Identification of Factors Influencing Cholesterol Changes in Elementary-School Children: A Longitudinal Study
Abstract
1. Introduction
2. Materials and Methods
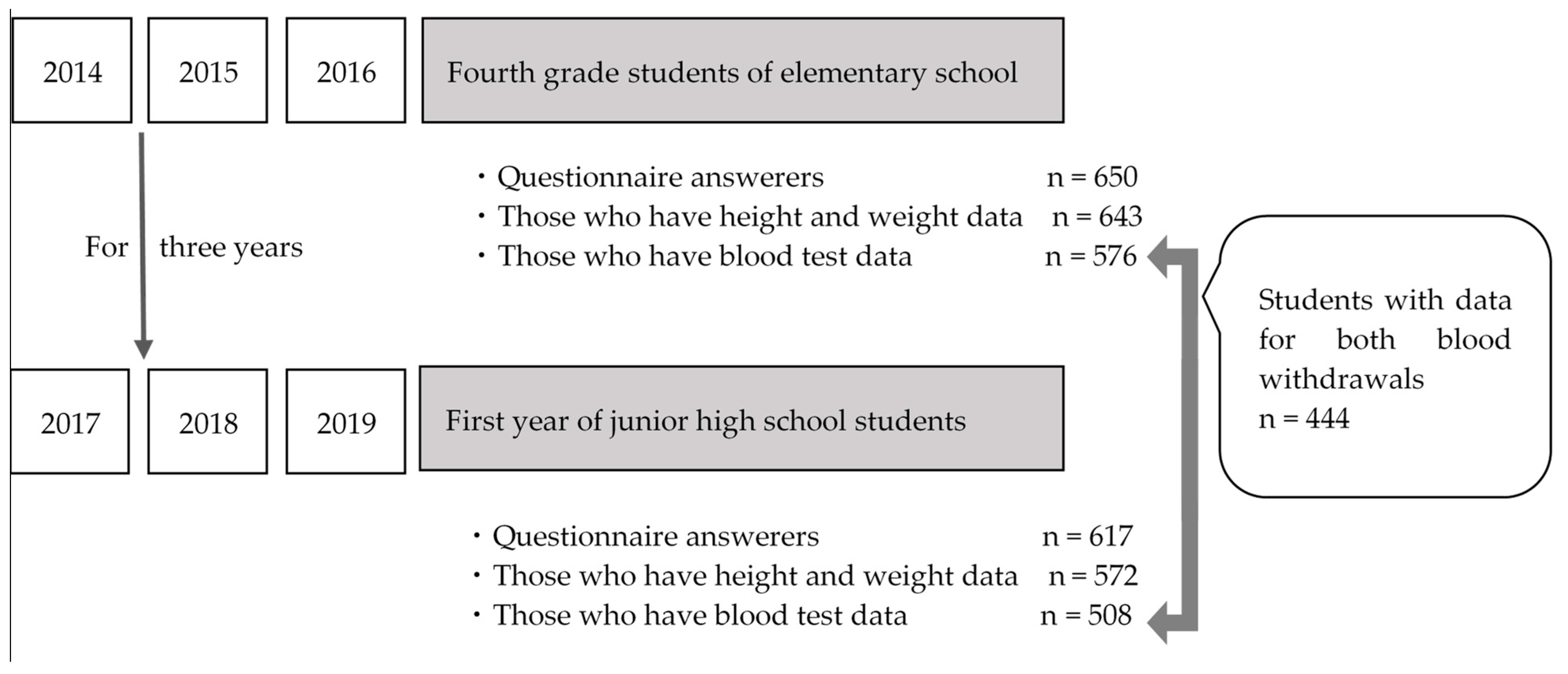
2.1. Study Participants
2.2. Study Survey
2.3. Data Overview
2.4. Statistical Analysis
3. Results
3.1. Demographic Characteristics of the Study Participants
3.2. Longitudinal Cholesterol Level Changes and Their Relationship with Demographic and Lifestyle Characteristics
3.3. Correlation of Cholesterol Levels and Changes with Growth- and Weight-Related Factors
3.4. Factors Predicting Changes in Cholesterol Levels Revealed by Multivariable Regression Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mangili, L. High prevalence of dyslipidemia in children and adolescents: Opportunity for prevention. Arq. Bras. Cardiol. 2020, 114, 57–58. [Google Scholar] [PubMed]
- Kihara, A.; Kawasaki, H.; Yamasaki, S.; Nishiyama, M.; Rahman, M. Factors affecting children’s cholesterol levels with a view to prevent cardiovascular disease-the unique benefits of health screening at the elementary school. Health 2017, 9, 172–188. [Google Scholar] [CrossRef][Green Version]
- Kouda, K.; Nakamura, H.; Tokunaga, R.; Takeuchi, H. Trends in levels of cholesterol in Japanese children from 1993 through 2001. J Epidemiol. 2004, 14, 78–82. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kouda, K.; Iki, M.; Fujita, Y.; Nakamura, H.; Ohara, K.; Tachiki, T.; Nishiyama, T. Trends in serum lipid levels of a 10- and 13-year-old population in Fukuroi City, Japan (2007–2017). J. Epidemiol. 2020, 30, 7724–7729. [Google Scholar] [CrossRef]
- Perak, A.M.; Ning, H.; Kit, B.K.; de Ferranti, S.D.; Van Horn, L.V.; Wilkins, J.T.; Lloyd-Jones, D.M. Trends in levels of lipids and apolipoprotein B in US youths aged 6 to 19 years, 1999–2016. JAMA 2019, 321, 1895–1905. [Google Scholar] [CrossRef]
