A Controlled Trial Evaluating the Impact of a Home-Visiting Program on Maternal Disruptive Communication in a Vulnerable Population
Abstract
:1. Introduction
1.1. Maternal Disruptive Communication in Vulnerable Populations
1.2. Intervention Programs Targeting Maternal Disruptive Communication
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.2.1. Assessment
2.2.2. The Intervention
2.3. Measures
- (1)
- Socioeconomic risk, composed of four sub-categories: educational level lower than 9 years of schooling; low income (defined as being sufficiently poor to be eligible for free health care); first generation immigrant; and single parenthood (defined as intending to bring up the child without the presence of the child’s father).
- (2)
- (3)
- Parenting risk, composed of four sub-categories: perinatal complications; unplanned/unwanted pregnancy; early loss of attachment figure (when the woman was less than 11 years old); and being under 20 years of age.
- (4)
- Infant risk, composed of two sub-categories: premature birth and tobacco and/or alcohol use during pregnancy.
2.4. Statistical Analysis Procedures
3. Results
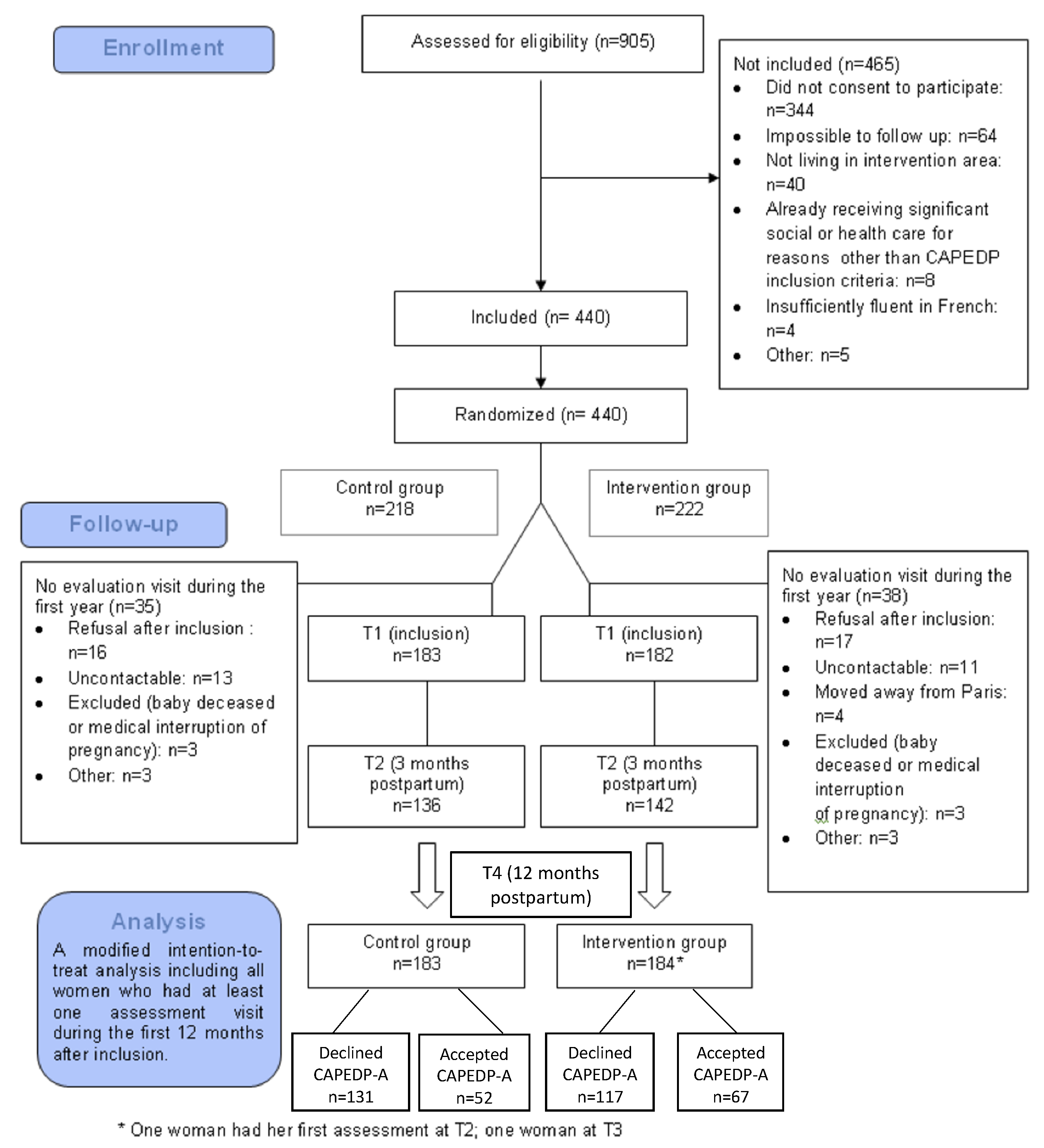
3.1. CAPEDP-A Flowchart
3.2. Risk Factors
- (1)
- The average age of the infants when assessment took place was 14.2 (SD = 2.8) months;
- (2)
- The mothers’ average age at inclusion was 22.3 (SD = 2.5; median age = 23.0 (20.0–24.5));
- (3)
- Almost half of the mothers (n = 57; 47.9%) were first generation immigrants;
- (4)
- 15.1% (n = 18) had less than 9 years of education, but a large majority (n = 100; 83%) had less than 12 years of education;
