Parent-Reported Perceived Cognitive Functioning Identifies Cognitive Problems in Children Who Survived Neonatal Critical Illness
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Data Collection
2.3. Measures
2.4. Data Analyses
- Cohen’s d (= mean–population mean/sample SD): small = 0.2, medium = 0.5, large = 0.8.
- r (= standardized test statistic/√N): small = 0.1, medium = 0.3, large = 0.5.
- Cohen’s f (= (√η2/1 − η2)): small = 0.1, medium = 0.25, large = 0.4.
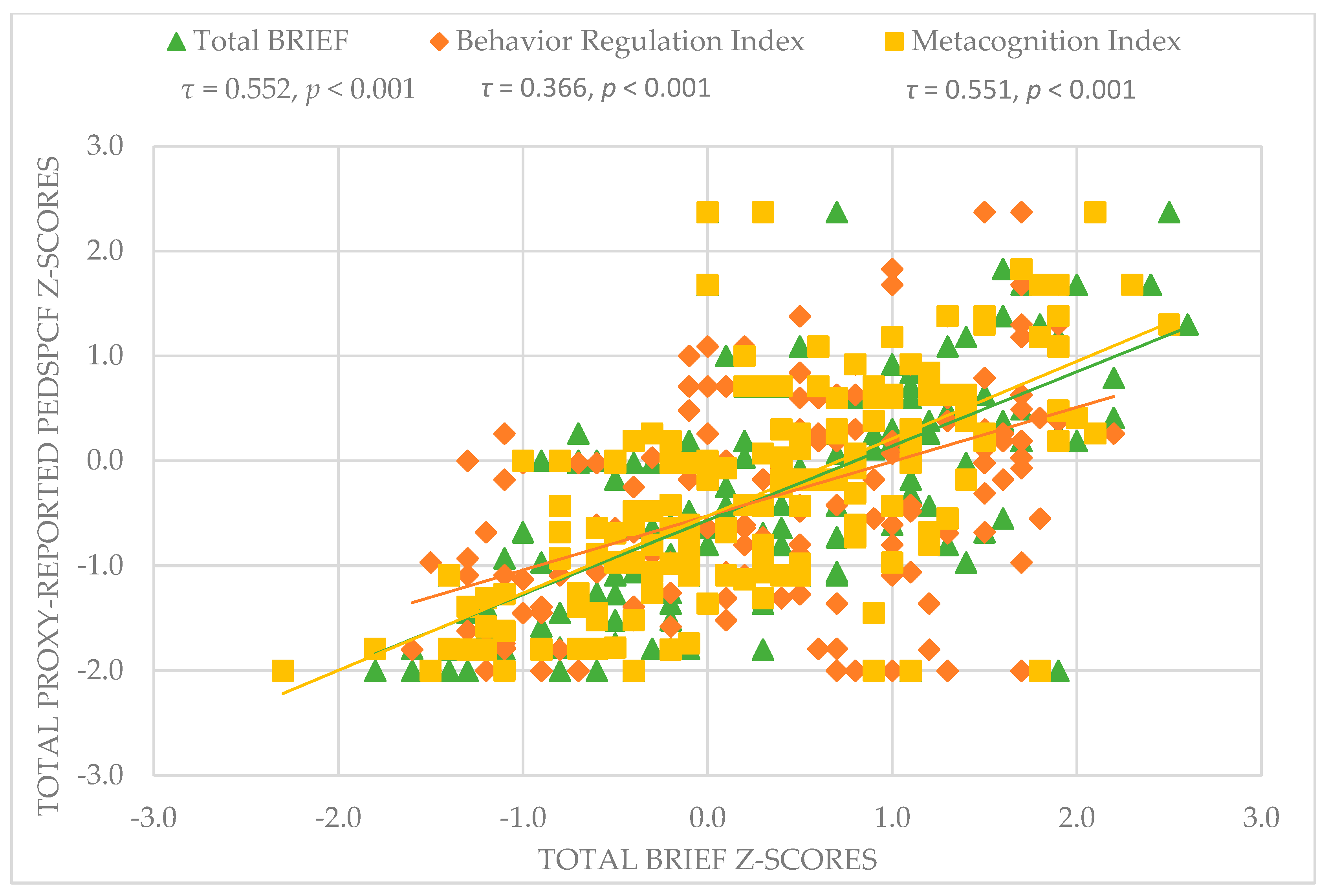
- Strengths of the Kendall tau correlation coefficients were interpreted as followed [35]: τ: weak = 0.1, moderate = 0.4, strong = 0.7.
