School-Based Exercise Programs for Promoting Cardiorespiratory Fitness in Overweight and Obese Children Aged 6 to 10
Abstract
:1. Introduction
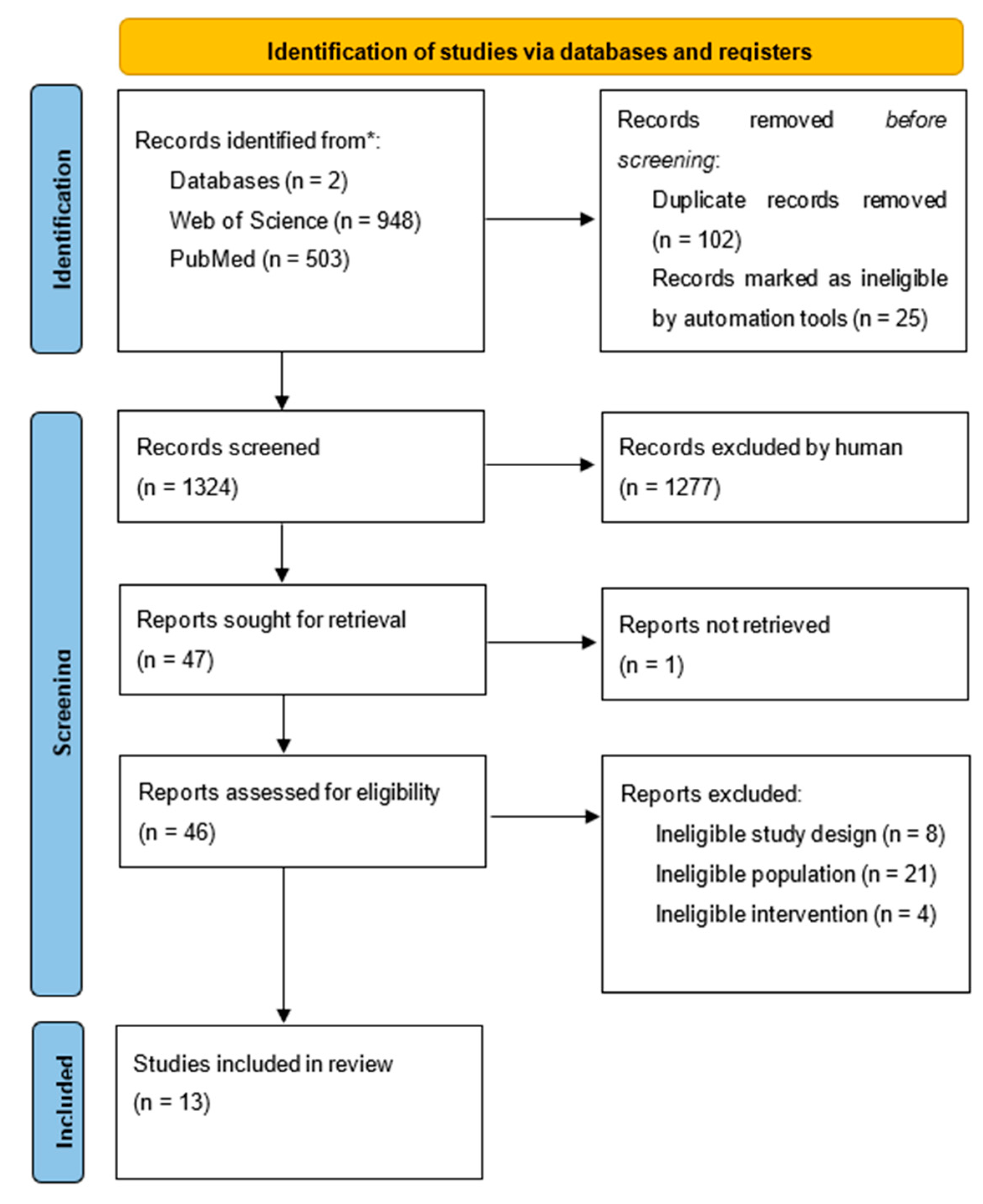
2. Materials and Methods
2.1. Literature Identification
2.2. Inclusion Criteria
2.3. Risk of Bias Assessment
3. Results
3.1. Quality of the Studies
3.2. Selection and Characteristics of Studies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Veijalainen, A.; Tompuri, T.; Haapala, E.A.; Viitasalo, A.; Lintu, N.; Väistö, J.; Laitinen, T.; Lindi, V.; Lakka, T.A. Associations of cardiorespiratory fitness, physical activity, and adiposity with arterial stiffness in children. Scand. J. Med. Sci. Sport 2016, 26, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.-c.; Artero, E.G.; Sui, X.; Blair, S.N. Mortality trends in the general population: The importance of cardiorespiratory fitness. J. Psychopharmacol. 2010, 24, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Ortega, F.B.; Ruiz, J.R.; Castillo, M.J.; Moreno, L.A.; Urzanqui, A.; González-Gross, M.; Sjöström, M.; Gutiérrez, A. Health-related physical fitness according to chronological and biological age in adolescents. The AVENA study. J. Sports Med. Phys. Fit. 2008, 48, 371–379. [Google Scholar]
- Ruiz, J.R.; Castro-Piñero, J.; Artero, E.G.; Ortega, F.B.; Sjöström, M.; Suni, J.; Castillo, M.J. Predictive validity of health-related fitness in youth: A systematic review. Br. J. Sports Med. 2009, 43, 909–923. [Google Scholar] [CrossRef]
- Ruiz, J.R.; Cavero-Redondo, I.; Ortega, F.B.; Welk, G.J.; Andersen, L.B.; Martinez-Vizcaino, V. Cardiorespiratory fitness cut points to avoid cardiovascular disease risk in children and adolescents; what level of fitness should raise a red flag? A systematic review and meta-analysis. Br. J. Sports Med. 2016, 50, 1451–1458. [Google Scholar] [CrossRef]
- Sui, X.; LaMonte, M.J.; Laditka, J.N.; Hardin, J.W.; Chase, N.; Hooker, S.P.; Blair, S.N. Cardiorespiratory fitness and adiposity as mortality predictors in older adults. JAMA 2007, 298, 2507–2516. [Google Scholar] [CrossRef]
- Rodrigues, A.N.; Perez, A.J.; Carletti, L.; Bissoli, N.S.; Abreu, G.R. The association between cardiorespiratory fitness and cardiovascular risk in adolescents. J. Pediatr. 2007, 83, 429–435. [Google Scholar] [CrossRef]
- Cao, C.; Yang, L.; Cade, W.T.; Racette, S.B.; Park, Y.; Cao, Y.; Friedenreich, C.M.; Hamer, M.; Stamatakis, E.; Smith, L. Cardiorespiratory Fitness Is Associated with Early Death among Healthy Young and Middle-Aged Baby Boomers and Generation Xers. Am. J. Med. 2020, 133, 961–968.e3. [Google Scholar] [CrossRef]
- Setty, P.; Padmanabha, B.V.; Doddamani, B.R. Correlation between obesity and cardio respiratory fitness. Int. J. Med. Sci. Public Health 2013, 2, 300–304. [Google Scholar] [CrossRef]
- Jastreboff, A.M.; Kotz, C.M.; Kelly, A.S.; Heymsfield, S.B. Obesity as a disease: The obesity society 2018 position statement. Obesity 2019, 27, 7–9. [Google Scholar] [CrossRef]
