Pediatric Open Long-Bone Fracture and Subsequent Deep Infection Risk: The Importance of Early Hospital Care
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Identification, Inclusion and Exclusion Criteria
2.2. Database Structure and Elements
2.3. Statistical Analyses
3. Results
3.1. Patient Characteristics
3.2. Open Fracture and Injury Event Characteristics
3.3. Open Fracture Management Characteristics
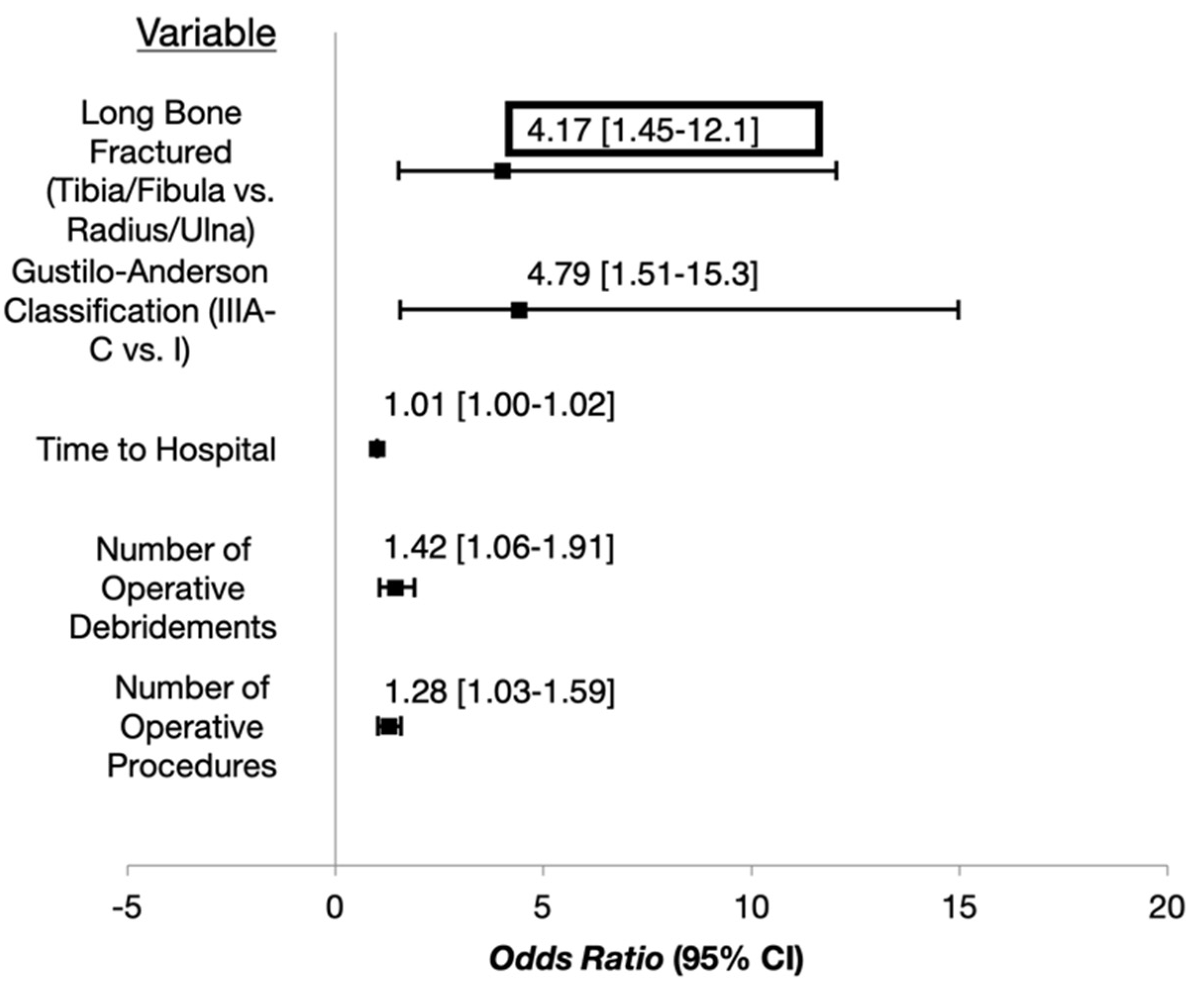
3.4. Multivariable Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Naranje, S.M.; Erali, R.A.; Warner, W.C., Jr.; Sawyer, J.R.; Kelly, D.M. Epidemiology of Pediatric Fractures Presenting to Emergency Departments in the United States. J. Pediatric Orthop. 2016, 36, e45–e48. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.C.; Shen, W.Y. Limb fracture pattern in different pediatric age groups: A study of 3350 children. J. Orthop. Trauma 1993, 7, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Galano, G.J.; Vitale, M.A.; Kessler, M.W.; Hyman, J.E.; Vitale, M.G. The most frequent traumatic orthopaedic injuries from a national pediatric inpatient population. J. Pediatric Orthop. 2005, 25, 39–44. [Google Scholar] [PubMed]
- Stewart, D.G., Jr.; Kay, R.M.; Skaggs, D.L. Open fractures in children. Principles of evaluation and management. J. Bone Jt. Surg. 2005, 87, 2784–2798. [Google Scholar] [CrossRef]
- Trionfo, A.; Cavanaugh, P.K.; Herman, M.J. Pediatric Open Fractures. Orthop. Clin. 2016, 47, 565–578. [Google Scholar] [CrossRef]
- Kelly, D.; Sheffer, B.; Elrod, R.; Piana, L.; Pattisapu, N.; Nolan, V.; Spence, D.; Sawyer, J. Infections After Open Fractures in Pediatric Patients: A Review of 288 Open Fractures. J. Surg. Orthop. Adv. 2022, 31, 73–75. [Google Scholar]
- Gustilo, R.B.; Anderson, J.T. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones. Retrospective and prospective analyses. J. Bone Jt. Surg. 2002, 84, 682. [Google Scholar] [CrossRef]
- Gustilo, R.B.; Anderson, J.T. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: Retrospective and prospective analyses. J. Bone Jt. Surg. 1976, 58, 453–458. [Google Scholar] [CrossRef]
- Lavelle, W.F.; Uhl, R.; Krieves, M.; Drvaric, D.M. Management of open fractures in pediatric patients: Current teaching in Accreditation Council for Graduate Medical Education (ACGME) accredited residency programs. J. Pediatric Orthop. B 2008, 17, 1–6. [Google Scholar] [CrossRef]
