the pandemic, exceptional circumstances prevailed in the world in 2020, the process of treating and accepting infertile couples did not change that year due to the age conditions and periodic medications of the patients, and strictness was only applied to the number of patients’ companions).
The required data, such as “the working hours” and “the admitted patients”, has been obtained from the available reports in the MIS, HIS, and HMIS as sources of data extraction (according to Table 1). Since we want to consider the impact of the integration of subsystems on the accuracy level of calculating the admission rate of all admission staff (not individually), we have included the average value of this characteristic in the calculations.
In 2019, the sum of the working hours which belong to these staff was divided by 21 to calculate the average (this calculation has occurred in the personnel attendance subsystem belongs to separate software of the MIS) while the number of admitted patients and also the average were extracted from the available reports in the HIS. In 2020, the mentioned variables were extracted from related reports in the reception and personnel attendance subsystem in the HMIS.
6.2. Statistical Analysis
According to the value of Sig. in the Shapiro–Wilk test in SPSS software, Sig. < 0.05 indicates that the variables are not normally distributed, so a Mann–Whitney U Test was applied to compare differences between the two groups.
The statistical data related to research variables are shown in Table 2.

Table 2.
Statistical data.
The statistical data in Table 2 indicates this study’s data distribution status. It also shows that the average admission rate in 2019 (RR_19) has been 0.35, and its standard deviation was 0.12; meanwhile, the number of these criteria for 2020 in the same order was (RR_20) 0.43 and (standard deviation) 0.11.
We are trying to answer this question: does adding the personnel attendance system to the HMIS affect the calculation of the admission rate, and if so, is it effective? To find an answer to this question, we used the Mann–Whitney statistical test in SPSS software, and the results have been inserted in Table 3.

Table 3.
The output of the Mann-Whitney Test.
Regarding Table 3, Mean Rank (related to the Reception Rate) was calculated at 18.71 in 2019, and the Sum of Ranks in the same year was 449.00, while the Mean Rank and Sum of Rank were 30.29 and 727.00 in 2020. As it shows, the Mann–Whitney value is 14,900. In addition, the number −2.87 was assigned to Z. Since the Significance Level was equal to 0.004 and the p-value < 0.05, we can conclude that the difference between the population medians is statistically significant and the assumption that adding personnel attendance system to the HMIS has caused the difference between RR_19 and RR_20 will be accepted.
6.3. Data Interpretation
We can look at this issue from another angle: looking at the statistics in Table 2, we will realize that the number of admitted patients in 2020 has increased by 31.24% compared to 2019, whereas the number of working hours in 2020 compared to 2019 has increased just by 4.2%. What is its meaning? The increasing trend of the admission rate in 2020 compared to 2019, with a ratio higher than the increasing working hours, shows the high accuracy of calculating RR_20. It is also indicated that due to the use of integrated information systems, personnel performance evaluation has been performed more accurately, and conversely, in the evaluation of performance among reception staff in 2019, some of the effective factors have been ignored.
7. Conclusions
Although immediately the number of hours related to the reception personnel increased in 2020 compared with 2019, this growth cannot cause an increase in the reception rate because the number of admitted patients increased by a more significant proportion. When an employee is working in the reception unit, they are spending their active time, and only the busy time should be the measurement criterion, not the length of time that the admission staff is in the hospital or medical center. Indeed, their busy time is a more critical factor and must be considered for the evaluation process, not just his or her presence at work. In the previous section, the effect of ignoring busy times due to the inability to separate software was visible. When a personnel attendance system is separate software, how can we (as an assessor) distinguish the active hours from inactive ones? The extracted reports from independent software will entail the arrival time, exit time, hourly leave, and duration (just these available data fields). It means that in this condition, when they calculate the reception rate, it cannot be accurate, and consequently, the evaluation which has been performed is not reliable.
When we are utilizing a separate MIS to calculate the reception rate, technically, it is impossible to consider and control all of the factors (even manually) affecting this calculation, and conversely. At the same time, HMIS is employed to gain the reception rate. Many influencing factors such as login time, active time, history of data entry (which user has registered patient’s data), and even canceled admitted patients will be carefully involved in the calculation. This is the same golden key and the great advantage of integrated systems.
Probably, many IT experts who are working in medical centers and hospitals have encountered the claim that in our expertise and field, the software of company X (for example) is the best and it has many features, and our group (for example, genetic group) prefers to utilize it. Although they are right, developing a subsystem that is completed every day and belongs to an integrated information system will help each company achieve its organizational purposes more than a complete and experienced but separate and independent software. This is precisely the same fact that we need to pay attention to about integration.