- de Ferranti, S.D. Declining cholesterol levels in US youths: A reason for optimism. JAMA 2012, 308, 621–622. [Google Scholar] [CrossRef]
- Nguyen, D.; Kit, B.; Carroll, M. Abnormal cholesterol among children and adolescents in the United States, 2011–2014. NCHS Data Brief 2015, 228, 1–8. [Google Scholar]
- Wiegman, A.; Gidding, S.S.; Watts, G.F.; Chapman, M.J.; Ginsberg, H.N.; Cuchel, M.; Ose, L.; Averna, M.; Boileau, C.; Borén, J.; et al. Familial hypercholesterolaemia in children and adolescents: Gaining decades of life by optimizing detection and treatment. Eur. Heart J. 2015, 36, 2425–2437. [Google Scholar] [CrossRef]
- Wang, L.; Jansen, W.; van Grieken, A.; Vlasblom, E.; Boere-Boonekamp, M.M.; L’Hoir, M.P.; Raat, H. Identifying patterns of lifestyle behaviours among children of 3 years old. Eur. J. Public Health 2020, 30, 1115–1121. [Google Scholar] [CrossRef]
- Daily Life of an Elementary School Pupil in Japan. Available online: https://www.nier.go.jp/English/educationjapan/pdf/201403DLE.pdf (accessed on 13 December 2021).
- Tanaka, H.; Morisaki, N.; Piedvache, A.; Harada, S.; Urayama, K.Y. Trends in obesity and blood lipid abnormalities in school-age children in Japan. Pediatrics Int. 2021, 63, 825–832. [Google Scholar] [CrossRef]
- Okuda, M.; Sugiyama, S.; Kunitsugu, I.; Hinoda, Y.; Okuda, Y.; Shirabe, K.; Yoshitake, N.; Hobara, T. Use of body mass index and percentage overweight cutoffs to screen Japanese children and adolescents for obesity-related risk factors. J. Epidemiol. 2010, 20, 46–53. [Google Scholar] [CrossRef] [PubMed]
- The Image of the Transformation of Learning Brought by “1 Device for 1 Student with a High-Speed Network”. Available online: https://www.mext.go.jp/en/content/20200716-mxt_kokusai-000005414_04.pdf (accessed on 13 December 2021).
- Education in Japan beyond the Crisis of COVID-19–Leave No One Behind. Available online: https://www.mext.go.jp/en/content/20200904_mxt_kouhou01-000008961_1.pdf (accessed on 13 December 2021).
