Access to Care for US Children with Co-Occurrence of Autism Spectrum Disorder and Epilepsy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Participants and Measures
2.3. Statistical Analysis
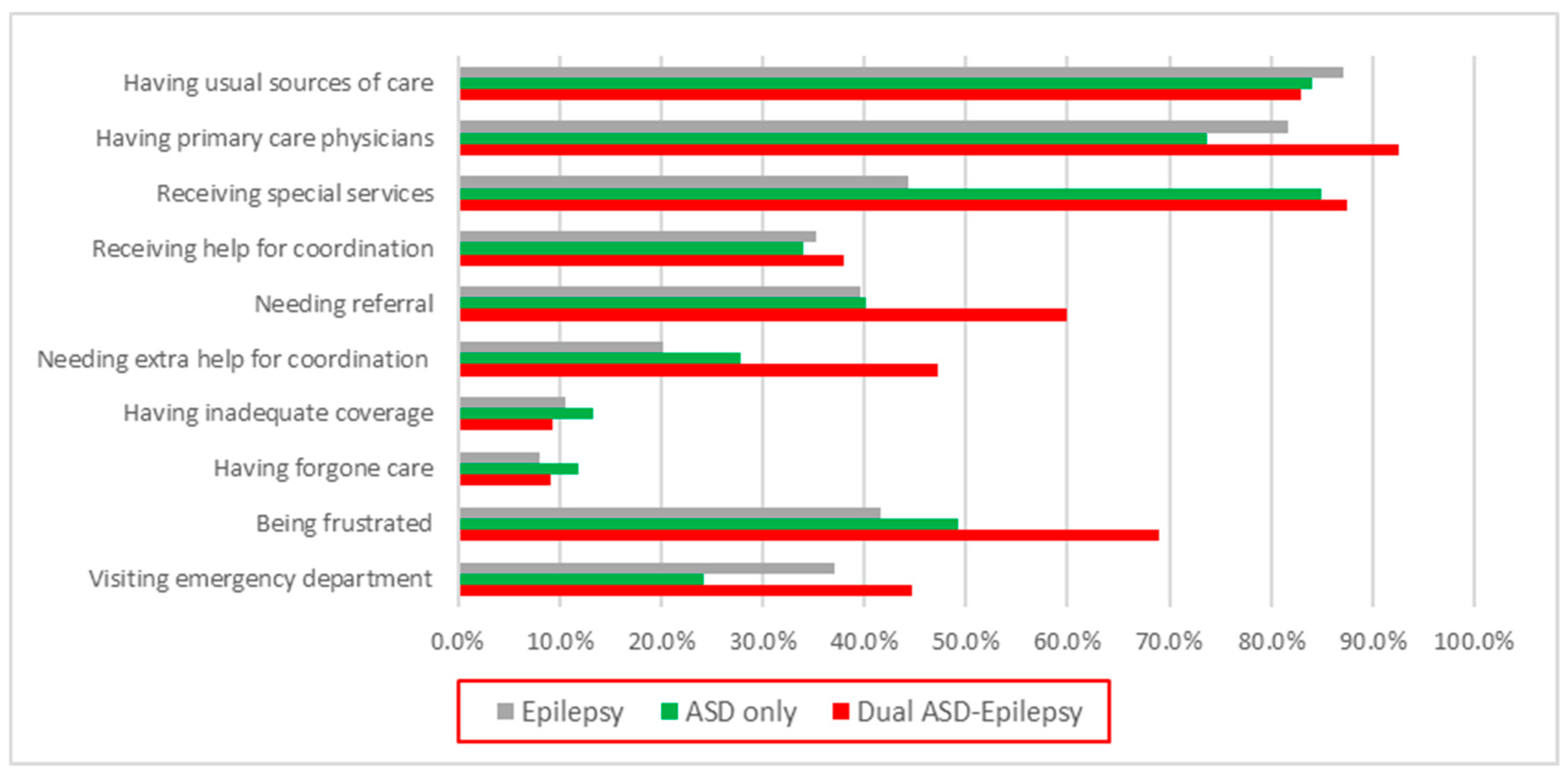
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Outcome Indicators | NSCH Category | Survey Questions |
|---|---|---|
| Having usual sources of care (USC) | Health Care Services | Is there a place that this child USUALLY goes when he or she is sick or you or another caregiver needs advice about his or her health? |
| Having primary care physicians (PCP) | Experience with Child’s Health Care Providers | Do you have one or more persons you think of as this child’s personal doctor or nurse? |
| Needing referral | Experience with Child’s Health Care Providers | DURING THE PAST 12 MONTHS, did this child need a referral to see any doctors or receive any services? |
| Visiting emergency department (ED) | Health Care Services | DURING THE PAST 12 MONTHS, how many times did this child visit a hospital emergency room? |
| Having adequate coverage | Child’s Health Insurance Coverage | How often does this child’s health insurance offer benefits or cover services that meet this child’s needs? |
| Having forgone health care | Health Care Services | DURING THE PAST 12 MONTHS, was there any time when this child needed health care but it was not received? |
| Being frustrated in efforts to get service | Health Care Services | DURING THE PAST 12 MONTHS, how often were you frustrated in your efforts to get services for this child? |
| Receiving special services | Health Care Services | Has this child EVER received special services to meet his or her developmental needs such as speech, occupational, or behavioral therapy? |
| Receiving help on care coordination | Experience with Child’s Health Care Providers | DURING THE PAST 12 MONTHS, did anyone help you arrange or coordinate this child’s care among the different doctors or services that this child uses? |