- (5)
- In total, 39.5% (n = 45) of households had a monthly income of less than EUR 840;
- (6)
- Overall, 40.3% (n = 48) declared that they were not living in a couple, and 59.7% (n = 71) were married to or living with the child’s father;
- (7)
- Overall, 24.2% (n = 29) of mothers declared themselves to be single parents (intending to raise their child without the father);
- (8)
- Overall, 42.9% (n = 51) were sufficiently poor to be eligible for free, state-funded healthcare.
- (1)
- The number of women under the age of 20 was lower in the intervention group (n = 20; 37.7%) than in control group (n = 14; 20.9%); χ2 (1) = 6.52; p = 0.01);
- (2)
- Women in the intervention group declared more tobacco and/or alcohol use during pregnancy (n = 24; 35.8%) than control-group mothers (n = 9; 17.3%; χ2 (1) = 5.01; p = 0.03).
3.3. Maternal Disruptive Communication
3.3.1. Maternal Disruptive Communication and Risk Factors
- (1)
- Benefited from free health care (χ2 (1) = 4.21; p = 0.04; disruptive mothers: n (%) = 26 (54.2%) vs. non-disruptive mothers: n (%) = 22 (33.8%);
- (2)
- Given birth prematurely (χ2 (1) = 4.24; p = 0.04; disruptive mothers: n (%) = 6 (13.0) vs. non-disruptive mothers: n (%) = 2 (3.2)).
- (1)
- A higher number of risk factors (F(1) = 6.74; p = 0.01; disruptive mothers: mean (SD) = 4.4 (2.1) vs. non-disruptive mothers: mean (SD) = 3.4 (2.0));
- (2)
- At least five risk factors (χ2 (1) = 5.61; p = 0.02; disruptive mothers: n (%) = 24 (50.0) vs. non-disruptive mothers: n (%) = 20 (30.3)).