3. Results
3.1. Participants
3.2. Questionnaire Outcomes
3.3. Associations of PedsPCF with BRIEF, Outcomes of NPA, and School Functioning
3.4. Associations of 30- and 10-Item PedsPCF
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Glinianaia, S.V.; Morris, J.K.; Best, K.E.; Santoro, M.; Coi, A.; Armaroli, A.; Rankin, J. Long-term survival of children born with congenital anomalies: A systematic review and meta-analysis of population-based studies. PLoS Med. 2020, 17, e1003356. [Google Scholar] [CrossRef] [PubMed]
- UK collaborative randomised trial of neonatal extracorporeal membrane oxygenation. UK Collaborative ECMO Trail Group. Lancet 1996, 348, 75–82. [CrossRef]
- Harmsen, W.J.; Aarsen, F.J.; Zijp, M.H.M.va.; van Rosmalen, J.M.; Wijnen, R.M.H.; Tibboel, D.; IJsselstijn, H. Developmental problems in patients with oesophageal atresia: A longitudinal follow-up study. Arch. Dis. Child. Fetal Neonatal Ed. 2017, 102, F214–F219. [Google Scholar] [CrossRef] [PubMed]
- Leeuwen, L.; Schiller, R.M.; Rietman, A.B.; van Rosmalen, J.; Wildschut, E.D.; Houmes, R.J.M.; Tibboel, D.; IJsselstijn, H. Risk Factors of Impaired Neuropsychologic Outcome in School-Aged Survivors of Neonatal Critical Illness. Crit. Care Med. 2018, 46, 401–410. [Google Scholar] [CrossRef] [PubMed]
- Madderom, M.J.; Reuser, J.J.; Utens, E.M.; van Rosmalen, J.; Raets, M.; Govaert, P.; Steiner, K.; Gischler, S.J.; Tibboel, D.; van Heijst, A.F.J.; et al. Neurodevelopmental, educational and behavioral outcome at 8 years after neonatal ECMO: A nationwide multicenter study. Intensive Care Med. 2013, 39, 1584–1593. [Google Scholar] [CrossRef]
- Madderom, M.J.; Schiller, R.M.; Gischler, S.J.; van Heijst, A.F.; Tibboel, D.; Aarsen, F.K.; IJsselstijn, H. Growing Up After Critical Illness: Verbal, Visual-Spatial, and Working Memory Problems in Neonatal Extracorporeal Membrane Oxygenation Survivors. Crit. Care Med. 2016, 44, 1182–1190. [Google Scholar] [CrossRef]
- Madderom, M.J.; Toussaint, L.; Zijp, M.H.M.v.-d.C.-v.; Gischler, S.J.; Wijnen, R.M.; Tibboel, D.; IJsselstijn, H. Congenital diaphragmatic hernia with(out) ECMO: Impaired development at 8 years. Arch. Dis. Child. Fetal Neonatal Ed. 2013, 98, F316–F322. [Google Scholar] [CrossRef]
- Mazer, P.; Gischler, S.J.; Zijp, M.H.M.V.D.C.-V.; Tibboel, D.; Bax, N.M.; IJsselstijn, H.; Dijk, M.V.A.N.; Duivenvoorden, H.J. Early developmental assessment of children with major non-cardiac congenital anomalies predicts development at the age of 5 years. Dev. Med. Child Neurol. 2010, 52, 1154–1159. [Google Scholar] [CrossRef]
- Schiller, R.M.; Madderom, M.J.; Reuser, J.J.; Steiner, K.; Gischler, S.J.; Tibboel, D.; van Heijst, A.F.J.; IJsselstijn, H. Neuropsychological Follow-up After Neonatal ECMO. Pediatrics 2016, 138, e20161313. [Google Scholar] [CrossRef] [PubMed]
- Schiller, R.; IJsselstijn, H.; Hoskote, A.; White, T.; Verhulst, F.; van Heijst, A.; Tibboel, D. Memory deficits following neonatal critical illness: A common neurodevelopmental pathway. Lancet Child Adolesc. Health 2018, 2, 281–289. [Google Scholar] [CrossRef]
