Abstract
Children with rare or life-limiting chronic conditions and their families are at high risk of psychosocial distress. However, despite its impact on patient and family health and functioning, psychosocial distress and its antecedents may not routinely be captured in medical records. The purpose of this study was to characterize current medical record documentation practices around psychosocial distress among children with rare or life-limiting chronic conditions and their families. Medical records for patients with rare or life-limiting chronic conditions (n = 60) followed by a pediatric complex care program were reviewed. Study team members extracted both structured data elements (e.g., diagnoses, demographic information) and note narratives from the most recent visit with a clinician in the program. Psychosocial topics were analyzed using a mixed quantitative (i.e., frequency counts of topics) and qualitative approach. Topics related to psychosocial distress that were documented in notes included child and parent emotional problems, parent social support, sibling emotional or physical problems, family structure (e.g., whether parents were together), and financial concerns. However, 35% of notes lacked any mention of psychosocial concerns. Although examples of psychosocial concerns were included in some notes, none were present in over one-third of this sample. For both patients with rare or life-limiting chronic conditions and their caregivers, more active elicitation and standard documentation of psychosocial concerns may improve the ability of healthcare providers to identify and intervene on psychosocial concerns and their risk factors.
1. Introduction
Over the past 50 years, medical advances have reduced overall childhood morbidity and mortality, allowing children with rare or life-limiting chronic conditions to survive and live longer [1,2,3,4,5]. Rare or life-limiting chronic conditions include congenital abnormalities, neurodegenerative diseases, metabolic disorders, the sequelae of extreme prematurity, and other disorders that are often serious and incurable but may be managed with ongoing medical intervention and lifestyle adaptations. However, despite medical and scientific advances, children with rare or life-limiting chronic conditions and their families often face significant challenges to their quality of life as a result of long-term, complex medical regimens [6], frequent provider visits and hospitalizations [3], gaps in care coordination [7,8], and functional limitations that are typically severe and may include reliance on technology [8,9,10]. In addition to healthcare and functional challenges, children with rare or life-limiting chronic conditions are at increased risk for the development of social [11], behavioral [12], and emotional problems [13], which, if not detected and treated, can impact the child’s adherence to medical recommendations [14,15], exacerbate physical illness [16], and increase healthcare utilization [17].
The struggles associated with childhood rare or life-limiting chronic conditions are not limited to the patients themselves, as parents and other family caregivers assume tremendous responsibility on behalf of these vulnerable patients [18]. Collectively, caregivers for children with rare or life-limiting chronic conditions have been described as a “shadow” healthcare system for children with medical complexity [19], forced to act as patient advocates, care coordinators, and home health aides, resulting in significant disruptions to work and family function [20,21,22]. Not surprisingly, parents of children with rare or life-limiting chronic conditions frequently report problems related to mood [23], physical function [24], marital discord [25], social isolation [22], and unmet needs [26]. Many parents of children with rare or life-limiting chronic conditions experience disruption to their careers [27,28] and financial insecurity [29]. High levels of parental distress, in turn, can impact a child’s medication adherence [30] and has been linked to greater emotional distress and reduced quality of life in the child [31,32]; highlighting the importance of attention to parental emotional functioning in the context of the child’s care [33].
Together, these behavioral, emotional, social, and financial challenges to children with rare or life-limiting chronic conditions and their families can be termed psychosocial distress. Pediatric psychosocial distress in this clinical context has been conceptualized in a variety of ways. Kazak et al. developed the widely used Pediatric Psychosocial Preventative Health Model (PPPHM), which employs a public health framework to match family psychosocial risk with appropriate interventions. The Psychosocial Assessment Tool (PAT) is a parent-reported screening tool based on the PPPHM that operationalizes psychosocial risk into the following domains: family structure/resources, family problems, social support, stress reactions, family beliefs, child problems, and sibling problems. Additional approaches to categorizing psychosocial risk among families with children who have rare or life-limiting chronic conditions include the Distress Thermometer, which screens for distress in domains related to practical, familial, emotional, and physical problems, as well as spiritual and religious concerns. Although no single definition exists for psychosocial distress among children with rare or life-limiting conditions, current approaches all take a broad, social-ecological approach that includes not only the psychological wellbeing of the patient but that of their caregivers and siblings, as well as their socio-economic circumstances, family structure, and social function.
While it is clear that children with rare or life-limiting chronic conditions and their families are at increased risk for psychosocial distress, the extent to which this phenomenon and its antecedents are documented during routine medical appointments is unknown. Without adequate or standardized documentation of psychosocial concerns, families who would likely benefit from further assessment, targeted referrals, and service linkages may be at risk of slipping through the cracks. Therefore, the goal of the current study was to characterize the current medical record documentation practices around child and family psychosocial distress and risk factors for distress. Specifically, this work sought to answer the following research questions: (1) What information about patient and family psychosocial distress is extractable from the narrative text of clinical notes? (2) How frequently is psychosocial distress or its antecedents mentioned in routine outpatient clinical notes? and (3) How is psychosocial distress characterized by providers in the medical record?
