Assessment of Cardio-Respiratory Function in Overweight and Obese Children Wearing Face Masks during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Trial Design
2.2. Participants and Study Period
2.3. Interventions
2.4. Objectives
2.5. Main Outcomes and Measures
2.6. Statistical Analysis
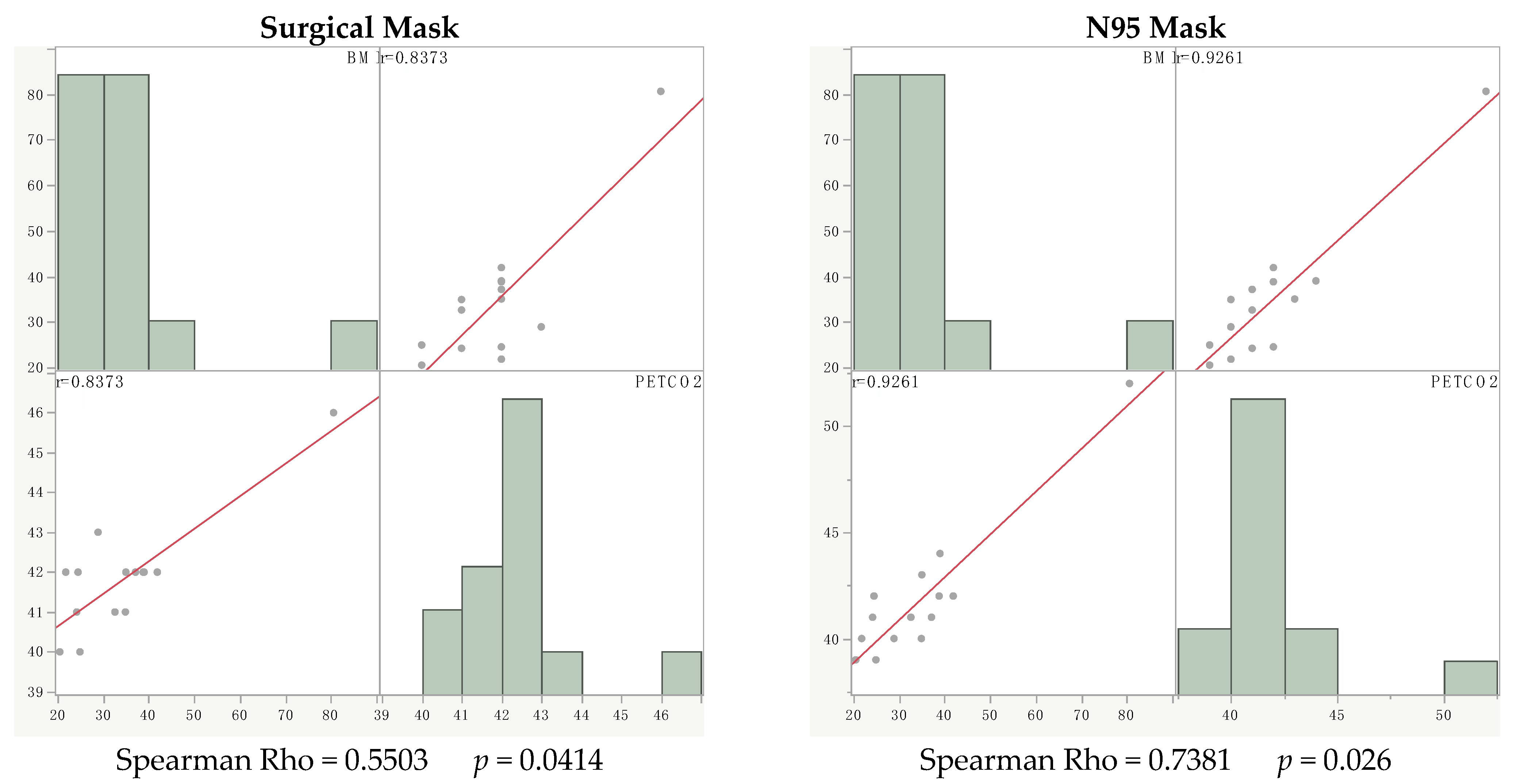
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhou, Y.; Chi, J.; Lv, W.; Wang, Y. Obesity and diabetes as high-risk factors for severe coronavirus disease 2019 (COVID-19). Diabetes/Metabolism Res. Rev. 2020, 37, e3377. [Google Scholar] [CrossRef] [PubMed]
- Petrakis, D.; Margină, D.; Tsarouhas, K.; Tekos, F.; Stan, M.; Nikitovic, D.; Kouretas, D.; Spandidos, D.A.; Tsatsakis, A. Obesity—A risk factor for increased COVID-19 prevalence, severity and lethality. Mol. Med. Rep. 2020, 22, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Dixon, A.E.; Peters, U. The effect of obesity on lung function. Expert Rev. Respir. Med. 2018, 12, 755–767. [Google Scholar] [CrossRef] [PubMed]
- Littleton, S.W.; Tulaimat, A. The effects of obesity on lung volumes and oxygenation. Respir. Med. 2017, 124, 15–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simonnet, A.; Chetboun, M.; Poissy, J.; Raverdy, V.; Noulette, J.; Duhamel, A.; Labreuche, J.; Mathieu, D.; Pattou, F.; Jourdain, M.; et al. High Prevalence of Obesity in Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) Requiring Invasive Mechanical Ventilation. Obesity 2020, 28, 1195–1199. [Google Scholar] [CrossRef]
- Tanaka, S.; Isoda, F.; Ishihara, Y.; Kimura, M.; Yamakawa, T. T lymphopaenia in relation to body mass index and TNF-alpha in human obesity: Adequate weight reduction can be corrective. Clin. Endocrinol. 2001, 54, 347–354. [Google Scholar] [CrossRef]
- Alwarawrah, Y.; Kiernan, K.; Maciver, N.J. Changes in Nutritional Status Impact Immune Cell Metabolism and Function. Front. Immunol. 2018, 9, 1055. [Google Scholar] [CrossRef] [Green Version]
