Application of a Cold Dry Air Provocation Test in Pediatric Patients with Asthma
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Methods
2.2.1. Blood Tests
2.2.2. Skin Prick Tests
2.2.3. Induced Sputum Tests
2.2.4. Pulmonary Function Tests and Spirometry
2.2.5. Methacholine Provocation Tests
2.2.6. CDA Provocation Test
2.3. Statistical Analysis
3. Results
3.1. CDA Provocation Tests in the Children with Suspected Asthma and/or Respiratory Allergies
3.2. CDA Provocation Test in Asthma Patients
3.3. Comparison between Asthma with Rhinitis and Asthma-Only Group
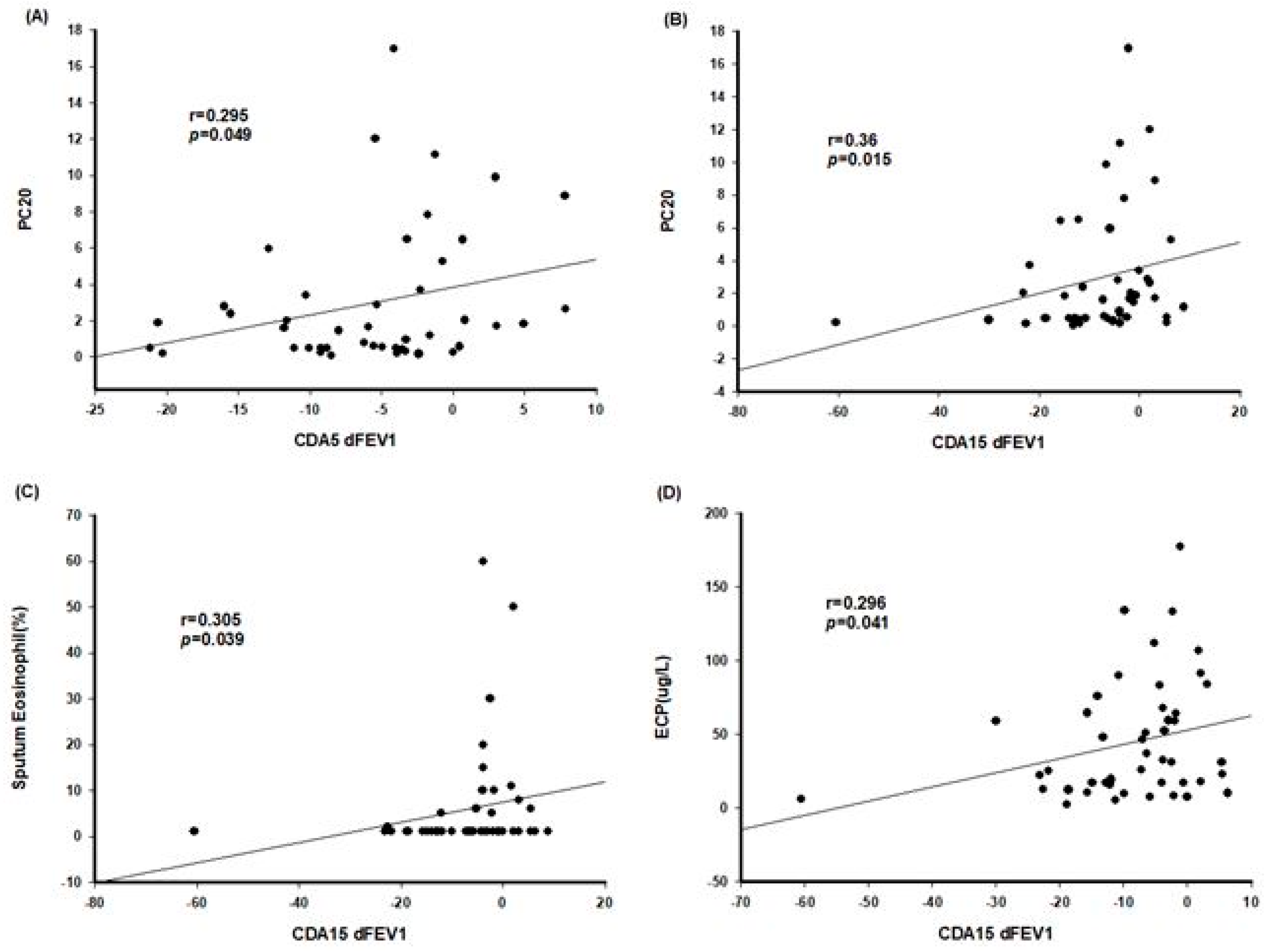
3.4. Comparison between Methacholine and CDA Provocation Tests
3.5. Others
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Busse, W.W.; Rosenwasser, L.J. Mechanisms of asthma. J. Allergy Clin. Immunol. 2003, 111, S799–S804. [Google Scholar] [CrossRef] [Green Version]
- Boonpiyathad, T.; Sözener, Z.C.; Satitsuksanoa, P.; Akdis, C.A. Immunologic mechanisms in asthma. Semin. Immunol. 2019, 46, 101333. [Google Scholar] [CrossRef] [PubMed]
- Tiffeneau, R.; Beauvallet, M. Epreuve de bronchoconstriction et de bronchodilation par aerosols. Bull. Acad. Med. 1945, 129, 165–168. [Google Scholar]
- Chapman, D.G.; Irvin, C.G. Mechanisms of airway hyper-responsiveness in asthma: The past, present and yet to come. Clin. Exp. Allergy 2015, 45, 706–719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cockcroft, D.W.; Davis, B.E. Diagnostic and therapeutic value of airway challenges in asthma. Curr. Allergy Asthma Rep. 2009, 9, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.H.; Kim, M.Y.; Lim, K.H.; Yang, M.S.; Song, W.J.; Lee, J.; Suh, D.I.; Shin, Y.S.; Kwon, J.W.; Kim, S.H.; et al. KAAACI Standardization Committee report on the procedure and application of induced sputum examination. Allergy Asthma Respir. Dis. 2017, 5, 307–311. [Google Scholar] [CrossRef] [Green Version]
- Cockcroft, D.; Davis, B. Direct and indirect challenges in the clinical assessment of asthma. Ann. Allergy Asthma Immunol. 2009, 103, 363–370. [Google Scholar] [CrossRef]