2. Materials and Methods
Eligible patients were children and adolescents (<20 years old) followed by a pediatric complex care coordination program at Mayo Clinic in Rochester, MN, USA (henceforth referred to as “the program”). The program is not a medical home but rather a consultative service that serves as the primary point of contact for patients and their families while receiving care from multiple specialty groups within Mayo Clinic. Approximately half of enrolled patients have at least one disease considered to be rare (i.e., affecting less than 200,000 Americans). The goal of the program is to improve communication among specialists at Mayo Clinic with local primary care providers and families to ensure a unified and holistic view of treatment plans and goals. Children who are followed by the program typically have significant chronic conditions in three or more body systems, need ongoing subspecialty care (longer than one year), and receive most of their subspecialty care at Mayo Clinic.
The program maintains a list of active patients (n = 166 at time of study), which was shared with the study team. Using a random number generator, 60 eligible patients from this list of active patients were identified for inclusion in our chart review. The most recent clinic visit with one of the program pediatricians or nurse practitioners was identified and the associated note was extracted for each patient in our sample. Two co-authors (EG and DG) each independently extracted five randomly selected patients to pilot test the extraction form and ensure consistency, which was deemed satisfactory after comparing responses and reaching consensus through discussion as a team. The remaining charts were divided between EG and DG and extracted individually. The following data elements were extracted from each patient’s chart using a REDCap [34] electronic data capture form: visit date and provider; demographic information, including patient age, gender, race, city and state of residence, preferred language, and health insurance; problem list; and the full narrative text of the note. Analysis proceeded according to a mixed methods explanatory sequential design (Figure 1).
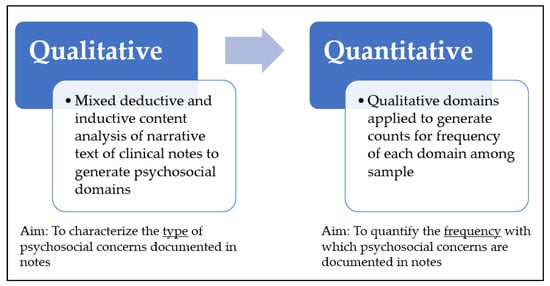
Figure 1.
Mixed methods explanatory sequential design.
2.1. Qualitative Analysis
Qualitative analysis was performed using NVivo qualitative data analysis software, Version 12. All clinical notes in the sample (n = 60) were coded on a line-by-line basis for narrative sections of the note (e.g., “History of Present Illness”, “Assessment”). The narrative text of the extracted encounter notes was coded using a mixed deductive (i.e., identified a priori based on existing literature on psychosocial distress in this population) and inductive (i.e., developing emergent codes that arose through review of the notes) approach. Key sources for deductive coding included domains from Kazak’s Psychosocial Assessment Tool (PAT) and the pediatric Distress Thermometer. An initial coding scheme was outlined based on previously described domains of psychosocial risk for children with serious medical illnesses and their families [35,36,37,38,39,40,41]. Authors then read through the narrative text of each note to further develop and refine the initial coding scheme, including determining which specific topics of discussion would be included in each broader coding category. After the development of the coding scheme, coding was performed on five notes in triplicate (SM, EG, and DG), using consensus to arrive at final code assignments for each note. Disagreements were taken as an indicator that the coding scheme required further clarification and the codebook was expanded and clarified as needed, eventually resulting in a final coding scheme organized into the following higher-order domains: Child Psychosocial Health, Family Adjustment and Support, and Family Structure and Resources. The final domains and subdomains reported on in this manuscript are detailed in Table 1 below. Each note was coded independently by two authors (DG, JC, EG). Any discrepancies between coding decisions were discussed as a team, with the third coder responsible for making final decisions in cases where disagreements could not be resolved. Quotes are used within the results section for illustrative purposes.

Table 1.
Psychosocial domains developed during qualitative coding, their descriptions, and their prevalence in the study sample of clinical notes (n = 60).
2.2. Quantitative Analysis
After the authors completed the coding of all 60 notes, descriptive statistics were generated for demographic information and visit diagnosis counts. Additionally, the number of notes in which each code appeared was counted. These counts acted as a proxy for the frequency in which discussion and documentation occurred around the respective topics in our sample of 60 patients.
3. Results
3.1. Sample Characteristics
Demographic information is shown in Table 2. Patients included in this study had a mean age of 7.3 years (ranging from 10 months to 18 years). Slightly over half (56.7%) of patients were male. Most of the sample (91.7%) was white. All patients’ preferred language was listed as English. Twenty-five percent of patients had private insurance, 40.0% had Medicaid, and 35.0% percent had a combination of the two. Patients’ average drive time to receive care at Mayo Clinic was 187.6 min. The most common visit-related diagnosis categories were neurologic/neuromuscular (63.3% of visits), gastrointestinal (53.3%), and respiratory (41.7%).