- Isoldi, S.; Mallardo, S.; Marcellino, A.; Bloise, S.; Dilillo, A.; Iorfida, D.; Testa, A.; Del Giudice, E.; Martucci, V.; Sanseviero, M.; et al. The comprehensive clinic, laboratory, and instrumental evaluation of children with COVID-19: A 6-months prospective study. J. Med Virol. 2021, 93, 3122–3132. [Google Scholar] [CrossRef]
- Bloise, S.; Marcellino, A.; Testa, A.; Dilillo, A.; Mallardo, S.; Isoldi, S.; Martucci, V.; Sanseviero, M.T.; Del Giudice, E.; Iorfida, D.; et al. Serum IgG levels in children 6 months after SARS-CoV-2 infection and comparison with adults. Eur. J. Pediatr. 2021, 180, 3335–3342. [Google Scholar] [CrossRef]
- Shekerdemian, L.S.; Mahmood, N.R.; Wolfe, K.K.; Riggs, B.J.; Ross, C.E.; McKiernan, C.A.; Heidemann, S.M.; Kleinman, L.C.; Sen, A.I.; Hall, M.W. Characteristics and outcomes of children with coronavirus disease 2019 (COVID-19) infection admitted to US and Ca-nadian pediatric intensive care units. JAMA Pediatr. 2020, 174, 868–873. [Google Scholar] [CrossRef]
- Zachariah, P.; Johnson, C.L.; Halabi, K.C.; Ahn, D.; Sen, A.I.; Fischer, A.; Banker, S.L.; Giordano, M.; Manice, C.S.; Diamond, R. Epidemiology, clinical features, and disease severity in patients with coronavirus disease 2019 (COVID-19) in a children’s hospital in New York City, New York. JAMA Pediatr. 2020, 174, e202430. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). In Use of Cloth Face Coverings to Help Slow the Spread of COVID-19. July.; 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/cloth-face-cover.html (accessed on 9 April 2020).
- American Academy of Pediatrics. Cloth Face Coverings for Children During COVID-19. 2020. Available online: https://www.healthychildren.org/English/health-issues/conditions/COVID-19/Pages/Cloth-Face-Coverings-for-Children-During-COVID-19.aspx (accessed on 9 April 2020).
