Perceived Difficulties in Physical Tasks and Physical Fitness in Treatment- and Non-Treatment-Seeking Youths with Obesity
Abstract
:1. Introduction
2. Materials and Methods
2.1. Anthropometric Measurements
2.2. Questionnaires: Sports Participation and Sedentary Habits
2.3. Questionnaires: Perceived Difficulties
2.4. Physical Fitness Assessment
- (1)
- Six-minute walking test was performed indoors [15]. The walking course length was 20 m along a corridor marked every 2 m with brightly colored tape. Cones were placed at either end of the walking course to indicate the beginning and the end points. Each participant was tested individually. Participants were informed that the purpose of the test was to assess how far they could walk in 6 min and were instructed to walk the longest distance possible during the allowed time. Hopping, skipping, running and jumping were not allowed during the test. Only the standardized phrases for encouragement (e.g., “keep going”, “you are doing well”) and announcement of time remaining were given. The six-minute walking distance (SMWD) was expressed in meters.
- (2)
- Long jump (LJ) was used to assess lower body muscle strength [16]. Participants performed a two-foot take-off and landing. The swinging of the arms and flexing of the knees were permitted to provide forward drive. Participants attempted to jump as far as possible, landing on both feet without falling backward. Length was measured to the nearest point of contact on the landing. Two attempts were performed and the best value was used for analysis. Results were expressed in centimeters.
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Garrido-Miguel, M.; Cavero-Redondo, I.; Álvarez-Bueno, C.; Rodríguez-Artalejo, F.; Moreno, L.A.; Ruiz, J.R.; Ahrens, W.; Martínez-Vizcaíno, V. Prevalence and Trends of Overweight and Obesity in European Children From 1999 to 2016: A Systematic Review and Meta-analysis. JAMA Pediatr. 2019, 173, e192430. [Google Scholar] [CrossRef] [PubMed]
- Spinelli, A.; Buoncristiano, M.; Kovacs, V.A.; Yngve, A.; Spiroski, I.; Obreja, G.; Starc, G.; Pérez, N.; Rito, A.I.; Kunešová, M.; et al. Prevalence of Severe Obesity among Primary School Children in 21 European Countries. Obes. Facts 2019, 12, 244–258. [Google Scholar] [CrossRef]
- Weihrauch-Blüher, S.; Schwarz, P.; Klusmann, J.-H. Childhood obesity: Increased risk for cardiometabolic disease and cancer in adulthood. Metabolism 2018, 92, 147–152. [Google Scholar] [CrossRef]
- Tsiros, M.D.; Tian, E.; Shultz, S.P.; Olds, T.; Hills, A.P.; Duff, J.; Kumar, S. Obesity, the new childhood disability? An umbrella review on the association between adiposity and physical function. Obes. Rev. 2020, 21, e13121. [Google Scholar] [CrossRef] [PubMed]
- Fontaine, K.R.; Barofsky, I. Obesity and health-related quality of life. Obes. Rev. 2001, 2, 173–182. [Google Scholar] [CrossRef]
- Hayes, M.; Baxter, H.; Müller-Nordhorn, J.; Hohls, J.K.; Muckelbauer, R. The longitudinal association between weight change and health-related quality of life in adults and children: A systematic review. Obes. Rev. 2017, 18, 1398–1411. [Google Scholar] [CrossRef] [PubMed]
- Mozzillo, E.; Zito, E.; Calcaterra, V.; Corciulo, N.; Di Pietro, M.; Di Sessa, A.; Franceschi, R.; Licenziati, M.R.; Maltoni, G.; Morino, G.; et al. Poor Health Related Quality of Life and Unhealthy Lifestyle Habits in Weight-Loss Treatment-Seeking Youth. Int. J. Environ. Res. Public Health 2021, 18, 9355. [Google Scholar] [CrossRef]
- Williams, J.; Wake, M.; Hesketh, K.; Maher, E.; Waters, E. Health-related quality of life of overweight and obese children. JAMA 2005, 293, 70–76. [Google Scholar] [CrossRef]
- García-Hermoso, A.; Izquierdo, M.; Alonso-Martínez, A.M.; Faigenbaum, A.; Olloquequi, J.; Ramírez-Vélez, R. Association between Exercise-Induced Changes in Cardiorespiratory Fitness and Adiposity among Overweight and Obese Youth: A Meta-Analysis and Meta-Regression Analysis. Children 2020, 7, 147. [Google Scholar] [CrossRef]
- Harder-Lauridsen, N.M.; Birk, N.M.; Ried-Larsen, M.; Juul, A.; Andersen, L.B.; Pedersen, B.K.; Krogh-Madsen, R. A randomized controlled trial on a multicomponent intervention for overweight school-aged children—Copenhagen, Denmark. BMC Pediatrics 2014, 14, 273. [Google Scholar] [CrossRef] [Green Version]
- Ørntoft, C.; Fuller, C.W.; Larsen, M.N.; Bangsbo, J.; Dvorak, J.; Krustrup, P. ‘FIFA 11 for Health’ for Europe. II: Effect on health markers and physical fitness in Danish schoolchildren aged 10–12 years. Br. J. Sports Med. 2016, 50, 1394–1399. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Mapping the Health System Response to Childhood Obesity in the WHO European Region 2019. Available online: https://www.euro.who.int/__data/assets/pdf_file/0019/401176/Childhood-obesity-web.pdf (accessed on 18 May 2022).
