1. Introduction
The Italian Government introduced severe restrictive measures (“lockdown”) against COVID-19 on the entire national territory between 9 March 2020 and 3 May 2020 [
1,
2,
3,
4]. These measures slowed the diffusion of the viral infection, but resulted in relevant social and economic costs in several sectors including the medical assistance of non-COVID-19 diseases [
4]. Many medical visits, diagnostic workups, and follow-up evaluations were suspended because all of the resources of the Health National System were addressed toward the management of the COVID-19 emergency [
4].
The direct consequences of COVID-19 on pediatric patients suffering from chronic neurological or neurodevelopmental diseases involved a minor number of patients while the psychological impacts resulting from the social limitations and damage resulting from the reduction in medical and rehabilitative follow-up were probably higher [
5,
6,
7]. Comparable negative consequences on the children’s well-being were also caused by the increased risk of experiencing stress and negative emotions in the parents [
8].
Table 1 summarizes the few available studies including five cross-sectional surveys on the social and health care nodes and the caregivers’ stress in the field of pediatric neurology since the onset of the pandemic.
The present study aimed to analyze the impact of COVID 19-related lockdown on the parental perceived stress and, subsequently, on the health and the care of children with chronic neurological and neurodevelopmental diseases through a parental self-reporting survey about the consequences of the interruption of in-presence school, medical periodical follow-up, and rehabilitation services. These descriptors were judged to represent the main negative social and clinical changes in the daily life of families of children with neurological diseases.
2. Patients and Methods
The parents of patients with chronic neurological or neurodevelopmental disorders followed at the Unit of Child Neurology and Psychiatry of “Azienda Ospedaliera Universitaria Umberto I Hospital-Sapienza Università di Roma” in Rome (Italy), the Unit of Child Neurology and Psychiatry and the Unit of Rare Diseases of the “Burlo Garofalo” pediatric Hospital in Trieste (Italy) were considered as eligible for the study.
Participation in the study was voluntary and no financial compensation was given to the recruited participants. A specific online-consent form for the collection and the publication of the data was signed before the enrollment according to the Italian legislation. The study obtained consent from the Institutional Ethic Committees (Institutional Review Border of IRCSS “Burlo Garofolo Pediatrc Hospital”, IRB code 10/20, approved on October 2020).
The list of consecutive recoveries or follow-up visits that were realized in the two centers between 4 May 2020 and 31 May 2020 was used as a source for recruiting the potential participants.
The inclusion criteria included: (a) the patient had to be in the continuity of care without discriminations based on the severity of the diseases and the required frequency of the controls; and (b) for each patient, they were asked to identify a single main caregiver, among the two parents, to fill in the questionnaire.
The survey was shared via email after an explanatory phone call. The collection of questionnaires lasted from 1 June to 30 July 2020 with a normal distribution of the completed forms during the whole period.
Participants were asked to fill in an anonymous online questionnaire in two parts (available at:
https://forms.gle/6jbDYNDhrHPFDiS7A (accessed on 15 April 2022); see an English version in
Supplementary File S1) focused on the lockdown period (9 March 2020–3 May 2020): (a) the first part included general information about the children’s diseases and their trend during the lockdown but also the families’ habits and their changes, especially in the care and the needs of the children in this period; and (b) the second part included the Perceived Stress Scale (PSS), in order to measure the degree to which lockdown was appraised as stressful (see
Supplementary File S1) [
9]. The first part included multiple choice answers including the possibility of an additional open answer (see
Supplementary File S1). No missing data were possible because the survey could not be uploaded if the participants did not fill in all the sections.
The survey covered all the possible lockdown-related stressors that were correlated with the management of the health care needs of the patients and required less than 5 min to be completed.
Three groups were defined according to the patient’s diagnosis: (a) epilepsy of unknown etiology; (b) neurodevelopmental disorders; and (c) genetic-metabolic diseases. A predominant symptom, according to clinical judgement, was identified for the assignment of patients with comorbidities (e.g., epilepsy and neurodevelopmental disorders) to one of the above-mentioned groups. Patients presenting with epilepsies with a known genetic etiology were assigned to the third group.