- Saha, A.K.; Sarkar, N.; Chatterjee, T. Health consequences of childhood obesity. Indian J. Pediatrics 2011, 78, 1349–1355. [Google Scholar] [CrossRef] [PubMed]
- Katzmarzyk, P.T.; Lear, S.A. Physical activity for obese individuals: A systematic review of effects on chronic disease risk factors. Obes. Rev. 2012, 13, 95–105. [Google Scholar] [CrossRef] [PubMed]
- Vasconcellos, F.; Seabra, A.; Katzmarzyk, P.T.; Kraemer-Aguiar, L.G.; Bouskela, E.; Farinatti, P. Physical activity in overweight and obese adolescents: Systematic review of the effects on physical fitness components and cardiovascular risk factors. Sports Med. 2014, 44, 1139–1152. [Google Scholar] [CrossRef]
- Góis Leandro, C.; Arnaut Brinco, R.; Góes Nobre, G.; Góes Nobre, I.; Silva-Santiago, L.C.; Aires-Dos-Santos, B.R.; Marinho-Dos-Santos, R.; Rodrigues-Ribeiro, M.; Marinho-Barros, M.R.; Alves-Macedo, F.; et al. Post-exercise hypotension effects in response to plyometric training of 7- to 9-year-old boys with overweight/obesity: A randomized controlled study. J. Sports Med. Phys. Fit. 2021, 61, 1281–1289. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Vizcaíno, V.; Soriano-Cano, A.; Garrido-Miguel, M.; Cavero-Redondo, I.; de Medio, E.P.; Madrid, V.M.; Martínez-Hortelano, J.A.; Berlanga-Macías, C.; Sánchez-López, M. The effectiveness of a high-intensity interval games intervention in schoolchildren: A cluster-randomized trial. Scand. J. Med. Sci. Sports 2022, 32, 765–781. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.L.; Litwin, S.E.; Pollock, N.K.; Waller, J.L.; Zhu, H.D.; Dong, Y.B.; Kapuku, G.; Bhagatwala, J.; Harris, R.A.; Looney, J.; et al. Exercise effects on arterial stiffness and heart health in children with excess weight: The SMART RCT. Int. J. Obes. 2020, 44, 1152–1163. [Google Scholar] [CrossRef] [PubMed]
- Van Leeuwen, J.; Andrinopoulou, E.R.; Hamoen, M.; Paulis, W.D.; Van Teeffelen, J.; Kornelisse, K.; Van Der Wijst-Ligthart, K.; Koes, B.W.; Van Middelkoop, M. The effect of a multidisciplinary intervention program for overweight and obese children on cardiorespiratory fitness and blood pressure. Fam. Pract. 2018, 36, 147–153. [Google Scholar] [CrossRef]
- Jankowski, M.; Niedzielska, A.; Brzezinski, M.; Drabik, J. Cardiorespiratory fitness in children: A simple screening test for population studies. Pediatr. Cardiol. 2015, 36, 27–32. [Google Scholar] [CrossRef]
- Martínez, S.R.; Ríos, L.J.C.; Tamayo, I.M.; Almeida, L.G.; López-Gomez, M.A.; Jara, C.C. An After-School, high-intensity, interval physical activity programme improves health-related fitness in children. Motriz Rev. Educ. Fis. 2016, 22, 359–367. [Google Scholar] [CrossRef]
- Meng, C.; Yucheng, T.; Shu, L.; Yu, Z. Effects of school-based high-intensity interval training on body composition, cardiorespiratory fitness and cardiometabolic markers in adolescent boys with obesity: A randomized controlled trial. BMC Pediatr. 2022, 22, 112. [Google Scholar] [CrossRef]