- Scherr, C.; Magalhães, C.K.; Malheiros, W. Lipid profile analysis in school children. Arq. Bras. Cardiol. 2007, 89, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Raitakari, O.T.; Juonala, M.; Kähönen, M.; Taittonen, L.; Laitinen, T.; Mäki-Torkko, N.; Järvisalo, M.J.; Uhari, M.; Jokinen, E.; Rönnemaa, T.; et al. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: The Cardiovascular Risk in Young Finns Study. JAMA 2003, 290, 2277–2283. [Google Scholar] [CrossRef] [PubMed]
- Benuck, I. Point: The rationale for universal lipid screening and treatment in children. J. Clin. Lipidol. 2015, 9, S93–S100. [Google Scholar] [CrossRef] [PubMed]
- Marks, D.; Thorogood, M.; Neil, H.A.; Wonderling, D.; Humphries, S.E. Comparing costs and benefits over a 10 year period of strategies for familial hypercholesterolaemia screening. J. Public Health Med. 2003, 25, 47–52. [Google Scholar] [CrossRef][Green Version]
- Familial Hypercholesterolemia (FH)–American Heart Association. Available online: https://www.heart.org/en/health-topics/cholesterol/causes-of-high-cholesterol/familial-hypercholesterolemia-fh (accessed on 3 February 2022).
- Okada, T.; Murata, M.; Yamauchi, K.; Harada, K. New criteria of normal serum lipid levels in Japanese children: The nationwide study. Pediatrics Int. 2002, 44, 596–601. [Google Scholar] [CrossRef]
- Uçar, B.; Kiliç, Z.; Dinleyici, E.C.; Colak, O.; Güneş, E. Serum lipid profiles including non-high density lipoprotein cholesterol levels in Turkish school-children. Anadolu Kardiyol. Derg. 2007, 7, 415–420. [Google Scholar]
- Gannagé-Yared, M.H.; Farah, V.; Chahine, E.; Balech, N.; Ibrahim, T.; Asmar, N.; Barakett-Hamadé, V.; Jambart, S. Distribution and correlates of non-high-density lipoprotein cholesterol and triglycerides in Lebanese school children. J. Clin. Lipidol. 2016, 10, 378–385. [Google Scholar] [CrossRef]
- Wilson, D.P.; Davis, S.; Matches, S.; Shah, D.; Leung-Pineda, V.; Mou, M.; Hamilton, L.; McNeal, C.J.; Bowman, W.P. Universal cholesterol screening of children in community-based ambulatory pediatric clinics. J. Clin. Lipidol. 2015, 9, S88–S92. [Google Scholar] [CrossRef]
- Couch, S.C.; Cross, A.T.; Kida, K.; Ros, E.; Plaza, I.; Shea, S.; Deckelbaum, R. Rapid westernization of children’s blood cholesterol in 3 countries: Evidence for nutrient-gene interactions? Am. J. Clin. Nutr. 2000, 72, 1266S–1274S. [Google Scholar] [CrossRef]
- Lampropoulou, M.; Chaini, M.; Rigopoulos, N.; Evangeliou, A.; Papadopoulou-Legbelou, K.; Koutelidakis, A.E. Association between serum lipid levels in Greek children with dyslipidemia and Mediterranean diet adherence, dietary habits, lifestyle and family focioeconomic factors. Nutrients 2020, 12, 1600. [Google Scholar] [CrossRef]
- Lauer, R.M.; Obarzanek, E.; Hunsberger, S.A.; Van Horn, L.; Hartmuller, V.W.; Barton, B.A.; Stevens, V.J.; Kwiterovich, P.O., Jr.; Franklin, F.A., Jr.; Kimm, S.Y.; et al. Efficacy and safety of lowering dietary intake of total fat, saturated fat, and cholesterol in children with elevated LDL cholesterol: The Dietary Intervention Study in Children. Am. J. Clin. Nutr. 2000, 72, 1332S–1342S. [Google Scholar] [CrossRef] [PubMed]