All statistical analyses were conducted using IBM SPSS Statistics version 25.0 (SPSS Inc., Chicago, IL, USA). A p value < 0.05 represented the statistical significance for all tests. Data were reported as frequencies and percentages for discrete variables as well as the means and standard deviations for continuous variables. The chi-squared test (χ2) was used to reveal the differences between and within groups in the discrete variables investigated, while one-way analysis of variance (ANOVA) was carried out to test the between and within group differences in continuous variables. Bonferroni corrections were applied to reduce problems associated with multiple comparisons. The dimensional effect of clinical variables on the outcome was evaluated by multiple linear regression analysis.
3. Results
3.1. Demographic and Clinical Data
The survey was sent to 511 families, and it was filled in by the parents of 250 patients (response rate = 48.9%; the optimal sample size according to
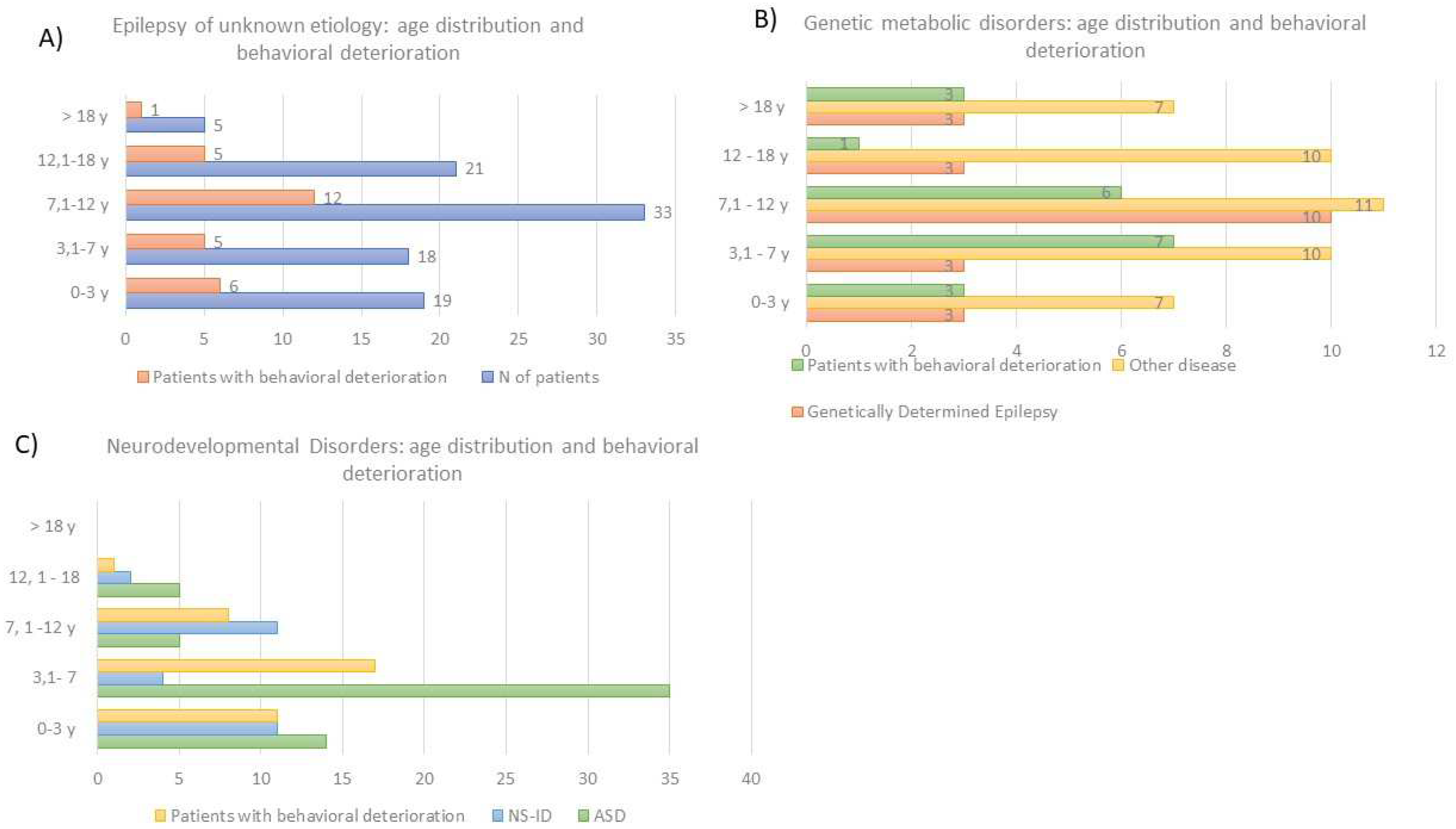
https://www.surveysystem.com/sscalc.htm (accessed on 15 April 2022) was 152 participants). The responders were mainly the mothers (71.5%). The cohort of the analyzed patients included: 96 patients with epilepsies of unknown etiology (38%), 88 patients with neurodevelopmental disorders (35%), 66 patients with genetics-metabolic diseases (33%; this group included 22 patients with genetically determined epilepsies). The mean age of the patients was 8 years and 9 months (age range: 12 months–37 years) and 53% of them was male. The age distribution among the three above-mentioned groups is indicated in
Figure 1.
Before lockdown, 238 patients (95.2%) attended school while 154 patients (61.6%) took advantage of regular rehabilitation/occupational therapy
Two patients (0.8%) tested positive for COVID-19. The disease presented with gastrointestinal symptoms in one patient and with an asymptomatic course in the other. A total of 6% of the participants reported at least one familial case of COVID-19 infection.
3.2. The Impact of Lockdown on Children Health and Care According to Parental Perspective