| Needing extra help for coordinating | Experience with Child’s Health Care Providers | DURING THE PAST 12 MONTHS, have you felt that you could have used extra help arranging or coordinating this child’s care among the different health care providers or services? |
References
- Newschaffer, C.J.; Croen, L.A.; Daniels, J.; Giarelli, E.; Grether, J.K.; Levy, S.E.; Mandell, D.S.; Miller, L.A.; Pinto-Martin, J.; Reaven, J.; et al. The epidemiology of autism spectrum disorders. Annu. Rev. Public Health 2007, 28, 235–258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lord, C.; Risi, S. Frameworks and methods in diagnosing autism spectrum disorders. Ment. Retard. Dev. Disabil. Res. Rev. 1998, 4, 90–96. [Google Scholar] [CrossRef]
- Kohane, I.S.; McMurry, A.; Weber, G.; MacFadden, D.; Rappaport, L.; Kunkel, L.; Bickel, J.; Wattanasin, N.; Spence, S.; Murphy, S.; et al. The co-morbidity burden of children and young adults with autism spectrum disorders. PLoS ONE 2012, 7, e33224. [Google Scholar] [CrossRef] [PubMed]
- Levy, S.E.; Giarelli, E.; Lee, L.C.; Schieve, L.A.; Kirby, R.S.; Cunniff, C.; Nicholas, J.; Reaven, J.; Rice, C.E. Autism spectrum disorder and co-occurring developmental, psychiatric, and medical conditions among children in multiple populations of the United States. J. Dev. Behav. Pediatr. 2010, 31, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Gurney, J.G.; McPheeters, M.L.; Davis, M.M. Parental report of health conditions and health care use among children with and without autism: National Survey of Children’s Health. Arch. Pediatr. Adolesc. Med. 2006, 160, 825–830. [Google Scholar] [CrossRef] [Green Version]
- Fisher, R.S.; van Emde Boas, W.; Blume, W.; Elger, C.; Genton, P.; Lee, P.; Engel, J., Jr. Epileptic seizures and epilepsy: Definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia 2005, 46, 470–472. [Google Scholar] [CrossRef]
- Canitano, R. Epilepsy in autism spectrum disorders. Eur. Child Adolesc. Psychiatry 2007, 16, 61–66. [Google Scholar] [CrossRef]
- Akhter, S. Epilepsy: A Common Co-Morbidity in ASD. In Autism Spectrum Disorder-Profile, Heterogeneity, Neurobiology and Intervention; IntechOpen: London, UK, 2021; Available online: https://www.intechopen.com/chapters/75612 (accessed on 27 April 2022).