- Wetzel, R.J.; Minhas, S.V.; Patrick, B.C.; Janicki, J.A. Current Practice in the Management of Type I Open Fractures in Children: A Survey of POSNA Membership. J. Pediatric Orthop. 2015, 35, 762–768. [Google Scholar] [CrossRef]
- Elia, G.; Blood, T.; Got, C. The Management of Pediatric Open Forearm Fractures. J. Hand Surg. 2020, 45, 523–527. [Google Scholar] [CrossRef]
- Singh, A.; Bierrum, W.; Wormald, J.; Eastwood, D.M. Non-operative versus operative management of open fractures in the paediatric population: A systematic review and meta-analysis of the adverse outcomes. Injury 2020, 51, 1477–1488. [Google Scholar] [CrossRef] [PubMed]
- Pace, J.L.; Kocher, M.S.; Skaggs, D.L. Evidence-based review: Management of open pediatric fractures. J. Pediatric Orthop. 2012, 32 (Suppl. S2), S123–S127. [Google Scholar] [CrossRef]
- Godfrey, J.; Pace, J.L. Type I Open Fractures Benefit From Immediate Antibiotic Administration But Not Necessarily Immediate Surgery. J. Pediatric Orthop. 2016, 36 (Suppl. S1), S6–S10. [Google Scholar] [CrossRef]
- Kreder, H.J.; Armstrong, P. The significance of perioperative cultures in open pediatric lower-extremity fractures. Clin. Orthop. Relat. Res. 1994, 302, 206–212. [Google Scholar] [CrossRef]
- Tomaszewski, R.; Gap, A. Results of the treatment of the open femoral shaft fractures in children. J. Orthop. 2014, 11, 78–81. [Google Scholar] [CrossRef] [PubMed]
- Allison, P.; Dahan-Oliel, N.; Jando, V.T.; Yang, S.S.; Hamdy, R.C. Open fractures of the femur in children: Analysis of various treatment methods. J. Child. Orthop. 2011, 5, 101–108. [Google Scholar] [CrossRef]
- Aslani, H.; Tabrizi, A.; Sadighi, A.; Mirblok, A.R. Treatment of open pediatric tibial fractures by external fixation versus flexible intramedullary nailing: A comparative study. Arch. Trauma Res. 2013, 2, 108–112. [Google Scholar] [CrossRef]
- Aslani, H.; Tabrizi, A.; Sadighi, A.; Mirbolook, A.R. Treatment of pediatric open femoral fractures with external fixator versus flexible intramedullary nails. Arch. Bone Jt. Surg. 2013, 1, 64–67. [Google Scholar]
- Bazzi, A.A.; Brooks, J.T.; Jain, A.; Ain, M.C.; Tis, J.E.; Sponseller, P.D. Is nonoperative treatment of pediatric type I open fractures safe and effective? J. Child. Orthop. 2014, 8, 467–471. [Google Scholar] [CrossRef]
- Doak, J.; Ferrick, M. Nonoperative management of pediatric grade 1 open fractures with less than a 24-h admission. J. Pediatric Orthop. 2009, 29, 49–51. [Google Scholar] [CrossRef]