School closure resulted in a complete interruption of any teaching experience in 114 patients (44.2%), who did not have access to remote lessons. Remote teaching was positively judged by almost all of the parents with children involved in this method (71%) because of the chance of a continuing relationship with their mates and teachers and the maintenance of some sort of regularity. Despite the positive impression, the parents reported some critical issues such as unavailable or stable Internet connection, standard technologies non-suitable for disabilities, and “virtual” relationships with peers insufficient for the children’s well-being.
Lockdown changed the parents ‘work activities in 70% of the cases via layoffs (27%), working from home (39%), or reduction/suspension (38%).
Health and welfare services were suspended for 77% of patients. According to the parents, the children were negatively affected by the lack of rehabilitation services (67%) and the loss of the usual clinical and instrumental checks (45%). A total of 79.1% of parents were able to contact doctors, mostly by phone call or email. Thirty-seven patients (15%) needed urgent specialist examination during the lockdown period and in 68% of cases for reason of their neurological condition: eight patients underwent hospitalization, four patients accessed the emergency room, 17 patients needed an urgent outpatient visit with their neurologist, and the remaining patients were managed at home by their pediatrician.
Access to remote rehabilitation services was available for 58 patients (22.5%). Only 5% of parents found this method to be adequate for the therapeutic goals; nevertheless, most of them provided positive feedback on telerehabilitation because it allowed for a continuing relationship between the children and therapists (48%) and provided support to the parents, involving them in rehabilitation activities (38%).
During the lockdown, the clinical conditions remained stable for most patients (83%) with a worsening in 15% (40 patients) of cases. Behavioral deteriorations were observed in 35% (86 patients) of cases.
3.3. The Impact of Lockdown on Parental Distress
Perceived stress, as measured by PSS, was high in 37 parents (14%); moderate in 146 parents (58%); and low in 70 (28%). No significant correlation was found between the PSS score and age or gender of the patients (
p = 0.06 and
p = 0.48, respectively). The parents of children affected by neurodevelopmental disorders had higher levels of stress than other parents (F
(2;247) = 3.391,
p = 0.035;
Table 2).