- Crapo, R.; Casaburi, R.; Coates, A.; Enright, P.; Hankinson, J.; Irvin, C.; Macintyre, N.; Mckay, R.; Wanger, J.; Anderson, S.D.; et al. Guidelines for methacholine and exercise challenge testing-1999. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. Am. J. Respir. Crit. Care Med. 2000, 161, 309–329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miller, M.R.; Hankinson, J.; Brusasco, V.; Burgos, F.; Casaburi, R.; Coates, A.; Crapo, R.; Enright, P.; Van Der Grinten, C.; Gustafsson, P.; et al. Standardisation of spirometry. Eur. Respir. J. 2005, 26, 319–338. [Google Scholar] [CrossRef] [Green Version]
- Magni, C.; Chellini, E.; Zanasi, A. Cough variant asthma and atopic cough. Multidiscip. Respir. Med. 2010, 5, 99–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bousquet, J.; Khaltaev, N.; Cruz, A.A.; Denburg, J.; Fokkens, W.; Togias, A.; Zuberbier, T.; Baena-Cagnani, C.E.; Canonica, G.; Van Weel, C.; et al. Allergic rhinitis and its impact on asthma (ARIA) 2008. Allergy 2008, 63 (Suppl. 86), 8–160. [Google Scholar] [CrossRef]
- Hellings, P.W.; Klimek, L.; Cingi, C.; Agache, I.; Akdis, C.; Bachert, C.; Bousquet, J.; Demoly, P.; Gevaert, P.; Hox, V.; et al. Non-allergic rhinitis: Position paper of the European Academy of Allergy and Clinical Immunology. Allergy 2017, 72, 1657–1665. [Google Scholar] [CrossRef] [Green Version]
- Heinzerling, L.; Mari, A.; Bergmann, K.-C.; Bresciani, M.; Burbach, G.; Darsow, U.; Durham, S.; Fokkens, W.; Gjomarkaj, M.; Haahtela, T.; et al. The skin prick test–European standards. Clin. Transl. Allergy 2013, 3, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hankinson, J.L.; Odencrantz, J.R.; Fedan, K.B. Spirometric reference values from a sample of the general US population. Am. J. Respir. Crit. Care Med. 1999, 159, 179–187. [Google Scholar] [CrossRef] [Green Version]
- Nielsen, K.G.; Bisgaard, H. Hyperventilation with cold versus dry air in 2-to 5-year-old children with asthma. Am. J. Respir. Crit. Care Med. 2005, 171, 238–241. [Google Scholar] [CrossRef] [Green Version]
- Modl, M.; Eber, E.; Steinbrugger, B.; Weinhandl, E.; Zach, M.S. Comparing methods for assessing bronchial responsiveness in children: Single step cold air challenge, multiple step cold air challenge, and histamine provocation. Eur. Respir. J. 1995, 8, 1742–1747. [Google Scholar] [CrossRef] [Green Version]
- Steinbrugger, B.; Eber, E.; Modl, M.; Weinhandl, E.; Zach, M.S. A comparison of a single-step cold-dry air challenge and a routine histamine provocation for the assessment of bronchial responsiveness in children and adolescents. Chest 1995, 108, 741–745. [Google Scholar] [CrossRef]
