Sensitivity to Pain Traumatization and Its Relationship to the Anxiety–Pain Connection in Youth with Chronic Pain: Implications for Treatment
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.1.1. Inclusion Criteria
2.1.2. Exclusion Criteria
2.2. Procedure
2.3. Measures
2.3.1. Sensitivity to Pain Traumatization Scale—Child Version (SPTS-C)
2.3.2. Youth Daily Survey
2.4. Data Preparation
2.5. Statistical Analyses
2.5.1. Model 1: Pain Intensity
2.5.2. Model 2: Pain Unpleasantness
2.5.3. Model 3: Pain Interference
3. Results
3.1. Descriptive Statistics
3.2. Tests of Multivariate Assumptions
3.3. Multiple Linear Regression Results
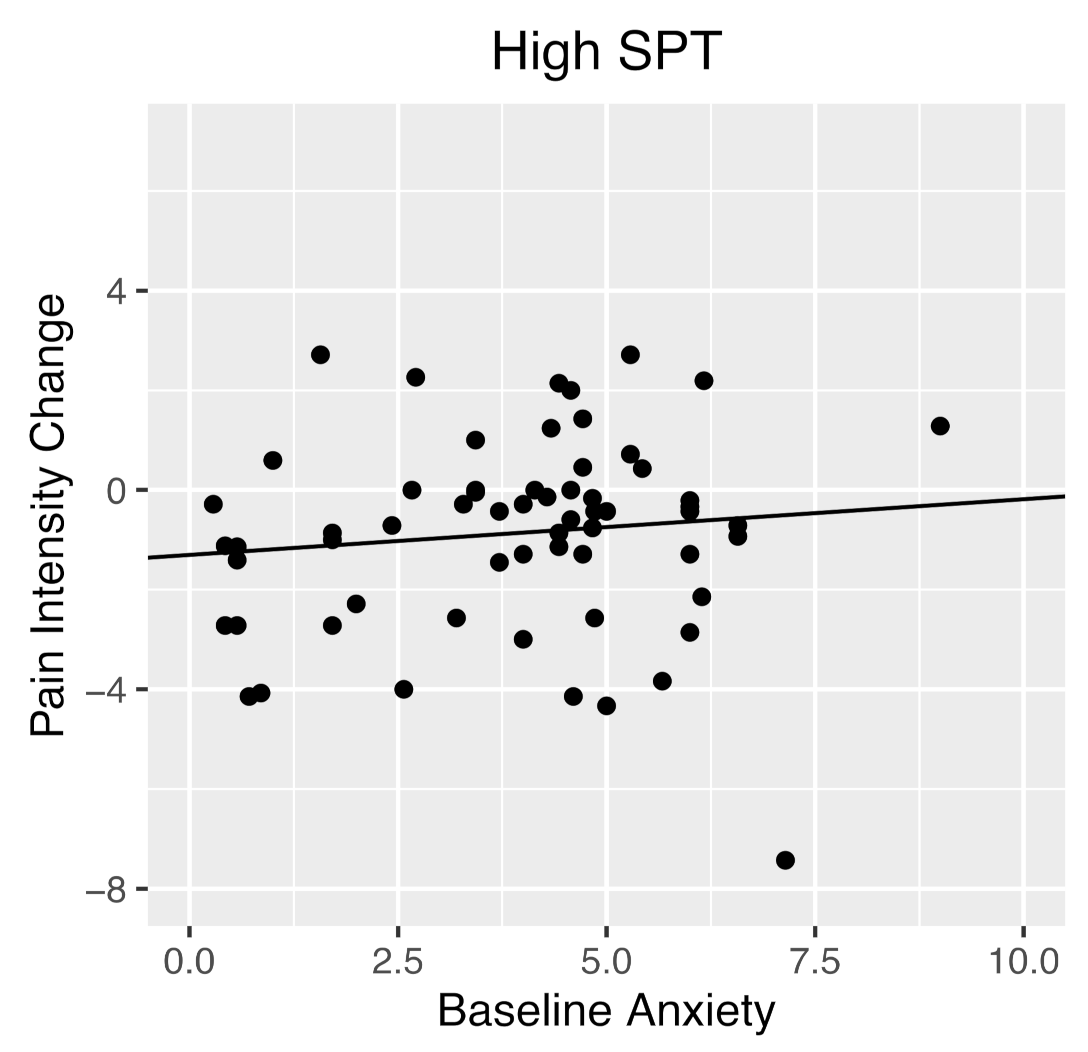
3.3.1. Model 1: Pain Intensity
3.3.2. Model 2: Pain Unpleasantness
3.3.3. Model 3: Pain Interference
3.4. Multilevel Model Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- King, S.; Chambers, C.T.; Huguet, A.; MacNevin, R.C.; McGrath, P.J.; Parker, L.; MacDonald, A.J. The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain 2011, 152, 2729–2738. [Google Scholar] [CrossRef] [PubMed]
- Sato, A.F.; Hainsworth, K.R.; Khan, K.A.; Ladwig, R.J.; Weisman, S.J.; Davies, W.H. School absenteeism in pediatric chronic pain: Identifying lessons learned from the general school absenteeism literature. Child. Healthc. 2007, 36, 355–372. [Google Scholar] [CrossRef]
- Meldrum, M.L.; Tsao, J.C.; Zeltzer, L.K. “Just be in pain and just move on”: Functioning limitations and strategies in the lives of children with chronic pain. J. Pain Manag. 2008, 1, 131. [Google Scholar]
- Huguet, A.; Miró, J. The severity of chronic pediatric pain: An epidemiological study. J. Pain 2008, 9, 226–236. [Google Scholar] [CrossRef]
- Fearon, P.; Hotopf, M. Relation between headache in childhood and physical and psychiatric symptoms in adulthood: National birth cohort study. BMJ 2001, 322, 1145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vinall, J.; Pavlova, M.; Asmundson, G.J.; Rasic, N.; Noel, M. Mental health comorbidities in pediatric chronic pain: A narrative review of epidemiology, models, neurobiological mechanisms and treatment. Children 2016, 3, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cornwall, A.; Donderi, D. The effect of experimentally induced anxiety on the experience of pressure pain. Pain 1988, 35, 105–113. [Google Scholar] [CrossRef] [Green Version]
- Benore, E.; D’Auria, A.; Banez, G.A.; Worley, S.; Tang, A. The influence of anxiety reduction on clinical response to pediatric chronic pain rehabilitation. Clin. J. Pain 2015, 31, 375–383. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, K.R.R.; France, R.D.; Pelton, S.; McCann, U.D.; Davidson, J.; Urban, B.J. Chronic pain and depression. II. Symptoms of anxiety in chronic low back pain patients and their relationship to subtypes of depression. Pain 1985, 22, 289–294. [Google Scholar] [CrossRef]