- Rauber, F.; Campagnolo, P.D.; Hoffman, D.J.; Vitolo, M.R. Consumption of ultra-processed food products and its effects on children’s lipid profiles: A longitudinal study. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Saadé, C.; Sleilaty, G.; Gannagé-Yared, M.H. Longitudinal changes of lipid profile in the Lebanese pediatric population. Lipids Health Dis. 2019, 18, 48. [Google Scholar] [CrossRef] [PubMed]
- Yamazaki, Y. Relation of adiposity rebound age to serum small dense low-density lipoprotein in young childhood. Dokkyo. J. Med. Sci. 2008, 35, 7–12. [Google Scholar]
- Zimmet, P.; Alberti, K.G.; Kaufman, F.; Tajima, N.; Silink, M.; Arslanian, S.; Wong, G.; Bennett, P.; Shaw, J.; Caprio, S.; et al. The metabolic syndrome in children and adolescents-an IDF consensus report. Pediatric Diabetes 2007, 8, 299–306. [Google Scholar] [CrossRef]
- Sparrenberger, K.; Sbaraini, M.; Cureau, F.V.; Teló, G.H.; Bahia, L.; Schaan, B.D. Higher adiponectin concentrations are associated with reduced metabolic syndrome risk independently of weight status in Brazilian adolescents. Diabetol. Metab. Syndr. 2019, 11, 40. [Google Scholar] [CrossRef]
- Tan, F.; Okamoto, M.; Suyama, A.; Miyamoto, T. Tracking of cardiovascular risk factors and a cohort study on hyperlipidemia in rural schoolchildren in Japan. J. Epidemiol. 2000, 10, 255–261. [Google Scholar] [CrossRef]
- Zachariah, J.P.; Shittu, T.; Wang, Y. Lipid temporal trends in normal-weight youth. Am. Heart J. 2021, 231, 68–72. [Google Scholar] [CrossRef]
- Fujita, Y.; Kouda, K.; Nakamura, H.; Nishio, N.; Takeuchi, H.; Iki, M. Height-specific serum cholesterol levels in pubertal children: Data from population-based Japanese school screening. J. Epidemiol. 2011, 21, 102–107. [Google Scholar] [CrossRef]
- The Japanese Society for Pediatric Endocrinology. Evaluation of the Physique of Japanese Children (Data of 2000) (In Japanese). Available online: http://jspe.umin.jp/medical/taikaku.html (accessed on 29 March 2022).
- Yin, Z.; Moore, J.B.; Johnson, M.H.; Vernon, M.M.; Gutin, B. The impact of a 3-year after-school obesity prevention program in elementary school children. Child. Obes. 2012, 8, 60–70. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, A.; Charlton, K.E.; Girdo, L.; Batterham, M. Using data from patient interactions in primary care for population level chronic disease surveillance: The Sentinel Practices Data Sourcing (SPDS) project. BMC Public Health. 2014, 14, 557. [Google Scholar] [CrossRef] [PubMed]
- Papoutsakis, C.; Yannakoulia, M.; Ntalla, I.; Dedoussis, G.V. Metabolic syndrome in a Mediterranean pediatric cohort: Prevalence using International Diabetes Federation-derived criteria and associations with adiponectin and leptin. Metabolism 2012, 61, 140–145. [Google Scholar] [CrossRef] [PubMed]
| Variables | n | % |
|---|---|---|
| Gender | ||
| Female | 321 | 49.4% |
| Male | 329 | 50.6% |
| Total | 650 | |
| Do you have a bowel movement every day? | ||
| May not have a bowel movement for 3 days or more | 41 | 6.3% |
| May not have a bowel movement for 1–2 days | 198 | 30.4% |
| I have a bowel movement every day but not at fixed times | 328 | 50.5% |
| I have a bowel movement every day at a fixed time | 74 | 11.4% |
| Unknown | 9 | 1.4% |
| Do you know your weight? | ||
| I do not know it | 240 | 36.9% |
| I know it | 397 | 61.1% |
| Unknown | 13 | 2.0% |
| Please tell me how you feel regarding your body shape | ||
| I want to be quite thin | 72 | 11.1% |