- de Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Fallon, E.M.; Tanofsky-Kraff, M.; Norman, A.-C.; McDuffie, J.R.; Taylor, E.D.; Cohen, M.L.; Young-Hyman, D.; Keil, M.; Kolotkin, R.L.; Yanovski, J.A. Health-related quality of life in overweight and nonoverweight black and white adolescents. J. Pediatr. 2005, 147, 443–450. [Google Scholar] [CrossRef] [PubMed]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit Care Med. 2002, 166, 111–117. [Google Scholar] [CrossRef]
- Marques, A.; Henriques-Neto, D.; Peralta, M.; Martins, J.; Gomes, F.; Popovic, S.; Masanovic, B.; Demetriou, Y.; Schlund, A.; Ihle, A. Field-Based Health-Related Physical Fitness Tests in Children and Adolescents: A Systematic Review. Front. Pediatr. 2021, 9, 640028. [Google Scholar] [CrossRef]
- Carson, V.; Tremblay, M.S.; Chaput, J.-P.; Chastin, S.F. Associations between sleep duration, sedentary time, physical activity, and health indicators among Canadian children and youth using compositional analyses. Appl. Physiol. Nutr. Metab. 2016, 41 (Suppl. S3), S294–S302. [Google Scholar] [CrossRef]
- Valerio, G.; Gallarato, V.; D’Amico, O.; Sticco, M.; Tortorelli, P.; Zito, E.; Nugnes, R.; Mozzillo, E.; Franzese, A. Perceived Difficulty with Physical Tasks, Lifestyle, and Physical Performance in Obese Children. BioMed Res. Int. 2014, 2014, 1–7. [Google Scholar] [CrossRef]
- Swallen, K.C.; Reither, E.N.; Haas, S.A.; Meier, A.M. Overweight, Obesity, and Health-Related Quality of Life Among Adolescents: The National Longitudinal Study of Adolescent Health. Pediatrics 2005, 115, 340–347. [Google Scholar] [CrossRef]
- Morano, M.; Colella, D.; Robazza, C.; Bortoli, L.; Capranica, L. Physical self-perception and motor performance in normal-weight, overweight and obese children. Scand. J. Med. Sci. Sports 2010, 21, 465–473. [Google Scholar] [CrossRef]
- Fiori, F.; Bravo, G.; Parpinel, M.; Messina, G.; Malavolta, R.; Lazzer, S. A 3-year school-based intervention improved physical fitness and reduced the prevalence of overweight and obesity in Italian prepubertal children. J. Sports Med. Phys. Fit. 2021, 61, 1682–1689. [Google Scholar] [CrossRef] [PubMed]
- Varni, J.W.; Seid, M.; Rode, C.A. The PedsQL™: Measurement Model for the Pediatric Quality of Life Inventory. Med. Care 1999, 37, 126–139. [Google Scholar] [CrossRef] [PubMed]
- Wille, N.; Bullinger, M.; Holl, R.; Hoffmeister, U.; Mann, R.; Goldapp, C.; Reinehr, T.; Westenhöfer, J.; Egmond-Froehlich, A.; Ravens-Sieberer, U. Health-related quality of life in overweight and obese youths: Results of a multicenter study. Health Qual. Life Outcomes 2010, 8, 36. [Google Scholar] [CrossRef] [PubMed]