Table 2.
Characteristics of the patient sample (n = 60).
3.2. Child Psychosocial Health
Problems or concerns specifically regarding the patient’s emotional function were mentioned in 30 of the 60 medical notes (50%). While some notes described specific behaviors (e.g., “She does not listen to what her parents ask her to do”) others were vaguer (e.g., “[patient] has been struggling with social media interactions”). Difficulties with the patient’s behavior (n = 9) and anxiety (n = 4) were discussed most frequently. Treatment for these concerns was discussed in seven notes, usually by referencing ongoing treatment (e.g., “he is followed locally by a psychiatrist to manage his ADHD and anxiety and is scheduled to see a local counselor for his anxiety” and “she has benefited from her ABA program”) or the discussion of a referral for further evaluation and treatment (n = 1). The child’s school situation was mentioned in a majority of notes (n = 49; 81.7% of notes), with providers typically noting the patient’s current grade level at a minimum. However, many notes contained additional context on the child’s school function (e.g., “School is not going well due to fatigue”; “has attended 4 days of school this year due to Make A Wish, illness and appointments”). Concerns related to development were less common (n = 18; 30%) but still present in nearly one-third of notes in our sample. Finally, remarks about social interaction were coded in one-fifth of notes (n = 12; 20%) and included references to both positive experiences related to patient extracurricular activities, hobbies, and friendships, as well as difficulties related to participating in activities and socializing (e.g., “She is having a lot of urinary incontinence. This is making it difficult socially for her.”).
3.3. Family Adjustment and Support
Although 10 notes (16.7%) referred to parental emotional function, none of them identified specific concerns regarding a parent’s emotional health (e.g., parent mental health diagnosis; parent mental health treatment). Five notes referenced how the child’s medical illness and caregiving responsibilities were a source of significant stress on the parent (“[Parent] feels she is ‘hanging on by a thread”). Respite care was the only potential intervention mentioned in response to these stressors. It is interesting to note, some of the notes had a family history section which included parental mental health history; however, whether this section was included depended on the template the author used, and we were not able to ascertain who had entered these data into the medical record, or when it was entered. Therefore, this information was not included in our analyses.
Seven of the 60 notes (11.7%) referenced the provision of social and material support to the parents or family. Examples of this included grandparents being trained to provide care for a patient, a patient’s mother who expressed feeling well-supported by resources being provided from the county, and another mother who was receiving extra supplies from a friend. A small number of notes (n = 5; 8.3%) mentioned instances of intra-family conflict (e.g., “Family has been under some stress as father is no longer involved with [child’s] care”). Finally, concerns regarding sibling emotional function were mentioned in 3 of the 60 notes (5%). In one case, a sibling’s diagnosis of autism was mentioned, and their aggression towards the patient was discussed as an ongoing stressor. In other cases, siblings were described as also having chronic health conditions, sometimes similar to those of the patient (e.g., “The family has been incredibly busy with managing three children (two with chronic health conditions)”.
3.4. Family Structure and Resources
Information about family structure was included in 47 of the 60 notes (78.3%). The most common descriptor was who the child lived with (n = 43), although specific information about risk factors, such as the age of these family members, was rarely included. Notes frequently mentioned the parents’ occupation (n = 29) if they were employed but did not include additional information about unemployment or underemployment. If the parents were not married, or were going through a divorce, this was also mentioned in some of the notes (n = 9). Nearly one-third of notes (n = 18) referenced barriers or facilitators to obtaining medical care and following treatment plans (e.g., “…as travelling to Rochester is a challenge for the family, they would like to limit medical appointments). However, financial concerns were specifically mentioned in only seven notes (11.7%). Most of these referenced struggles with obtaining insurance authorization or appealing denials for coverage of specific tests (e.g., genome sequencing), medications (e.g., injections), or services (e.g., increased nursing hours). Information regarding the impact of the child’s medical illness on parental employment (e.g., mother left the workforce to care for the child; stress taking care of the child and the family business simultaneously) were included explicitly in five notes (8.3%).
4. Discussion
In this chart review and analysis of pediatric outpatient encounter notes, we found that psychosocial distress and/or risk factors for distress were not consistently documented. Only one-third of notes in our sample documented discussion of the child’s emotional health, while mention of parent’s emotional concerns was largely absent—despite recent national data indicating that almost 20% of parents of children with rare or life-limiting chronic conditions report poor or fair mental health [23]. In addition, most notes in our sample did not capture risk factors and vulnerabilities of the broader family system (i.e., financial, parent and sibling adjustment). Although financial concerns were discussed in 12% of visits in our sample, survey data indicate much higher rates of financial hardship among this population [20], as well as high rates of unmet healthcare needs due to cost [42].