3.3.2. Impact of Intervention on Maternal Disruptive Communication
4. Discussion
4.1. Maternal Disruptive Communication and Risk Factors
4.2. Impact of the Intervention Program on Maternal Disruptive Communication
4.3. Study Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sroufe, A. The place of attachment in development. In Handbook of Attachment: Theory, Research, and Clinical Applications, 3rd ed.; Cassidy, J., Shaver, P.R., Eds.; The Guilford Press: New York, NY, USA, 2016; pp. 935–949. [Google Scholar]
- Lyons-Ruth, K.; Repacholi, B.; McLeod, S.; Silva, E. Disorganized attachment behavior in infancy: Short-term stability, maternal and infant correlates, and risk-related subtypes. Dev. Psychopathol. 1991, 3, 377–396. [Google Scholar] [CrossRef]
- Deater-Deckard, K.; Dodge, K.A.; Bates, J.E.; Pettit, G.S. Multiple risk factors in the development of externalizing behavior problems: Group and individual differences. Dev. Psychopathol. 1998, 10, 469–493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greenberg, M.T.; Speltz, M.L.; Deklyen, M.; Jones, K. Correlates of clinic referral for early conduct problems: Variable- and person-oriented approaches. Dev. Psychopathol. 2001, 13, 255–276. [Google Scholar] [CrossRef]
- Jones, D.J.; Forehand, R.; Brody, G.; Armistead, L. Psychosocial adjustment of African American children in single-mother families: A test of three risk models. J. Marriage Fam. 2002, 64, 105–115. [Google Scholar] [CrossRef]
- Sameroff, A.J. Developmental systems and psychopathology. Dev. Psychopathol. 2000, 12, 297–312. [Google Scholar] [CrossRef] [PubMed]
- Lyons-Ruth, K.; Bronfman, E.; Parsons, E. Chapter IV. Maternal Frightened, Frightening, or Atypical Behavior and Disorganized Infant Attachment Patterns. Monogr. Soc. Res. Child Dev. 1999, 64, 67–96. [Google Scholar] [PubMed]
- Cyr, C.; Euser, E.; Bakermans-Kranenburg, M.; van IJzendoorn, M. Attachment security and disorganization in maltreating and high-risk families: A series of meta-analyses. Dev. Psychopathol. 2010, 22, 87–108. [Google Scholar] [CrossRef]
- Main, M.; Hesse, E. Parents’ unresolved traumatic experiences are related to infant disorganized attachment status: Is frightened and/or frightening parental behavior the linking mechanism? In Attachment in the Preschool Years: Theory, Research, and Intervention; The University of Chicago Press: Chicago, IL, USA, 1990; pp. 161–182. [Google Scholar]
- Solomon, J.; George, C. The place of disorganization in attachment theory: Linking classic observations with contemporary findings. In Attachment Disorganization; The Guilford Press: New York, NY, USA, 1999; pp. 3–32. [Google Scholar]
- Carlson, E.A. A Prospective Longitudinal Study of Attachment Disorganization/Disorientation. Child Dev. 1998, 69, 1107–1128. [Google Scholar] [CrossRef]
- Crittenden, P. Relationships at risk. In Clinical Implications of Attachment; Lawrence Erlbaum Associates, Inc.: Hillsdale, NJ, USA, 1988; pp. 136–174. [Google Scholar]
- Schneider-Rosen, K.; Braunwald, K.G.; Carlson, V.; Cicchetti, D. Current perspectives in attachment theory: Illustration from the study of maltreated infants. Monogr. Soc. Res. Child Dev. 1985, 50, 194–210. [Google Scholar] [CrossRef]
- Belsky, J.; Rosenberger, K.; Crnic, K. Maternal personality, marital quality, social support and infant temperament: Their significance for infant–mother attachment in human families. In Motherhood in Human and Nonhuman Primates: Biosocial Determinants; Karger: Basel, Switzerland, 1995; pp. 115–124. [Google Scholar]
- Bronfenbrenner, U. Ecology of the family as a context for human development: Research perspectives. Dev. Psychol. 1986, 22, 723–742. [Google Scholar] [CrossRef]
- Shaw, D.; Vondra, J.; Dowdell, K.; Keenan, K.; Dunn, M. Chronic Family Adversity and Early Child Behavior Problems: A Longitudinal Study of Low Income Families. J. Child Psychol. Psychiatry 1994, 35, 1109–1122. [Google Scholar] [CrossRef]
- Belsky, J. Parent, infant, and social-contextual antecedents of father-son attachment security. Dev. Psychol. 1996, 32, 905–913. [Google Scholar] [CrossRef]
- Fearon, R.P.; Bakermans-Kranenburg, M.J.; Van IJzendoorn, M.H.; Lapsley, A.M.; Roisman, G.I. The Significance of Insecure Attachment and Disorganization in the Development of Children’s Externalizing Behavior: A Meta-Analytic Study. Child Dev. 2010, 81, 435–456. [Google Scholar] [CrossRef]
- Bakermans-Kranenburg, M.J.; van IJzendoorn, M.H.; Juffer, F. Less is more: Meta-analyses of sensitivity and attachment interventions in early childhood. Psychol. Bull. 2003, 129, 195–215. [Google Scholar] [CrossRef]