- Gischler, S.J.; Mazer, P.; Duivenvoorden, H.J.; van Dijk, M.; Bax, N.M.; Hazebroek, F.W.; Tibboel, D. Interdisciplinary structural follow-up of surgical newborns: A prospective evaluation. J. Pediatr. Surg. 2009, 44, 1382–1389. [Google Scholar] [CrossRef] [PubMed]
- IJsselstijn, H.; Gischler, S.J.; Wijnen, R.M.H.; Tibboel, D. Assessment and significance of long-term outcomes in pediatric surgery. Semin. Pediatr. Surg. 2017, 26, 281–285. [Google Scholar] [CrossRef]
- IJsselstijn, H.; Gischler, S.J.; Toussaint, L.; Spoel, M.; Zijp, M.H.; Tibboel, D. Growth and development after oesophageal atresia surgery: Need for long-term multidisciplinary follow-up. Paediatr. Respir. Rev. 2016, 19, 34–38. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sreeram, I.I.; Ten Kate, C.A.; van Rosmalen, J.; Schnater, J.M.; Gischler, S.J.; Wijnen, R.M.H.; IJsselstijn, H.; Rietman, A.B. Patient-Reported Outcome Measures and Clinical Outcomes in Children with Foregut Anomalies. Children 2021, 8, 587. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.S.; Butt, Z.; Zelko, F.; Cella, D.; Krull, K.R.; Kieran, M.W.; Goldman, S. Development of a parent-report cognitive function item bank using item response theory and exploration of its clinical utility in computerized adaptive testing. J. Pediatr. Psychol. 2011, 36, 766–779. [Google Scholar] [CrossRef]
- Lai, J.S.; Zelko, F.; Butt, Z.; Cella, D.; Kieran, M.W.; Krull, K.R.; Magasi, S.; Goldman, S. Parent-perceived child cognitive function: Results from a sample drawn from the US general population. Childs Nerv. Syst. 2011, 27, 285–293. [Google Scholar] [CrossRef]
- Marchal, J.P.; de Vries, M.; Conijn, J.; Rietman, A.B.; IJsselstijn, H.; Tibboel, D.; Haverman, L.; Maurice-Stam, H.; Oostrom, K.J.; Grootenhuis, M.A. Pediatric Perceived Cognitive Functioning: Psychometric Properties and Normative Data of the Dutch Item Bank and Short Form. J. Int. Neuropsychol. Soc. 2019, 25, 845–856. [Google Scholar] [CrossRef]
- Hijkoop, A.; Rietman, A.B.; Wijnen, R.M.H.; Tibboel, D.; Cohen-Overbeek, T.E.; van Rosmalen, J.; IJsselstijn, H. Omphalocele at school age: What do parents report? A call for long-term follow-up of complex omphalocele patients. Early Hum. Dev. 2019, 137, 104830. [Google Scholar] [CrossRef] [PubMed]
- Hijkoop, A.; Rietman, A.B.; Wijnen, R.M.H.; Tibboel, D.; Cohen-Overbeek, T.E.; van Rosmalen, J.; IJsselstijn, H. Gastroschisis at school age: What do parents report? Eur. J. Pediatr. 2019, 178, 1405–1412. [Google Scholar] [CrossRef]
- Lai, J.S.; Bregman, C.; Zelko, F.; Nowinski, C.; Cella, D.; Beaumont, J.J.; Goldman, S. Parent-reported cognitive function is associated with leukoencephalopathy in children with brain tumors. Qual. Life Res. 2017, 26, 2541–2550. [Google Scholar] [CrossRef]
- Ohnemus, D.; Neighbors, K.; Sorensen, L.G.; Lai, J.S.; Alonso, E.M. A Pilot Study of a Screening Tool for Pediatric Minimal Hepatic Encephalopathy. J. Pediatr. Gastroenterol. Nutr. 2019, 69, 655–661. [Google Scholar] [CrossRef] [PubMed]