It is important to note that we do not intend for these findings to be critical of individual clinicians, as the reasons for lack of documentation are multifactorial and, in most cases, cultural and institutional. First, one key limitation of medical record data in the absence of validation methods (e.g., recording or observation of the clinical visit) is the inability to shed light on discussions that occurred but were not explicitly documented. Providers may be discussing psychosocial concerns to some degree during appointments but may feel reluctant to incorporate this information into medical notes for many reasons, including ambiguity about which problems rise to the level of clinical significance and which are a function of temporary stressors [43]. In addition, providers may also work under the assumption that psychosocial information is better covered in notes by social work or psychology. However, given the direct association between patient and caregiver psychosocial distress and medical outcomes, we argue that this information should also be included in medical provider documentation. Finally, psychosocial concerns in this population are often not limited to patients but are linked to family circumstances or parental factors. Providers may feel that questions about—let alone, formal documentation of—parental mental health or stressors are perceived as intrusive. However, the importance of including parents and caregivers in psychosocial assessments needs to be stressed, since these concerns are inextricably linked to the child’s well-being [44].
For both patients and their caregivers, universal psychosocial screening offers an opportunity to normalize the psychosocial impact of a child’s illness on the child and the family, and proactively identify children and families who may be experiencing current psychosocial distress or who are at risk for distress during the course of medical care [40,45,46]. Feedback about psychosocial concerns provided to clinicians through screening tools has been found to systematically increase discussion of emotional and psychosocial functioning [47]. Evidence suggests both pediatric clinicians and the parents of their patients support the practice of documenting psychosocial and mental health information in the patient’s health record [43].
There are several evidence-based tools available for screening for psychosocial risks and concerns in pediatric populations. These include the Distress Thermometer [39,40,48], the Psychosocial Assessment Tool 3.0 [37] and Checking In [49]. Research in pediatric oncology [37,39,49] (e.g., Kazak et al., 2018; Patel et al., 2019; Wiener 2021), organ transplant [50] and other life-threatening conditions [41] has demonstrated that psychosocial screening is feasible and acceptable to patients, caregivers, and medical providers. Systematic and routine psychosocial screening provides the opportunity to match the psychosocial care to the specific needs of the child and family, including providing further assessment, preventative interventions, and more specific evidenced-based care [46], with the goal of improving overall quality of life for the patient and their family [51]. The implementation of psychosocial screening increases the number of performed and accepted referrals to psychosocial providers [52], and vastly improves documentation of psychosocial concerns [53]. Screening tools also provide a starting point for clinicians, patients, and families to ease into what may be difficult or awkward conversations. In addition, several of these existing tools include instruments tailored for pediatric patients themselves to answer, allowing older children and adolescents an opportunity to actively participate in these discussions. However, further research is needed to inform best practices around implementation of pediatric psychosocial screening programs as well as the long-term impacts of screening on process and outcome metrics related to how effectively this information is integrated into clinical care [44,54,55]. It is important to note that psychosocial screening in the absence of appropriate referral or intervention strategies will not be sufficient to improve outcomes.
There are several limitations of our study. Our findings are a function of provider documentation in a single clinical note at one academic institution, which may limit the generalizability of these results. Additionally, the clinic notes assessed were from a complex care program which is not designated as a primary care medical home because the majority of patients do not live in the clinic’s immediate vicinity. Therefore, it is certainly possible that patients and families may be receiving social services in their local communities. However, even if psychosocial concerns are being discussed at a higher frequency than our study would imply, or if a patient and their family are receiving social support locally, we argue that documentation of these issues in the medical records of children with rare or life-limiting chronic conditions are critical to ensure surveillance, follow-up, and care coordination.
Another limitation of our study is that data are from patients at a single academic medical center, limiting the generalizability of these results to other settings. In addition, only a single note from a medical provider at our institution was evaluated for this study, leaving the possibility that other notes could have mentioned topics related to psychosocial distress. However, we argue that these discussions should be occurring frequently, if not during each visit. Patients and their families may also be receiving social services outside our hospital system, especially given that many patients in the program do not live in the immediate vicinity of Mayo Clinic.
5. Conclusions
Children with rare or life-limiting chronic conditions and members of their families are at increased risk for the development of psychosocial distress, which, if left unidentified and untreated, can negatively impact the child and the family. The purpose of this research was to identify which elements of psychosocial distress and its antecedents are documented in the medical record, as well as their frequency and nature. While information related to family structure and patient school status was widely documented in our sample, many other important psychosocial domains (namely, child and family emotional function) were not routinely documented within medical provider notes. As these children continue to survive and live longer, they and their families may benefit from universal psychosocial screening, and an integrated medical and behavioral service model which could provide an evidence-based system of care encompassing more of the patient’s lived experience (Appendix A).
