Staff Perceptions of Family-Centered Care in Italian Neonatal Intensive Care Units: A Multicenter Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Ethics
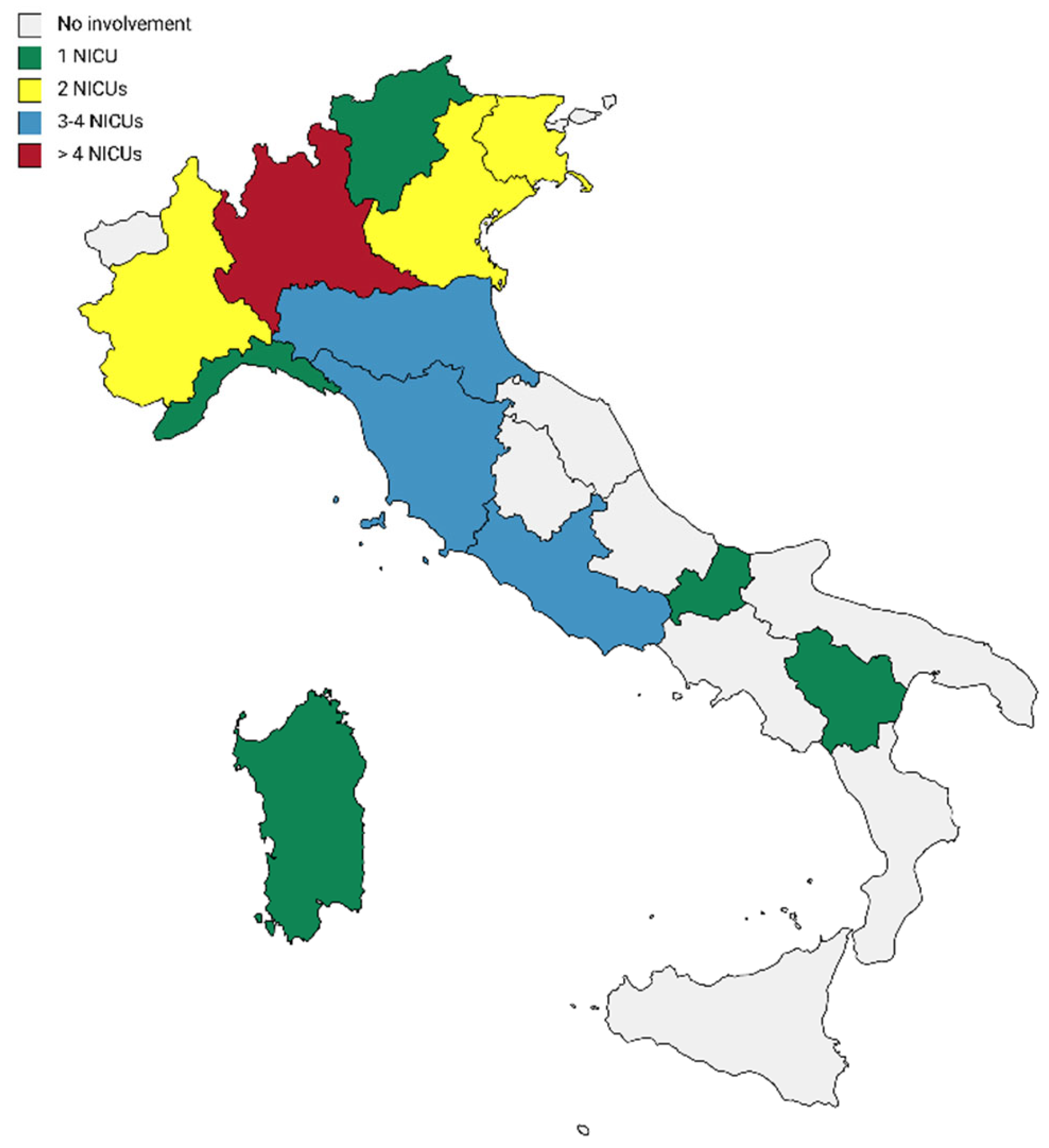
2.2. Participants
2.3. The Family-Centred Care Questionnaire-Revised (FCCQ-R)
2.4. Data Collection
2.5. Data Analysis
3. Results
3.1. Participants
3.2. Reliability of the FCCQ-R@it-NICU
3.3. Current and Necessary Activities of the FCCQ-R@it-NICU
3.4. Associations between FCCQ-R@it-NICU Scores and Participants’ Characteristics
3.5. Regression Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Current | Necessary | |
|---|---|---|
| FCCQ-R@it-NICU | Mean (SD) | Mean (SD) |
| The family as the constant of the child’s life | ||
| 1. Staff encourage parents and just in case also siblings to come and go any time that meets the family’s needs | 3.30 (1.16) | 4.15 (0.98) |
| 2. Staff work with families to determine the level of participation in direct care and decision-making that suits the family’s needs best | 3.50 (1.03) | 4.33 (0.77) |
| 3. The family is the key decision maker in the care of their infant | 2.37 (1.00) | 3.20 (1.16) |
| Parent and professional collaboration | ||
| 4. Staff determine the infant’s needs in consultation with the family and other health professionals | 3.35 (1.06) | 4.18 (0.85) |
| 5. Parents contribute to the development and review of hospital policies and practices | 2.24 (0.99) | 2.23 (0.98) |
| 6. Parents and siblings are involved in staff continuing education Programs in various ways. | 1.98 (0.98) | 1.96 (0.96) |
| 7. Educational programs (for family members) and written material convey the sense that families are the key actors in care. | 2.82 (1.05) | 2.80 (1.05) |
| 8. The admission process is used, when possible, as an opportunity to begin involving the family as members in the health care team. [if possible] | 3.50 (1.05) | 3.48 (1.05) |
| 9. Hospital facilities, policies, and procedures foster family choices for participation. | 2.92 (1.10) | 2.90 (1.09) |
| 10. Interviews with families are conducted in a private location. | 3.12 (1.31) | 4.57 (0.70) |
| 11. Explanations are presented to the family, using a variety of techniques depending on the individual needs and learning styles of the family | 3.58 (1.08) | 4.52 (0.67) |
| 12. Staff are aware of and take approaches that address the fact that families take time to develop trust. | 3.77 (0.82) | 4.45 (0.60) |
| 13. Staff discuss with the family what helps them deal with events during hospitalization | 3.68 (0.85) | 4.40 (0.66) |
| 14. Staff assess the level of understanding and skills of the family before and after teaching. | 3.78 (0.87) | 4.44 (0.60) |
| Sharing information with parents | ||
| 15. Staff promote, when possible, the infant’s preadmission information program, through which families familiarize with hospital ward staff, routines, and equipment prior to a scheduled admission to the PICU. | 2.40 (1.08) | 3.82 (0.97) |
| 16. After an emergency admission or unscheduled admission, there is an organized system for helping families understand and adjust to the health care experience. | 2.94 (1.10) | 4.22 (0.70) |
| 17. Information is routinely communicated to help families understand each aspect of care that their infant will experience such as anticipated sequence of events, reasons for change/treatment/procedure, ways to cope. | 3.50 (0.95) | 4.38 (0.68) |