- Asmundson, G.J.; Katz, J. Understanding the co-occurrence of anxiety disorders and chronic pain: State-of-the-art. Depress. Anxiety 2009, 26, 888–901. [Google Scholar] [CrossRef] [PubMed]
- Jordan, K.D.; Okifuji, A. Anxiety disorders: Differential diagnosis and their relationship to chronic pain. J. Pain Palliat. Care Pharmacother. 2011, 25, 231–245. [Google Scholar] [CrossRef] [PubMed]
- Knook, L.M.E.; Konijnenberg, A.Y.; van der Hoeven, J.; Kimpen, J.L.L.; Buitelaar, J.K.; van Engeland, H.; de Graeff-Meeder, E.R. Psychiatric disorders in children and adolescents presenting with unexplained chronic pain: What is the prevalence and clinical relevancy? Eur. Child Adolesc. Psychiatry 2011, 20, 39–48. [Google Scholar] [CrossRef] [Green Version]
- Kashikar-Zuck, S.; Parkins, I.S.; Graham, T.B.; Lynch, A.M.; Passo, M.; Johnston, M.; Schikler, K.N.; Hashkes, P.J.; Banez, G.; Richards, M.M. Anxiety, mood, and behavioral disorders among pediatric patients with juvenile fibromyalgia syndrome. Clin. J. Pain 2008, 24, 620–626. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campo, J.V.; Bridge, J.; Ehmann, M.; Altman, S.; Lucas, A.; Birmaher, B.; Lorenzo, C.D.; Iyengar, S.; Brent, D.A. Recurrent abdominal pain, anxiety, and depression in primary care. Pediatrics 2004, 113, 817–824. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rogers, A.H.; Bakhshaie, J.; Ditre, J.W.; Manning, K.; Mayorga, N.A.; Viana, A.G.; Zvolensky, M.J. Worry and rumination: Explanatory roles in the relation between pain and anxiety and depressive symptoms among college students with pain. J. Am. Coll. Health 2019, 67, 275–282. [Google Scholar] [CrossRef]
- Kleiman, V.; Clarke, H.; Katz, J. Sensitivity to pain traumatization: A higher-order factor underlying pain-related anxiety, pain catastrophizing and anxiety sensitivity among patients scheduled for major surgery. Pain Res. Manag. 2011, 16, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Katz, J.; Fashler, S.R.; Wicks, C.; Pagé, M.G.; Roosen, K.M.; Kleiman, V.; Clarke, H. Sensitivity to Pain Traumatization Scale: Development, validation, and preliminary findings. J. Pain Res. 2017, 10, 1297. [Google Scholar] [CrossRef] [Green Version]
- Pavlova, M.; Beveridge, J.; Soltani, S.; Maunder, L.; Salomons, T.; Katz, J.; Noel, M. The sensitivity to pain traumatization scale-child version (SPTS-C): Development and preliminary validation. Article Submitted for Publication 2022. [Google Scholar]
- Engelhard, I.M.; van den Hout, M.A.; Kindt, M. The relationship between neuroticism, pre-traumatic stress, and post-traumatic stress: A prospective study. Personal. Individ. Differ. 2003, 35, 381–388. [Google Scholar] [CrossRef]