Author Contributions
Conceptualization, S.R.M., E.H.G., D.L.G., J.C., V.M.M. and A.J.; data curation, S.R.M., E.H.G. and D.L.G.; formal analysis, S.R.M., E.H.G., D.L.G. and J.E.C.; funding acquisition, S.R.M.; investigation, S.R.M., E.H.G., D.L.G. and J.E.C.; methodology, S.R.M., E.H.G., D.L.G. and V.M.M.; project administration, S.R.M.; resources, S.R.M., J.C., C.F., V.M.M. and A.J.; software, E.H.G. and D.L.G.; supervision, S.R.M., V.M.M. and A.J.; validation, S.R.M., E.H.G., D.L.G. and J.E.C.; visualization, S.R.M., E.H.G. and D.L.G.; writing—original draft, S.R.M., E.H.G., D.L.G. and V.M.M.; writing—review and editing, S.R.M., E.H.G., D.L.G., J.C., C.F., H.M., K.B., V.M.M. and A.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the Agency for Healthcare Research Quality (AHRQ) (K12HS026379) and Patient-Centered Outcomes Research Institute (PCORI) (K12HS026379) to Sarah Brand-McCarthy. The content is solely the responsibility of the authors and does not necessarily represent the official views of AHRQ, PCORI, or Minnesota Learning Health System Mentored Career Development Program.
Institutional Review Board Statement
The Mayo Clinic Institutional Review Board (IRB) reviewed this study and determined it to be exempt from continued IRB human subjects review because the research was limited to a retrospective review of electronic medical records.
Informed Consent Statement
Patient informed consent was waived in light of the retrospective nature of the data presented.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Appendix A

Table A1.
Coding Categories.
Table A1.
Coding Categories.
| Code | Definition |
|---|---|
| Emotional Function | Ability to regulate their emotional expression and identify emotional expressions of others. Trauma, mood problems, anxiety, depression, sadness, behavior problems, attention problems, ADHD, fear, aggression, past or current therapy, past or current psychiatric medication |
| Family Structure | Who lives in the home Single-parent home Who is involved in care |
| Financial Concerns | Transportation Insurance Parent’s ability to work Government assistance for food Money problems (phone, heat, light bills, rent/mortgage, medical bills, child care) Housing quality (evidence of overcrowding, frequent moves/evictions, health hazards e.g., mold) |
| Parent Ability to Navigate the Health System | Take time off to attend medical appointments, arrange child care, follow through on medical treatment plan |
| Parent Emotional Function | Coping, worry/anxiety, mood problems, depression/sadness, alcohol/drug abuse, avoidance, jumpy hypervigilance, disabling parent health concern, current therapy, past therapy |
| Parents’ Work Family Conflict | Difficult hours/shifts Part-time/full-time/unemployed Caregiver occupation/employment Mention of the interaction of caregivers’ work and subsequent stress or inability to care for child |
| Parent Social Support | Community, friends, partner, family |
| Sibling Emotional and Physical Function | Anxiety, mood concerns, disruptive behavior, current or past medical condition Sibling rivalry or conflict |
References
- Wong, L.-Y.C.; Paulozzi, L.J. Survival of infants with spina bifida: A population study, 1979–94. Paediatr. Peérinat. Epidemiol. 2001, 15, 374–378. [Google Scholar] [CrossRef]
- Msall, M.E.; Tremont, M.R. Measuring functional outcomes after prematurity: Developmental impact of very low birth weight and extremely low birth weight status on childhood disability. Ment. Retard. Dev. Disabil. Res. Rev. 2002, 8, 258–272. [Google Scholar] [CrossRef]
- Burns, K.H.; Casey, P.H.; Lyle, R.E.; Mac Bird, T.; Fussell, J.J.; Robbins, J.M. Increasing prevalence of medically complex children in US hospitals. Pediatrics 2010, 126, 638–646. [Google Scholar] [CrossRef] [Green Version]
- Tennant, P.; Pearce, M.; Bythell, M.; Rankin, J. 20-year survival of children born with congenital anomalies: A population-based study. Lancet 2010, 375, 649–656. [Google Scholar] [CrossRef]
- Feudtner, C.; Feinstein, J.A.; Zhong, W.; Hall, M.; Dai, D. Pediatric complex chronic conditions classification system version 2: Updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014, 14, 199. [Google Scholar] [CrossRef] [Green Version]