- Larsen, M.N.; Nielsen, C.M.; Helge, E.W.; Madsen, M.; Manniche, V.; Hansen, L.; Hansen, P.R.; Bangsbo, J.; Krustrup, P. Positive effects on bone mineralisation and muscular fitness after 10 months of intense school-based physical training for children aged 8-10 years: The FIT FIRST randomised controlled trial. Br. J. Sports Med. 2018, 52, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Ye, S.; Pope, Z.C.; Lee, J.E.; Gao, Z. Effects of school-based exergaming on urban children’s physical activity and cardiorespiratory fitness: A quasi-experimental study. Int. J. Environ. Res. Public Health 2019, 16, 4080. [Google Scholar] [CrossRef] [PubMed]
- Castro-Piñero, J.; Perez-Bey, A.; Segura-Jiménez, V.; Aparicio, V.A.; Gómez-Martínez, S.; Izquierdo-Gomez, R.; Marcos, A.; Ruiz, J.R.; Veiga, O.L.; Bandres, F.; et al. Cardiorespiratory Fitness Cutoff Points for Early Detection of Present and Future Cardiovascular Risk in Children: A 2-Year Follow-up Study. Mayo Clin. Proc. 2017, 92, 1753–1762. [Google Scholar] [CrossRef] [PubMed]
- Braaksma, P.; Stuive, I.; Garst, R.; Wesselink, C.F.; van der Sluis, C.K.; Dekker, R.; Schoemaker, M.M. Characteristics of physical activity interventions and effects on cardiorespiratory fitness in children aged 6–12 years-A systematic review. J. Sci. Med. Sport 2018, 21, 296–306. [Google Scholar] [CrossRef] [PubMed]
- Engel, F.A.; Wagner, M.O.; Schelhorn, F.; Deubert, F.; Leutzsch, S.; Stolz, A.; Sperlich, B. Classroom-Based Micro-Sessions of Functional High-Intensity Circuit Training Enhances Functional Strength but Not Cardiorespiratory Fitness in School Children—A Feasibility Study. Front. Public Health 2019, 7, 291. [Google Scholar] [CrossRef] [PubMed]
- Bauer, N.; Sperlich, B.; Holmberg, H.C.; Engel, F.A. Effects of High-Intensity Interval Training in School on the Physical Performance and Health of Children and Adolescents: A Systematic Review with Meta-Analysis. Sport Med. Open 2022, 8, 50. [Google Scholar] [CrossRef]
- Stanly, S.L.; Maniazhagu, D. Individual and combined interventions of tai chi, pilates and yogic practices on cardio respiratory endurance of b.ed. trainees. Int. J. Phys. Educ. Sport Manag. Yogic Sci. 2020, 10, 25–31. [Google Scholar] [CrossRef]
- Kodama, S.; Saito, K.; Tanaka, S.; Maki, M.; Yachi, Y.; Asumi, M.; Sugawara, A.; Totsuka, K.; Shimano, H.; Ohashi, Y.; et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis. JAMA 2009, 301, 2024–2035. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef]
- Thivel, D.; Isacco, L.; Lazaar, N.; Aucouturier, J.; Ratel, S.; Doré, E.; Meyer, M.; Duché, P. Effect of a 6-month school-based physical activity program on body composition and physical fitness in lean and obese schoolchildren. Eur. J. Pediatr. 2011, 170, 1435–1443. [Google Scholar] [CrossRef]