| 18. Any family member significantly involved in the infant care is encouraged to discuss or chart information about the care of their infant. | 2.80 (1.04) | 3.79 (0.98) |
| 19. Staff coordinate the flow and sequence of information given to families, ensuring that the infant’s needs are apriority. | 3.57 (0.94) | 4.29 (0.69) |
| Parent-to-parent support | ||
| 20. Staff encourage parents to discuss concerns with other parents with similar experiences informally or in formal parent groups. | 3.16 (1.09) | 4.11 (0.88) |
| 21. Staff provide programs and support for parents, siblings and members of the extended family to assist families in managing needs | 2.94 (1.09) | 4.19 (0.78) |
| 22. Staff assess the needs and concerns of siblings. | 2.44 (1.09) | 3.78 (0.98) |
| 23. There is a designated comfortable area for parents to gather. | 2.97 (1.35) | 4.29 (0.78) |
| Developmental needs | ||
| 24. Staff help family to establish/stay in touch with their family and significant others | 2.68 (1.04) | 3.71 (0.92) |
| 25. Direct care managers have an adequate knowledge in infant development to support hospital staff in the practice of family-centred care. | 3.44 (1.12) | 4.29 (0.72) |
| 26. Hospital brochures accurately describe the health care experience for infant and their families. | 3.08 (1.12) | 4.27 (0.75) |
| 27. Staff maintain familiar routines for each infant and family. | 2.56 (1.01) | 3.71 (0.94) |
| 28. Staff assess the infant interaction with staff and family. | 3.56 (0.91) | 4.15 (0.75) |
| Emotional and financial support for families | ||
| 29. When possible, the same staff are assigned to care for the infant and family. | 3.05 (1.19) | 3.93 (1.00) |
| 30. Information and support are provided to help families understand the illness process and the impact on the infant and family, choices and risks, services, and roles of various health professionals | 3.61 (0.91) | 4.36 (0.69) |
| 31. Staff recognize the financial strain on families and assist them in obtaining help | 3.40 (1.00) | 4.06 (0.80) |
| 32. During procedures, a staff member is designated to explain to the family exactly what is happening. | 2.64 (1.06) | 3.98 (0.84) |
| Design of health care system | ||
| 33. Outpatient services are available daily and in the evening hours. | 2.10 (1.04) | 3.62 (1.03) |
| 34. All written material for families is available in Italian or in the mostly commonly spoken languages | 3.33 (1.11) | 4.19 (0.76) |
| 35. A written summary of relevant information about the infant is available in the primary official language of the family. | 2.40 (1.12) | 4.08 (0.82) |
| 36. The physical layout of the unit is designed to meet the developmental and psychosocial needs of infant and family | 2.32 (1.12) | 4.24 (0.86) |
| 37. Resources exist to help provide families with the appropriate support that they need at varying times | 2.86 (1.04) | 4.13 (0.78) |
| 38. Parent evaluations are considered reliable sources of information about how well the hospital meets their needs. | 3.29 (0.93) | 3.99 (0.80) |
| 39. Staffing patterns are planned according to the developmental and psychosocial needs of infant. | 2.98 (1.10) | 4.08 (0.84) |
| Emotional support for staff | ||
| 40. There are guidelines to assist staff in providing care during painful procedures such as: implementing pain-relieving techniques and ways to keep the child calm during and after the procedure | 4.11 (0.92) | 4.56 (0.65) |