- Guo, W.; Xue, J.-M.; Shao, D.; Long, Z.-T.; Cao, F.-L. Effect of the interplay between trauma severity and trait neuroticism on posttraumatic stress disorder symptoms among adolescents exposed to a pipeline explosion. PLoS ONE 2015, 10, e0120493. [Google Scholar] [CrossRef] [PubMed]
- Pagé, M.G.; Stinson, J.; Campbell, F.; Isaac, L.; Katz, J. Identification of pain-related psychological risk factors for the development and maintenance of pediatric chronic postsurgical pain. J. Pain Res. 2013, 6, 167–180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beveridge, J.K.; Pavlova, M.; Katz, J.; Noel, M. The Parent Version of the Sensitivity to Pain Traumatization Scale (SPTS-P): A preliminary validation. Children 2021, 8, 537. [Google Scholar] [CrossRef] [PubMed]
- Nelson, S.; Beveridge, J.K.; Mychasiuk, R.; Noel, M. Adverse childhood experiences (ACEs) and internalizing mental health, pain, and quality of life in youth with chronic pain: A longitudinal examination. J. Pain 2021, 22, 1210–1220. [Google Scholar] [CrossRef] [PubMed]
- Neville, A.; Griep, Y.; Palermo, T.M.; Vervoort, T.; Schulte, F.; Yeates, K.O.; Sumpton, J.E.; Mychasiuk, R.; Noel, M. A “dyadic dance”: Pain catastrophizing moderates the daily relationships between parent mood and protective responses and child chronic pain. Pain 2020, 161, 1072–1082. [Google Scholar] [CrossRef] [PubMed]
- Neville, A.; Kopala-Sibley, D.C.; Soltani, S.; Asmundson, G.J.; Jordan, A.; Carleton, R.N.; Yeates, K.O.; Schulte, F.; Noel, M. A longitudinal examination of the interpersonal fear avoidance model of pain: The role of intolerance of uncertainty. Pain 2021, 162, 152–160. [Google Scholar] [CrossRef]
- Pavlova, M.; Kopala-Sibley, D.C.; Nania, C.; Mychasiuk, R.; Christensen, J.; McPeak, A.; Tomfohr-Madsen, L.; Katz, J.; Palermo, T.M.; Noel, M. Sleep disturbance underlies the co-occurrence of trauma and pediatric chronic pain: A longitudinal examination. Pain 2020, 161, 821–830. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crandall, M.; Lammers, C.; Senders, C.; Savedra, M.; Braun, J.V. Initial validation of a numeric zero to ten scale to measure children's state anxiety. Anesth. Analg. 2007, 105, 1250–1253. [Google Scholar] [CrossRef] [PubMed]
- Castarlenas, E.; Jensen, M.P.; von Baeyer, C.L.; Miró, J. Psychometric properties of the numerical rating scale to assess self-reported pain intensity in children and adolescents. Clin. J. Pain 2017, 33, 376–383. [Google Scholar] [CrossRef]
- Pagé, M.G.; Katz, J.; Stinson, J.; Isaac, L.; Martin-Pichora, A.L.; Campbell, F. Validation of the numerical rating scale for pain intensity and unpleasantness in pediatric acute postoperative pain: Sensitivity to change over time. J. Pain 2012, 13, 359–369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palermo, T.M.; Valenzuela, D.; Stork, P.P. A randomized trial of electronic versus paper pain diaries in children: Impact on compliance, accuracy, and acceptability. Pain 2004, 107, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Noel, M.; Rabbitts, J.A.; Tai, G.G.; Palermo, T.M. Remembering pain after surgery: A longitudinal examination of the role of pain catastrophizing in children’s and parents’ recall. Pain 2015, 156, 800. [Google Scholar] [CrossRef]