- El Achkar, C.M.; Spence, S.J. Clinical characteristics of children and young adults with co-occurring autism spectrum disorder and epilepsy. Epilepsy Behav. 2015, 47, 183–190. [Google Scholar] [CrossRef]
- Viscidi, E.W.; Triche, E.W.; Pescosolido, M.F.; McLean, R.L.; Joseph, R.M.; Spence, S.J.; Morrow, E.M. Clinical characteristics of children with autism spectrum disorder and co-occurring epilepsy. PLoS ONE 2013, 8, e67797. [Google Scholar] [CrossRef] [Green Version]
- Jensen, F.E. Epilepsy as a spectrum disorder: Implications from novel clinical and basic neuroscience. Epilepsia 2011, 52 (Suppl. S1), 1–6. [Google Scholar] [CrossRef]
- Zhang, W.; Baranek, G.; Boyd, B. Brief Report: Factors Associated with Emergency Department Visits for Epilepsy Among Children with Autism Spectrum Disorder. J. Autism Dev. Disord. 2018, 48, 1854–1860. [Google Scholar] [CrossRef] [PubMed]
- Deavenport-Saman, A.; Lu, Y.; Smith, K.; Yin, L. Do Children with Autism Overutilize the Emergency Department? Examining Visit Urgency and Subsequent Hospital Admissions. Matern. Child Health J. 2016, 20, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.M.; Kung, P.T.; Li, C.I.; Tsai, W.C. The difference in medical utilization and associated factors between children and adolescents with and without autism spectrum disorders. Res. Dev. Disabil. 2015, 36C, 78–86. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Committee on the Public Health Dimensions of the Epilepsies. Available online: https://www.ncbi.nlm.nih.gov/books/NBK100604 (accessed on 27 April 2022).
- Puka, K.; Smith, M.L.; Moineddin, R.; Snead, O.C.; Widjaja, E. Health resource utilization varies by comorbidities in children with epilepsy. Epilepsy Behav. 2016, 57 Pt A, 151–154. [Google Scholar] [CrossRef]
- Data Resource Center for child & Adolescent Health. The National Survey of children’s Health. Available online: https://www.childhealthdata.org/learn-about-the-nsch (accessed on 1 August 2021).
- Data Resource Center for child & Adolescent Health. NSCH Survey Methodology. Available online: https://www.childhealthdata.org/learn-about-the-nsch/methods (accessed on 1 August 2021).
- Volkmar, F.R.; Nelson, D.S. Seizure disorders in autism. J. Am. Acad. Child Adolesc. Psychiatry 1990, 29, 127–129. [Google Scholar] [CrossRef]
- DeVoe, J.E.; Tillotson, C.J.; Wallace, L.S. Insurance coverage gaps among US children with insured parents: Are middle income children more likely to have longer gaps? Matern. Child Health J. 2011, 15, 342–351. [Google Scholar] [CrossRef] [PubMed]
- Kuhlthau, K.; Hill, K.S.; Yucel, R.; Perrin, J.M. Financial burden for families of children with special health care needs. Matern. Child Health J. 2005, 9, 207–218. [Google Scholar] [CrossRef]
- Zimmer, K.P.; Walker, A.; Minkovitz, C.S. Epidemiology of pediatric emergency department use at an urban medical center. Pediatr. Emerg. Care 2005, 21, 84–89. [Google Scholar] [CrossRef]
- Moon, T.D.; Laurens, M.B.; Weimer, S.M.; Levy, J.A. Nonemergent emergency room utilization for an inner-city pediatric population. Pediatr. Emerg. Care 2005, 21, 363–366. [Google Scholar] [CrossRef]