- Kazak, A.E.; Rourke, M.T.; Crump, T.A. Families and other systems in pediatric psychology. In Handbook of Pediatric Psychology; The Guilford Press: New York, NY, USA, 2003. [Google Scholar]
- Stille, C.J.; Antonelli, R.C. Coordination of care for children with special health care needs. Curr. Opin. Pediatr. 2004, 16, 700–705. [Google Scholar] [CrossRef] [Green Version]
- Cohen, E.; Kuo, D.Z.; Agrawal, R.; Berry, J.G.; Bhagat, S.K.M.; Simon, T.D.; Srivastava, R. Children with medical complexity: An emerging population for clinical and research initiatives. Pediatrics 2011, 127, 529–538. [Google Scholar] [CrossRef] [Green Version]
- Glendinning, C.; Kirk, S.; Guiffrida, A.E.; Lawton, D. Technology-dependent children in the community: Definitions, numbers and costs. Child Care Health Dev. 2001, 27, 321–334. [Google Scholar] [CrossRef] [Green Version]
- Thompson, J.R.; Carter, R.L.; Edwards, A.R.; Roth, J.; Ariet, M.; Ross, N.L.; Resnick, M.B. A population-based study of the effects of birth weight on early developmental delay or disability in children. Am. J. Perinatol. 2003, 20, 321–332. [Google Scholar] [CrossRef] [Green Version]
- Yeates, K.O.; Bigler, E.D.; Dennis, M.; Gerhardt, C.A.; Rubin, K.H.; Stancin, T.; Taylor, H.G.; Vannatta, K. Social outcomes in childhood brain disorder: A heuristic integration of social neuroscience and developmental psychology. Psychol. Bull. 2007, 133, 535–556. [Google Scholar] [CrossRef]
- Merikangas, K.R.; Calkins, M.E.; Burstein, M.; He, J.-P.; Chiavacci, R.; Lateef, T.; Ruparel, K.; Gur, R.C.; Lehner, T.; Hakonarson, H.; et al. Comorbidity of physical and mental disorders in the neurodevelopmental genomics cohort study. Pediatrics 2015, 135, e927–e938. [Google Scholar] [CrossRef] [Green Version]
- Barker, M.M.; Beresford, B.; Bland, M.; Fraser, L.K. Prevalence and incidence of anxiety and depression among children, adolescents, and young adults with life-limiting conditions: A systematic review and meta-analysis. JAMA Pediatr. 2019, 173, 835–844. [Google Scholar] [CrossRef]
- Spitzer, R.L. Health-related quality of life in primary care patients with mental disorders. Results from the PRIME-MD 1000 Study. JAMA 1995, 274, 1511–1517. [Google Scholar] [CrossRef]
- Smith, B.A.; Modi, A.C.; Quittner, A.L.; Wood, B.L. Depressive symptoms in children with cystic fibrosis and parents and its effects on adherence to airway clearance. Pediatr. Pulmonol. 2010, 45, 756–763. [Google Scholar] [CrossRef]
- Pulgar, Á.; Garrido, S.; Alcala, A.; Del Paso, G.A.R. Psychosocial predictors of immune response following bone marrow transplantation. Behav. Med. 2012, 38, 12–18. [Google Scholar] [CrossRef]
- Snell, C.; Fernandes, S.; Bujoreanu, I.S.; Garcia, G. Depression, illness severity, and healthcare utilization in cystic fibrosis. Pediatr. Pulmonol. 2014, 49, 1177–1181. [Google Scholar] [CrossRef]
- Adams, L.S.; Miller, J.L.; Grady, P.A. The spectrum of caregiving in palliative care for serious, advanced, rare diseases: Key issues and research directions. J. Palliat. Med. 2016, 19, 698–705. [Google Scholar] [CrossRef] [Green Version]
- Schuster, M.A.; Chung, P.J.; Vestal, K.D. Children with health issues. Future Child. 2011, 21, 91–116. [Google Scholar] [CrossRef]
- Thomson, J.; Shah, S.S.; Simmons, J.M.; Sauers, H.; Brunswick, S.; Hall, D.; Kahn, R.S.; Beck, A.F. Financial and social hardships in families of children with medical complexity. J. Pediatr. 2016, 172, 187–193. [Google Scholar] [CrossRef] [Green Version]
- Pelentsov, L.J.; Fielder, A.L.; Esterman, A.J. The supportive care needs of parents with a child with a rare disease: A qualitative descriptive study. J. Pediatr. Nurs. 2016, 31, e207–e218. [Google Scholar] [CrossRef]
- Pelentsov, L.J.; Laws, T.A.; Esterman, A.J. The supportive care needs of parents caring for a child with a rare disease: A scoping review. Disabil. Health J. 2015, 8, 475–491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bayer, N.D.; Wang, H.; Yu, J.A.; Kuo, D.Z.; Halterman, J.S.; Li, Y. A national mental health profile of parents of children with medical complexity. Pediatrics 2021, 148, e2020023358. [Google Scholar] [CrossRef] [PubMed]