- Zach, M.; Polgar, G.; Kump, H.; Kroisel, P. Cold air challenge of airway hyperreactivity in children: Practical application and theoretical aspects. Pediatr. Res. 1984, 18, 469–478. [Google Scholar] [CrossRef] [Green Version]
- Zach, M.S.; Polgar, G. Cold air challenge of airway hyperreactivity in children: Dose-response interrelation with a reaction plateau. J. Allergy Clin. Immunol. 1987, 80, 9–17. [Google Scholar] [CrossRef]
- Steinbacher, M.; Pfleger, A.; Schwantzer, G.; Jauk, S.; Weinhandl, E.; Eber, E. Small airway function before and after cold dry air challenge in pediatric asthma patients during remission. Pediatr. Pulmonol. 2017, 52, 873–879. [Google Scholar] [CrossRef]
- Piss, L.; Ingenito, E.P.; Ingram, R.; Pichurko, B. Assessment of bronchoalveolar cell and mediator response to isocapnic hyperpnea in asthma. Am. Rev. Respir. Dis. 1990, 142, 73–78. [Google Scholar] [CrossRef]
- Hallstrand, T.S.; Leuppi, J.D.; Joos, G.; Hall, G.L.; Carlsen, K.-H.; Kaminsky, D.A.; Coates, A.L.; Cockcroft, D.W.; Culver, B.H.; Diamant, Z. ERS technical standard on bronchial challenge testing: Pathophysiology and methodology of indirect airway challenge testing. Eur. Respir. J. 2018, 52, 1801033. [Google Scholar] [CrossRef] [Green Version]
- Anderson, S.D.; Smith, C.M. Osmotic Challenges in the Assessment of Bronchial Hyperrespcnelveness’. Am. Rev. Respir. Dis. 1991, 991, 543–546. [Google Scholar]
- Aquilina, A.T. Comparison of airway reactivity induced by histamine, methacholine, and isocapnic hyperventilation in normal and asthmatic subjects. Thorax 1983, 38, 766–770. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.H.; Jang, T.Y. Usefulness of the subjective cold hyperresponsiveness scale as evaluated by cold dry air provocation. Am. J. Rhinol. Allergy 2012, 26, 45–48. [Google Scholar] [CrossRef]
- Joos, G.F.; O’Connor, B.; Anderson, S.D.; Chung, F.; Cockcroft, D.W.; Dahlén, B.; DiMaria, G.; Foresi, A.; Hargreave, F.E.; Holgate, S.T.; et al. Indirect airway challenges. Eur. Respir. J. 2003, 21, 1050–1068. [Google Scholar] [CrossRef] [Green Version]
- Nair, N.; Hopp, R.; Alper, B.; Bewtra, A.K.; Townley, R.G. Correlation of methacholine-induced non-specific bronchial reactivity and cold air hyperventilation challenge. Ann. Allergy 1986, 56, 226–228. [Google Scholar] [PubMed]