- CDC. Children Just as Vulnerable to COVID as Adults. WebMD. 13 October 2021. Available online: https://www.webmd.com/lung/news/20211013/children-at-risk-of-covid (accessed on 10 June 2021).
- Jefferson, T.; Del Mar, C.B.; Dooley, L.; Ferroni, E.; Al-Ansary, L.A.; Bawazeer, G.A.; van Driel, M.L.; Jones, M.A.; Thorning, S.; Beller, E.M.; et al. Physical interventions to interrupt or reduce the spread of respiratory viruses: Systematic review. BMJ 2009, 336, b3675. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- MacIntyre, C.R.; Cauchemez, S.; Dwyer, D.E.; Seale, H.; Cheung, P.; Browne, G.; Fasher, M.; Wood, J.; Gao, Z.; Booy, R.; et al. Face Mask Use and Control of Respiratory Virus Transmission in Households. Emerg. Infect. Dis. 2009, 15, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Lau, J.T.; Tsui, H.; Lau, M.; Yang, X. SARS Transmission, Risk Factors, and Prevention in Hong Kong. Emerg. Infect. Dis. 2004, 10, 587–592. [Google Scholar] [CrossRef]
- Eikenberry, S.E.; Mancuso, M.; Iboi, E.; Phan, T.; Eikenberry, K.; Kuang, Y.; Kostelich, E.; Gumel, A.B. To mask or not to mask: Modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect. Dis. Model. 2020, 5, 293–308. [Google Scholar] [CrossRef] [PubMed]
- Ciocan, C.; Clari, M.; Fabbro, D.; De Piano, M.L.; Garzaro, G.; Godono, A.; Gullino, A.; Romano, C. Impact of wearing a surgical mask on respiratory function in view of a widespread use during COVID-19 outbreak. A case-series study. Med. Lav. 2020, 111, 354–364. [Google Scholar] [CrossRef]
- Fikenzer, S.; Uhe, T.; Lavall, D.; Rudolph, U.; Falz, R.; Busse, M.; Hepp, P.; Laufs, U. Effects of surgical and FFP2/N95 face masks on cardiopulmonary exercise capacity. Clin. Res. Cardiol. 2020, 109, 1522–1530. [Google Scholar] [CrossRef]
- Lubrano, R.; Bloise, S.; Testa, A.; Marcellino, A.; Dilillo, A.; Mallardo, S.; Isoldi, S.; Martucci, V.; Sanseviero, M.; Del Giudice, E.; et al. Assessment of Respiratory Function in Infants and Young Children Wearing Face Masks During the COVID-19 Pandemic. JAMA Netw. Open 2021, 4, e210414. [Google Scholar] [CrossRef]
- Lubrano, R.; Bloise, S.; Marcellino, A.; Ciolli, C.P.; Testa, A.; De Luca, E.; Dilillo, A.; Mallardo, S.; Isoldi, S.; Martucci, V.; et al. Effects of N95 Mask Use on Pulmonary Function in Children. J. Pediatr. 2021, 237, 143–147. [Google Scholar] [CrossRef]
- Hopkins, S.R.; Dominelli, P.B.; Davis, C.K.; Guenette, J.A.; Luks, A.M.; Molgat-Seon, Y.; Sá, R.C.; Sheel, A.W.; Swenson, E.R.; Stickland, M.K. Face Masks and the Cardiorespiratory Response to Physical Activity in Health and Disease. Ann. Am. Thorac. Soc. 2021, 18, 399–407. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. World Health Organization Child Growth Standards. 2006. Available online: https://www.who.int/tools/child-growth-standards/standards (accessed on 5 March 2012).