This study shows that when senior managers and decision-makers utilize the reports extracted from integrated information, they can be more accurate and reliable. So, despite the common method among many medical centers and hospitals in which they employ some professional software but independent and in the form of an island, it is not recommended by IT experts who perceive the importance of data integration. Even in some cases, there may be several defects and information gaps that definitely affect decision-making. Now, imagine this hazard taking place in the medical decision system and the fate of the patients.
We hope this issue can be good evidence to encourage all those who determine the strategies in the field of medical information systems, especially medical ones, and it can help to change (even a bit) their attitude.
Author Contributions
Funding
This research was partially funded by the Spanish Government Ministry of Science and Innovation through the AVisSA project grant number (PID2020-118345RB-I00).
Informed Consent Statement
Assurance was given to the participants that throughout the study, merely the summation of the working hours and admitted patients will be used and there are none of the reports related to the staff (separately for each user or personnel) in this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- García-Peñalvo, F.; Vázquez-Ingelmo, A.; García-Holgado, A.; Sampedro-Gómez, J.; Sánchez-Puente, A.; Vicente-Palacios, V.; Dorado-Díaz, P.I.; Sánchez, P.L. Application of Artificial Intelligence Algorithms Within the Medical Context for Non-Specialized Users: The CARTIER-IA Platform. Int. J. Interact. Multimed. Artif. Intell. 2021, 6, 46. [Google Scholar] [CrossRef]
- Hyla, T.; Pejaś, J. eHealth Integrity Model Based on a Permissioned Blockchain. In Proceedings of the 2019 Cybersecurity and Cyberforensics Conference (CCC), Melbourne, Australia, 8–9 May 2019; pp. 172–177. [Google Scholar]
- Hruby, G.W.; Matsoukas, K.; Cimino, J.J.; Weng, C. Facilitating biomedical researchers’ interrogation of electronic health record data: Ideas from outside of biomedical informatics. Biomed. Inform. 2016, 60, 376–384. [Google Scholar] [CrossRef] [PubMed]
- Martin, M. Available online: https://www.guru99.com/mis-definition.html (accessed on 15 January 2022).
- Johns, M. Information Management for Health Professions, 2nd ed.; Cengage Learning: Boston, MA, USA, 2002. [Google Scholar]
- Greve, P. HealthTrek: Medical Malpractice Claim Trends in 2017; Willis Towers Watson: London, UK, 2017. [Google Scholar]
- Strepetova, V. Ten A.R. Medical errors. Colloquium 2019, 12, 68–70. [Google Scholar]
- Adenuga, O.A.; Kekwaletswe, R.M.; Coleman, A. eHealth integration and interoperability issues: Towards a solution through enterprise architecture. Health Inf. Sci. Syst. 2015, 3, 1. [Google Scholar] [CrossRef]
- Pandey, K.A.; Irshad Khan, A.; Abushark, Y.B.; Alam, M.; Agrawal, A.; Kumar, R.; Khan, R.A. Key Issues in Healthcare Data Integrity: Analysis and Recommendations. IEEE Access 2020, 8, 40612–40628. [Google Scholar] [CrossRef]
- Mantas, G.; Lymberopoulos, D.; Komninos, N. Integrity Mechanism for eHealth Tele-monitoring System in Smart Home Environment. In Proceedings of the 31st Annual International Conference of the IEEE EMBS, Minneapolis, MN, USA, 3–6 September 2009. [Google Scholar]
- Calì, A.; Calvanese, D.; De Giacomo, G.; Lenzerini, M. Data integration under integrity constraints. Inf. Syst. 2004, 29, 147–163. [Google Scholar] [CrossRef]
- Prasser, F.; Kohlbacher, O.; Mansmann, U.; Bauer, B.; Kuhn, K.A. Data integration for future medicine (DIFUTURE). Methods Inf. Med. 2018, 57, e57–e65. [Google Scholar] [CrossRef]
- Tsumoto, S.; Hirano, S. Healthcare IT: Integration of consumer healthcare data an electronic medical records for chronic disease management. In Proceedings of the 2014 IEEE International Conference on Granular Computing (GrC), Noboribetsu, Japan, 22–24 October 2014; pp. 310–315. [Google Scholar]
- Bowman, S. Impact of Electronic Health Record Systems on Information Integrity: Quality and Safety Implications. Perspect. Health Inf. Manag. 2013, 10, 1c. [Google Scholar]