- Filuk, R.B.; Serrette, C.; Anthonisen, N.R. Comparison of responses to methacholine and cold air in patients suspected of having asthma. Chest 1989, 95, 948–952. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anderson, S.; Argyros, G.; Magnussen, H.; Holzer, K. Provocation by eucapnic voluntary hyperpnoea to identify exercise induced bronchoconstriction. Br. J. Sports Med. 2001, 35, 344–347. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dreßler, M.; Friedrich, T.; Lasowski, N.; Herrmann, E.; Zielen, S.; Schulze, J. Predictors and reproducibility of exercise-induced bronchoconstriction in cold air. BMC Pulm. Med. 2019, 19, 94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tordera, M.P.; Río, F.G.; Gutierrez, F.J.Ã.; Serrano, C.C.; Torrero, L.C.; Costa, L.M.E.; Moreno, C.M.; Nieto, M.J.R.; Fernández, A.T.; Of Pulmonology, S.S. Guidelines for the study of nonspecific bronchial hyperresponsiveness in asthma. Spanish Society of Pulmonology and Thoracic Surgery (SEPAR). Arch. Bronconeumol. 2013, 49, 432–446. [Google Scholar] [CrossRef]
- Sterck, P.; Fabbri, L.; Quanjer, P.; Cockcroft, D.; O’byrne, P.; Anderson, S.; Juniper, E.; Malo, J. Airway responsiveness. Standardized challenge testing with pharmalogical, physical and sensitizing stimuli in adults. Eur. Respir. J. 1993, 6, 53–83. [Google Scholar] [CrossRef] [Green Version]
- Cockcroft, D.W. Direct challenge tests: Airway hyperresponsiveness in asthma: Its measurement and clinical significance. Chest 2010, 138, 18S–24S. [Google Scholar] [CrossRef] [Green Version]
- Kim, C.W. Bronchial asthma with negative methacholine challenge test. Korean J. Asthma Allergy Clin. Immunol. 2012, 32, 150–151. [Google Scholar]
- Holzer, K.; Anderson, S.D.; Douglass, J. Exercise in elite summer athletes: Challenges for diagnosis. J. Allergy Clin. Immunol. 2002, 110, 374–380. [Google Scholar] [CrossRef]
- Ban, G.Y.; Park, H.L.; Hwang, E.K.; Ye, Y.M.; Shin, Y.S.; Nahm, D.H.; Park, H.S. Clinical characteristics of asthmatics having negative results to methacholine bronchial challenge test. Korean J. Asthma Allergy Clin. Immunol. 2012, 32, 152–158. [Google Scholar]
- Aldes-Sebaldt, M.; Mclaughlin, F.; Levison, H. Comparison of cold air, ultrasonic mist, and methacholine inhalations as tests of bronchial reactivity in normal and asthmatic children. J. Pediatr. 1985, 107, 526–530. [Google Scholar] [CrossRef]