- Resaland, G.K.; Andersen, L.B.; Mamen, A.; Anderssen, S.A. Effects of a 2-year school-based daily physical activity intervention on cardiorespiratory fitness: The Sogndal school-intervention study. Scand. J. Med. Sci. Sport 2011, 21, 302–309. [Google Scholar] [CrossRef] [PubMed]
- Yin, Z.; Moore, J.B.; Johnson, M.H.; Vernon, M.M.; Gutin, B. The impact of a 3-year after-school obesity prevention program in elementary school children. Child. Obes. 2012, 8, 60–70. [Google Scholar] [CrossRef] [PubMed]
- Krustrup, P.; Hansen, P.R.; Nielsen, C.M.; Larsen, M.N.; Randers, M.B.; Manniche, V.; Hansen, L.; Dvorak, J.; Bangsbo, J. Structural and functional cardiac adaptations to a 10-week school-based football intervention for 9-10-year-old children. Scand. J. Med. Sci. Sport 2014, 24, 4–9. [Google Scholar] [CrossRef] [PubMed]
- Khan, N.A.; Raine, L.B.; Drollette, E.S.; Scudder, M.R.; Pontifex, M.B.; Castelli, D.M.; Donovan, S.M.; Evans, E.M.; Hillman, C.H. Impact of the fitkids physical activity intervention on adiposity in prepubertal children. Pediatrics 2014, 133, e875–e883. [Google Scholar] [CrossRef]
- Tan, S.; Wang, J.; Cao, L. Exercise training at the intensity of maximal fat oxidation in obese boys. Appl. Physiol. Nutr. Metab. 2015, 41, 49–54. [Google Scholar] [CrossRef]
- Espinoza-Silva, M.; Latorre-Román, P.; Párraga-Montilla, J.; Caamaño-Navarrete, F.; Jerez-Mayorga, D.; Delgado-Floody, P. Response of obese schoolchildren to high-intensity interval training applied in the school context. Endocrinol. Diabetes Nutr. 2019, 66, 611–619. [Google Scholar] [CrossRef]
- Al-Mallah, M.H.; Sakr, S.; Al-Qunaibet, A. Cardiorespiratory Fitness and Cardiovascular Disease Prevention: An Update. Curr. Atheroscler. Rep. 2018, 20, 1. [Google Scholar] [CrossRef]
- Ferguson, B. ACSM’s Guidelines for Exercise Testing and Prescription 9th Ed. 2014. J. Can. Chiropr. Assoc. 2014, 58, 328. [Google Scholar]
- Burgomaster, K.A.; Heigenhauser, G.J.F.; Gibala, M.J. Effect of short-term sprint interval training on human skeletal muscle carbohydrate metabolism during exercise and time-trial performance. J. Appl. Physiol. 2006, 100, 2041–2047. [Google Scholar] [CrossRef]
- Gibala, M.J.; Little, J.P.; Macdonald, M.J.; Hawley, J.A. Physiological adaptations to low-volume, high-intensity interval training in health and disease. J. Physiol. 2012, 590, 1077–1084. [Google Scholar] [CrossRef] [PubMed]
- Whyte, L.J.; Gill, J.M.R.; Cathcart, A.J. Effect of 2 weeks of sprint interval training on health-related outcomes in sedentary overweight/obese men. Metabolism 2010, 59, 1421–1428. [Google Scholar] [CrossRef] [PubMed]
- Bogataj, Š.; Trajković, N.; Cadenas-Sanchez, C.; Sember, V. Effects of School-Based Exercise and Nutrition Intervention on Body Composition and Physical Fitness in Overweight Adolescent Girls. Nutrients 2021, 13, 238. [Google Scholar] [CrossRef] [PubMed]