| 41. Job descriptions and performance appraisal systems incorporate expectations of family-centred care such as: knowledge of family dynamics and skills in collaboration, problem solving and interventions that address family’s needs | 2.90 (0.97) | 3.96 (0.76) |
| 42. Continuing education programs provide opportunities for staff to learn to approach families effectively | 3.06 (1.0) | 4.23 (0.75) |
| 43. The hospital recognizes and rewards staff’s specific knowledge and skills that are needed to care for infants and families | 2.17 (1.04) | 4.21 (0.87) |
| 44. Staff are encouraged to identify, plan and evaluate new programs, policies and procedures to improve the quality of infant and family care. | 3.11 (1.11) | 4.32 (0.70) |
| 45. Staff are able to express confidentially to those responsible for assuring quality care, their concerns related to those demands of providing care for their infants and families | 3.40 (1.06) | 4.26 (0.67) |
References
- Latour, J.M.; Hazelzet, J.A.; Duivenvoorden, H.J.; van Goudoever, J.B. Perceptions of Parents, Nurses, and Physicians on Neonatal Intensive Care Practices. J. Pediatr. 2010, 157, 215–220.e3. [Google Scholar] [CrossRef] [PubMed]
- Montirosso, R.; Del Prete, A.; Bellù, R.; Tronick, E.; Borgatti, R. Neonatal Adequate Care for Quality of Life (NEO-ACQUA) Study Group Level of NICU Quality of Developmental Care and Neurobehavioral Performance in Very Preterm Infants. Pediatrics 2012, 129, e1129–e1137. [Google Scholar] [CrossRef] [PubMed]
- Ramezani, T.; Hadian Shirazi, Z.; Sabet Sarvestani, R.; Moattari, M. Family-Centered Care in Neonatal Intensive Care Unit: A Concept Analysis. Int. J. Community Based Nurs. Midwifery 2014, 2, 268–278. [Google Scholar] [PubMed]
- Hadian Shirazi, Z.; Sharif, F.; Rakhshan, M.; Pishva, N.; Jahanpour, F. The Obstacles against Nurse-Family Communication in Family-Centered Care in Neonatal Intensive Care Unit: A Qualitative Study. J. Caring Sci. 2015, 4, 207–216. [Google Scholar] [CrossRef]
- Harrison, T.M. Family Centered Pediatric Nursing Care: State of the Science. J. Pediatr. Nurs. 2010, 25, 335–343. [Google Scholar] [CrossRef]
- Malusky, S.K. A Concept Analysis of Family-Centered Care in the NICU. Neonatal Netw. 2005, 24, 25–32. [Google Scholar] [CrossRef]
- Mirlashari, J.; Brown, H.; Fomani, F.K.; de Salaberry, J.; Zadeh, T.K.; Khoshkhou, F. The Challenges of Implementing Family-Centered Care in NICU from the Perspectives of Physicians and Nurses. J. Pediatr. Nurs. 2020, 50, e91–e98. [Google Scholar] [CrossRef]
- Saxton, S.N.; Walker, B.L.; Dukhovny, D. Parents Matter: Examination of Family Presence in the Neonatal Intensive Care Unit. Am. J. Perinatol. 2021, 38, 1023–1030. [Google Scholar] [CrossRef]
- Soni, R.; Tscherning, C. Family-Centred and Developmental Care on the Neonatal Unit. Paediatr. Child Health 2021, 31, 18–23. [Google Scholar] [CrossRef]
- Klein, V.; Zores-Koenig, C.; Dillenseger, L.; Langlet, C.; Escande, B.; Astruc, D.; Le Ray, I.; Kuhn, P.; Group, S.N.S. Changes of Infant- and Family-Centered Care Practices Administered to Extremely Preterm Infants during Implementation of the NIDCAP Program. Front. Pediatr. 2021, 9, 718813. [Google Scholar] [CrossRef]
- Solhaug, M.; Torunn Bjørk, I.; Pettersen Sandtrø, H. Staff Perception One Year After Implementation of the The Newborn Individualized Developmental Care and Assessment Program (NIDCAP). J. Pediatr. Nurs. 2010, 25, 89–97. [Google Scholar] [CrossRef]
- Arabiat, D.; Whitehead, L.; Foster, M.; Shields, L.; Harris, L. Parents’ Experiences of Family Centred Care Practices. J. Pediatr. Nurs. 2018, 42, 39–44. [Google Scholar] [CrossRef]