- Varni, J.W.; Stucky, B.D.; Thissen, D.; DeWitt, E.M.; Irwin, D.; Lai, J.-S.; Yeatts, K.; DeWalt, D.A. PROMIS Pediatric Pain Interference Scale: An item response theory analysis of the Pediatric Pain Item Bank. J. Pain 2010, 11, 1109–1119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kashikar-Zuck, S.; Carle, A.; Barnett, K.; Goldschneider, K.R.; Sherry, D.D.; Mara, C.A.; Cunningham, N.; Farrell, J.; Tress, J.; DeWitt, E.M. Longitudinal evaluation of Patient Reported Outcomes Measurement Information Systems (PROMIS) measures in pediatric chronic pain. Pain 2016, 157, 339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aiken, L.; West, S. Multiple Regression: Testing and Interpreting Interactions; Sage: Thousand Oaks, CA, USA, 1991. [Google Scholar]
- Johnson, P.O.; Fay, L.C. The Johnson-Neyman technique, its theory and application. Psychometrika 1950, 15, 349–367. [Google Scholar] [CrossRef] [PubMed]
- Scholz, J.; Woolf, C.J. Can we conquer pain? Nat. Neurosci. 2002, 5, 1062–1067. [Google Scholar] [CrossRef] [PubMed]
- Foa, E.B.; Kozak, M.J. Emotional processing of fear: Exposure to corrective information. Psychol. Bull. 1986, 99, 20. [Google Scholar] [CrossRef]
- Bosco, M.A.; Gallinati, J.L.; Clark, M.E. Conceptualizing and treating comorbid chronic pain and PTSD. Pain Res. Treat. 2013, 2013, 174728. [Google Scholar] [CrossRef]
- Simons, L.E.; Vlaeyen, J.W.; Declercq, L.; Smith, A.M.; Beebe, J.; Hogan, M.; Li, E.; Kronman, C.A.; Mahmud, F.; Corey, J.R. Avoid or engage? Outcomes of graded exposure in youth with chronic pain using a sequential replicated single-case randomized design. Pain 2020, 161, 520–531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holley, A.; Wilson, A.; Noel, M.; Palermo, T. Post-traumatic stress symptoms in children and adolescents with chronic pain: A topical review of the literature and a proposed framework for future research. Eur. J. Pain 2016, 20, 1371–1383. [Google Scholar] [CrossRef] [Green Version]
- Borgers, N.; de Leeuw, E.; Hox, J. Children as respondents in survey research: Cognitive development and response quality 1. Bull. Sociol. Methodol./Bull. Méthodologie Sociol. 2000, 66, 60–75. [Google Scholar] [CrossRef]
- Pinheiro, J.; Bates, D.; DebRoy, S.; Sarkar, D.; R Core Team. Nlme: Linear and Nonlinear Mixed Effects Models. R Package Version 3.1-153. 2021. Available online: https://CRAN.R-project.org/package=nlme (accessed on 23 February 2022).