- Eather, N.; Riley, N.; Miller, A.; Smith, V.; Poole, A.; Vincze, L.; Morgan, P.J.; Lubans, D.R. Efficacy and feasibility of HIIT training for university students: The Uni-HIIT RCT. J. Sci. Med. Sport 2019, 22, 596–601. [Google Scholar] [CrossRef]
- Berge, J.; Hjelmesæth, J.; Hertel, J.K.; Gjevestad, E.; Småstuen, M.C.; Johnson, L.K.; Martins, C.; Andersen, E.; Helgerud, J.; Støren, Ø. Effect of Aerobic Exercise Intensity on Energy Expenditure and Weight Loss in Severe Obesity-A Randomized Controlled Trial. Obesity 2021, 29, 359–369. [Google Scholar] [CrossRef]
- Jiménez-García, J.D.; Hita-Contreras, F.; de la Torre-Cruz, M.J.; Aibar-Almazán, A.; Achalandabaso-Ochoa, A.; Fábrega-Cuadros, R.; Martínez-Amat, A. Effects of HIIT and MIIT Suspension Training Programs on Sleep Quality and Fatigue in Older Adults: Randomized Controlled Clinical Trial. Int. J. Environ. Res. Public Health 2021, 18, 1211. [Google Scholar] [CrossRef]
- Jiménez-García, J.D.; Martínez-Amat, A.; De La Torre-Cruz, M.J.; Fábrega-Cuadros, R.; Cruz-Díaz, D.; Aibar-Almazán, A.; Achalandabaso-Ochoa, A.; Hita-Contreras, F. Suspension Training HIIT Improves Gait Speed, Strength and Quality of Life in Older Adults. Int. J. Sports Med. 2019, 40, 116–124. [Google Scholar] [CrossRef]
| Search 1 | Search 2 | Search 3 | Filters |
|---|---|---|---|
| school-based school program Intervention preschool primary school elementary school | cardio-respiratory fitness CRF cardio fitness VO2max maximal oxygen consumption heart rate | overweight obese | child: 6–12 years |
| Criterion | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | ∑ |
| Thivel et al. (2011) [31] | Y | Y | Y | Y | N | N | N | Y | Y | Y | Y | 7 |
| Resaland et al. (2011) [32] | Y | N | N | Y | N | N | N | N | Y | Y | Y | 4 |
| Yin et al. (2012) [33] | Y | Y | Y | Y | N | N | N | N | Y | Y | Y | 6 |
| Krustrup et al. (2014) [34] | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 |
| Khan et al. (2014) [35] | Y | Y | Y | Y | Y | N | N | Y | Y | Y | Y | 8 |
| Tan et al. (2015) [36] | Y | Y | Y | Y | N | N | N | Y | Y | Y | Y | 7 |
| Martinez et al. (2016) [19] | Y | Y | Y | Y | N | N | N | Y | Y | Y | Y | 7 |
| Leeuwen et al. (2018) [17] | Y | N | N | N | N | N | N | Y | Y | N | Y | 3 |
| Ye et al. (2019) [22] | Y | Y | Y | N | N | N | N | Y | N | Y | Y | 5 |
| Davis et al. (2019) [16] | Y | Y | Y | Y | Y | N | N | Y | Y | Y | Y | 8 |
| Espinoza-Silva et al. (2019) [37] | Y | N | N | Y | N | N | N | Y | Y | Y | Y | 5 |
| Leandro et al. (2021) [14] | Y | Y | Y | Y | N | N | N | Y | Y | Y | Y | 7 |
| Martinez-Viscaiano et al. (2022) [15] | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | 9 |
| First Author and Year of Publication | Sample of Participants | PF | Type of Intervention | Duration of Intervention | Results | |
|---|---|---|---|---|---|---|
| Number | Age | Weeks | ||||
| Thivel et al. (2011) [31] | N—457 | 6–10 | SRT, CPP, RHR, HRR | AL, 2/week (60 min) | 26 | HRR↑ RHR↑ (E&C) |