- Godfrey, J.; Choi, P.D.; Shabtai, L.; Nossov, S.B.; Williams, A.; Lindberg, A.W.; Silva, S.; Caird, M.S.; Schur, M.D.; Arkader, A. Management of Pediatric Type I Open Fractures in the Emergency Department or Operating Room: A Multicenter Perspective. J. Pediatric Orthop. 2017, 39, 372–376. [Google Scholar] [CrossRef]
- Iobst, C.A.; Spurdle, C.; Baitner, A.C.; King, W.F.; Tidwell, M.; Swirsky, S. A protocol for the management of pediatric type I open fractures. J. Child. Orthop. 2014, 8, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Iobst, C.A.; Tidwell, M.A.; King, W.F. Nonoperative management of pediatric type I open fractures. J. Pediatric Orthop. 2005, 25, 513–517. [Google Scholar] [CrossRef] [PubMed]
- Laine, J.C.; Cherkashin, A.; Samchukov, M.; Birch, J.G.; Rathjen, K.E. The Management of Soft Tissue and Bone Loss in Type IIIB and IIIC Pediatric Open Tibia Fractures. J. Pediatric Orthop. 2016, 36, 453–458. [Google Scholar] [CrossRef] [PubMed]
- Ozkul, E.; Gem, M.; Arslan, H.; Alemdar, C.; Azboy, I.; Arslan, S.G. Minimally Invasive Plate Osteosynthesis in Open Pediatric Tibial Fractures. J. Pediatric Orthop. 2016, 36, 416–422. [Google Scholar] [CrossRef]
- Ibrahim, T.; Riaz, M.; Hegazy, A.; Erwin, P.J.; Tleyjeh, I.M. Delayed surgical debridement in pediatric open fractures: A systematic review and meta-analysis. J. Child. Orthop. 2014, 8, 135–141. [Google Scholar] [CrossRef]
- Skaggs, D.L.; Friend, L.; Alman, B.; Chambers, H.G.; Schmitz, M.; Leake, B.; Kay, R.M.; Flynn, J.M. The effect of surgical delay on acute infection following 554 open fractures in children. J. Bone Jt. Surg. 2005, 87, 8–12. [Google Scholar] [CrossRef]
- Skaggs, D.L.; Kautz, S.M.; Kay, R.M.; Tolo, V.T. Effect of delay of surgical treatment on rate of infection in open fractures in children. J. Pediatric Orthop. 2000, 20, 19–22. [Google Scholar] [CrossRef]
- Dedmond, B.T.; Kortesis, B.; Punger, K.; Simpson, J.; Argenta, J.; Kulp, B.; Morykwas, M.; Webb, L.X. Subatmospheric pressure dressings in the temporary treatment of soft tissue injuries associated with type III open tibial shaft fractures in children. J. Pediatric Orthop. 2006, 26, 728–732. [Google Scholar] [CrossRef]