- Gioia, G.A.; Isquith, P.K.; Guy, S.C.; Kenworthy, L. Behavior Rating Inventory of Executive Function BRIEF: Professional Manual; Psychological Assessment Resources(PAR): Lutz, FL, USA, 2000. [Google Scholar]
- Smidts, D.P.; Huizinga, M. BRIEF Behavior Rating Inventory of Executive Function-Manual 2. Norms (Dutch: Executieve Functies Gedragsvragenlijsten: Handleiding), 4-23; Hogrefe: Amsterdam, The Netherlands, 2009. [Google Scholar]
- Kort, W.; Schittekatte, M.; Dekker, P.H.; Verhaeghe, P.; Compaan, E.L.; Bosmans, M.; Vermeir, G. WISC-III NL Wechsler Intelligence Scale for Children. Handleiding en Verantwoording [Dutch version of the WISC-III], 3rd ed.; Harcourt Test Publishers/Nederlands Instituut voor Psychologen: Amsterdam, The Netherlands, 2005. [Google Scholar]
- Pearson. WAIS-IV-NL, Nederlandstalige berwerking. In Technische Handleiding; Pearson Assessment & Information: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Pearson. WAIS-IV-NL, Nederlandstalige bewerking. In Afname En Scoringshandleiding; Pearson Assessment & Information: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Emslie, H.; WIlson, F.C.; Burden, V. Behavioral Assessment of the Dysexecutive Syndrome for Children (BADS-C), Dutch Version; Amsterdam Harcourt: Amsterdam, The Netherlands, 2006. [Google Scholar]
- Lezak, M.D.; Howieson, D.B.; Loring, D.W. Neuropsychological Assessment, 4th ed; Oxford University Press: Oxford, UK, 2004. [Google Scholar]
- Schmand, B.; Houx, P.; De Koning, I. Dutch Norms for STROOP Color-Word Test, Trail Making Test, Rey Auditory Verbal-Learning Test, Verbal Fluency, and Story Recall of Rivermead Behavioural Memory Test; Division Neuropsychology of the Dutch Institute for Psychology: Amsterdam, The Netherlands, 2003. [Google Scholar]
- van den Burg, W.; Kingma, A. Performance of 225 Dutch school children on Rey’s Auditory Verbal Learning Test (AVLT): Parallel test-retest reliabilities with an interval of 3 months and normative data. Arch. Clin. Neuropsychol. 1999, 14, 545–559. [Google Scholar] [PubMed]
- Vos, P. Bourdon-Vos. Handleiding (Manual Dot Cancellation Test); Swets en Zeitlinger: Lisse, The Netherlands, 1992. [Google Scholar]
- Watanabe, K.; Ogino, T.; Nakano, K.; Hattori, J.; Kado, Y.; Sanada, S.; Ohtsuka, Y. The Rey-Osterrieth Complex Figure as a measure of executive function in childhood. Brain Dev. 2005, 27, 564–569. [Google Scholar] [CrossRef] [PubMed]
- Wechsler, D.; Naglieri, J.A. Wechsler Nonverbal Scale of Ability; Pearson: San Antonio, TX, USA, 2006. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed; Lawrence Erlbaum Associates: New York, NY, USA, 1988. [Google Scholar]
- Akoglu, H. User’s guide to correlation coefficients. Turk J. Emerg. Med. 2018, 18, 91–93. [Google Scholar] [CrossRef]
- Goyal, S.; Park, A.; Zeglam, A.; Brown, H.; Pemberton, J.D. Choroidal Ganglioneuroma and Orbital Plexiform Neurofibroma Presenting as Buphthalmos in an Infant With Neurofibromatosis Type 1. Ophthalmic. Plast Reconstr. Surg. 2016, 32, e87–e89. [Google Scholar] [CrossRef] [PubMed]