- Shields, L. What Is “Family-Centred Care”? Eur. J. Pers. Cent. Healthc. 2015, 3, 139–144. [Google Scholar] [CrossRef]
- Dunn, M.S.; Reilly, M.C.; Johnston, A.M.; Hoopes, R.D.; Abraham, M.R. Development and Dissemination of Potentially Better Practices for the Provision of Family-Centered Care in Neonatology: The Family-Centered Care Map. Pediatrics 2006, 118 (Suppl. S2), S95–S107. [Google Scholar] [CrossRef]
- Fisher, C.; Lindhorst, H.; Matthews, T.; Munroe, D.J.; Paulin, D.; Scott, D. Nursing Staff Attitudes and Behaviours Regarding Family Presence in the Hospital Setting. J. Adv. Nurs. 2008, 64, 615–624. [Google Scholar] [CrossRef]
- Foster, M.J.; Whitehead, L.; Maybee, P.; Cullens, V. The Parents’, Hospitalized Child’s, and Health Care Providers’ Perceptions and Experiences of Family Centered Care within a Pediatric Critical Care Setting: A Metasynthesis of Qualitative Research. J. Fam. Nurs. 2013, 19, 431–468. [Google Scholar] [CrossRef]
- Gill, S.D.; Dunning, T.; McKinnon, F.; Cook, D.; Bourke, J. Understanding the Experience of Inpatient Rehabilitation: Insights into Patient-Centred Care from Patients and Family Members. Scand. J. Caring Sci. 2014, 28, 264–272. [Google Scholar] [CrossRef]
- Franki, I.; Desloovere, K.; De Cat, J.; Feys, H.; Molenaers, G.; Calders, P.; Vanderstraeten, G.; Himpens, E.; Van Den Broeck, C. The Evidence-Base for Conceptual Approaches and Additional Therapies Targeting Lower Limb Function in Children with Cerebral Palsy: A Systematic Review Using the International Clasification of Functioning, Disability and Health as a Framework. J. Rehabil. Med. 2012, 44, 396–405. [Google Scholar] [CrossRef]
- Foster, M.; Whitehead, L.; Maybee, P. The Parents’, Hospitalized Child’s, and Health Care Providers’ Perceptions and Experiences of Family-Centered Care Within a Pediatric Critical Care Setting: A Synthesis of Quantitative Research. J. Fam. Nurs. 2016, 22, 6–73. [Google Scholar] [CrossRef]
- Al-Motlaq, M.A.; Carter, B.; Neill, S.; Hallstrom, I.K.; Foster, M.; Coyne, I.; Arabiat, D.; Darbyshire, P.; Feeg, V.D.; Shields, L. Toward Developing Consensus on Family-Centred Care: An International Descriptive Study and Discussion. J. Child Health Care 2019, 23, 458–467. [Google Scholar] [CrossRef]
- Sitzia, J.; Wood, N. Patient Satisfaction: A Review of Issues and Concepts. Soc. Sci. Med. 1997, 45, 1829–1843. [Google Scholar] [CrossRef]
- Mastro, K.A.; Flynn, L.; Preuster, C. Patient- and Family-Centered Care: A Call to Action for New Knowledge and Innovation. J. Nurs. Adm. 2014, 44, 446–451. [Google Scholar] [CrossRef]
- Feeg, V.D.; Paraszczuk, A.M.; Çavuşoğlu, H.; Shields, L.; Pars, H.; Al Mamun, A. How Is Family Centered Care Perceived by Healthcare Providers from Different Countries? An International Comparison Study. J. Pediatr. Nurs. 2016, 31, 267–276. [Google Scholar] [CrossRef]
- Davies, R. Marking the 50th Anniversary of the Platt Report: From Exclusion, to Toleration and Parental Participation in the Care of the Hospitalized Child. J. Child Health Care 2010, 14, 6–23. [Google Scholar] [CrossRef]
- Abraham, M.; Moretz, J.G. Implementing Patient- and Family-Centered Care: Part I—Understanding the Challenges. Pediatr. Nurs. 2012, 38, 44–47. [Google Scholar]
- Moretz, J.G.; Abraham, M. Implementing Patient- and Family-Centered Care: Part II—Strategies and Resources for Success. Pediatr. Nurs. 2012, 38, 106–171. [Google Scholar]