- Lindly, O.J.; Zuckerman, K.E.; Kuhlthau, K.A. Healthcare access and services use among US children with autism spectrum disorder. Autism 2019, 23, 1419–1430. [Google Scholar] [CrossRef]
- Lockwood Estrin, G.; Milner, V.; Spain, D.; Happé, F.; Colvert, E. Barriers to Autism Spectrum Disorder Diagnosis for Young Women and Girls: A Systematic Review. Rev. J. Autism. Dev. Disord. 2021, 8, 454–470. [Google Scholar] [CrossRef] [PubMed]
- Thomas, S.; Hovinga, M.E.; Rai, D.; Lee, B.K. Brief Report: Prevalence of Co-occurring Epilepsy and Autism Spectrum Disorder: The U.S. National Survey of Children’s Health 2011–2012. J. Autism Dev. Disord. 2017, 47, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Jokiranta, E.; Sourander, A.; Suominen, A.; Timonen-Soivio, L.; Brown, A.S.; Sillanpää, M. Epilepsy among children and adolescents with autism spectrum disorders: A population-based study. J. Autism Dev. Disord. 2014, 44, 2547–2557. [Google Scholar] [CrossRef]
- Blackmon, K.; Bluvstein, J.; MacAllister, W.S.; Avallone, J.; Misajon, J.; Hedlund, J.; Goldberg, R.; Bojko, A.; Mitra, N.; Giridharan, R.; et al. Treatment Resistant Epilepsy in Autism Spectrum Disorder: Increased Risk for Females. Autism Res. 2016, 9, 311–320. [Google Scholar] [CrossRef]
- Sharma, V.; Saini, A.G.; Malhi, P.; Singhi, P. Epilepsy and EEG Abnormalities in Children with Autism Spectrum Disorders. Indian J. Pediatr. 2021, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Baranek, G. The Impact of Insurance Coverage Types on Access to and Utilization of Health Services for U.S. Children With Autism. Psychiatr. Serv. 2016, 67, 908–911. [Google Scholar] [CrossRef]
- Wang, L.; Mandell, D.S.; Lawer, L.; Cidav, Z.; Leslie, D.L. Healthcare service use and costs for autism spectrum disorder: A comparison between medicaid and private insurance. J. Autism Dev. Disord. 2013, 43, 1057–1064. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Young, A.; Ruble, L.; McGrew, J. Public vs. private insurance: Cost, use, accessibility, and outcomes of services for children with autism spectrum disorders. Res. Autism Spectr. Disord. 2009, 4, 1023–1033. [Google Scholar] [CrossRef]
- Lukmanji, S.; Manji, S.A.; Kadhim, S.; Sauro, K.M.; Wirrell, E.C.; Kwon, C.S.; Jetté, N. The co-occurrence of epilepsy and autism: A systematic review. Epilepsy Behav. 2019, 98 Pt A, 238–248. [Google Scholar] [CrossRef]
- Berg, A.T.; Plioplys, S. Epilepsy and autism: Is there a special relationship? Epilepsy Behav. 2012, 23, 193–198. [Google Scholar] [CrossRef] [Green Version]
| Variable | ASD N = 2150 Weighted N = 5,622,349 | EP N = 711 Weighted N = 1,678,116 | ASD-EP N = 143 Weighted N = 301,714 |
|---|---|---|---|
| Age | |||
| 2–5 | 13.8% | 21.7% | 11.9% |
| 6–11 | 69.0% | 66.1% | 65.8% |
| 12–17 | 17.2% | 12.2% | 22.3% |
| Sex | |||
| Male | 79.8% | 55.5% | 69.0% |
| Female | 20.2% | 44.5% | 31.0% |
| Race | |||
| White | 62.5% | 58.8% | 70.8% |
| Black | 15.5% | 20.1% | 11.6% |
| Other | 22.0% | 21.0% | 17.6% |