- Moss, E.; Dubois-Comtois, K.; Cyr, C.; Tarabulsy, G.M.; St-Laurent, D.; Bernier, A. Efficacy of a home-visiting intervention aimed at improving maternal sensitivity, child attachment, and behavioral outcomes for maltreated children: A randomized control trial. Dev. Psychopathol. 2011, 23, 195–210. [Google Scholar] [CrossRef]
- Moran, G.; Pederson, D.R.; Krupka, A. Maternal unresolved attachment status impedes the effectiveness of interventions with adolescent mothers. Infant Ment. Health J. 2005, 26, 231–249. [Google Scholar] [CrossRef]
- Saïas, T.; Greacen, T.; Tubach, F.; Dugravier, R.; Marcault, E.; Tereno, S.; Guédeney, A.; The CAPEDP Study Group. Supporting families in challenging contexts: The CAPEDP project. Glob. Health Promot. 2013, 20, 66–70. [Google Scholar] [CrossRef] [Green Version]
- Tereno, S.; Guedeney, N.; Dugravier, R.; Greacen, T.; Saïas, T.; Tubach, F. Implementation and assessment of an early home-based intervention on infant attachment organisation: The CAPEDP attachment study in France. Glob. Health Promot. 2012, 20, 71–75. [Google Scholar] [CrossRef]
- Tubach, F.; Greacen, T.; Saïas, T.; Dugravier, R.; Guedeney, N.; Ravaud, P.; Tereno, S.; Tremblay, R.; Falissard, B.; Guedeney, A.; et al. A home-visiting intervention targeting determinants of infant mental health: The study protocol for the CAPEDP randomized controlled trial in France. BMC Public Health 2012, 12, 648. [Google Scholar] [CrossRef] [Green Version]
- Tereno, S.; Guedeney, N.; Greacen, T.; Guedeney, A.; The CAPEDP Study Group. CAPEDP-Attachment: An early home-based intervention targeting multi-risk families. In Handbook of Attachment-Based Therapies; Steele, H., Steele, M., Eds.; The Guilford Press: New York, NY, USA, 2018. [Google Scholar]
- Bronfman, E.; Madigan, S.; Lyons-Ruth, K. The Atypical Behavior Instrument for Assessment and Classification Harvard Medical School, Cambridge, MA, USA, Unpublished manuscript. 1992–2009.
- Ainsworth, M.D.S. (Ed.) Patterns of Attachment: A Psychological Study of the Strange Situation; Routledge: New York, NY, USA, 2015; 417p. [Google Scholar]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of Postnatal Depression: Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef] [Green Version]
- Derogatis, L.R. SCL 90 R Administration, Scoring and Procedures Manual II for the Revised Version and Other Instruments of the Psychopathology Rating Scale Series; Clinical Psychometric Research: Towson, MD, USA, 1986. [Google Scholar]
- Foulon, S.; Greacen, T.; Pasquet, B.; Dugravier, R.; Saïas, T.; Guedeney, N.; Guedeney, A.; Tubach, F.; CAPEDP Study Group. Predictors of Study Attrition in a Randomized Controlled Trial Evaluating a Perinatal Home-Visiting Program with Mothers with Psychosocial Vulnerabilities. PLoS ONE 2015, 10, e0142495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raikes, H.; Thompson, R. Links between risk and attachment security: Models of influence. J. Appl. Dev. Psychol. 2005, 26, 440–455. [Google Scholar] [CrossRef]
- Bakermans-Kranenburg, M.J.; van IJzendoorn, M.H.; Kroonenberg, P.M. Differences in attachment security between African-American and white children: Ethnicity or socio-economic status? Infant Behav. Dev. 2004, 27, 417–433. [Google Scholar] [CrossRef]
- Tereno, S.; Madigan, S.; Lyons-Ruth, K.; Plamondon, A.; Atkinson, L.; Guedeney, N.; Greacen, T.; Dugravier, R.; Saias, T.; Guedeney, A. Assessing a change mechanism in a randomized home-visiting trial: Reducing disrupted maternal communication decreases infant disorganization. Dev. Psychopathol. 2017, 29, 637–649. [Google Scholar] [CrossRef]
- Madigan, S.; Hawkins, E.; Goldberg, S.; Benoit, D. Reduction of disrupted caregiver behavior using modified interaction guidance. Infant Ment. Health J. 2006, 27, 509–527. [Google Scholar] [CrossRef]
- Guedeney, A.; Tereno, S. La vidéo dans l’observation d’évaluation et d’intervention en santé mentale du jeune enfant: Un outil pour la transmission. Neuropsychiatr. Enfance Adolesc. 2012, 60, 261–266. [Google Scholar] [CrossRef]
- Clarke, K.; King, M.; Prost, A. Psychosocial Interventions for Perinatal Common Mental Disorders Delivered by Providers Who Are Not Mental Health Specialists in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis. PLoS Med. 2013, 10, e1001541. [Google Scholar] [CrossRef] [Green Version]
- Reynolds, A.J.; Rolnick, A.J.; Englund, M.M.; Temple, J. Childhood Programs and Practices in the First Decade of Life: A Human Capital Integration; Cambridge University Press: Cambridge, UK, 2010; Available online: http://www.scopus.com/inward/record.url?scp=84923507281&partnerID=8YFLogxK (accessed on 19 April 2022).