- Dall’Oglio, I.; Di Furia, M.; Tiozzo, E.; Gawronski, O.; Biagioli, V.; Di Ciommo, V.M.; Paoletti, S.; Bianchi, N.; Celesti, L.; Raponi, M.; et al. Practices and Perceptions of Family Centered Care among Healthcare Providers: A Cross-Sectional Study in a Pediatric Hospital. J. Pediatr. Nurs. 2018, 43, e18–e25. [Google Scholar] [CrossRef]
- Bruce, B.; Ritchie, J. Nurses’ Practices and Perceptions of Family-Centered Care. J. Pediatr. Nurs. 1997, 12, 214–222. [Google Scholar] [CrossRef]
- Greenlaw, C.; Brown-Welty, S. A Comparison of Web-Based and Paper-Based Survey Methods: Testing Assumptions of Survey Mode and Response Cost. Eval. Rev. 2009, 33, 464–480. Available online: https://journals.sagepub.com/doi/10.1177/0193841X09340214 (accessed on 18 February 2022). [CrossRef] [PubMed]
- Monticone, M.; Galeoto, G.; Berardi, A.; Tofani, M. Psychometric Properties of Assessment Tools. In Measuring Spinal Cord Injury: A Practical Guide of Outcome Measures; Galeoto, G., Berardi, A., Tofani, M., Auxiliadora Marquez, M., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 7–15. ISBN 978-3-03068-382-5. [Google Scholar]
- Mokkink, L.; Terwee, C.; Knol, D.; Stratford, P.; Alonso, J.; Patrick, D.; Bouter, L.; de Vet, H. Protocol of the COSMIN Study: COnsensus-Based Standards for the Selection of Health Measurement INstruments. BMC Med. Res. Methodol. 2006, 6, 2. [Google Scholar] [CrossRef] [PubMed]
- Mokkink, L.B.; Terwee, C.B.; Patrick, D.L.; Alonso, J.; Stratford, P.W.; Knol, D.L.; Bouter, L.M.; de Vet, H.C.W. The COSMIN Checklist for Assessing the Methodological Quality of Studies on Measurement Properties of Health Status Measurement Instruments: An International Delphi Study. Qual. Life Res. 2010, 19, 539–549. [Google Scholar] [CrossRef]
- Bruce, B.; Letourneau, N.; Ritchie, J.; Larocque, S.; Dennis, C.; Elliott, M.R. A Multisite Study of Health Professionals’ Perceptions and Practices of Family-Centered Care. J. Fam. Nurs. 2002, 8, 408–429. [Google Scholar] [CrossRef]
- Dall’Oglio, I.; Mascolo, R.; Tiozzo, E.; Portanova, A.; Fiori, M.; Gawronski, O.; Dotta, A.; Piga, S.; Offidani, C.; Alvaro, R.; et al. The Current Practice of Family-Centred Care in Italian Neonatal Intensive Care Units: A Multicentre Descriptive Study. Intensive Crit. Care Nurs. 2019, 50, 36–43. [Google Scholar] [CrossRef]
- Coyne, I.; Murphy, M.; Costello, T.; O’Neill, C.; Donnellan, C. A Survey of Nurses’ Practices and Perceptions of Family-Centered Care in Ireland. J. Fam. Nurs. 2013, 19, 469–488. [Google Scholar] [CrossRef]
- Phiri, P.G.M.C.; Chan, C.W.H.; Wong, C.L.; Choi, K.C.; Ng, M.S.N. Discrepancies between Nurses’ Current and Perceived Necessary Practices of Family-Centred Care for Hospitalised Children and Their Families: A Cross-Sectional Study. J. Pediatr. Nurs. 2022, 62, e25–e31. [Google Scholar] [CrossRef]
- Vetcho, S.; Ullman, A.J.; Petsky, H.; Wiroonpanich, W.; Cooke, M. Parent and Interdisciplinary Professional Perceptions of Family-Centered Care in Thai NICU: A Qualitative Study. Nurs. Crit. Care 2021. [Google Scholar] [CrossRef]
- Asai, H. Predictors of Nurses’ Family-Centered Care Practises in the Neonatal Intensive Care Unit. Jpn. J. Nurs. Sci. 2011, 8, 57–65. [Google Scholar] [CrossRef]
- F.A. Davis Company. Wright & Leahey’s Nurses and Families: A Guide to Family Assessment and Intervention. Available online: https://www.fadavis.com/product/nursing-community-public-health-nurses-families-assessment-intervention-wright-leahey-6 (accessed on 18 February 2022).