| Insurance Type | |||
| Public | 41.2% | 34.2% | 43.5% |
| Private | 41.0% | 47.9% | 28.1% |
| Public and private | 13.5% | 11.7% | 24.1% |
| Uninsured | 4.3% | 6.1% | 4.3% |
| Household Poverty Level | |||
| 0–99% FPL | 25.1% | 28.2% | 29.5% |
| 100–199% FPL | 29.4% | 23.0% | 24.8% |
| 200–399% FPL | 24.1% | 20.6% | 23.2% |
| 400%+ FPL | 21.3% | 28.2% | 22.5% |
| Parent Education Level | |||
| Below high school | 10.1% | 9.5% | 10.5% |
| High school | 23.4% | 18.1% | 18.6% |
| Above high school | 66.5% | 72.4% | 70.8% |
| Intellectual Disability | |||
| Yes | 16.5% | 10.8% | 36.3% |
| No | 83.5% | 89.2% | 63.7% |
| Variable. | Visiting Emergency Department (ED) | Having Primary Care Physicians (PCP) | ||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p | Odds Ratio (95% CI) | p | |
| ASD-EP | ||||
| ASD-EP (vs. EP only) | 1.290 (0.651–2.557) | 0.4661 | 2.511 (1.018–6.196) | 0.0457 |
| ASD-EP (vs. ASD only) | 2.423 (1.254–4.682) | 0.0084 | 4.314 (1.819–10.23) | 0.0009 |
| Age | ||||
| 6–11 (vs. 2–5) | 0.606 (0.388–0.946) | 0.0276 | 1.039 (0.625–1.726) | 0.8839 |
| 12–17 (vs. 2–5) | 0.670 (0.382–1.175) | 0.1622 | 1.120 (0.544–2.308) | 0.7576 |
| Sex | ||||
| Female (vs. male) | 1.031 (0.690–1.542) | 0.8798 | 1.277 (0.760–2.146) | 0.3564 |
| Race | ||||
| Black (vs. White) | 1.943 (1.236–3.054) | 0.0040 | 0.701 (0.398–1.237) | 0.2201 |
| Other (vs. White) | 0.945 (0.514–1.736) | 0.8550 | 0.623 (0.340–1.141) | 0.1253 |
| Insurance Type | ||||
| Private (vs. public) | 0.334 (0.202–0.554) | <0.0001 | 0.662 (0.386–1.134) | 0.1328 |
| Household Poverty Level | ||||
| 0–99% FPL (vs. 400+) | 1.034 (0.537–1.991) | 0.9192 | 0.305 (0.145–0.645) | 0.0019 |
| 100–199% FPL (vs. 400+) | 0.797 (0.494–1.285) | 0.3520 | 0.367 (0.203–0.665) | 0.0009 |
| 200–399% FPL (vs. 400+) | 1.316 (0.893–1.940) | 0.1647 | 0.485 (0.297–0.794) | 0.0040 |
| Parent Education Level | ||||
| High school (vs. below) | 0.611 (0.247–1.512) | 0.2861 | 2.033 (0.691–5.982) | 0.1974 |
| Above high school (vs. below) | 0.900 (0.342–2.366) | 0.8309 | 2.080 (0.728–5.940) | 0.1714 |
| Intellectual Disability (ID) | ||||
| Yes (vs. no) | 1.095 (0.681–1.762) | 0.7075 | 0.916 (0.476–1.764) | 0.7932 |
| Variable | Parental Frustration | Needing Referral | ||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p | Odds Ratio (95% CI) | p | |
| ASD-EP | ||||
| ASD–EP (vs. EP only) | 2.816 (1.420–5.582) | 0.0030 | 2.131 (1.082–4.200) | 0.0287 |
| ASD–EP (vs. ASD only) | 2.035 (1.072–3.863) | 0.0298 | 1.735 (0.913–3.299) | 0.0926 |
| Age | ||||
| 6–11 (vs. 2–5) | 0.960 (0.650–1.432) | 0.8590 | 0.470 (0.313–0.705) | 0.0003 |
| 12–17 (vs. 2–5) | 0.812 (0.458–1.442) | 0.4773 | 0.518 (0.295–0.907) | 0.0215 |
| Sex | ||||
| Female (vs. male) | 1.196 (0.835–1.715) | 0.3292 | 1.661 (1.187–2.326) | 0.0031 |
| Race | ||||
| Black (vs. White) | 0.917 (0.589–1.430) | 0.7035 | 1.466 (0.925–2.323) | 0.1036 |
| Other (vs. White) | 0.678 (0.401–1.147) | 0.1477 | 0.712 (0.448–1.133) | 0.1515 |
| Insurance Type | ||||
| Private (vs. public) | 0.864 (0.523–1.426) | 0.5666 | 0.727 (0.473–1.117) | 0.1456 |