- White, S.; Marquez de Prado, B.; Russo, A.F.; Hammond, D.L. Heat hyperalgesia and mechanical hypersensitivity induced by calcitonin gene-related peptide in a mouse model of neurofibromatosis. PLoS ONE 2014, 9, e106767. [Google Scholar]
- Petrie, A.; Sabin, C. Medical Statistics at a Glance, 3rd ed; Wiley-Blackwell: Oxford, UK, 2009. [Google Scholar]
- Bone, M.F.; Feinglass, J.M.; Goodman, D.M. Risk factors for acquiring functional and cognitive disabilities during admission to a PICU*. Pediatr. Crit. Care Med. 2014, 15, 640–648. [Google Scholar] [CrossRef] [PubMed]
- Heath, N.L.; Glen, T. Positive illusory bias and the self-protective hypothesis in children with learning disabilities. J. Clin. Child Adolesc. Psychol. 2005, 34, 272–281. [Google Scholar] [CrossRef] [PubMed]
- IJsselstijn, H.; Breatnach, C.; Hoskote, A.; Greenough, A.; Patel, N.; Capolupo, I.; Morini, F.; Scharbatke, H.; Kipfmueller, F.; Ertresvag, K.; et al. Defining outcomes following congenital diaphragmatic hernia using standardised clinical assessment and management plan (SCAMP) methodology within the CDH EURO consortium. Pediatr. Res. 2018, 84, 181–189. [Google Scholar] [CrossRef]

| Demographic Characteristics | |
| Sex | |
| Male | 99 (59%) |
| Female | 69 (41%) |
| Clinical characteristics | |
| Diagnosis | |
| CDH | 57 (34%) |
| without ECMO treatment | 46 (81%) |
| with ECMO treatment | 11 (19%) |
| EA | 54 (32%) |
| CLM | 20 (12%) |
| Neonatal ECMO, non-CDH | 37 (22%) |
| Gestational age (weeks) | 39.0 (37.1–40.4) |
| Birth weight (grams) | 3150 (2725–3530) |
| Duration of initial hospital stay (days) | 22 (13–48) |
| Duration of initial ventilation (days) | 7 (2–16) |
| At follow-up | |
| Age at assessment | |
| 8 years | 57 (34%) |
| 12 years | 64 (38%) |
| 17 years | 47 (28%) |
| School functioning | |
| Regular | 130 (78%) |
| Regular with help | 22 (13%) |
| Special educational needs | 14 (8%) |
| Missing | 2 (1%) |
| Measurement | Mean (SD) | p-Value | Effect Size (d/r) | |
|---|---|---|---|---|
| Self-reported | PedsPCF 30-item | −0.35 (0.88) | <0.001 | 0.40 1 |
| Proxy-reported | PedsPCF 30-item | −0.36 (1.06) | <0.001 | 0.33 1 |
| Total BRIEF | 0.33 (0.98) | <0.001 | 0.34 2 | |
| BRI | 0.37 (0.97) | <0.001 | 0.35 1 | |
| MCI | 0.26 (0.96) | 0.001 | 0.27 2 |
| Variable | Mean (SD) | p-Value | Effect Size (d/r) | |
|---|---|---|---|---|
| Intelligence | Total IQ | 100 (18) | 0.951 | 0.00 2 |
| Attention | TMTA t | 0.30 (1.15) | <0.001 *** | 0.37 1 |
| Stroop IF | −0.23 (1.19) | 0.051 | 0.16 1 | |
| DCT-ST | −0.93 (1.28) | <0.001 *** | 0.60 1 | |
| DCT-SD | −1.17 (1.52) | <0.001 *** | 0.60 1 | |
| Verbal Memory | Total Digit Span | 0.04 (1.00) | 0.565 | 0.04 1 |
| RAVLT total | −0.35 (1.26) | <0.001 *** | 0.28 2 | |
| RAVLT recall | −0.64 (1.38) | <0.001 *** | 0.40 1 | |
| Visuospatial Memory | WNV-SS total | −0.21 (0.92) | 0.004 ** | 0.23 2 |
| WNV-SS forward | −0.07 (1.04) | 0.298 | 0.08 1 | |
| RCFT immediate | −0.62 (1.23) | <0.001 *** | 0.42 1 | |
| RCFT delayed | −0.76 (1.26) | <0.001 *** | 0.51 1 | |
| RCFT recognition | −0.08 (1.21) | 0.933 | 0.01 1 | |
| Executive Functioning | BADS-C Key Search | 0.18 (1.10) | 0.052 | 0.15 1 |
