Does a Graf Type-I Hip Justify the Discontinuation of Pavlik Harness Treatment in Patients with Developmental Dislocation of the Hip?
Abstract
1. Introduction
2. Materials and Methods
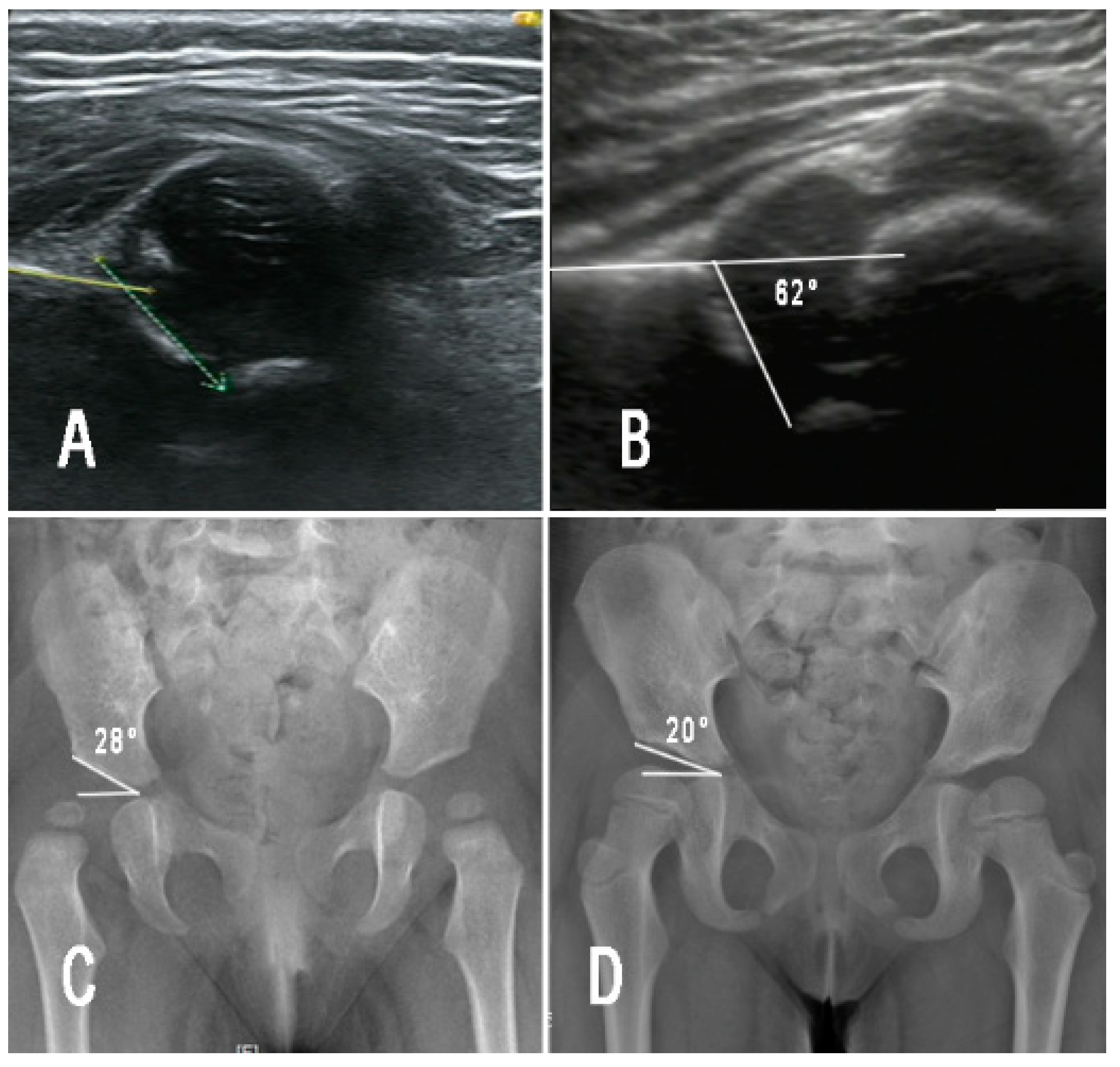
2.1. Ultrasonography and Radiographic Assessment
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kotlarsky, P.; Haber, R.; Bialik, V.; Eidelman, M. Developmental dysplasia of the hip: What has changed in the last 20 years? World J. Orthop. 2015, 6, 886–901. [Google Scholar] [CrossRef]
- Vaquero-Picado, A.; González-Morán, G.; Garay, E.G.; Moraleda, L. Developmental dysplasia of the hip: Update of management. EFORT Open Rev. 2019, 4, 548–556. [Google Scholar] [CrossRef] [PubMed]
- Swarup, I.; Penny, C.L.; Dodwell, E.R. Developmental dysplasia of the hip: An update on diagnosis and management from birth to 6 months. Curr. Opin. Pediatr. 2018, 30, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Ömeroglu, H. Treatment of developmental dysplasia of the hip with the Pavlik harness in children under six months of age: Indications, results and failures. J. Child. Orthop. 2018, 12, 308–316. [Google Scholar] [CrossRef] [PubMed]
- Hines, A.C.; Neal, D.C.; Beckwith, T.; Jo, C.; Kim, H.K.W. A Comparison of Pavlik Harness Treatment Regimens for Dislocated But Reducible (Ortolani+) Hips in Infantile Developmental Dysplasia of the Hip. J. Pediatr. Orthop. 2019, 39, 505–509. [Google Scholar] [CrossRef]
- Imerci, A.; Rogers, K.J.; Bhattacharjee, A.; Bowen, J.R.; Thacker, M.M. Risk Factors for Failure of Pavlik Harness Treatment in Infants With Dislocated Hips That Are Evaluated by Dynamic Sonography. J. Pediatr. Orthop. 2021, 41, e386–e391. [Google Scholar] [CrossRef]
- Novais, E.N.; Sanders, J.; Kestel, L.A.; Carry, P.M.; Meyers, M.L. Graf Type-IV Hips Have a Higher Risk of Residual Acetabular Dysplasia at 1 Year of Age Following Successful Pavlik Harness Treatment for Developmental Hip Dysplasia. J. Pediatr. Orthop. 2018, 38, 498–502. [Google Scholar] [CrossRef]
- Shaw, K.A.; Moreland, C.M.; Olszewski, D.; Schrader, T. Late acetabular dysplasia after successful treatment for developmental dysplasia of the hip using the Pavlik method: A systematic literature review. J. Orthop. 2019, 16, 5–10. [Google Scholar] [CrossRef]
- Kelley, S.P.; Feeney, M.M.; Maddock, C.L.; Murnaghan, M.L.; Bradley, C.S. Expert-Based Consensus on the Principles of Pavlik Harness Management of Developmental Dysplasia of the Hip. JBJS Open Access 2019, 4, e0054. [Google Scholar] [CrossRef]