- de Izaskun, L.C.; Saioa, U.G.; de Gurutze, L.C.; Silvia, A.G. Perception of Competence as Mediator between Motor Competence and Physical Activity. Int. J. Environ. Res. Public Health 2022, 19, 392. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-Efficacy: The Exercise of Control; W H Freeman/Times Books/Henry Holt & Co.: New York, NY, USA, 1997. [Google Scholar]
- McAuley, E.; Szabo, A.; Gothe, N.; Olson, E.A. Self-Efficacy: Implications for Physical Activity, Function, and Functional Limitations in Older Adults. Am. J. Lifestyle Med. 2011, 5, 361–369. [Google Scholar] [CrossRef] [PubMed]
- Häcker, A.-L.; Bigras, J.-L.; Henderson, M.; Barnett, T.A.; Mathieu, M.-E. Motor Skills of Children and Adolescents With Obesity and Severe Obesity—A CIRCUIT Study. J. Strength Cond. Res. 2020, 34, 3577–3586. [Google Scholar] [CrossRef] [PubMed]
- Morinder, G.; Mattsson, E.; Sollander, C.; Marcus, C.; Larsson, U.E. Six-minute walk test in obese children and adolescents: Reproducibility and validity. Physiother. Res. Int. 2009, 14, 91–104. [Google Scholar] [CrossRef]
- Vandoni, M.; Calcaterra, V.; Pellino, V.C.; De Silvestri, A.; Marin, L.; Zuccotti, G.V.; Tranfaglia, V.; Giuriato, M.; Codella, R.; Lovecchio, N. “Fitness and Fatness” in Children and Adolescents: An Italian Cross-Sectional Study. Children 2021, 8, 762. [Google Scholar] [CrossRef]
- Dong, X.; Ding, L.; Zhang, R.; Ding, M.; Wang, B.; Yi, X. Physical Activity, Screen-Based Sedentary Behavior and Physical Fitness in Chinese Adolescents: A Cross-Sectional Study. Front. Pediatr. 2021, 9, 722079. [Google Scholar] [CrossRef]
- Thivel, D.; Ring-Dimitriou, S.; Weghuber, D.; Frelut, M.-L.; O’Malley, G. Muscle Strength and Fitness in Pediatric Obesity: A Systematic Review from the European Childhood Obesity Group. Obes. Facts 2016, 9, 52–63. [Google Scholar] [CrossRef]
- Moliner-Urdiales, D.; Ruiz, J.R.; Vicente-Rodriguez, G.; Rey-Lopez, J.P.; España-Romero, V.; Casajús, J.A.; Molnar, D.; Widhalm, K.; Dallongeville, J.; González-Gross, M.; et al. Associations of muscular and cardiorespiratory fitness with total and central body fat in adolescents: The HELENA study. Br. J. Sports Med. 2011, 45, 101–108. [Google Scholar] [CrossRef] [Green Version]

| School (n = 82) | Hospital (n = 269) | p | |
|---|---|---|---|
| Boys N (%) | 50 (61.0) | 148 (55.0) | |
| Age (years) | 10.4 | 10.6 | 0.317 |
| Weight (kg) | 56.3 | 63.2 | <0.001 |
| Stature (cm) | 146.0 | 146.0 | 0.981 |
| BMI Z-score | 2.8 | 3.3 | <0.001 |
| Sports participation N (%) | 37 (45) | (121) 45 | 0.982 |
| Sedentary time (h/day) | 3.2 | 4.5 | <0.001 |
| Six-minute walking distance (m) | 568 | 456 | <0.001 |