Higher scores on the PSS were obtained by parents who underwent job changes (
p < 0.05) while no significant perceived effects were associated with the presence of remote homeschooling and remote rehabilitation services (
p value of 0. 43 and 0.58, respectively;
Table 3).
Another significant stressor was represented by the loss/discontinuation of specialist follow-up programs and the need for urgent medical care, while no relevant effects were associated with the inability to contact the referring specialist (
Table 3 and
Table 4).
The three analyzed diagnostic groups did not differ in terms of the perceived clinical worsening by parents (chi-square = 7.71; p = 0.26). A significant behavioral deterioration (chi-square = 16.12; p < 0.05) was detected in all three groups, independent of the etiologies, with a higher negative perceived impact in patients with a neurodevelopmental disorder (45% of patients versus 29% of patients with epilepsy of unknown etiology and 30% of patients with genetic-metabolic diseases). A marginally significant perceived worsening in the functioning and adaptive behavior was assessed in all three diagnostic groups (chi-square = 16.66; p = 0.05).
4. Discussion
This study confirmed that the COVID-19 pandemic had broader effects than infections only on several aspects of daily life and health care. The survey highlighted a negative impact of lockdown-related limitations and closures on the parental perception of the clinical conditions and the adequacy of access to health care services for children with chronic neurological and neurodevelopmental disorders. This negative perception contributed to an increase in the number of parental stressors and probably affected the patients’ care and quality of life. The most significant difficulties were reported by the parents of children with neurodevelopmental disorders because of a higher frequency of behavioral disturbances. This finding is consistent with previously published data that had shown more remarkable consequences of restrictions in children with autism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD) than in pediatric patients with other chronic disorders [
9]. The higher vulnerability of these patients resulted from the known negative impact of changes in their daily routine and the limitations in the preferred activities in children with an autism spectrum disorder [
10]. Data from a U.S. survey suggested that higher levels of stress in the parents of autistic children were mainly related to isolation, fear of illness or clinical worsening because of the lack of specialist care, economic worries, the severity of autistic symptoms, and younger age [
11,
12]. An increase in behavioral disruption was also reported in a significant proportion of patients with other diseases, ranging between 30–35.9% of children with epilepsy and 55% of children with cerebral palsy, neuromuscular disorders, and other neurological diseases [
13,
14,
15]. The lack of human resources in providing health care and psychological support were perceived as the main stressors by parents in these last cases [
15]. A few other studies have shown several additional behavioral changes in children with special needs during isolation and quarantine [
7,
13,
16,
17,
18,
19]. In these contexts, children might become more demanding with their parents and experience feelings of impatience, annoyance, and hostility, in addition to the fear of infection and frustration for the loss of their daily routine [
7,
13,
16,
17,
18,
19]. These reactions might complicate the global support granted by caregivers and should be considered in designing specific pathways for psychological support for parents [
7,
13,
16,
17,
18,
19].
The level of parental stress during the Sars-COV2 pandemic was assessed as significantly higher in the parents of children with chronic physical and/or chronic mental conditions than in the parents of healthy children [
16]. The main stressors that were identified by the parents of children with chronic neurological diseases included: perception or fear of clinical worsening or increased clinical risk for their children, loss of regular health checks, inability to reach the referring neurologist using telemedicine resources, loss of economic income, anxiety and/or depression of the caregivers, and difficulties in finding specific drugs on the market (e.g., antiepileptic drugs) [
13,
18,
19]. The interruption of clinical follow-up and rehabilitative programs represented the most relevant stressor for parents, in the herein reported, cohort, even if the experience with remote technologies was not completely negative and most of the caregivers had no difficulties in contacting the referring specialists. Remote schooling, telemedicine, and telerehabilitation services were perceived as partially useful to replace the direct relationship of children with medical specialists, therapists, support teachers, and mates while the suspension of medical care was considered more stressful than the closure of schools and rehabilitation services. The relevance of these stressors was independent of the etiology of the diseases of the reported children. This aspect suggests that parental worries and fears might be far more correlated with the loss of certainty about follow-up planning than with the basic clinical conditions. The relationship between the mentioned stressors and the fears of eventual clinical worsening might be a subject for debate, but both our data and the ones obtained in previously published cohorts suggested that this perception might be high in the caregivers [
13,
14]. These fears seem to be correlated with an effective increase in seizure frequency, which ranged between 13.3 and 14%, in two different cohorts of children with epilepsy in Spain and Italy, respectively [
13,
14].