- Savanh, P.; Aita, M.; Héon, M. A Review of Siblings’ Needs and Interventions Supporting Their Adaptation in the Neonatal Intensive Care Unit. Infants Young Child. 2020, 33, 332–351. [Google Scholar] [CrossRef]
- Larocque, C.; Peterson, W.E.; Squires, J.E.; Mason-Ward, M.; Mayhew, K.; Harrison, D. Family-Centred Care in the Neonatal Intensive Care Unit: A Concept Analysis and Literature Review. J. Neonatal Nurs. 2021, 27, 402–411. [Google Scholar] [CrossRef]
- Carter, B.S.; Willis, T.; Knackstedt, A. Neonatal Family-Centered Care in a Pandemic. J. Perinatol. 2021, 41, 1177–1179. [Google Scholar] [CrossRef]
- Giuseppe, D.B.; Giuseppina, N.; Desiree, S.; Angela, S.; Maurizio, G.; Perrone, S. Improving Care in Neonatal Intensive Units During the COVID-19 Pandemic: A Survey on Electronic Health Communication. J. Intensive Care Med. 2022, 37, 671–678. [Google Scholar] [CrossRef]
| Variables | Sample | Number | Percentage (%) |
|---|---|---|---|
| Sex (n = 921) | |||
| Female | 821 | (88.3) | |
| Male | 100 | (10.9) | |
| Staff (n = 890) | |||
| Fixed-term | 810 | (91.01) | |
| Temporary | 80 | (8.99) | |
| Health Professionals (n = 916) | |||
| Nurse | 546 | (59.61) | |
| Pediatric Nurse | 151 | (16.48) | |
| Medical Doctor | 176 | (19.21) | |
| Others | 26 | (2.84) | |
| HC Professional | 17 | (1.86) | |
| Job Position (n = 828) | |||
| Head/Coordinator | 46 | (5.56) | |
| Non coordinator | 782 | (94.44) | |
| Education (n = 870) | |||
| Regional Diploma | 212 | (24.5) | |
| Bachelor of Science | 330 | (37.9) | |
| Master of Science | 66 | (7.5) | |
| PhD or MD | 152 | (17.5) | |
| Other | 110 | (12.6) | |
| Clinical Setting (n = 914) | |||
| NICU | 48 | (5.25) | |
| Intermediate Care | 22 | (2.41) | |
| Both | 844 | (92.34) | |
| Family information (n = 906) | |||
| Staff with children | 565 | (62.36) | |
| Staff without children | 341 | (37.64) | |
| Age (n = 914) | |||
| >51 | 150 | (16.41) | |
| 41–50 | 333 | (36.43) | |
| 31–40 | 304 | (33.26) | |
| 20–30 | 127 | (13.89) | |
| Years of experiences (n = 437) | |||
| >10 | 162 | (37.1) | |
| ≤10 | 275 | (62.9) | |
| Subscales | Current | Necessary |
|---|---|---|
| The family as the constant of the child’s life | 0.66 | 0.65 |
| Collaboration between parents and health professionals | 0.76 | 0.70 |
| Recognize family individuality | 0.70 | 0.80 |
| Share complete information | 0.72 | 0.76 |
| Understand the developmental needs of the child | 0.65 | 0.75 |
| Encourage parent-to-parent support | 0.66 | 0.78 |
| Provide emotional and financial support | 0.57 | 0.61 |
| Assuring that the healthcare delivery system responds to family needs | 0.73 | 0.82 |
| Provide emotional support to staff | 0.74 | 0.85 |
| Total index | 0.91 | 0.92 |
| Sub-Scales for Current Domains | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. |
| 1. The family as the constant of the child’s life | 1 | ||||||||
| 2. Collaboration between parents and health professionals | 0.639 ** | 1 | |||||||
| 3. Recognize family individuality | 0.426 ** | 0.558 ** | 1 | ||||||
| 4. Share complete information | 0.434 ** | 0.553 ** | 0.739 ** | 1 | |||||
| 5. Understand the developmental needs of the child | 0.431 ** | 0.489 ** | 0.508 ** | 0.572 ** | 1 | ||||
| 6. Encourage parent-to-parent support | 0.477 ** | 0.575 ** | 0.598 ** | 0.622 ** | 0.590 ** | 1 | |||
| 7. Provide emotional and financial support | 0.394 ** | 0.459 ** | 0.559 ** | 0.591 ** | 0.545 ** | 0.614 ** | 1 | ||
| 8. Assuring that the healthcare delivery system responds to family needs | 0.396 ** | 0.514 ** | 0.477 ** | 0.518 ** | 0.526 ** | 0.599 ** | 0.539 ** | 1 | |