| Long jump distance (cm) | 103.4 | 89.1 | <0.001 |
| Perceived difficulties | |||
| Walking N (%) | 10 (12) | 156 (58) | <0.001 |
| Running N (%) | 23 (28) | 210 (78) | <0.001 |
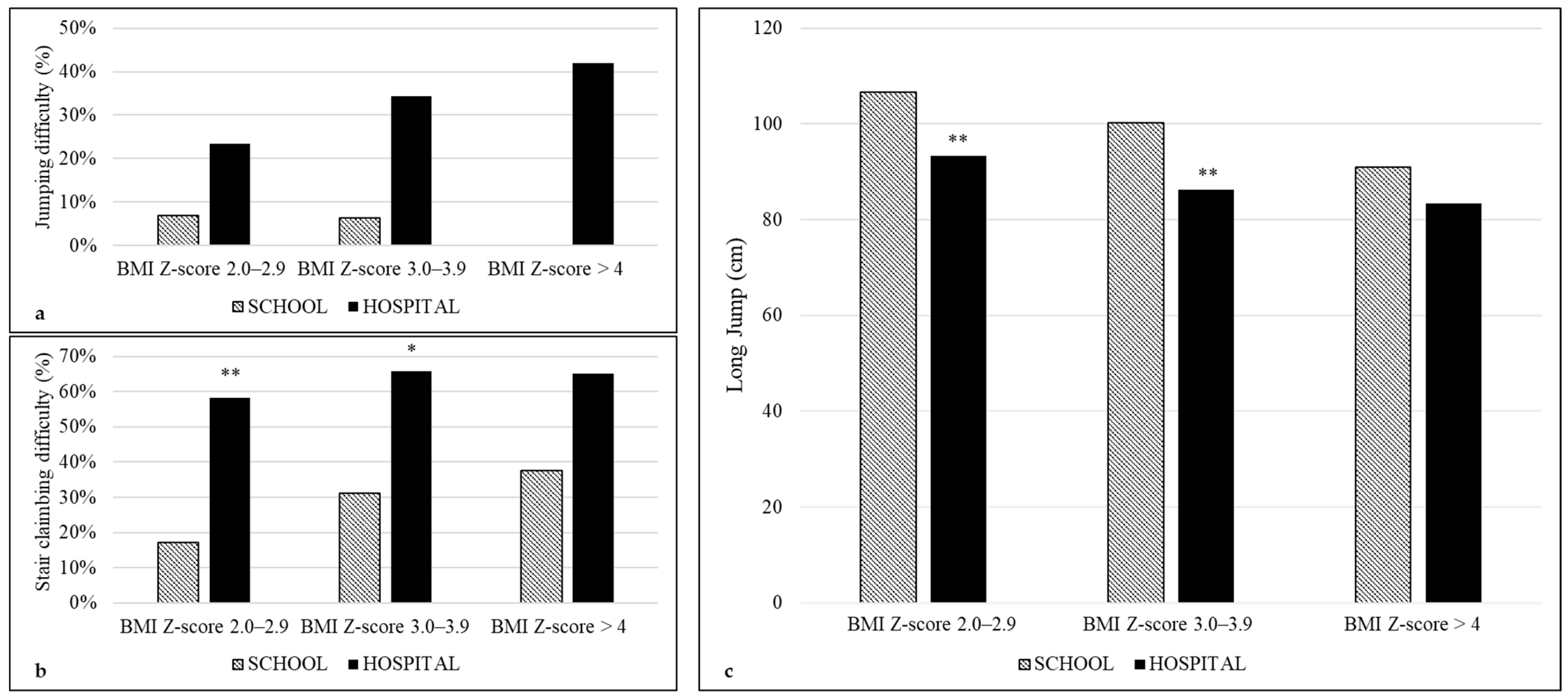
| Jumping N (%) | 5 (6) | 81 (30) | <0.001 |
| Stair climbing N (%) | 18 (22) | 167 (62) | <0.001 |
| BMI Z-score categories | |||
| 2.0–2.9 N (%) | 58 (70.7) | 124 (46.1) | <0.001 |
| 3.0–3.9 N (%) | 16 (19.5) | 102 (37.9) | |
| 4.0–4.9 N (%) | 8 (9.8) | 43 (16.0) |
| Perceived Difficulty | Variables (p in Brackets) | OR | 95% C.I. | |
|---|---|---|---|---|
| Walking | Setting * (<0.001) | 7.846 | 3.779 | 16.289 |
| Sedentary time * (0.010) | 1.171 | 1.039 | 1.320 | |
| Running | Setting * (<0.001) | 6.197 | 3.400 | 11.292 |
| BMI Z-score * (0.015) | 1.633 | 1.100 | 2.427 | |
| Sedentary time * (0.001) | 1.274 | 1.100 | 1.475 | |
| Sex * (0.049) | 1.763 | 1.023 | 3.143 | |
| Jumping | Setting * (<0.001) | 5.688 | 2.158 | 14.996 |
| BMI Z-score * (0.006) | 1.578 | 1.133 | 2.196 | |
| Stair Climbing | Setting * (<0.001) | 4.627 | 2.523 | 8.486 |
| Significant Predictors (Standardized Coefficients in Brackets) | R2 | SEE | |
|---|---|---|---|
| Six-minute walking distance | Setting * (−0.642), age * (0.208), sedentary habits * (−0.132), sex * (0.088) | 0.496 | 50.207 |
| Long jump distance | Setting * (−0.252), sex * (0.279), BMI Z-score * (−0.200), age * (0.137), sports participation * (0.117) | 0.243 | 17.776 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ballarin, G.; Licenziati, M.R.; Di Vincenzo, O.; Scalfi, L.; Valerio, G. Perceived Difficulties in Physical Tasks and Physical Fitness in Treatment- and Non-Treatment-Seeking Youths with Obesity. Children 2022, 9, 1351. https://doi.org/10.3390/children9091351
Ballarin G, Licenziati MR, Di Vincenzo O, Scalfi L, Valerio G. Perceived Difficulties in Physical Tasks and Physical Fitness in Treatment- and Non-Treatment-Seeking Youths with Obesity. Children. 2022; 9(9):1351. https://doi.org/10.3390/children9091351
Chicago/Turabian StyleBallarin, Giada, Maria Rosaria Licenziati, Olivia Di Vincenzo, Luca Scalfi, and Giuliana Valerio. 2022. "Perceived Difficulties in Physical Tasks and Physical Fitness in Treatment- and Non-Treatment-Seeking Youths with Obesity" Children 9, no. 9: 1351. https://doi.org/10.3390/children9091351
APA StyleBallarin, G., Licenziati, M. R., Di Vincenzo, O., Scalfi, L., & Valerio, G. (2022). Perceived Difficulties in Physical Tasks and Physical Fitness in Treatment- and Non-Treatment-Seeking Youths with Obesity. Children, 9(9), 1351. https://doi.org/10.3390/children9091351