- Hatzmann, J.; Heymans, H.S.A.; Ferrer-I-Carbonell, A.; van Praag, B.M.S.; Grootenhuis, M.A. Hidden consequences of success in pediatrics: Parental health-related quality of life—results from the care project. Pediatrics 2008, 122, e1030–e1038. [Google Scholar] [CrossRef] [PubMed]
- Kazak, A.E.; Holmbeck, G.N.; Gorey-Ferguson, L.; Hudson, T.; Sefeldt, T.; Shapera, W.; Turner, T.; Uhler, J. Maternal, paternal, and marital functioning in families of preadolescents with spina bifida. J. Pediatr. Psychol. 1997, 22, 167–181. [Google Scholar] [CrossRef]
- Pelentsov, L.J.; Fielder, A.L.; Laws, T.A.; Esterman, A.J. The supportive care needs of parents with a child with a rare disease: Results of an online survey. BMC Fam. Pract. 2016, 17, 88. [Google Scholar] [CrossRef] [Green Version]
- Kuo, D.Z. A national profile of caregiver challenges among more medically complex children with special health care needs. Arch. Pediatr. Adolesc. Med. 2011, 165, 1020–1026. [Google Scholar] [CrossRef]
- Collins, A.; Hennessy-Anderson, N.; Hosking, S.; Hynson, J.; Remedios, C.; Thomas, K. Lived experiences of parents caring for a child with a life-limiting condition in Australia: A qualitative study. Palliat. Med. 2016, 30, 950–959. [Google Scholar] [CrossRef]
- Ratliffe, C.E.; Harrigan, R.C.; Haley, J.; Tse, A.; Olson, T. Stress in families with medically fragile children. Issues Compr. Pediatr. Nurs. 2002, 25, 167–188. [Google Scholar] [CrossRef]
- Dew, M.A.; Dabbs, A.D.; Myaskovsky, L.; Shyu, S.; Shellmer, D.A.; DiMartini, A.F.; Steel, J.; Unruh, M.; Switzer, G.E.; Shapiro, R.; et al. Meta-analysis of medical regimen adherence outcomes in pediatric solid organ transplantation. Transplantation 2009, 88, 736–746. [Google Scholar] [CrossRef] [Green Version]
- Bakula, D.M.; Sharkey, C.M.; Perez, M.N.; Espeleta, H.C.; Gamwell, K.; Baudino, M.; DeLozier, A.M.; Chaney, J.M.; Alderson, R.M.; Mullins, L.L. Featured article: The relationship between parent and child distress in pediatric cancer: A meta-analysis. J. Pediatr. Psychol. 2019, 44, 1121–1136. [Google Scholar] [CrossRef]
- Cohen, J.S.; Biesecker, B.B. Quality of life in rare genetic conditions: A systematic review of the literature. Am. J. Med. Genet. Part A 2010, 152A, 1136–1156. [Google Scholar] [CrossRef] [PubMed]
- Haverman, L.; van Oers, H.A.; Limperg, P.F.; Houtzager, B.A.; Huisman, J.; Darlington, A.-S.; Maurice-Stam, H.; Grootenhuis, M.A. Development and validation of the distress thermometer for parents of a chronically ill child. J. Pediatr. 2013, 163, 1140–1146. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kazak, A.E. Pediatric Psychosocial Preventative Health Model (PPPHM): Research, practice, and collaboration in pediatric family systems medicine. Fam. Syst. Health 2006, 24, 381–395. [Google Scholar] [CrossRef] [Green Version]
- Kazak, A.E.; Barakat, L.P.; Askins, M.A.; McCafferty, M.; Lattomus, A.; Ruppe, N.; Deatrick, J. Provider perspectives on the implementation of psychosocial risk screening in pediatric cancer. J. Pediatr. Psychol. 2017, 42, 700–710. [Google Scholar] [CrossRef]
- Kazak, A.E.; Hwang, W.-T.; Chen, F.F.; Askins, M.A.; Carlson, O.; Argueta-Ortiz, F.; Barakat, L.P. Screening for Family Psychosocial Risk in Pediatric Cancer: Validation of the Psychosocial Assessment Tool (PAT) Version 3. J. Pediatr. Psychol. 2018, 43, 737–748. [Google Scholar] [CrossRef] [PubMed]
- Patel, D.; Sharpe, L.; Thewes, B.; Bell, M.L.; Clarke, S. Using the distress thermometer and hospital anxiety and depression scale to screen for psychosocial morbidity in patients diagnosed with colorectal cancer. J. Affect. Disord. 2011, 131, 412–416. [Google Scholar] [CrossRef]
- Patel, S.K.; Kim, S.; Johansen, C.; Mullins, W.; Nolty, A.; Fernandez, N.; Delgado, N.; Folbrecht, J.; Dekel, N.; Meier, A. Threshold score for the self-report Pediatric Distress Thermometer Rating Scale in childhood cancer patients. Psycho-Oncology 2020, 30, 340–348. [Google Scholar] [CrossRef]
- Wiener, L.; Battles, H.B.; Zadeh, S.; Widemann, B.C.; Pao, M. Validity, specificity, feasibility and acceptability of a brief pediatric distress thermometer in outpatient clinics. Psycho-Oncology 2015, 26, 461–468. [Google Scholar] [CrossRef] [Green Version]