- Halvorson, J.; Jinnah, R.; Kulp, B.; Frino, J. Use of vacuum-assisted closure in pediatric open fractures with a focus on the rate of infection. Orthopedics 2011, 34, e256–e260. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Lopez, E.; Vutescu, E.S.; Orman, S.; Schiller, J.; Eberson, C.P.; Cruz, A.I. Antibiotic Considerations in the Management of Pediatric Open Fractures: Current Concept Review. JPOSNA 2021, 3. Available online: https://www.jposna.org/index.php/jposna/article/view/225 (accessed on 3 August 2022).
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Heinze, G.; Ploner, M.; Dunkler, D.; Southworth, H. Firth’s Bias-Reduced Logistic Regression, Version 1.23; 2018. Available online: https://search.r-project.org/CRAN/refmans/logistf/html/logistf.html (accessed on 3 August 2022).
- Kortram, K.; Bezstarosti, H.; Metsemakers, W.J.; Raschke, M.J.; Van Lieshout, E.M.M.; Verhofstad, M.H.J. Risk factors for infectious complications after open fractures; a systematic review and meta-analysis. Int. Orthop. 2017, 41, 1965–1982. [Google Scholar] [CrossRef] [PubMed]
- Baldwin, K.D.; Babatunde, O.M.; Russell Huffman, G.; Hosalkar, H.S. Open fractures of the tibia in the pediatric population: A systematic review. J. Child. Orthop. 2009, 3, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Luhmann, S.J.; Schootman, M.; Schoenecker, P.L.; Dobbs, M.B.; Gordon, J.E. Complications and outcomes of open pediatric forearm fractures. J. Pediatric Orthop. 2004, 24, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Patzakis, M.J.; Wilkins, J. Factors influencing infection rate in open fracture wounds. Clin. Orthop. Relat. Res. 1989, 243, 36–40. [Google Scholar] [CrossRef]

| Characteristic | Coded |
|---|---|
| Age | (Continuous Measurement) |
| Sex | Female, Male |
| Race a | White, Non-White |
| Weight b | (Continuous) |
| Comorbidities c | No, Yes |
| Self-Reported Antibiotic Allergies | No, Yes |
| Season d | Spring, Summer, Fall, Winter |
| Mechanism of Injury e | Low Energy, High Energy |
| Setting and Contamination Risk f | Low Risk, Medium Risk, High Risk |
| Polytrauma g | No, Yes |
| Multiple Open Fractures | No, Yes |
| Long-Bone Fractured | Femur, Humerus, Radius/Ulna, Tibia/Fibula |
| Segment of Long Bone Fractured | Diaphyseal, Metaphyseal/Epiphyseal |
| Revised Gustilo-Anderson Classification h | I, II, IIIA-C |
| Vascular Compromise/Injury | No, Yes |
| Nerve Injury | No, Yes |
| Compartment Syndrome Requiring Fasciotomy | No, Yes |
| Time to Admission (min) | (Continuous Measurement) |
| Transferred From Outside Facility | No, Yes |
| Time to Antibiotics (min) | (Continuous Measurement), < or ≥3 h |