| BA | Others | Total | |
|---|---|---|---|
| Numbers | 51 | 21 | 72 |
| Sex (male) | 37 | 10 | 47 (65.3%) |
| Age (years) | 8.78 ± 2.72 | 9.90 ± 3.12 | 9.11 ± 2.87 |
| Height (cm) | 133.51 ± 15.39 | 138.84 ± 16.07 | 135.07 ± 15.67 |
| Weight (kg) | 35.79 ± 15.26 | 39.92 ± 14.40 | 36.99 ± 15.03 |
| Cough | 36 | 12 | 48 (66.7%) |
| Dyspnea | 22 | 7 | 29 (40.3%) |
| Cough on exercise | 8 | 3 | 11 (15.3%) |
| Dyspnea on exercise | 10 | 5 | 15 (20.8%) |
| Symptoms to cold air | 19 | 6 | 25 (34.7%) |
| History of rhinitis | 36 | 11 | 47 (65.3%) |
| History of atopic dermatitis | 16 | 9 | 25 (34.7%) |
| History of food allergy | 14 | 4 | 18 (25%) |
| Exposure to smoking | 12 | 3 | 15 (20.8%) |
| Family history of asthma | 3 | 1 | 4 (5.6%) |
| Family history of allergy | 24 | 6 | 30 (41.7%) |
| Atopy | 43 | 15 | 58 (81.7%) |
| BA | Others | p | |
|---|---|---|---|
| Numbers | 51 | 21 | |
| Sputum eosinophil (%) | 5.87 ± 12.1 | 1.27 ± 1.03 | 0.014 |
| Eosinophils (/mm3) | 511.02 ± 361.89 | 331.25 ± 426.17 | 0.143 |
| ECP (μg/L) | 44.39 ± 40.17 | 19.58 ± 15.15 | 0.001 |
| Total IgE (IU/mL) | 684.03 ± 841.04 | 438.91 ± 651.82 | 0.256 |
| Vitamin D (ng/mL) | 25.64 ± 7.17 | 27.38 ± 12.01 | 0.872 |
| Numbers of positive skin prick test | 5.7 ± 4.54 | 4.58 ± 3.75 | 0.302 |
| FVC (%) | 104.53 ± 13.88 | 101.29 ± 10.15 | 0.336 |
| FEV1 (%) | 94.20 ± 17.17 | 97.14 ± 10.38 | 0.467 |
| FEV1/FVC | 78.24 ± 7.02 | 84.43 ± 3.28 | <0.001 |
| FEF25-75 (%) | 81.06 ± 29.24 | 94.67 ± 22.39 | 0.060 |
| PC20 (mg/mL) | 2.94 ± 3.80 | 19.29 ± 2.08 | <0.001 |
| p | |
|---|---|
| Age | 0.885 |
| Height | 0.835 |
| Weight | 0.829 |
| BMI | 0.607 |
| Cough | 0.504 |
| Dyspnea | 0.530 |
| Dyspnea on exercise | 0.961 |
| Symptoms to cold air | 0.622 |
| History of atopic dermatitis | 0.521 |
| History of food allergy | 0.633 |
| Exposure to smoking | 0.744 |
| Family history of asthma | 0.936 |
| Family history of allergy | 0.812 |
| Atopy | 0.521 |
| Sputum eosinophil | 0.020 |
| Eosinophils | 0.353 |
| ECP | 0.085 |
| Total IgE | 0.890 |
| Positivity of specific IgE | 0.587 |
| Positivity of skin prick test | 0.525 |
| Positive numbers in skin prick test | 0.650 |
| FVC | 0.204 |
| FEV1 | 0.168 |
| FEV1/FVC | 0.735 |
| FEF25-75 | 0.447 |