- World Health Organization. Multicentre Growth Reference Study Group. WHO Child growth standards based on length/height, weight and age. Acta Paediatr. 2006, 450, 76–85. [Google Scholar]
- De Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef]
- Cacciari, E.; Milani, S.; Balsamo, A.; Spada, E.; Bona, G.; Cavallo, L.; Cerutti, F.; Gargantini, L.; Greggio, N.; Tonini, G.; et al. Italian cross-sectional growth charts for height, weight and BMI (2 to 20 yr). J. Endocrinol. Investig. 2006, 29, 581–593. [Google Scholar] [CrossRef]
- Cazzola, M.; Biscione, G.L.; Pasqua, F.; Crigna, G.; Appodia, M.; Cardaci, V.; Ferri, L. Use of 6-min and 12-min walking test for assessing the efficacy of formoterol in COPD. Respir. Med. 2008, 102, 1425–1430. [Google Scholar] [CrossRef]
- Regli, A.; Sommerfield, A.; Von Ungern-Sternberg, B.S. The role of fit testing N95/FFP2/FFP3 masks: A narrative review. Anaesthesia 2020, 76, 91–100. [Google Scholar] [CrossRef]
- Salome, C.M.; King, G.G.; Berend, N. Physiology of obesity and effects on lung function. J. Appl. Physiol. 2010, 108, 206–211. [Google Scholar] [CrossRef] [Green Version]
- Bokov, P.; Delclaux, C. Impact fonctionnel respiratoire de l’obésité. Rev. des Mal. Respir. 2019, 36, 1057–1063. [Google Scholar] [CrossRef]
- Pasarica, M.; Sereda, O.R.; Redman, L.M.; Albarado, D.C.; Hymel, D.T.; Roan, L.E.; Rood, J.C.; Burk, D.H.; Smith, S.R. Reduced Adipose Tissue Oxygenation in Human Obesity: Evidence for rarefaction, macrophage chemotaxis, and inflammation without an angio-genic response. Diabetes 2009, 58, 718–725. [Google Scholar] [CrossRef] [Green Version]
- Rausch, M.E.; Weisberg, S.; Vardhana, P.; Tortoriello, D.V. Obesity in C57BL/6J mice is characterized by adipose tissue hypoxia and cytotoxic T-cell infiltratio. Int. J. Obes. 2008, 32, 451–463. [Google Scholar] [CrossRef] [Green Version]
- Goossens, G.H. The Metabolic Phenotype in Obesity: Fat Mass, Body Fat Distribution, and Adipose Tissue Function. Obes. Facts 2017, 10, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Balmain, B.N.; Halverson, Q.M.; Tomlinson, A.R.; Edwards, T.; Ganio, M.S.; Babb, T.G. Obesity Blunts the Ventilatory Response to Exercise in Men and Women. Ann. Am. Thorac. Soc. 2021, 18, 1167–1174. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Occupational Safety and Health. 42 CFR 84: Respiratory protective devices—Final rules and notice. Fed. Regist. 1995, 60, 30336–30398. [Google Scholar]
- Roberge, R.J.; Bayer, E.; Powell, J.B.; Coca, A.; Roberge, M.R.; Benson, S.M. Effect of Exhaled Moisture on Breathing Resistance of N95 Filtering Facepiece Respirators. Ann. Occup. Hyg. 2010, 54, 671–677. [Google Scholar]
- Poirier, M.P.; Del-Rey, J.A.G.; McAneney, C.M.; Digiulio, A.G. Utility of monitoring capnography, pulse oximetry, and vital signs in the detection of airway mishaps: A hyperoxemic animal model. Am. J. Emerg. Med. 1998, 16, 350–352. [Google Scholar] [CrossRef]
- Napolitano, N.; Nishisaki, A.; Buffman, H.S.; Leffelman, J.; Maltese, M.R.; Nadkarni, V.M. Redesign of an Open-System Oxygen Face Mask with Mainstream Capnometer for Children. Respir. Care 2016, 62, 70–77. [Google Scholar] [CrossRef] [Green Version]