The main limitations of our study include the cross-sectional design, the bias selection given by the voluntary participation of parents, the small size of the sample that might underrepresent the effective population of patients and parents referring to the two involved tertiary centers, the self-reported nature of all the collected data, and the possible effect of confounders. Another possible confounding effect was given by the different diffusion of the infections in the regions of the two enrolling centers, even if these two hospitals have a national catchment area. A further source of bias selection might be represented by the selection of patients who referred to two specialistic tertiary centers with a possible exclusion of children suffering from less severe neurological diseases. Moreover, the feelings and other events experienced by parents during the lockdown were recorded in the aftermath using a self-reporting questionnaire and no previous data on parental distress before and after the pandemic were available to compare the differences (e.g., behavioral changes were perceived as lockdown correlated by parents, but they might also be influenced by other individual and social factors). Similarly, the specific burden for neurological and neurodevelopmental disorders of the reported results was not quantifiable because no comparable data were available on children with non-neurological disorders.
5. Conclusions
Social distancing limited the Sars-CoV2 outbreak during the so-called “first wave” and caused a reorganization of health care settings and clinical practice that have affected the well-being of families caring for pediatric neurologic children. It seems necessary to adapt the health response to the families’ needs since the continuity of care for chronic patients could be considered as a protective factor by their parents and related to the caregivers’ mental health. Higher levels of stress in this at-risk population seems to be related to the suspension of the usual clinical checks. The maintenance of high-quality medical assistance for patients with diseases other than COVID-19 will represent a remarkable challenge for all health care systems during the next phases of the current Sars-CoV2 pandemic.
Author Contributions
Conceptualization, S.C., M.M. and G.A.; Methodology, S.C. and C.B.; Software, R.M.E.; Validation, M.M., G.A. and S.C.; Formal analysis, R.M.E. and M.T.; Resources, F.G., F.M. and C.B.; Data curation, R.M.E. and M.T.; Writing—original draft: preparation, S.C.; Writing—review and editing, M.M.; Supervision, M.M., F.M. and G.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved by the Institutional Review Border of the IRCSS “Burlo Garofolo Pediatric Hospital”, IRB code 10/20, approved on October 2020.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available on request from the authors.
Acknowledgments
The authors acknowledge all of the parents who completed the survey and thank Mario Brinciotti, Francesca Nardecchia, Serena Galosi, Carla Sogos, Barbara Caravale, and Andrea Magnolato for their support in the recruitment of the patients and parents.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization. Available online: https://covid19.who.int/ (accessed on 15 April 2022).
- Istituto Superiore di Sanità. Available online: https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_27-ottobre-2020.pdf (accessed on 15 April 2022).
- Bellino, S.; Punzo, O.; Rota, M.C.; Del Manso, M.; Urdiales, A.M.; Andrianou, X. COVID-19 Disease Severity Risk Factors for Pediatric Patients in Italy. Pediatrics 2020, 146, e2020009399. [Google Scholar] [CrossRef] [PubMed]
- Governo, I. Presidenza dei Ministry. Available online: http://www.governo.it/it/articolo/firmato-il-dpcm-9-marzo-2020/14276# (accessed on 15 April 2022).