- Westacott, D.J.; Perry, D.C. The treatment of neonatal hip dysplasia with splints in the United Kingdom: Time for consensus? J. Child. Orthop. 2020, 14, 112–117. [Google Scholar] [CrossRef]
- Sarkissian, E.J.; Sankar, W.N.; Zhu, X.; Wu, C.H.; Flynn, J.M. Radiographic Follow-up of DDH in Infants: Are X-rays Necessary After a Normalized Ultrasound? J. Pediatr. Orthop. 2015, 35, 551–555. [Google Scholar] [CrossRef]
- Dornacher, D.; Cakir, B.; Reichel, H.; Nelitz, M. Early radiological outcome of ultrasound monitoring in infants with developmental dysplasia of the hips. J. Pediatr. Orthop. B 2010, 19, 27–31. [Google Scholar] [CrossRef]
- Graf, R. Advantages and disadvantages of various access routes in sonographic diagnosis of dysplasia and luxation in the infant hip. J. Pediatr. Orthop. B 1997, 6, 248–252. [Google Scholar] [CrossRef]
- Graf, R. Hip sonography: Background; technique and common mistakes; results; debate and politics; challenges. Hip Int. 2017, 27, 215–219. [Google Scholar] [CrossRef]
- Li, Y.; Guo, Y.; Li, M.; Zhou, Q.; Liu, Y.; Chen, W.; Li, J.; Canavese, F.; Xu, H. Acetabular index is the best predictor of late residual acetabular dysplasia after closed reduction in developmental dysplasia of the hip. Int. Orthop. 2018, 42, 631–640. [Google Scholar] [CrossRef]
- Shi, Y.; Liu, T.; Zhao, Q.; Zhang, L.; Ji, S. The measurements of normal acetabular index and Sharp acetabular angle in Chinese hips. Chin. J. Orthop. 2010, 30, 748–753. [Google Scholar] [CrossRef]
- Harris, I.E.; Dickens, R.; Menelaus, M.B. Use of the Pavlik harness for hip displacements. When to abandon treatment. Clin. Orthop. Relat. Res. 1992, 281, 29–33. [Google Scholar] [CrossRef]
- Bradley, J.; Wetherill, M.; Benson, M.K. Splintage for congenital dislocation of the hip. Is it safe and reliable? J. Bone Jt. Surg. Br. 1987, 69, 257–263. [Google Scholar] [CrossRef]
- Kolb, A.; Benca, E.; Willegger, M.; Puchner, S.E.; Windhager, R.; Chiari, C. Measurement considerations on examiner-dependent factors in the ultrasound assessment of developmental dysplasia of the hip. Int. Orthop. 2017, 41, 1245–1250. [Google Scholar] [CrossRef]
- Quader, N.; Schaeffer, E.K.; Hodgson, A.J.; Abugharbieh, R.; Mulpuri, K. A Systematic Review and Meta-analysis on the Reproducibility of Ultrasound-based Metrics for Assessing Developmental Dysplasia of the Hip. J. Pediatr. Orthop. 2018, 38, e305–e311. [Google Scholar] [CrossRef]