| 9. Provide emotional support to staff | 0.384 ** | 0.516 ** | 0.551 ** | 0.566 ** | 0.470 ** | 0.600 ** | 0.548 ** | 0.587 ** | 1 |
| Sub-Scales for Necessary Domains | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. |
| 1. The family as the constant of the child’s life | 1 | ||||||||
| 2. Collaboration between parents and health professionals | 0.623 ** | 1 | |||||||
| 3. Recognize family individuality | 0.450 ** | 0.605 ** | 1 | ||||||
| 4. Share complete information | 0.424 ** | 0.585 ** | 0.791 ** | 1 | |||||
| 5. Understand the developmental needs of the child | 0.464 ** | 0.565 ** | 0.648 ** | 0.658 ** | 1 | ||||
| 6. Encourage parent-to-parent support | 0.516 ** | 0.642 ** | 0.678 ** | 0.698 ** | 0.717 ** | 1 | |||
| 7. Provide emotional and financial support | 0.432 ** | 0.544 ** | 0.629 ** | 0.635 ** | 0.643 ** | 0.728 ** | 1 | ||
| 8. Assuring that the healthcare delivery system responds to family needs | 0.448 ** | 0.570 ** | 0.653 ** | 0.653 ** | 0.647 ** | 0.726 ** | 0.729 ** | 1 | |
| 9. Provide emotional support to staff | 0.422 ** | 0.542 ** | 0.659 ** | 0.683 ** | 0.631 ** | 0.701 ** | 0.698 ** | 0.778 ** | 1 |
| FCCQ-R@it-NICU | Current Mean (SD) | Necessary Mean (SD) | Gap Mean (SD) | p-Value |
|---|---|---|---|---|
| The family as the constant of the child’s life | 30.05 (0.84) | 30.90 (0.76) | 0.86 (0.87) | <0.01 |
| Collaboration between parents and health professionals | 2.79 (0.72) | 3.75 (0.67) | 0.97 (0.83) | <0.01 |
| Recognize family individuality | 3.39 (0.66) | 4.37 (0.51) | 0.98 (0.72) | <0.01 |
| Share complete information | 3.03 (0.72) | 4.10 (0.59) | 1.08 (0.83) | <0.01 |
| Understand the developmental needs of the child | 2.86 (0.82) | 4.09 (0.67) | 1.23 (0.93) | <0.01 |
| Encourage parent-to-parent support | 3.06 (0.70) | 4.03 (0.61) | 0.98 (0.79) | <0.01 |
| Provide emotional and financial support | 3.16 (0.70) | 4.08 (0.62) | 0.92 (0.76) | <0.01 |
| Assuring that the healthcare delivery system responds to family needs | 2.75 (0.67) | 4.05 (0.59) | 1.31 (0.85) | <0.01 |
| Provide emotional support to staff | 3.13 (0.70) | 4.26 (0.56) | 1.15 (0.83) | <0.01 |
| Total index | 3.02 (0.20) | 4.07 (0.18) | 1.05 (0.02) | <0.01 |
| Current Mean (SD) | p-Value | Necessary Mean (SD) | p-Value | Gap Mean (SD) | p-Value | |
|---|---|---|---|---|---|---|
| Sex | ||||||
| Female | 2.99 (0.01) | 0.34 | 4.08 (0.48) | 0.42 | 1.12 (0.84) | 0.07 |
| Male | 3.05 (0.45) | 4.04 (0.39) | 0.97 (0.64) | |||
| Age | ||||||
| 20–30 | 3.01 (0.52) | 0.30 | 4.13 (0.41) | 0.06 | 1.12 (0.83) | 0.07 |
| 31–40 | 2.99 (0.5) | 4.13 (0.51) | 1.19 (0.89) | |||
| 41–50 | 3.00 (0.53) | 4.06 (0.48) | 1.11 (0.82) | |||
| >51 | 3.04 (0.51) | 4.02 (0.46) | 0.97 (0.70) | |||
| Parental Status | ||||||
| With children | 2.99 (0.53) | 0.48 | 4.05 (0.48) | 0.01 * | 1.09 (0.85) | 0.37 |
| Without children | 3.01 (0.53) | 4.13 (0.45) | 1.14 (0.77) | |||
| Professions | ||||||
| Pediatric Nurse | 2.93 (0.55) | <0.01 ** | 4.07 (0.49) | 0.02 * | 1.22 (0.89) | <0.01 ** |
| General Nurse | 3.03 (0.47) | 4.01 (0.52) | 0.94 (0.75) | |||
| Physician | 3.13 (0.60) | 4.16 (0.41) | 0.97 (0.65) | |||
| Other Allied Healthcare Professionals | 3.31 (0.60) | 4.19 (0.45) | 0.69 (0.63) | |||
| Others | 3.22 (0.62) | 4.26 (0.39) | 1.12 (0.72) | |||
| Job Position | ||||||
| Head/Coordinator | 3.20 (0.45) | <0.01 ** | 4.27 (0.43) | <0.01 ** | 1.14 (0.64) | 0.89 |
| Non coordinator | 2.99 (0.53) | 4.08 (0.46) | 1.12 (0.80) | |||
| Education | ||||||
| Regional School | 2.95 (0.54) | <0.01 ** | 3.99 (0.52) | 0.002 ** | 1.06 (0.88) | <0.01 ** |
| BSc | 3.02 (0.53) | 4.11 (0.48) | 1.15 (0.84) | |||
| MSc | 2.91 (0.56) | 4.17 (0.40) | 1.27 (0.84) | |||
| PhD or MD | 3.17 (0.50) | 4.18 (0.44) | 1.05 (0.66) | |||