- Orsini, A.; Corsi, M.; Santangelo, A.; Riva, A.; Peroni, D.; Foiadelli, T.; Savasta, S.; Striano, P. Challenges and management of neurological and psychiatric manifestations in SARS-CoV-2 (COVID-19) patients. Neurol. Sci. 2020, 41, 2353–2366. [Google Scholar] [CrossRef] [PubMed]
- Panda, P.K.; Sharawat, I.K. COVID-19 (SARS-CoV-2 Infection) and Children: Pediatric Neurologist’s Perspective. Indian J. Pediatr. 2020, 87, 556–557. [Google Scholar] [CrossRef] [PubMed]
- Spinelli, M.; Lionetti, F.; Pastore, M.; Fasolo, M. Parents’ Stress and Children’s Psychological Problems in Families Facing the COVID-19 Outbreak in Italy. Front. Psychol. 2020, 11, 1713. [Google Scholar] [CrossRef] [PubMed]
- Sprang, G.; Silman, M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med. Public Health Prep. 2013, 7, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Serlachius, A.; Badawy, S.M.; Thabrew, H. Psychosocial Challenges and Opportunities for Youth with Chronic Health Conditions During the COVID-19 Pandemic. JMIR Pediatr. Parent. 2020, 3, e23057. [Google Scholar] [CrossRef] [PubMed]
- Hayes, S.A.; Watson, S.L. The impact of parenting stress: A meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. J. Autism Dev. Disord. 2013, 43, 629–642. [Google Scholar] [CrossRef] [PubMed]
- Manning, J.; Billian, J.; Matson, J.; Allen, C.; Soares, N. Perceptions of Families of Individuals with Autism Spectrum Disorder during the COVID-19 Crisis. J. Autism Dev. Disord. 2020, 22, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Grumi, S.; Provenzi, L.; Gardani, A.; Aramini, V.; Dargenio, E.; Naboni, C.; Vacchini, V.; Borgatti, R. Engaging with Families through On-line Rehabilitation for Children during the Emergency (EnFORCE) Group. Engaging with Families through On-line Rehabilitation for Children during the Emergency (EnFORCE) Group. Rehabilitation services lockdown during the COVID-19 emergency: The mental health response of caregivers of children with neurodevelopmental disabilities. Disabil. Rehabil. 2020, 10, 1–6. [Google Scholar] [CrossRef]
- Aledo-Serrano, Á.; Mingorance, A.; Jiménez-Huete, A.; Toledano, R.; García-Morales, I.; Anciones, C.; Gil-Nagel, A. Genetic epilepsies and COVID-19 pandemic: Lessons from the caregiver perspective. Epilepsia 2020, 61, 1312–1314. [Google Scholar] [CrossRef] [PubMed]
- Trivisano, M.; Specchio, N.; Pietrafusa, N.; Calabrese, C.; Ferretti, A.; Ricci, R.; Renzetti, T.; Raponi, M.; Vigevano, F. Impact of COVID-19 pandemic on pediatric patients with epilepsy—The caregiver perspective. Epilepsy Behav. 2020, 23, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Cacioppo, M.; Bouvier, S.; Bailly, R.; Houx, L.; Lempereur, M.; Mensah-Gourmel, J. Emerging health challenges for children with physical disabilities and their parents during the COVID-19 pandemic: The ECHO French survey. Ann. Phys. Rehabil. Med. 2020, 64, 101429. [Google Scholar] [CrossRef] [PubMed]
- AL van Tilburg, M.; Edlynn, E.; Maddaloni, M.; van Kempen, K.; Díaz-González de Ferris, M.; Thomas, J. High Levels of Stress Due to the SARS-CoV-2 Pandemic among Parents of Children with and without Chronic Conditions across the USA. Children 2020, 7, 193. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Wang, G.; Zhang, Y.; Zhao, J.; Zhang, J.; Jiang, F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet 2020, 395, 945–947. [Google Scholar] [CrossRef]
- Dilek, T.D.; Boybay, Z.; Kologlu, N.; Tin, O.; Güler, S.; Saltık, S. The impact of SARS-CoV2 on the anxiety levels of subjects on the anxiety and depression levels of their parents. Mult. Scler. Relat. Disord. 2020, 26, 102595–102600. [Google Scholar] [CrossRef] [PubMed]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).