| BADS-C Modified Six Elements | −0.48 (0.81) | <0.001 *** | 0.50 1 | |
| TMTB t | 0.09 (1.08) | 0.013 * | 0.20 1 | |
| WNV-SS backwards | −0.29 (0.86) | <0.001 *** | 0.35 1 | |
| PSI | −0.04 (1.13) | 0.620 | 0.04 2 |
| Variable | Cases (n) | B (SE) | 95% CI of B | R2 | p-Value | |
|---|---|---|---|---|---|---|
| Intelligence | WISC-III-NL Total IQ | 158 | 0.022 (0.004) | 0.013–0.031 | 0.141 | <0.001 *** |
| Attention | TMTA t | 155 | 0.223 (0.071) | 0.082–0.364 | 0.060 | 0.002 ** |
| Stroop IF | 149 | 0.067 (0.074) | −0.079–0.213 | 0.006 | 0.365 | |
| DCT-ST | 151 | 0.139 (0.066) | 0.009–0.269 | 0.029 | 0.036 * | |
| DCT-SD | 151 | 0.106 (0.056) | −0.004–0.271 | 0.024 | 0.059 | |
| Verbal Memory | WISC-III-NL Total Digit Span | 157 | 0.255 (0.083) | 0.090–0.419 | 0.057 | 0.003 ** |
| RAVLT total | 158 | 0.231 (0.065) | 0.103–0.359 | 0.075 | <0.001 *** | |
| RAVLT recall | 158 | 0.188 (0.060) | 0.070–0.305 | 0.060 | 0.002 ** | |
| Visuospatial Memory | WNV-SS total | 155 | 0.266 (0.091) | 0.085–0.446 | 0.052 | 0.004 ** |
| WNV-SS forwards | 155 | 0.159 (0.082) | −0.003–0.322 | 0.024 | 0.055 | |
| RCFT immediate | 155 | 0.191 (0.067) | 0.059–0.323 | 0.051 | 0.005 ** | |
| RCFT delayed | 155 | 0.191 (0.066) | 0.061–0.321 | 0.052 | 0.004 ** | |
| RCFT recognition | 156 | 0.164 (0.071) | 0.024–0.304 | 0.034 | 0.022 * | |
| Executive Functioning | BADS-C Key Search | 155 | 0.208 (0.076) | 0.058–0.358 | 0.047 | 0.007 ** |
| BADS-C Modified Six Elements | 88 **** | 0.083 (0.144) | −0.202–0.369 | 0.004 | 0.563 | |
| TMTB t | 147 | 0.236 (0.083) | 0.071–0.400 | 0.052 | 0.005 ** | |
| WNV-SS backwards | 155 | 0.275 (0.097) | 0.082–0.467 | 0.049 | 0.005 ** | |
| Processing Speed Index | 158 | 0.319 (0.069) | 0.183–0.456 | 0.120 | <0.001 *** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ilik, Y.; IJsselstijn, H.; Gischler, S.J.; van Gils-Frijters, A.; Schnater, J.M.; Rietman, A.B. Parent-Reported Perceived Cognitive Functioning Identifies Cognitive Problems in Children Who Survived Neonatal Critical Illness. Children 2022, 9, 900. https://doi.org/10.3390/children9060900
Ilik Y, IJsselstijn H, Gischler SJ, van Gils-Frijters A, Schnater JM, Rietman AB. Parent-Reported Perceived Cognitive Functioning Identifies Cognitive Problems in Children Who Survived Neonatal Critical Illness. Children. 2022; 9(6):900. https://doi.org/10.3390/children9060900
Chicago/Turabian StyleIlik, Yerel, Hanneke IJsselstijn, Saskia J. Gischler, Annabel van Gils-Frijters, Johannes M. Schnater, and Andre B. Rietman. 2022. "Parent-Reported Perceived Cognitive Functioning Identifies Cognitive Problems in Children Who Survived Neonatal Critical Illness" Children 9, no. 6: 900. https://doi.org/10.3390/children9060900
APA StyleIlik, Y., IJsselstijn, H., Gischler, S. J., van Gils-Frijters, A., Schnater, J. M., & Rietman, A. B. (2022). Parent-Reported Perceived Cognitive Functioning Identifies Cognitive Problems in Children Who Survived Neonatal Critical Illness. Children, 9(6), 900. https://doi.org/10.3390/children9060900