| Other | 2.90 (0.52) | 4.07 (0.45) | 1.26 (0.87) | |||
| Work Experience | ||||||
| Up to 10 years | 3.00 (0.56) | 0.92 | 4.13 (0.44) | <0.01 ** | 1.14 (0.86) | 0.39 |
| >10 years | 3.00 (0.50) | 4.04 (0.49) | 1.09 (0.80) | |||
| Hospital employed | ||||||
| Yes | 3.00 (0.53) | 0.99 | 4.08 (0.47) | 0.87 | 1.11 (0.82) | 0.62 |
| No | 3.00 (0.63) | 4.09 (0.54) | 1.06 (0.88) | |||
| Work Setting | ||||||
| NICU | 2.99 (0.55) | 0.39 | 4.05 (0.49) | 0.78 | 1.10 (0.89) | 0.62 |
| Intermediate Care | 3.16 (0.66) | 4.04 (0.42) | 0.95 (0.80) | |||
| Both | 3.00 (0.53) | 4.09 (0.48) | 1.12 (0.83) | |||
| Current | Necessary | Gap | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Coeff. | CI | p | Coeff. | CI | p | Coeff. | CI | p | |
| Sex | |||||||||
| Male [Ref] | |||||||||
| Female | - | - | - | - | - | - | 0.92 | −0.39–2.23 | 0.16 |
| Job Profession | |||||||||
| Nurse [Ref] | |||||||||
| Pediatric Nurse | 0.73 | −0.27–0.17 | 0.15 | −0.43 | −0.13–0.05 | 0.48 | −0.13 | −0.24–−0.23 | 0.02 |
| MD | 0.15 | −0.66–0.37 | 0.17 | −0.09 | −0.30–0.11 | 0.11 | −0.28 | −0.53–−0.37 | 0.03 |
| HC Professionals | 0.37 | 0.10–0.64 | 0.01 | 0-13 | −0.11–0.37 | 0.38 | −0.34 | −0.59–−0.11 | 0.04 |
| Others | 0.21 | −0.22–0.44 | 0.07 | 0.16 | −0.05–0.37 | 0.37 | −0.69 | −0.32–0.19 | 0.59 |
| Job Position | |||||||||
| Staff [Ref] | |||||||||
| Management | 0.20 | 0.38–0.36 | 0.015 | −0.01 | −0.89–0.08 | 0.90 | - | - | - |
| Education | |||||||||
| Other [Ref] | |||||||||
| PhD/MD | 0.15 | −0.88–0.40 | 0.21 | 0.19 | −0.03–0.42 | 0.08 | 0.10 | −0.17–0.37 | 0.46 |
| MSc | −0.01 | −0.20–0.18 | 0.92 | 0.09 | −0.07–0.27 | 0.26 | 0.16 | −0.40–0.36 | 0.12 |
| BSc | 0.18 | 0.59–0.30 | 0.01 | −0.01 | −0.13–0.09 | 0.79 | −0.13 | −0.27–0.01 | 0.05 |
| Regional Diploma | 0.98 | −0.03–0.22 | 0.12 | −0.84 | −0.20–0.03 | 0.14 | −0.12 | −0.26–0.19 | 0.09 |
| Age | |||||||||
| >51 [Ref] | |||||||||
| 20–30 | - | - | - | 0.11 | −0.51–0.27 | 0.18 | - | - | - |
| 31–40 | - | - | - | 0.12 | −0.01–0.23 | 0.05 | - | - | - |
| 41–50 | - | - | - | 0.05 | −0.46–0.15 | 0.29 | - | - | - |
| Work Experience | |||||||||
| Rif ≤ 10 | |||||||||
| >10 years | - | - | - | −0.01 | −0.90–0.79 | 0.79 | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dall’Oglio, I.; Mascolo, R.; Portanova, A.; Ragni, A.; Amadio, P.; Fiori, M.; Tofani, M.; Gawronski, O.; Piga, S.; Rocco, G.; et al. Staff Perceptions of Family-Centered Care in Italian Neonatal Intensive Care Units: A Multicenter Cross-Sectional Study. Children 2022, 9, 1401. https://doi.org/10.3390/children9091401
Dall’Oglio I, Mascolo R, Portanova A, Ragni A, Amadio P, Fiori M, Tofani M, Gawronski O, Piga S, Rocco G, et al. Staff Perceptions of Family-Centered Care in Italian Neonatal Intensive Care Units: A Multicenter Cross-Sectional Study. Children. 2022; 9(9):1401. https://doi.org/10.3390/children9091401
Chicago/Turabian StyleDall’Oglio, Immacolata, Rachele Mascolo, Anna Portanova, Angela Ragni, Patrizia Amadio, Martina Fiori, Marco Tofani, Orsola Gawronski, Simone Piga, Gennaro Rocco, and et al. 2022. "Staff Perceptions of Family-Centered Care in Italian Neonatal Intensive Care Units: A Multicenter Cross-Sectional Study" Children 9, no. 9: 1401. https://doi.org/10.3390/children9091401
APA StyleDall’Oglio, I., Mascolo, R., Portanova, A., Ragni, A., Amadio, P., Fiori, M., Tofani, M., Gawronski, O., Piga, S., Rocco, G., Tiozzo, E., Latour, J. M., & on behalf of the FCC Italian NICUs Study Group. (2022). Staff Perceptions of Family-Centered Care in Italian Neonatal Intensive Care Units: A Multicenter Cross-Sectional Study. Children, 9(9), 1401. https://doi.org/10.3390/children9091401