| Number of Antibiotic Classes Administered | (Count Measurement) |
| Time to Operative Debridement (h) | (Continuous Measurement), < or ≥6 h |
| Number of Operative Debridements | (Count Variable) |
| Time to Definitive Fixation (h) | (Continuous Measurement) |
| Duration of Antibiotics While Admitted (h) | (Continuous Measurement) |
| Length of Hospital Stay (days) | (Continuous Measurement) |
| Discharged with Antibiotics | No, Yes |
| Discharge Disposition | Home, Rehabilitation/Other |
| Total Number of Operative Procedures | (Count Measurement) |
| Characteristic Mean (SD), Median (IQR), or n (%) | No Infection (n = 279) | Deep Infection (n = 24) | TOTAL (n = 303) | OR [95%OR] | p-Value |
|---|---|---|---|---|---|
| Age | 11.8 (±4.2) | 12.4 (±4.7) | 11.8 (±4.2) | 1.029 [0.934, 1.143] | 0.563 |
| Sex | |||||
| Female * | 101 (36.2) | 5 (20.8) | 106 (35.0) | ||
| Male | 178 (63.8) | 19 (79.1) | 197 (65.0) | 2.015 [0.807, 5.912] | 0.139 |
| Race | |||||
| White * | 205 (73.5) | 17 (70.8) | 222 (73.3) | ||
| Non-White | 74 (26.5) | 7 (29.2) | 81 (26.7) | 1.182 [0.456, 2.801] | 0.717 |
| Weight (Standardized Z-Score) | 0.4 (±1.2) | 0.6 (±1.3) | 0.4 (±1.2) | 1.182 [0.834, 1.687] | 0.349 |
| Comorbidities | |||||
| No * | 207 (74.2) | 15 (62.5) | 222 (73.3) | ||
| Yes | 72 (25.8) | 9 (37.5) | 81 (26.7) | 1.754 [0.725, 4.051] | 0.205 |
| Self-Reported Antibiotic Allergies | |||||
| No * | |||||
| Yes | 237 (84.9) 42 (15.1) | 19 (79.2) 5 (20.8) | 256 (84.5) 47 (15.5) | 1.576 [0.527, 4.051 | 0.390 |
| Characteristic Mean (SD), Median (IQR), or n (%) | No Infection (n = 279) | Deep Infection (n = 24) | TOTAL (n = 303) | OR [95%OR] | p-Value |
|---|---|---|---|---|---|
| Season | 0.279 | ||||
| Winter * | 34 (12.2) | 1 (4.2) | 35 (11.6) | ||
| Spring | 75 (26.9) | 7 (29.2) | 82 (27.1) | 2.284 [0.472, 22.26] | 331 |
| Summer | 102 (36.6) | 13 (54.2) | 115 (38.0) | 3.028 [0.698, 28.42] | 0.154 |
| Fall | 68 (24.4) | 3 (12.5) | 71 (23.4) | 1.175 [0.185, 12.47] | 0.870 |
| Mechanism of Injury | |||||
| Low Energy * | 126 (45.2) | 6 (25.0) | 132 (43.6) | ||
| High Energy | 153 (54.8) | 18 (75.0) | 171 (56.4) | 2.347 [0.974, 6.379] | 0.057 |
| Setting and Contamination | 0.239 | ||||
| Low Risk * | 58 (22.4) | 3 (12.5) | 61 (21.6) | ||
| Medium Risk | 78 (30.1) | 5 (20.8) | 83 (29.3) | 1.171 [0.299, 5.228] | 0.822 |
| High Risk | 123 (47.5) | 16 (66.7) | 139 (49.1) | 2.232 [0.750, 8.785] | 0.158 |
| Polytrauma | |||||