| Household Poverty Level | ||||
| 0–99% FPL (vs. 400+) | 0.802 (0.467–1.378) | 0.4243 | 1.327 (0.757–2.325) | 0.3235 |
| 100–199% FPL (vs. 400+) | 0.706 (0.427–1.168) | 0.1751 | 1.077 (0.675–1.720) | 0.7552 |
| 200–399% FPL (vs. 400+) | 1.184 (0.846–1.657) | 0.3251 | 1.573 (1.114–2.221) | 0.0100 |
| Parent Education Level | ||||
| High school (vs. below) | 1.067 (0.428–2.662) | 0.8889 | 1.428 (0.564–3.616) | 0.4519 |
| Above high school (vs. below) | 0.781 (0.331–1.844) | 0.5730 | 1.833 (0.745–4.507) | 0.1870 |
| Intellectual Disability (ID) | ||||
| Yes (vs. no) | 2.039 (1.292–3.219) | 0.0022 | 1.872 (1.190–2.944) | 0.0067 |
| Variable | Needing Extra Help | Receiving Help | ||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p | Odds Ratio (95% CI) | p | |
| ASD-EP | ||||
| ASD–EP (vs. EP only) | 3.590 (1.618–7.967) | 0.0017 | 1.034 (0.511–2.091) | 0.9257 |
| ASD–EP (vs. ASD only) | 1.998 (1.054–3.787) | 0.0338 | 1.020 (0.525–1.983) | 0.9528 |
| Age | ||||
| 6–11 (vs. 2–5) | 0.834 (0.535–1.301) | 0.4234 | 0.449 (0.297–0.679) | 0.0002 |
| 12–17 (vs. 2–5) | 0.798 (0.446–1.425) | 0.4452 | 0.733 (0.421–1.275) | 0.2706 |
| Sex | ||||
| Female (vs. male) | 1.556 (0.974–2.485) | 0.0641 | 1.754 (1.190–2.585) | 0.0045 |
| Race | ||||
| Black (vs. White) | 1.763 (1.052–2.955) | 0.0314 | 0.906 (0.529–1.549) | 0.7170 |
| Other (vs. White) | 0.798 (0.446–1.425) | 0.9490 | 0.856 (0.530–1.385) | 0.5271 |
| Insurance Type | ||||
| Private (vs. public) | 0.847 (0.505–1.419) | 0.5274 | 0.448 (0.266–0.755) | 0.0026 |
| Household Poverty Level | ||||
| 0–99% FPL (vs. 400+) | 0.996 (0.518–1.917) | 0.9909 | 0.782 (0.426–1.434) | 0.4259 |
| 100–199% FPL (vs. 400+) | 0.706 (0.410–1.217) | 0.2106 | 1.121 (0.672–1.871) | 0.6614 |
| 200–399% FPL (vs. 400+) | 1.525 (0.992–2.344) | 0.0547 | 1.081 (0.722–1.616) | 0.7060 |
| Parent Education Level | ||||
| High school (vs. below) | 0.877 (0.262–2.936) | 0.8312 | 0.973 (0.325–2.915) | 0.9613 |
| Above high school (vs. below) | 1.119 (0.335–3.732) | 0.8549 | 0.787 (0.274–2.263) | 0.6570 |
| Intellectual Disability (ID) | ||||
| Yes (vs. no) | 1.676 (1.029–2.731) | 0.0381 | 1.156 (0.697–1.917) | 0.5746 |
| Variable | Forgone Health Care | Inadequacy of Benefits | ||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p | Odds Ratio (95% CI) | p | |
| ASD-EP | ||||
| ASD–EP (vs. EP only) | 0.928 (0.367–2.348) | 0.8749 | 1.229 (0.484–3.118) | 0.6644 |
| ASD–EP (vs. ASD only) | 0.653 (0.283–1.506) | 0.3172 | 1.649 (0.719–3.781) | 0.2378 |
| Age | ||||
| 6–11 (vs. 2–5) | 1.636 (0.838–3.193) | 0.1493 | 0.802 (0.457–1.405) | 0.4400 |
| 12–17 (vs. 2–5) | 2.694 (1.087–6.677) | 0.0324 | 0.712 (0.336–1.507) | 0.3741 |
| Sex | ||||
| Female (vs. male) | 1.114 (0.622–1.996) | 0.7163 | 0.601 (0.341–1.057) | 0.0772 |
| Race | ||||
| Black (vs. White) | 0.835 (0.382–1.826) | 0.6517 | 1.570 (0.745–3.309) | 0.2360 |
| Other (vs. White) | 1.585 (0.732–3.431) | 0.2420 | 0.675 (0.377–1.209) | 0.1859 |
| Insurance Type | ||||
| Private (vs. public) | 1.443 (0.621–3.352) | 0.3940 | 0.815 (0.454–1.464) | 0.4934 |