- García-Holgado, A.; García-Peñalvo, F.J. Validation of the learning ecosystem metamodel using transformation rules. Future Gener. Comput. Syst. 2019, 91, 300–309. [Google Scholar] [CrossRef]
- Zarour, M.; Alenezi, M.; Ansari, T.J.; Oandey, A.P.; Ahmad, M.; Agrawal, A.; Kumar, R.; Ahamd Khan, R. Ensuring data integrity of healthcare information in the era of digital health. IET Inst. Eng. Technol. 2021, 8, 66–77. [Google Scholar] [CrossRef]
- Camach, A.; Merayo, M.; Nunez, M. A Formal Passive Testing Approach to Control the Integrity of Private Information in eHealth Systems. In Recent Developments in Intelligent Information and Database Systems; Springer: Berlin, Germany, 2021; pp. 221–231. [Google Scholar]
- Vázquez-Ingelmo, A.; García-Holgado, A.; García-Peñalvo, F.J.; Therón, R. A Meta-Model Integration for Supporting Knowledge Discovery in Specific Domains: A Case Study in Healthcare. Sensors 2020, 20, 4072. [Google Scholar] [CrossRef] [PubMed]
- Vimalachandran, P.; Wang, H.; Zhang, Y.; Heyward, B.; Whittaker, F. Ensuring Data Integrity in Electronic Health Records: A Quality Health Care Implication. In Proceedings of the International Confrence on Orange Technologies, Melbourne, Australia, 18–20 December 2016. [Google Scholar]
- Ward, M.J.; Froehle, C.M.; Hart, K.W.; Lindsell, C.J. Operational data integrity during electronic health record implementation in the ED. Am. J. Emerg. Med. 2013, 31, 1029–1033. [Google Scholar] [CrossRef] [PubMed]
- García-Holgado, A.; Marcos-Pablos, S.; Therón-Sánchez, R.; García-Peñalvo, F.J. Technological Ecosystems in the Health Sector: A Mapping Study of European Research Projects. J. Med. Syst. 2019, 43, 100. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, A.; Alharbe, N.R. Need and Importance of Healthcare Data Integrity. Int. J. Eng. Technol. 2019, 11, 854–859. [Google Scholar] [CrossRef]
- Heart, T.; Ben-Assuli, O.; Shabtai, I. A review of PHR, EMR and EHR integration: A more personalized health care and public policy. Health Policy Technol. 2017, 6, 20–25. [Google Scholar] [CrossRef]
- Hsiao, T.-C.; Wu, Z.-Y.; Chung, Y.-F.; Chen, T.-S.; Horng, G.-B. A Secure Integrated Medical Information System. Meical Syst. 2012, 36, 3103–3113. [Google Scholar] [CrossRef]
- Wang, S.; Mao, J.; Tang, J.; Cao, Y. Content Characteristics of Knowledge Integration in the eHealth Field: An analysis based on citation contexts. Data Inf. Sci. 2021, 6, 58–74. [Google Scholar] [CrossRef]
- Wu, Z.; Trigo, V. Impact of information system integration on the healthcare management and medical services. Healthc. Manag. 2021, 14, 1348–1356. [Google Scholar] [CrossRef]
- Raji, S. Regional Integration: Physician Perceptions on Electronic Medical Record Use and Impact in Souhth West Ontario. Ph.D. Thesis, Western University, London, ON, Canada, 2020. [Google Scholar]
- Franček, P.; Žagar, M.; Sruk, V. Interoperability Within E-Health Arena. Fac. Electr. Enginnering Comput. Unska Zagreb Croat. 2015. [Google Scholar] [CrossRef]
- Kumar, M.; Mostafa, J. Research evidence on strategies enabling integration of electronic health records in the health care systems of low- and middle-income countries: A literature review. Health Plan. Manag. 2019, 34, e1016–e1025. [Google Scholar] [CrossRef]
- Zhang, R.; Burgess, E.R.; Reddy, M.C.; Rothrock, N.E.; Bhatt, S.; Rasmussen, L.V.; Butt, Z.; Starren, J.B. Provider perspectives on the integration of patient-reported outcomes in an electronic health record. JAMIA 2019, 2, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Jetelina, K.K.; Woodson, T.T.; Gunn, R.; Muller, B.; Khaya, D.C.; DeVoe, J.E.; Balasubramanian, B.A.; Cohen, D.J. Evaluation of an Electronic Health Record (EHR) Tool for Integrated Behavioral Health in Primary Care. Am. Board Fam. Med. 2018, 31, 712–723. [Google Scholar] [CrossRef] [PubMed]
- Dalal, A.K.; Dykes, P.; Samal, L.; McNally, K.; Mlaver, E.; Yoon, C.S.; Lipsitz, S.R.; Bates, D.W. Potential of an Electronic Health Record-Integrated Patient Portal for Improving Care Plan Concordance during Acute Care. Clin. Inform. 2019, 10, 358–366. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).