- Roovers, E.A.; Boere-Boonekamp, M.M.; Geertsma, T.S.; Zielhuis, G.A.; Kerkhoff, A.H. Ultrasonographic screening for developmental dysplasia of the hip in infants. Reproducibility of assessments made by radiographers. J. Bone Jt. Surg. Br. 2003, 85, 726–730. [Google Scholar] [CrossRef][Green Version]
- Shi, Y.Y.; Liu, T.J.; Zhao, Q.; Zhang, L.J.; Ji, S.J.; Wang, E.B. The normal centre-edge angle of Wiberg in the Chinese population: A population-based cross-sectional study. J. Bone Jt. Surg. Br. 2010, 92, 1144–1147. [Google Scholar] [CrossRef]
- Novais, E.N.; Kestel, L.A.; Carry, P.M.; Meyers, M.L. Higher Pavlik Harness Treatment Failure Is Seen in Graf Type IV Ortolani-positive Hips in Males. Clin. Orthop. Relat. Res. 2016, 474, 1847–1854. [Google Scholar] [CrossRef]
- Ömeroğlu, H.; Köse, N.; Akceylan, A. Success of Pavlik Harness Treatment Decreases in Patients ≥ 4 Months and in Ultrasonographically Dislocated Hips in Developmental Dysplasia of the Hip. Clin. Orthop. Relat. Res. 2016, 474, 1146–1152. [Google Scholar] [CrossRef]
- Mulpuri, K.; Song, K.M.; Gross, R.H.; Tebor, G.B.; Otsuka, N.Y.; Lubicky, J.P.; Szalay, E.A.; Harcke, H.T.; Zehr, B.; Spooner, A.; et al. The American Academy of Orthopaedic Surgeons Evidence-Based Guideline on Detection and Nonoperative Management of Pediatric Developmental Dysplasia of the Hip in Infants up to Six Months of Age. J. Bone Jt. Surg. Am. 2015, 97, 1717–1718. [Google Scholar] [CrossRef]

| Group A | Group B | χ2/t | p | ||
|---|---|---|---|---|---|
| Hips | n | 45 (71.4%) | 18 (28.6%) | - | - |
| Age (weeks) | 10.7 ± 5.4 | 13.7 ± 7.0 | 1.794 | 0.078 | |
| Gender | Female | 37 (69.8%) | 16 (30.2%) | - | 0.710 |
| Male | 8 (80%) | 2 (20%) | |||
| Side | Left | 25 (75.8%) | 8 (24.2%) | 3.359 | 0.239 |
| Right | 6 (50%) | 6 (50%) | |||
| Bilateral | 14 (77.8%) | 4 (22.2%) | |||
| Preoperative α-angle | 42.4° ± 4.5° | 40.8° ± 6.4° | 1.023 | 0.311 | |
| Graf classification | II-D | 18 (85.7%) | 3 (14.3) | 1.266 | 0.583 |
| III | 20 (76.9%) | 6 (23.1%) | |||
| IV | 7 (70%) | 3 (30%) | |||
| Duration of PH treatment (months) | 3.0 ± 0.3 | 3.2 ± 0.4 | 1.213 | 0.236 | |
| Follow-up time (months) | 26.0 ± 16.0 | 20.5 ± 6.3 | 1.931 | 0.058 | |
| RAD following removal of PH | No | 22 (56.4%) | 17 (43.6%) | 11.314 | 0.001 |
| Yes | 23 (95.8) | 1 (4.2%) | |||
| AI (6 months after completion of PH treatment) | 27.1° ± 6.8° | 21.9° ± 3.5° | 4.045 | 0.000 | |