| Household Poverty Level | ||||
| 0–99% FPL (vs. 400+) | 2.252 (1.055–4.806) | 0.0358 | 2.771 (1.075–7.140) | 0.0349 |
| 100–199% FPL (vs. 400+) | 3.232 (1.432–7.294) | 0.0047 | 0.919 (0.487–1.736) | 0.7953 |
| 200–399% FPL (vs. 400+) | 2.662 (1.418–4.999) | 0.0023 | 0.928 (0.562–1.532) | 0.7693 |
| Parent Education Level | ||||
| High school (vs. below) | 1.379 (0.407–4.671) | 0.6057 | 4.854 (1.386–16.99) | 0.0135 |
| Above high school (vs. below) | 1.458 (0.482–4.411) | 0.5043 | 3.235 (1.027–10.19) | 0.0449 |
| Intellectual Disability (ID) | ||||
| Yes (vs. no) | 1.793 (0.990–3.249) | 0.0541 | 0.537 (0.294–0.980) | 0.0427 |
| Variable | Having Usual Sources of Care (USC) | Receiving Special Services | ||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p | Odds Ratio (95% CI) | p | |
| ASD-EP | ||||
| ASD–EP (vs. EP only) | 0.777 (0.314–1.923) | 0.5846 | 8.201 (2.712–24.80) | 0.0002 |
| ASD–EP (vs. ASD only) | 1.057 (0.453–2.467) | 0.8979 | 1.112 (0.365–3.383) | 0.8519 |
| Age | ||||
| 6–11 (vs. 2–5) | 0.942 (0.508–1.748) | 0.8504 | 0.643 (0.422–0.980) | 0.0400 |
| 12–17 (vs. 2–5) | 0.631 (0.286–1.391) | 0.2534 | 0.319 (0.165–0.617) | 0.0007 |
| Sex | ||||
| Female (vs. male) | 0.917 (0.571–1.471) | 0.7178 | 0.575 (0.382–0.866) | 0.0081 |
| Race | ||||
| Black (vs. White) | 0.840 (0.446–1.581) | 0.5890 | 1.791 (0.999–3.209) | 0.0503 |
| Other (vs. White) | 0.874 (0.480–1.593) | 0.6610 | 1.612 (0.893–2.908) | 0.1128 |
| Insurance Type | ||||
| Private (vs. public) | 0.959 (0.510–1.802) | 0.8964 | 0.601 (0.368–0.981) | 0.0416 |
| Household Poverty Level | ||||
| 0–99% FPL (vs. 400+) | 0.282 (0.129–0.620) | 0.0016 | 0.430 (0.217–0.854) | 0.0159 |
| 100–199% FPL (vs. 400+) | 0.366 (0.186–0.722) | 0.0037 | 0.521 (0.302–0.900) | 0.0193 |
| 200–399% FPL (vs. 400+) | 0.482 (0.271–0.855) | 0.0127 | 0.819 (0.539–1.243) | 0.3474 |
| Parent Education Level | ||||
| High school (vs. below) | 0.546 (0.182–1.641) | 0.2812 | 0.785 (0.291–2.118) | 0.6323 |
| Above high school (vs. below) | 0.522 (0.178–1.531) | 0.2363 | 0.594 (0.233–1.514) | 0.2749 |
| Intellectual Disability (ID) | ||||
| Yes (vs. no) | 1.110 (0.599–2.057) | 0.7396 | 4.312 (1.653–11.25) | 0.0028 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, W.; Thompson, K.L. Access to Care for US Children with Co-Occurrence of Autism Spectrum Disorder and Epilepsy. Children 2022, 9, 1094. https://doi.org/10.3390/children9071094
Zhang W, Thompson KL. Access to Care for US Children with Co-Occurrence of Autism Spectrum Disorder and Epilepsy. Children. 2022; 9(7):1094. https://doi.org/10.3390/children9071094
Chicago/Turabian StyleZhang, Wanqing, and Kelsey L. Thompson. 2022. "Access to Care for US Children with Co-Occurrence of Autism Spectrum Disorder and Epilepsy" Children 9, no. 7: 1094. https://doi.org/10.3390/children9071094
APA StyleZhang, W., & Thompson, K. L. (2022). Access to Care for US Children with Co-Occurrence of Autism Spectrum Disorder and Epilepsy. Children, 9(7), 1094. https://doi.org/10.3390/children9071094