- Wiener, L.; Battles, H.; Bedoya, S.Z.; Baldwin, A.; Widemann, B.C.; Pao, M. Identifying Symptoms of Distress in Youth Living with Neurofibromatosis Type 1 (NF1). J. Genet. Couns. 2017, 27, 115–123. [Google Scholar] [CrossRef]
- Callahan, S.T.; Cooper, W.O. Access to Health Care for Young Adults with Disabling Chronic Conditions. Arch. Pediatr. Adolesc. Med. 2006, 160, 178–182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Busack, C.; Daskalakis, C.; Rosen, P. Physician and Parent Perspectives on Psychosocial and Emotional Data Entry in the Electronic Medical Record in a Pediatric Setting. J. Patient Exp. 2016, 3, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Haverman, L.; van Oers, H.A.; Limperg, P.F.; Hijmans, C.T.; Schepers, S.A.; Nicolaas, S.M.S.; Verhaak, C.M.; Bouts, A.H.M.; Fijnvandraat, K.; Peters, M.; et al. Implementation of electronic patient reported outcomes in pediatric daily clinical practice: The KLIK experience. Clin. Pract. Pediatr. Psychol. 2014, 2, 50–67. [Google Scholar] [CrossRef]
- Boat, T.F.; Land, M.L., Jr.; Leslie, L.K. Health Care Workforce Development to Enhance Mental and Behavioral Health of Children and Youths. JAMA Pediatr. 2017, 171, 1031–1032. [Google Scholar] [CrossRef] [PubMed]
- Kazak, A.E.; Rourke, M.T.; Alderfer, M.A.; Pai, A.; Reilly, A.F.; Meadows, A.T. Evidence-based Assessment, Intervention and Psychosocial Care in Pediatric Oncology: A Blueprint for Comprehensive Services Across Treatment. J. Pediatr. Psychol. 2007, 32, 1099–1110. [Google Scholar] [CrossRef] [Green Version]
- Engelen, V.; van Zwieten, M.; Koopman, H.; Detmar, S.; Caron, H.; Brons, P.; Egeler, M.; Kaspers, G.-J.; Grootenhuis, M. The influence of patient reported outcomes on the discussion of psychosocial issues in children with cancer. Pediatr. Blood Cancer 2012, 59, 161–166. [Google Scholar] [CrossRef]
- Patel, S.K.; Fernandez, N.; Wong, A.L.; Mullins, W.; Turk, A.; Dekel, N.; Smith, M.; Ferrell, B. Changes in self-reported distress in end-of-life pediatric cancer patients and their parents using the pediatric distress thermometer. Psycho-Oncology 2014, 23, 592–596. [Google Scholar] [CrossRef]
- Wiener, L.; Bedoya, S.Z. Checking in: A new generation electronic screening tool for pediatric and adolescents in outpatient settings. Psycho-Oncology 2021, 30, 20. [Google Scholar]
- Pai, A.L.; Tackett, A.; Ittenbach, R.F.; Goebel, J. Psychosocial Assessment Tool 2.0 _General: Validity of a psychosocial risk screener in a pediatric kidney transplant sample. Pediatr. Transplant. 2012, 16, 92–98. [Google Scholar] [CrossRef]
- Pierce, L.; Hocking, M.; Schwartz, L.A.; Alderfer, M.A.; Kazak, A.E.; Barakat, L.P. Caregiver distress and patient health-related quality of life: Psychosocial screening during pediatric cancer treatment. Psycho-Oncology 2016, 26, 1555–1561. [Google Scholar] [CrossRef]
- Bauwens, S.; Baillon, C.; Distelmans, W.; Theuns, P. Systematic screening for distress in oncology practice using the Distress Barometer: The impact on referrals to psychosocial care. Psycho-Oncology 2014, 23, 804–811. [Google Scholar] [CrossRef] [PubMed]
- Berger-Jenkins, E.; Monk, C.; D’Onfro, K.; Sultana, M.; Brandt, L.; Ankam, J.; Vazquez, N.; Lane, M.; Meyer, D. Screening for Both Child Behavior and Social Determinants of Health in Pediatric Primary Care. J. Dev. Behav. Pediatr. 2019, 40, 415–424. [Google Scholar] [CrossRef] [PubMed]
- Anderson, L.M.; Papadakis, J.L.; Vesco, A.T.; Shapiro, J.B.; Feldman, M.A.; Evans, M.A.; Weissberg-Benchell, J. Patient-Reported and Parent Proxy-Reported Outcomes in Pediatric Medical Specialty Clinical Settings: A Systematic Review of Implementation. J. Pediatr. Psychol. 2019, 45, 247–265. [Google Scholar] [CrossRef] [PubMed]
- Lyon, M.E.; Thompkins, J.D.; Fratantoni, K.; Fraser, J.L.; Schellinger, S.E.; Briggs, L.; Friebert, S.; Aoun, S.; Cheng, Y.I.; Wang, J. Family caregivers of children and adolescents with rare diseases: A novel palliative care intervention. BMJ Support. Palliat. Care 2019. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).