| Final AI | 20.5° ± 3.3° | 21.9° ± 3.3° | 1.528 | 0.132 | |
| Final CEA | 17.4° ± 6.1° | 19.3° ± 4.5° | 1.153 | 0.255 | |
| RAD at final follow-up | No | 40 (69%) | 18 (31%) | - | 0.31 |
| Yes | 5 (100%) | 0 (0%) |
| RAD | χ2/t | p | |||
|---|---|---|---|---|---|
| No | Yes | ||||
| Hips | n | 22 (48.9%) | 23 (51.1%) | - | - |
| Age (weeks) | 7.6 ± 3.8 | 13.7 ± 4.9 | 4.666 | 0.000 | |
| Gender | Female | 16 (43.2%) | 21 (56.8%) | - | 0.135 |
| Male | 6 (75%) | 2 (25%) | |||
| Side | Left | 11 (44%) | 14 (56%) | - | 0.239 |
| Right | 5 (83.3%) | 1 (16.7%) | |||
| Bilateral | 6 (42.9%) | 8 (57.1%) | |||
| Preoperative α-angle | 43.6° ± 4.7° | 41.1° ± 4.0° | 1.901 | 0.064 | |
| Graf classification | II-D | 14 (77.8%) | 4 (22.2%) | - | 0.006 |
| III | 6 (30%) | 14 (70%) | |||
| IV | 2 (28.6%) | 5 (71.4%) | |||
| Duration of PH treatment (months) | 3.1 ± 0.3 | 3.1 ± 0.4 | 0.075 | 0.94 | |
| Coefficient | SE | Wald | p | RR | 95% of CI for RR | |
|---|---|---|---|---|---|---|
| Age | 0.179 | 0.064 | 7.927 | 0.005 | 1.196 | 1.056, 1.355 |
| Graf type | 0.564 | 0.447 | 1.593 | 0.207 | 1.758 | 0.732, 4.222 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.; Canavese, F.; Liu, Y.; Wu, J.; Li, J.; Yuan, Z.; Zhou, Q.; Liu, Y.; Chen, W.; Xu, H. Does a Graf Type-I Hip Justify the Discontinuation of Pavlik Harness Treatment in Patients with Developmental Dislocation of the Hip? Children 2022, 9, 752. https://doi.org/10.3390/children9050752
Li Y, Canavese F, Liu Y, Wu J, Li J, Yuan Z, Zhou Q, Liu Y, Chen W, Xu H. Does a Graf Type-I Hip Justify the Discontinuation of Pavlik Harness Treatment in Patients with Developmental Dislocation of the Hip? Children. 2022; 9(5):752. https://doi.org/10.3390/children9050752
Chicago/Turabian StyleLi, Yiqiang, Federico Canavese, Yanhan Liu, Jianping Wu, Jingchun Li, Zhe Yuan, Qinghe Zhou, Yuanzhong Liu, Weidong Chen, and Hongwen Xu. 2022. "Does a Graf Type-I Hip Justify the Discontinuation of Pavlik Harness Treatment in Patients with Developmental Dislocation of the Hip?" Children 9, no. 5: 752. https://doi.org/10.3390/children9050752
APA StyleLi, Y., Canavese, F., Liu, Y., Wu, J., Li, J., Yuan, Z., Zhou, Q., Liu, Y., Chen, W., & Xu, H. (2022). Does a Graf Type-I Hip Justify the Discontinuation of Pavlik Harness Treatment in Patients with Developmental Dislocation of the Hip? Children, 9(5), 752. https://doi.org/10.3390/children9050752