| Characteristic | Percentage | Number |
|---|---|---|
| Age, M = 14.21 years, SD = 2.23, range = 10–18 | ||
| Gender | ||
| Girl | 71 | 130 |
| Boy | 25 | 46 |
| Nondisclosed | 4 | 8 |
| Race/Ethnicity | ||
| White | 79 | 145 |
| Bi- or multiracial | 8 | 14 |
| Other or declined to answer | 4 | 8 |
| Arab/West Asian | 2 | 4 |
| Black | 2 | 3 |
| South Asian | 2 | 3 |
| Latin American | 1 | 2 |
| Indigenous | 1 | 2 |
| Filipino | <1 | 1 |
| Pain duration, M = 2.69 years, SD = 3.04, range = 0.25–12 | ||
| Pain locations * | ||
| Head | 72 | 126 |
| Other | 25 | 43 |
| Muscle and joints | 24 | 42 |
| Stomach | 18 | 32 |
| Legs | 14 | 25 |
| Chest | 11 | 19 |
| Characteristic | Baseline (Time 1) | Time 2 | ||
|---|---|---|---|---|
| Mean (SD) | Sample Range | Mean (SD) | Sample Range | |
| Anxiety | 3.22 (2.11) | 0–9 | - | - |
| Pain Intensity | 4.55 (2.29) | 0–8.71 | 3.92 (2.52) | 0–9.43 |
| Pain Unpleasantness | 1.61 (0.77) | 0–3.57 | 1.36 (0.84) | 0–3.57 |
| Pain Interference | 5.09 (4.02) | 0–15.83 | 4.35 (4.13) | 0–16 |
| Baseline Anxiety | Baseline Pain Intensity | Baseline Pain Unpleasantness | Baseline Pain Interference | Baseline SPT | Time 2 Pain Intensity | Time 2 Pain Unpleasantness | Time 2 Pain Interference | |
|---|---|---|---|---|---|---|---|---|
| Baseline anxiety | 1 | |||||||
| Baseline pain intensity | 0.39 | 1 | ||||||
| Baseline pain unpleasantness | 0.3 | 0.73 | 1 | |||||
| Baseline pain interference | 0.40 | 0.58 | 0.68 | 1 | ||||
| Baseline SPT | 0.37 | 0.28 | 0.37 | 0.47 | 1 | |||
| Time 2 pain intensity | 0.34 | 0.70 | 0.57 | 0.49 | 0.28 | 1 | ||
| Time 2 pain unpleasantness | 0.42 | 0.45 | 0.6 | 0.55 | 0.39 | 0.74 | 1 | |
| Time 2 pain interference | 0.32 | 0.35 | 0.43 | 0.73 | 0.36 | 0.55 | 0.62 | 1 |
| Pain Measure | ||
|---|---|---|
| Predictor | Adj. R2 | b |
| Model 1 | 0.48 *** | |
| Pain intensity | 0.69 *** | |
| Baseline anxiety | –0.15 | |
| SPT | –0.059 | |
| Baseline anxiety x SPT | 0.02 * | |
| n | ||
| Model 2 | 0.41 *** | |
| Pain unpleasantness | 0.10 *** | |
| Baseline anxiety | 0.005 | |
| SPT | –0.002 | |
| Baseline anxiety x SPT | 0.001 | |
| n | ||
| Model 3 | 0.47 *** | |
| Pain interference | 0.058 *** | |
| Baseline anxiety | –0.058 | |
| SPT | –0.018 | |
| Baseline anxiety x SPT | 0.025 | |
| n | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maunder, L.; Pavlova, M.; Beveridge, J.K.; Katz, J.; Salomons, T.V.; Noel, M. Sensitivity to Pain Traumatization and Its Relationship to the Anxiety–Pain Connection in Youth with Chronic Pain: Implications for Treatment. Children 2022, 9, 529. https://doi.org/10.3390/children9040529
Maunder L, Pavlova M, Beveridge JK, Katz J, Salomons TV, Noel M. Sensitivity to Pain Traumatization and Its Relationship to the Anxiety–Pain Connection in Youth with Chronic Pain: Implications for Treatment. Children. 2022; 9(4):529. https://doi.org/10.3390/children9040529
Chicago/Turabian StyleMaunder, Larah, Maria Pavlova, Jaimie K. Beveridge, Joel Katz, Tim V. Salomons, and Melanie Noel. 2022. "Sensitivity to Pain Traumatization and Its Relationship to the Anxiety–Pain Connection in Youth with Chronic Pain: Implications for Treatment" Children 9, no. 4: 529. https://doi.org/10.3390/children9040529
APA StyleMaunder, L., Pavlova, M., Beveridge, J. K., Katz, J., Salomons, T. V., & Noel, M. (2022). Sensitivity to Pain Traumatization and Its Relationship to the Anxiety–Pain Connection in Youth with Chronic Pain: Implications for Treatment. Children, 9(4), 529. https://doi.org/10.3390/children9040529