- Fraiberg, S. Clinical Studies in Infant Mental Health: The First Year of Life; Basic Books: New York, NY, USA, 1980. [Google Scholar]
| Declined CAPEDP-A (n = 248) n (%) | Accepted CAPEDP-A (n = 119) n (%) | p-Value | ||
|---|---|---|---|---|
| Group | Care as usual | 131 (52.8) | 52 (43.7) | |
| intervention | 117 (47.2) | 67 (56.3) | p = 0.10 | |
| Age | Min/Max | 16.0/26.0 | 16.0/26.0 | |
| Mean (std) | 22.3 (2.4) | 22.3 (2.5) | p = 0.85 | |
| Access to free health care | Yes | 120 (49.0) | 50 (42.4) | |
| No | 125 (51.0) | 68 (57.6) | p = 0.24 | |
| <9 years of education | Yes | 43 (17.5) | 18 (15.1) | |
| No | 203 (82.5) | 101 (84.9) | p = 0.57 | |
| Marital status | In couple | 132 (53.9) | 71 (59.7) | |
| Single | 113 (46.1) | 48 (40.3) | p = 0.30 | |
| Monthly income < EUR 840 | Yes | 105 (44.9) | 45 (39.5) | |
| No | 129 (55.1) | 69 (60.5) | p = 0.34 | |
| Nationality | French | 141 (57.3) | 70 (58.8) | |
| Other | 105 (42.7) | 49 (41.2) | p = 0.79 | |
| Planned pregnancy | Yes | 145 (59.2) | 81 (68.1) | |
| No | 100 (40.8) | 38 (31.9) | p = 0.10 | |
| Tobacco and drug use | Yes | 61 (24.9) | 33 (27.7) | |
| during pregnancy | No | 184 (75.1) | 86 (72.3) | p = 0.56 |
| Depressive symptomatology | Mean (std) | 10.8 (5.7) | 10.6 (5.5) | p = 0.70 |
| Intervention Group (n = 63) n (%) | Control Group (n = 51) n (%) | |
|---|---|---|
| Child age mean, SD in months | 14.3 (2.9) | 14.0 (2.7) |
| Maternal age mean, SD in years | 22.1 (2.5) | 22.5 (2.5) |
| <20 years old | 20 (37.7) ** | 14 (20.9) |
| Infant gender males | 21 (46.7) | 27 (45.8) |
| Marital status married/living together | 34 (65.4) | 37 (55.2) |
| Educational level <= 9 years | 9 (17.3) | 9 (13.4) |
| Monthly income < EUR 840 | 20 (40.8) | 25 (38.5) |
| Tobacco/drug use during pregnancy | 24 (35.8) * | 9 (17.3) |
| Risk Factors | MDC (n = 48) n (%) | No MDC (n = 66) n (%) | p-Value |
|---|---|---|---|
| Socioeconomic Risk | |||
| At least one | 37 (77.1) | 47 (71.2) | p = 0.40 |
| Total number (mean; SD) | 1.5 (1.1) | 1.2 (1.0) | p = 0.04 * |
| <9 years education | 9 (19.1%) | 8 (12.1%) | p = 0.32 |
| Low income < EUR 834 month | 26 (54.2%) | 22 (33.8%) | p = 0.04 * |
| Single parent | 11 (22.9%) | 16 (24.2%) | p = 0.91 |
| Psychopathologic Risk | |||
| At least one | 32 (66.7) | 42 (63.6) | p = 0.55 |
| Total number (mean; SD) | 1.2 (1.0) | 1.1 (1.0) | p = 0.31 |
| EPDS > 11 à T1 | 23 (48.9) | 23 (35.4) | p = 0.14 |
| SCL > 0.80 | 25 (53.2) | 27 (41.5) | p = 0.17 |
| Tobacco/alcohol/substance use during pregnancy | 10 (21.3) | 21 (31.8) | p = 0.37 |