| Resaland et al. (2011) [32] | N—256 M—125 F—131 | 9–10 | TRE, VO2peak, HRpeak | Daily, MVPA (60 min) | 104 | VO2peak↑ (E) |
| Yin et al. (2012) [33] | N—574 | 8.7 ± 0.5 | ST, HR | Daily, Kids4Fit (120 min) | 156 | HR↑ (E&C) |
| Krustrup et al. (2014) [34] | N—51 M—21 F—30 | 9–10 | CTE, IVRTglobal, LVSEF, LVPWD, RHR, RBP, HR, HRmax | SSF, 3x/week (40 min) | 10 | LVSEF↑ IVRTglobal↑(E) |
| Khan et al. (2014) [35] | N—220 M—117 F—103 | 8–9 | TRE, HR, VO2max | Daily MVPA (70 min) | 39 | VO2max↑ (E) |
| Tan et al. (2015) [36] | M—46 | 8–10 | SRT, VO2max, HR, FATmax | Daily PA (40 min) | 10 | VO2max↑ (E) |
| Martinez et al. (2016) [19] | N—94 M—52 F-42 | 7–9 | SRT, TRE, VO2max, EPOC, HRmax | HIIT, 2x/week (90 min) | 13 | VO2max↑ EPOC↑ (E) |
| Leeuwen et al. (2018) [17] | N—154 M—66 F—88 | 8.5 ± 1.8 | SRT, VO2max, BP | Kids4Fit, 2xweek; 1xweek (20 min) | 13 | VO2max↑ BP↑ (E) |
| Ye et al. (2019) [22] | N—81 M—42 F—39 | 9.23 ± 0.62 | HMR, VO2max | EXG, 1/week (50 min) | 35 | / |
| Davis et al. (2019) [16] | N—75 M—29 F—46 | 9.5–9.8 | TRE, PWV, BP, VO2peak | Daily, ASAE (40 min) | 35 | VO2peak↑ (E) |
| Espinoza-Silva et al. (2019) [37] | N—274 M—120 F—154 | 7–9 | 6MWT, BP, VO2max | HIIT, 2x/week (40–50 min) | 30 | VO2max↑ (E) |
| Leandro et al. (2021) [14] | M—41 | 7–9 | ABPM, RHR, BP | PLT 3x/week (20 min) | 13 | BP↑ RHR↑ (E) |
| Martinez-Viscaiano et al. (2022) [15] | N—487 M—233 F—254 | 9.89 ± 0.71 | SRT, BP, VO2max | HIIT, 4x/week (60 min) | 39 | BP↑ VO2max↑ (E/onlyF) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mijalković, S.; Stanković, D.; Tomljanović, M.; Batez, M.; Grle, M.; Grle, I.; Brkljačić, I.; Jularić, J.; Sporiš, G.; Fišer, S.Ž. School-Based Exercise Programs for Promoting Cardiorespiratory Fitness in Overweight and Obese Children Aged 6 to 10. Children 2022, 9, 1323. https://doi.org/10.3390/children9091323
Mijalković S, Stanković D, Tomljanović M, Batez M, Grle M, Grle I, Brkljačić I, Jularić J, Sporiš G, Fišer SŽ. School-Based Exercise Programs for Promoting Cardiorespiratory Fitness in Overweight and Obese Children Aged 6 to 10. Children. 2022; 9(9):1323. https://doi.org/10.3390/children9091323
Chicago/Turabian StyleMijalković, Stefan, Dušan Stanković, Mario Tomljanović, Maja Batez, Maki Grle, Ivana Grle, Ivan Brkljačić, Josip Jularić, Goran Sporiš, and Suzana Žilič Fišer. 2022. "School-Based Exercise Programs for Promoting Cardiorespiratory Fitness in Overweight and Obese Children Aged 6 to 10" Children 9, no. 9: 1323. https://doi.org/10.3390/children9091323
APA StyleMijalković, S., Stanković, D., Tomljanović, M., Batez, M., Grle, M., Grle, I., Brkljačić, I., Jularić, J., Sporiš, G., & Fišer, S. Ž. (2022). School-Based Exercise Programs for Promoting Cardiorespiratory Fitness in Overweight and Obese Children Aged 6 to 10. Children, 9(9), 1323. https://doi.org/10.3390/children9091323