- Lightdale, J.R.; Goldmann, D.A.; Feldman, H.A.; Newburg, A.R.; DiNardo, J.A.; Fox, V.L. Microstream Capnography Improves Patient Monitoring During Moderate Sedation: A Randomized, Controlled Trial. Pediatrics 2006, 117, e1170–e1178. [Google Scholar] [CrossRef]
- Soto, R.G.; Fu, E.S.; Vila, H.; Miguel, R.V. Capnography Accurately Detects Apnea During Monitored Anesthesia Care. Anesthesia Analg. 2004, 99, 379–382. [Google Scholar] [CrossRef]
- Vargo, J.; Zuccaro, G.; Dumot, J.A.; Conwell, D.L.; Morrow, J.; Shay, S.S. Automated graphic assessment of respiratory activity is superior to pulse oximetry and visual assessment for the detection of early respiratory depression during therapeutic upper endoscopy. Gastrointest. Endosc. 2002, 55, 826–831. [Google Scholar] [CrossRef]
| Children | Age | Weight | Height | Body Mass Index | Males/Females |
|---|---|---|---|---|---|
| Months | kg | cm | n/n | ||
| Healthy | 108 | 39 | 139 | 18.61 | 8/7 |
| 72–130 | 28.8–42 | 131–145 | 18.08–20.83 | ||
| Obese | 144 | 73.95 | 149 | 33.75 | 4/10 |
| 107.5–184.75 | 48.55–92.45 | 139–157.88 | 24.43–38.85 |
| Test with Surgical Mask | Test with N95 Mask | |||||||
|---|---|---|---|---|---|---|---|---|
| Without Mask | With Mask | With Mask and Walking Test | Kruskal–Wallis Test | Without Mask | With Mask | With Mask and Walking Test | Kruskal–Wallis Test | |
| T30 | T60 | Twt | T30 | T60 | Twt | p | ||
| SaO2 | 98 | 98 | 98 | NS | 98 | 98 | 97 | NS |
| % | 97–98 | 97–98 | 96–98 | 97–98 | 96–98 | 96–98 | ||
| PETCO2 | 36 | 36 | 35 | NS | 35 | 38 | 39 | NS |
| mmHg | 35–37 | 33–37 | 33–39 | 35–40 | 35–41 | 37–41 | ||
| PR | 96 | 106 | 115 | <0.0015 | 99 | 100 | 109 | <0.0304 |
| pulsation/min | 89–100 | 100–115 | 110–120 | 87–105 | 82–106 | 105–114 | ||
| RR | 22 | 21 | 26 | <0.0001 | 21 | 22 | 25 | <0.0098 |
| breaths/min | 20–23 | 21–22 | 24–28 | 19–22 | 20–23 | 20–30 | ||
| Clinical signs of respiratory distress * | Absent | Absent | Absent | Absent | Absent | Absent | ||
| Test with Surgical Mask | Test with N95 Mask | |||||||
|---|---|---|---|---|---|---|---|---|
| Without Mask | With Mask | With Mask and Walking Test | Kruskal–Wallis Test | Without Mask | With Mask | With Mask and Walking Test | Kruskal–Wallis Test | |
| T30 | T60 | Twt | T30 | T60 | Twt | p | ||
| SaO2 | 98 | 97.5 | 97.5 | NS | 98 | 98 | 97 | NS |
| % | 96.75–98.25 | 96.75–98 | 96–98 | 96.75–98.25 | 97–98 | 96–98 | ||
| PETCO2 | 37 | 39 | 42 | <0.0001 | 37 | 39 | 41.5 | <0.0001 |
| mmHg | 35.75–39 | 38–43.25 | 41–42 | 35.75–39.25 | 38.75–41.75 | 40–43.25 | ||
| PR | 93 | 90.5 | 127 | <0.0001 | 93 | 94 | 131 | <0.0002 |
| pulsation/min | 85.75–100.5 | 85.25–102.25 | 118.75–137.25 | 85.75–100.5 | 88.25–105.25 | 112.25–140 | ||
| RR | 20 | 20 | 30 | <0.0001 | 20 | 20.5 | 32 | <0.0001 |
| breaths/min | 16–21.25 | 16–23 | 25.5–36 | 16–21.25 | 18–23.25 | 25.5–34 | ||
| Clinical signs of respiratory distress * | Absent | Absent | Present | Absent | Absent | Present | ||
| Test with Surgical Mask | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Without Mask | With Mask | With Mask and Walking Test | |||||||
