Age and Gender Are Associated with the Component of Psychosocial Impact of Dental Aesthetics Questionnaire in Young People: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Sample
2.3. Measures
2.4. Statistical Procedures
3. Results
3.1. Demographics and Preliminary Analyses
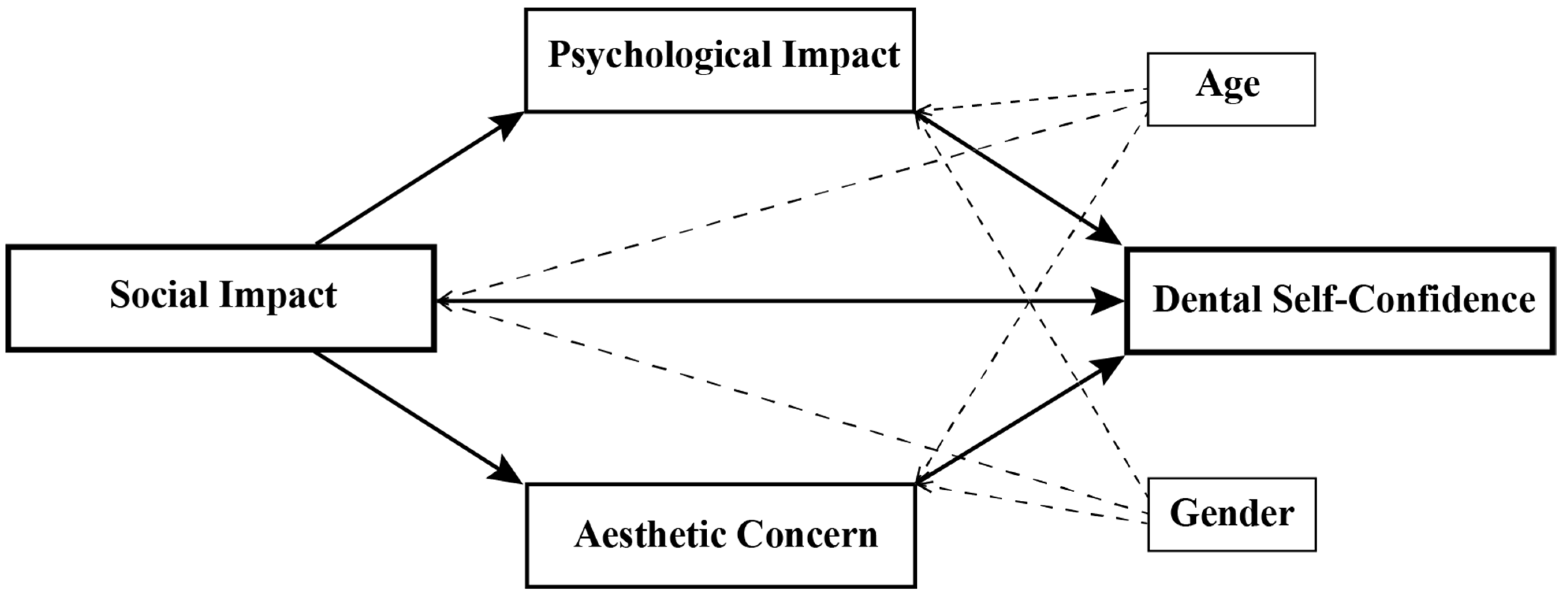
3.2. Mediation Analysis
3.3. Moderated Mediation Analysis
4. Discussion
4.1. Direct Influence of Social Impact on Dental Self-Confidence in Boys and Young Adolescents
4.2. Indirect Influence of Social Impact on Dental Self-Confidence via Psychological Impact in Older Participants and Girls
4.3. Indirect Influence of Social Impact on Dental Self-Confidence via Aesthetic Concern
4.4. Study Limitations
4.5. Recommendations from the Study Outcome
5. Conclusions
- SI was directly and indirectly associated with DSC. PI and AC were directly associated with DSC.