| No * | 168 (60.2) | 12 (50.0) | 180 (59.4) | ||
| Yes | 111 (39.8) | 12 (50.0) | 123 (40.6) | 1.511 [0.660, 3.463] | 0.325 |
| Multiple Open Fractures | |||||
| No * | 256 (91.8) | 23 (95.8) | 279 (92.1) | ||
| Yes | 23 (8.2) | 1 (4.2) | 24 (7.9) | 0.697 [0.075, 2.900] | 0.663 |
| Long-Bone | 0.022 ** | ||||
| Tibia/Fibula * | 84 (30.1) | 14 (58.3) | 98 (32.3) | ||
| Femur | 35 (12.5) | 4 (16.7) | 39 (12.9) | 0.730 [0.211, 2.117] | 0.531 |
| Humerus | 35 (12.5) | 1 (4.2) | 36 (11.9) | 0.243 [0.026, 1.048] | 0.059 |
| Radius/Ulna | 125 (44.8) | 5 (20.8) | 130 (42.9) | 0.250 [0.083, 0.660] | 0.005 |
| Segment of Long Bone | |||||
| Diaphyseal * | 197 (70.6) | 18 (75.0) | 215 (71.0) | ||
| Metaphyseal/Epiphyseal | 82 (29.4) | 6 (25.0) | 88 (29.0) | 0.841 [0.308, 2.038] | 0.712 |
| Gustilo-Anderson | 0.017 ** | ||||
| I * | 112 (40.1) | 4 (16.7) | 116 (38.3) | ||
| II | 91 (32.6) | 7 (29.2) | 98 (32.3) | 2.048 [0.632, 7.434] | 0.232 |
| IIIA-C | 76 (27.2) | 13 (54.2) | 89 (29.4) | 4.411 [1.559, 14.984] | 0.004 |
| Vascular Compromise/Injury | |||||
| No * | 257 (92.1) | 20 (83.3) | 277 (91.4) | ||
| Yes | 22 (7.9) | 4 (16.7) | 26 (8.6) | 2.512 [0.738, 7.092] | 0.130 |
| Nerve Injury | |||||
| No * | 242 (86.7) | 23 (95.8) | 265 (87.5) | ||
| Yes | 37 (13.3) | 1 (4.2) | 38 (12.5) | 0.413 [0.045, 1.674] | 0.246 |
| Compartment Syndrome Requiring | |||||
| Fasciotomy | |||||
| No * | 264 (94.6) | 21 (87.5) | 285 (94.1) | ||
| Yes | 15 (5.4) | 3 (12.5) | 18 (5.9) | 2.779 [0.684, 8.776] | 0.139 |
| Characteristic Mean (SD), Median (IQR), or n (%) | No Infection (n = 279) | Deep Infection (n = 24) | TOTAL (n = 303) | OR [95%OR] | p-Value |
|---|---|---|---|---|---|
| Time to Hospital (min) | 61.8 (±41.2) | 89.9 (±64.8) | 64.0 (±44.0) | 1.009 [1.003, 1.016] | 0.008 ** |
| Transferred From OSF | |||||
| No * | 192 (68.8) | 14 (58.3) | 206 (68.0) | ||
| Yes | 87 (31.2) | 10 (41.7) | 97 (32.0) | 1.594 [0.676, 3.644] | 0.280 |
| Time to Antibiotics (min) | 161.5 (±157.4) | 159.8 (±83.9) | 161.4 (±152.8) | 1.000 [0.997, 1.002] | 0.689 |
| <3 h * | 206 (73.8) | 18 (75.0) | 224 (73.9) | ||
| ≥3 h | 73 (26.2) | 6 (25.0) | 79 (26.1) | 0.987 [0.361, 2.399] | 0.978 |
| Number of Antibiotic Classes Administered | 1 (1–2) | 2 (1–3) | 1 (1–2) | 1.271 [0.884, 1.761] | 0.185 |
| Time to Operative Debridement (h) | 14.5 (±8.5) | 18.8 (±27.3) | 14.8 (±11.1) | 1.021 [0.996, 1.047] | 0.093 |
| <6 h * | 46 (17.2) | 6 (27.3) | 52 (17.9) | ||