| T30 | T60 | Twt | |||||||
| Healthy | Obese | p | Healthy | Obese | p | Healthy | Obese | p | |
| SaO2 | 98 | 98 | NS | 98 | 97.5 | NS | 98 | 97.5 | NS |
| % | 97–98 | 96.75–98.25 | 97–98 | 96.75–98 | 96–98 | 96–98 | |||
| PETCO2 | 36 | 37 | NS | 36 | 39 | 0.0046 | 35 | 42 | 0.0001 |
| mmHg | 35–37 | 35.75–39 | 33–37 | 38–43.25 | 33–39 | 41–42 | |||
| PR | 96 | 93 | NS | 106 | 90.5 | NS | 115 | 127 | NS |
| pulsation/min | 89–100 | 85.75–100.5 | 100–115 | 85.25–102.25 | 110–120 | 118.75–137.25 | |||
| RR | 22 | 20 | NS | 21 | 20 | NS | 26 | 30 | 0.041 |
| breaths/min | 20–23 | 16–21.25 | 21–22 | 16–23 | 24–28 | 25.5–36 | |||
| Clinical signs of respiratory distress * | Absent | Absent | Absent | Absent | Absent | Present | |||
| Test with surgical mask | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Without Mask | With Mask | With Mask and Walking Test | |||||||
| T30 | T60 | Twt | |||||||
| Healthy | Obese | p | Healthy | Obese | p | Healthy | Obese | p | |
| SaO2 | 98 | 98 | NS | 98 | 98 | NS | 97 | 97 | NS |
| % | 97–98 | 96.75–98.25 | 96–98 | 97–98 | 96–98 | 96–98 | |||
| PETCO2 | 35 | 37 | NS | 38 | 39 | NS | 39 | 41.5 | 0.0062 |
| mmHg | 35–40 | 35.75–39.25 | 35–41 | 38.75–41.75 | 37–41 | 40–43.25 | |||
| PR | 99 | 93 | NS | 100 | 94 | NS | 109 | 131 | 0.01 |
| pulsation/min | 87–105 | 85.75–100.5 | 82–106 | 88.25–105.25 | 105–114 | 115.25–140 | |||
| RR | 21 | 20 | NS | 22 | 20.5 | NS | 25 | 32 | 0.0053 |
| breaths/min | 19–22 | 16–21.25 | 20–23 | 18–23.5 | 20–30 | 25.5–34 | |||
| Clinical signs of respiratory distress * | Absent | Absent | Absent | Absent | Absent | Present | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lubrano, R.; Bloise, S.; Sanseviero, M.; Marcellino, A.; Proietti Ciolli, C.; De Luca, E.; Testa, A.; Dilillo, A.; Mallardo, S.; Isoldi, S.; et al. Assessment of Cardio-Respiratory Function in Overweight and Obese Children Wearing Face Masks during the COVID-19 Pandemic. Children 2022, 9, 1053. https://doi.org/10.3390/children9071053
Lubrano R, Bloise S, Sanseviero M, Marcellino A, Proietti Ciolli C, De Luca E, Testa A, Dilillo A, Mallardo S, Isoldi S, et al. Assessment of Cardio-Respiratory Function in Overweight and Obese Children Wearing Face Masks during the COVID-19 Pandemic. Children. 2022; 9(7):1053. https://doi.org/10.3390/children9071053
Chicago/Turabian StyleLubrano, Riccardo, Silvia Bloise, Mariateresa Sanseviero, Alessia Marcellino, Claudia Proietti Ciolli, Enrica De Luca, Alessia Testa, Anna Dilillo, Saverio Mallardo, Sara Isoldi, and et al. 2022. "Assessment of Cardio-Respiratory Function in Overweight and Obese Children Wearing Face Masks during the COVID-19 Pandemic" Children 9, no. 7: 1053. https://doi.org/10.3390/children9071053
APA StyleLubrano, R., Bloise, S., Sanseviero, M., Marcellino, A., Proietti Ciolli, C., De Luca, E., Testa, A., Dilillo, A., Mallardo, S., Isoldi, S., Martucci, V., Del Giudice, E., Leone, R., Iorfida, D., & Ventriglia, F. (2022). Assessment of Cardio-Respiratory Function in Overweight and Obese Children Wearing Face Masks during the COVID-19 Pandemic. Children, 9(7), 1053. https://doi.org/10.3390/children9071053