| I want to be a little thinner | 192 | 29.5% |
| It should be as it is | 324 | 49.9% |
| I want to gain a little weight | 47 | 7.2% |
| I want to gain a lot of weight | 6 | 0.9% |
| Unknown | 9 | 1.4% |
| Have you ever tried to deliberately lose weight? | ||
| I was told by a hospital or schoolteacher that I was overweight, and I was instructed to do it | 2 | 0.3% |
| I did it because I wanted to lose weight | 102 | 15.7% |
| I wanted to, but I have not done it yet | 98 | 15.1% |
| Never thought about it | 439 | 67.5% |
| Unknown | 9 | 1.4% |
| How much time do you spend each day playing video games, on TV, the internet, smartphones/phones, etc. after returning from school? | ||
| None | 49 | 7.5% |
| Less than 1 h | 182 | 28.0% |
| 1 h or more and less than 2 h | 164 | 25.2% |
| 2 h or more and less than 3 h | 115 | 17.7% |
| 3 h or more | 131 | 20.2% |
| Unknown | 9 | 1.4% |
| Do you think you are healthy? | ||
| No | 11 | 1.7% |
| Seldom | 72 | 11.1% |
| Sometimes | 337 | 51.9% |
| Yes | 220 | 33.8% |
| Unknown | 10 | 1.5% |
| Can you consciously improve your mood? | ||
| No | 62 | 9.5% |
| Seldom | 118 | 18.2% |
| Sometimes | 209 | 32.1% |
| Yes | 254 | 39.1% |
| Unknown | 7 | 1.1% |
| Do you know about lifestyle-related disease? | ||
| No | 400 | 61.6% |
| A little | 171 | 26.3% |
| I cannot explain them, but I think I know | 60 | 9.2% |
| I can explain them | 7 | 1.1% |
| Unknown | 12 | 1.8% |
| Variable | N | Mean | Standard Deviation |
|---|---|---|---|
| Height in the fourth grade of elementary school | 643 | 132.7 | 6.13 |
| Weight in the fourth grade of elementary school | 643 | 30.3 | 6.15 |
| BMI in the fourth grade of elementary school | 643 | 17.1 | 2.55 |
| BMI z-score in the fourth grade of elementary school | 643 | 3.15 | 3.32 |
| Height z-score in the fourth grade of elementary school | 643 | 0.03 | 1.00 |
| Height in the first year of junior high school | 572 | 152.2 | 8.35 |
| Weight in the first year of junior high school | 572 | 44.6 | 9.33 |
| BMI in the first year of junior high school | 572 | 19.4 | 6.88 |
| BMI z-score in the first year of junior high school | 572 | 0.88 | 3.49 |
| Height z-score in the first year of junior high school | 572 | 0.29 | 1.23 |
| Variable | N | Mean | Standard Deviation |
|---|---|---|---|
| Total cholesterol (mg/dL) in the fourth grade of elementary school | 444 | 174 | 24.8 |
| Total cholesterol (mg/dL) in the first year of junior high school | 444 | 166 | 24.7 |
| Average total cholesterol change (mg/dL) | 444 | −8.1 | 20.7 |
| Variable | Fourth Grade of Elementary School | First Grade of Junior High School | p-Value |
|---|---|---|---|
| Total | 142.8 | 127.7 | <0.0001 |
| Gender | |||
| Female | 148.3 | 139.0 | 0.0299 |
| Male | 137.6 | 116.6 | <0.0001 |
| Do you have a bowel movement every day? | |||
| May not have a bowel movement for 3 days or more | 147.7 | 127.3 | 0.0654 |
| May not have a bowel movement for 1–2 days | 141.5 | 132.1 | 0.0804 |
| I have a bowel movement every day but not at fixed times | 142.8 | 127.1 | 0.0011 |
| I have a bowel movement every day at a fixed time | 149.8 | 121.0 | 0.0018 |
| Do you know your weight? | |||
| I do not know it | 137.0 | 124.5 | 0.0193 |
| I know it | 146.5 | 129.2 | 0.0001 |
| Please tell me how you feel regarding your body shape | |||
| I want to be quite thin | 155.2 | 135.1 | 0.0235 |