| ≥6 h | 222 (82.2) | 16 (72.7) | 238 (82.1) | 0.530 [0.211, 1.486] | 0.214 |
| Number of Operative Debridements | 1 (1-1) | 1 (1-2) | 1 (1-1) | 1.429 [1.060, 1.893] | 0.022 ** |
| Time to Definitive Fixation (h) | 23.9 (±36.8) | 30.9 (±37.9) | 24.5 (±36.9) | 1.005 [0.995, 1.012] | 0.273 |
| Duration of Antibiotics While Admitted (h) | 67.1 (±99.2) | 100.3 (±136.1) | 69.8 (±102.7) | 1.002 [0.999, 1.005] | 0.120 |
| Length of Hospital Stay (days) | 4.0 (±4.7) | 4.8 (±5.7) | 4.0 (±4.8) | 1.038 [0.954, 1.108] | 0.351 |
| Discharged with Antibiotics | |||||
| No * | 220 (80.0) | 18 (81.8) | 238 (80.1) | ||
| Yes | 55 (20.0) | 4 (18.2) | 59 (19.9) | 0.967 [0.292, 2.611] | 0.950 |
| Discharge Disposition | |||||
| Home * | 265 (95.3) | 21 (87.5) | 286 (94.7) | ||
| Rehabilitation/Other | 13 (4.7) | 3 (12.5) | 16 (5.3) | 3.203 [0.780, 10.319] | 0.099 |
| Number of Operative Procedures | 1 (1-1) | 1 (1-3) | 1 (1-1) | 1.278 [1.034, 1.584] | 0.026 ** |
| Characteristic | OR [95% CI] | p-Value |
|---|---|---|
| Long-Bone | ||
| Tibia/Fibula * | ||
| Femur | 0.508 [0.131, 1.614] | 0.262 |
| Humerus | 236 [0.025, 1.064] | 0.062 |
| Radius/Ulna | 0.380 [0.107, 1.178] | 0.096 |
| Gustilo-Anderson | ||
| I * | ||
| II | 1.169 [0.302, 4.845] | 0.822 |
| IIIA-C | 2.366 [0.622, 10.074] | 0.210 |
| Time to Hospital | 1.010 [1.003, 1.017] | 0.009 ** |
| Number of Operative Debridements | 1.209 [0.621, 2.408] | 0.573 |
| Number of Operative Procedures | 1.001 [0.581, 1.557] | 0.996 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuhn, A.W.; Troyer, S.C.; Martus, J.E. Pediatric Open Long-Bone Fracture and Subsequent Deep Infection Risk: The Importance of Early Hospital Care. Children 2022, 9, 1243. https://doi.org/10.3390/children9081243
Kuhn AW, Troyer SC, Martus JE. Pediatric Open Long-Bone Fracture and Subsequent Deep Infection Risk: The Importance of Early Hospital Care. Children. 2022; 9(8):1243. https://doi.org/10.3390/children9081243
Chicago/Turabian StyleKuhn, Andrew W., Stockton C. Troyer, and Jeffrey E. Martus. 2022. "Pediatric Open Long-Bone Fracture and Subsequent Deep Infection Risk: The Importance of Early Hospital Care" Children 9, no. 8: 1243. https://doi.org/10.3390/children9081243
APA StyleKuhn, A. W., Troyer, S. C., & Martus, J. E. (2022). Pediatric Open Long-Bone Fracture and Subsequent Deep Infection Risk: The Importance of Early Hospital Care. Children, 9(8), 1243. https://doi.org/10.3390/children9081243