| PC20 | 0.188 |
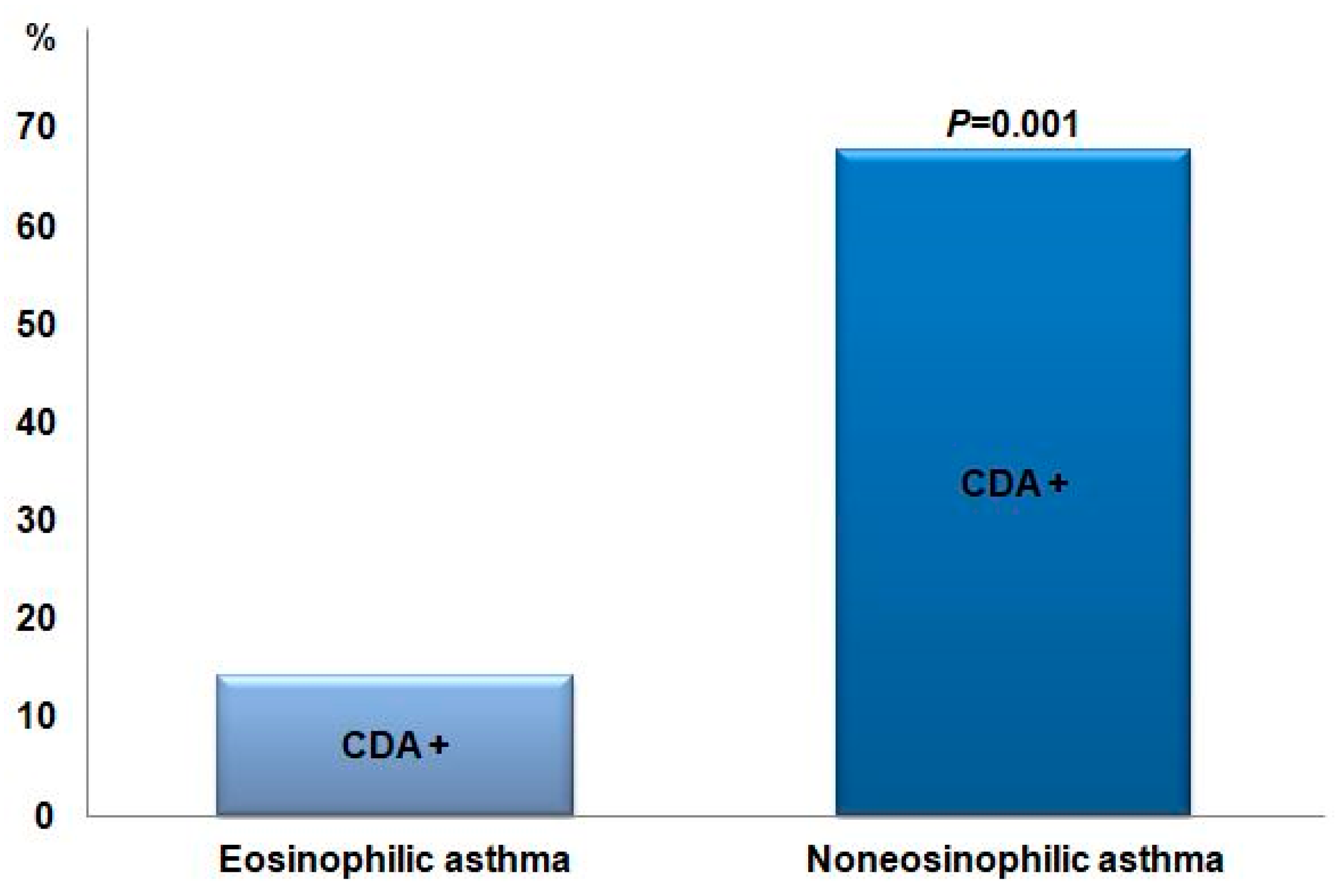
| CDA Positive | CDA Negative | p | |
|---|---|---|---|
| Eosinophilic BA | 2 | 12 | |
| Non-eosinophilic BA | 25 | 12 | 0.001 |
| Classic BA | 21 | 16 | |
| Cough-variant BA | 6 | 8 | 0.375 |
| Cough | 21 | 15 | 0.232 |
| Dyspnea | 12 | 10 | 0.842 |
| Cough on exercise | 2 | 6 | 0.085 |
| Dyspnea on exercise | 3 | 7 | 0.105 |
| Symptoms to cold air | 10 | 9 | 0.686 |
| Sputum eosinophil (%) | 1.6 | 10.1 | 0.019 |
| Eosinophils (/mm3) | 457.2 | 567.1 | 0.293 |
| ECP (μg/L) | 34.3 | 57.4 | 0.047 |
| Total IgE (IU/mL) | 26.0 | 25.3 | 0.704 |
| BA with Rhinitis | BA Only | p | |
|---|---|---|---|
| Numbers | 33 | 18 | |
| Age (years) | 9.24 ± 3.06 | 7.94 ± 1.73 | 0.059 |
| Height (cm) | 137.22 ± 16.68 | 126.73 ± 9.87 | 0.018 |
| Weight (kg) | 38.45 ± 17.39 | 30.92 ± 8.73 | 0.045 |
| Sputum eosinophil (%) | 5.90 ± 10.73 | 5.81 ± 14.70 | 0.982 |
| Eosinophils (/mm3) | 517.19 ± 342.74 | 499.41 ± 406.30 | 0.872 |
| ECP (μg/L) | 40.54 ± 40.42 | 52.09 ± 39.81 | 0.353 |
| Total IgE (IU/mL) | 666.01 ± 795.29 | 716.07 ± 940.09 | 0.842 |
| Numbers of positive skin prick test | 5.53 ± 4.03 | 6.0 ± 5.44 | 0.730 |
| FVC (%) | 102.94 ± 15.82 | 107.44 ± 9.01 | 0.272 |
| FEV1 (%) | 92.18 ± 19.51 | 97.89 ± 11.35 | 0.261 |
| FEV1/FVC | 77.53 ± 6.77 | 79.54 ± 7.45 | 0.331 |
| FEF25-75 (%) | 76.18 ± 27.65 | 90.0 ± 30.74 | 0.107 |
| PC20 (mg/mL) | 2.50 ± 3.23 | 3.74 ± 4.68 | 0.302 |
| Positive CDA | 19 (57.6%) | 8 (44.4%) | 0.379 |
| PT10 (min) | 8.34 ± 3.36 | 8.54 ± 2.12 | 0.916 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahn, J.Y.; Choi, B.S. Application of a Cold Dry Air Provocation Test in Pediatric Patients with Asthma. Children 2022, 9, 920. https://doi.org/10.3390/children9060920
Ahn JY, Choi BS. Application of a Cold Dry Air Provocation Test in Pediatric Patients with Asthma. Children. 2022; 9(6):920. https://doi.org/10.3390/children9060920
Chicago/Turabian StyleAhn, Ji Young, and Bong Seok Choi. 2022. "Application of a Cold Dry Air Provocation Test in Pediatric Patients with Asthma" Children 9, no. 6: 920. https://doi.org/10.3390/children9060920
APA StyleAhn, J. Y., & Choi, B. S. (2022). Application of a Cold Dry Air Provocation Test in Pediatric Patients with Asthma. Children, 9(6), 920. https://doi.org/10.3390/children9060920