| Parenting Risk | |||
| At least one | 43 (89.6) | 53 (80.3) | p = 0.18 |
| Total number (mean; SD) | 1.9 (1.1) | 1.5 (1.1) | p = 0.08 |
| Previous pregnancy not brought to term | 21 (44.7) | 23 (34.8) | p = 0.27 |
| Planned pregnancy | 30 (63.8) | 48 (72.7) | p = 0.33 |
| Loss of key attachment figure < 11 years-old | 16 (39.0) | 27 (44.3) | p = 0.52 |
| Less than 20 years old | 31 (66.0) | 50 (75.8) | p = 0.43 |
| Infant Risk | |||
| At least one | 15 (31.3) | 23 (34.8) | p = 0.94 |
| Total number (mean; SD) | 0.3 (0.5) | 0.3 (0.5) | p = 0.73 |
| Premature | 6 (13.0) | 2 (3.2) | p = 0.04 * |
| Tobacco/alcohol/substance use during pregnancy | 10 (21.3) | 21 (31.8) | p = 0.37 |
| Cumulative Risk Factors | |||
| Total number (mean; SD) | 4.4 (2.1) | 3.4(2.0) | p = 0.01 ** |
| At least 3 | 40 (83.3) | 49 (74.2) | p = 0.28 |
| At least 4 | 33 (68.8) | 35 (53.0) | p = 0.07 |
| At least 5 | 24 (50.0) | 20 (30.3) | p = 0.02 * |
| Number of home visits (mean; SD) | 18.5 (7.05) | 19.1 (7.7) | p = 0.75 |
| Intervention Group n = 63 | Control Group n = 51 | Total N = 114 | χ2 (dl) | p-Value | |
|---|---|---|---|---|---|
| Disrupted | 20 (31.7%) | 27 (51.9%) | 47 (41.2%) | 4.45 (1) | 0.04 * |
| Not disrupted | 43 (68.3%) | 24 (48.1%) | 67 (58.8%) |
| Variables | OR | 95% CI | p-Value | Effect Size |
|---|---|---|---|---|
| Impact of CAPEDP intervention on MDC | 0.44 | 0.28–0.95 | 0.04 | 2.27 |
| Impact adjusting for significant risk factors (low income, premature baby) | 0.31 | 0.10–0.93 | 0.04 | 3.23 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tereno, S.; Greacen, T.; Guedeney, A.C. A Controlled Trial Evaluating the Impact of a Home-Visiting Program on Maternal Disruptive Communication in a Vulnerable Population. Children 2022, 9, 1166. https://doi.org/10.3390/children9081166
Tereno S, Greacen T, Guedeney AC. A Controlled Trial Evaluating the Impact of a Home-Visiting Program on Maternal Disruptive Communication in a Vulnerable Population. Children. 2022; 9(8):1166. https://doi.org/10.3390/children9081166
Chicago/Turabian StyleTereno, Susana, Tim Greacen, and Antoine C. Guedeney. 2022. "A Controlled Trial Evaluating the Impact of a Home-Visiting Program on Maternal Disruptive Communication in a Vulnerable Population" Children 9, no. 8: 1166. https://doi.org/10.3390/children9081166
APA StyleTereno, S., Greacen, T., & Guedeney, A. C. (2022). A Controlled Trial Evaluating the Impact of a Home-Visiting Program on Maternal Disruptive Communication in a Vulnerable Population. Children, 9(8), 1166. https://doi.org/10.3390/children9081166