| I want to be a little thinner | 143.9 | 125.3 | 0.0030 |
| It should be as it is | 142.1 | 128.3 | 0.0034 |
| I want to gain a little weight | 139.0 | 122.2 | 0.1082 |
| I want to gain a lot of weight | 108.3 | 131.3 | 0.6488 |
| Have you ever tried to deliberately lose weight? | |||
| I was told by a hospital or schoolteacher that I was overweight, and I was instructed to do it | 140.5 | 143.5 | 0.5307 |
| I did it because I wanted to lose weight | 146.4 | 128.2 | 0.0148 |
| I wanted to, but I have not done it yet | 143.3 | 131.7 | 0.1284 |
| Never thought about it | 142.9 | 126.7 | 0.0001 |
| How much time do you spend a day on video games, TV, the internet, smartphones/phones, etc., after returning from school? | |||
| None | 144.0 | 132.2 | 0.1638 |
| Less than 1 h | 151.2 | 134.8 | 0.0028 |
| 1 h or more and less than 2 h | 146.1 | 129.6 | 0.0087 |
| 2 h or more and less than 3 h | 139.5 | 121.4 | 0.0278 |
| 3 h or more | 146.6 | 133.2 | 0.0725 |
| Do you think you are healthy? | |||
| No | 136.6 | 138.4 | 0.5177 |
| Seldom | 138.6 | 132.1 | 0.2501 |
| Sometimes | 142.9 | 128.1 | 0.0021 |
| Yes | 146.0 | 124.8 | 0.0002 |
| Can you consciously improve your mood? | |||
| No | 126.4 | 122.6 | 0.3830 |
| Seldom | 144.5 | 132.6 | 0.0725 |
| Sometimes | 145.3 | 127.0 | 0.0020 |
| Yes | 145.9 | 127.6 | 0.0006 |
| Do you know about lifestyle habits? | |||
| No | 141.9 | 127.5 | 0.0011 |
| A little | 144.8 | 131.2 | 0.0266 |
| I cannot explain them, but I think I know | 152.1 | 118.8 | 0.0012 |
| I can explain them | 123.6 | 110.9 | 0.3759 |
| TC Timepoint 1 | TC Timepoint 2 | Change in TC | ||||
|---|---|---|---|---|---|---|
| r | p-Value | r | p-Value | r | p-Value | |
| Height | −0.0599 | 0.2074 | −0.0991 | 0.0369 | −0.0467 | 0.3265 |
| Weight | 0.0477 | 0.3163 | −0.0974 | 0.0402 | −0.1733 | 0.0002 |
| BMI | −0.0364 | 0.4447 | −0.0638 | 0.1796 | −0.0327 | 0.4914 |
| TC Timepoint 1 | 1 | 0.6496 | <0.0001 | −0.4192 | <0.0001 | |
| TC Timepoint 2 | 0.6496 | <0.0001 | 1 | 0.4179 | <0.0001 | |
| Change in TC | −0.4192 | <0.0001 | 0.4179 | <0.0001 | 1 | |
| Variable | Coefficient | p-Value | Low CI | High CI |
|---|---|---|---|---|
| Height | 0.42 | 0.041 | 0.02 | 0.83 |
| Weight | −0.92 | <0.001 | −1.34 | −0.50 |
| BMI | −0.03 | 0.263 | −0.08 | 0.02 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kawasaki, H.; Yamasaki, S.; Shintaku, H.; Fukita, S. Identification of Factors Influencing Cholesterol Changes in Elementary-School Children: A Longitudinal Study. Children 2022, 9, 518. https://doi.org/10.3390/children9040518
Kawasaki H, Yamasaki S, Shintaku H, Fukita S. Identification of Factors Influencing Cholesterol Changes in Elementary-School Children: A Longitudinal Study. Children. 2022; 9(4):518. https://doi.org/10.3390/children9040518
Chicago/Turabian StyleKawasaki, Hiromi, Satoko Yamasaki, Hazuki Shintaku, and Susumu Fukita. 2022. "Identification of Factors Influencing Cholesterol Changes in Elementary-School Children: A Longitudinal Study" Children 9, no. 4: 518. https://doi.org/10.3390/children9040518
APA StyleKawasaki, H., Yamasaki, S., Shintaku, H., & Fukita, S. (2022). Identification of Factors Influencing Cholesterol Changes in Elementary-School Children: A Longitudinal Study. Children, 9(4), 518. https://doi.org/10.3390/children9040518