- Age and gender acted as moderators to modify the strength of the association. In girls and in older adolescents as well as young adults, the effect of SI was more deeply rooted, occurring through the PI, which, in turn, influenced DSC.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Klages, U.; Bruckner, A.; Zentner, A. Dental Aesthetics, Self-Awareness, and Oral Health-Related Quality of Life in Young Adults. Eur. J. Orthod. 2004, 26, 507–514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henson, S.T.; Lindauer, S.J.; Gardner, W.G.; Shroff, B.; Tufekci, E.; Best, A.M. Influence of Dental Esthetics on Social Perceptions of Adolescents Judged by Peers. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Tristão, S.K.P.C.; Magno, M.B.; Pintor, A.V.B.; Christovam, I.F.O.; Ferreira, D.M.T.P.; Maia, L.C.; de Souza, I.P.R. Is There a Relationship between Malocclusion and Bullying? A Systematic Review. Prog. Orthod. 2020, 21, 26. [Google Scholar] [CrossRef] [PubMed]
- Klages, U.; Zentner, A. Dentofacial Aesthetics and Quality of Life. Semin. Orthod. 2007, 13, 104–115. [Google Scholar] [CrossRef]
- Pearsall, J.; Hanks, P. Oxford Dictionary of English, 2nd ed.; Oxford University Press: Oxford, UK, 2003; p. 1671. [Google Scholar]
- Afroz, S.; Rathi, S.; Rajput, G.; Rahman, S.A. Dental Esthetics and Its Impact on Psycho-Social Well-Being and Dental Self Confidence: A Campus Based Survey of North Indian University Students. J. Indian Prosthodont Soc. 2013, 13, 455–460. [Google Scholar] [CrossRef]
- Kraft, T.L.; Pressman, S.D. Grin and Bear It: The Influence of Manipulated Facial Expression on the Stress Response. Psychol. Sci. 2012, 23, 1372–1378. [Google Scholar] [CrossRef]
- Janson, G.; Branco, N.C.; Morais, J.F.; Freitas, M.R. Smile Attractiveness in Patients with Class II Division 1 Subdivision Malocclusions Treated with Different Tooth Extraction Protocols. Eur. J. Orthod. 2014, 36, 1–8. [Google Scholar] [CrossRef]
- Lopez, Y.; Rouzic, J.; Bertaud, V.; Pérard, M.; Clerc, J.; Vulcain, J. Influence of Teeth on the Smile and Physical Attractiveness. A New Internet Based Assessing Method. Open J. Stomatol. 2013, 3, 52–57. [Google Scholar] [CrossRef] [Green Version]
- Marmolejo-Ramos, F.; Murata, A.; Sasaki, K.; Yamada, Y.; Ikeda, A.; Hinojosa, J.A.; Watanabe, K.; Parzuchowski, M.; Tirado, C.; Ospina, R. Your Face and Moves Seem Happier When I Smile. Exp. Psychol. 2020, 67, 14–22. [Google Scholar] [CrossRef]
- Lewis, M.B. The Interactions between Botulinum-Toxin-Based Facial Treatments and Embodied Emotions. Sci. Rep. 2018, 8, 14720. [Google Scholar] [CrossRef]
- Miguel, J.A.; Sales, H.X.; Quintao, C.C.; Oliveira, B.H.; Feu, D. Factors Associated with Orthodontic Treatment Seeking by 12–15-Year-Old Children at a State University-Funded Clinic. J. Orthod. 2010, 37, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Feldens, C.A.; Nakamura, E.K.; Tessarollo, F.R.; Closs, L.Q. Desire for Orthodontic Treatment and Associated Factors among Adolescents in Southern Brazil. Angle Orthod. 2015, 85, 224–232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marques, L.S.; Pordeus, I.A.; Ramos-Jorge, M.L.; Filogonio, C.A.; Filogonio, C.B.; Pereira, L.J.; Paiva, S.M. Factors Associated with the Desire for Orthodontic Treatment among Brazilian Adolescents and Their Parents. BMC Oral Health 2009, 9, 34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pabari, S.; Moles, D.R.; Cunningham, S.J. Assessment of Motivation and Psychological Characteristics of Adult Orthodontic Patients. Am. J. Orthod. Dentofac. Orthop. 2011, 140, e263–e272. [Google Scholar] [CrossRef]
- Bradley, E.; Shelton, A.; Hodge, T.; Morris, D.; Bekker, H.; Fletcher, S.; Barber, S. Patient-Reported Experience and Outcomes from Orthodontic Treatment. J. Orthod. 2020, 47, 107–115. [Google Scholar] [CrossRef]
- Samorodnitzky-Naveh, G.R.; Geiger, S.B.; Levin, L. Patients’ Satisfaction with Dental Esthetics. J. Am. Dent. Assoc. 2007, 138, 805–808. [Google Scholar] [CrossRef]
- Muniz, F.; Cavalcante, D.J.; Moreira, M.M.S.M.; Rodrigues, L.K.A.; de Oliveira Fernandes, C.A.; de Almeida, P.C.; de Sousa Carvalho, R. Association between Confidence in Smiling and Esthetic Characteristics. J. Esthet. Restor. Dent. 2017, 29, e56–e66. [Google Scholar] [CrossRef]
- Klages, U.; Erbe, C.; Sandru, S.D.; Brullman, D.; Wehrbein, H. Psychosocial Impact of Dental Aesthetics in Adolescence: Validity and Reliability of a Questionnaire across Age-Groups. Qual. Life Res. 2015, 24, 379–390. [Google Scholar] [CrossRef]
- Masood, M.; Masood, Y.; Newton, T.; Lahti, S. Development of a Conceptual Model of Oral Health for Malocclusion Patients. Angle Orthod. 2015, 85, 1057–1063. [Google Scholar] [CrossRef] [Green Version]
- Bandura, A. Social Cognitive Theory of Mass Communication. Media Psychol. 2001, 3, 265–299. [Google Scholar] [CrossRef]
- Bittencourt, J.M.; Martins, L.P.; Bendo, C.B.; Vale, M.P.; Paiva, S.M. Negative Effect of Malocclusion on the Emotional and Social Well-Being of Brazilian Adolescents: A Population-Based Study. Eur. J. Orthod. 2017, 39, 628–633. [Google Scholar] [CrossRef] [PubMed]
- Dann, C., IV; Phillips, C.; Broder, H.L.; Tulloch, J.F. Self-Concept, Class II Malocclusion, and Early Treatment. Angle Orthod. 1995, 65, 411–416. [Google Scholar]
- Spalj, S.; Novsak, A.; Bilobrk, P.; Katic, V.; Zrinski, M.T.; Pavlic, A. Mediation and Moderation Effect of the Big Five Personality Traits on the Relationship between Self-Perceived Malocclusion and Psychosocial Impact of Dental Esthetics. Angle Orthod. 2016, 86, 413–420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wan Hassan, W.N.; Yusof, Z.Y.M.; Yuen, S.W.; Mohd Tajudin, Z.; Lokman, N.; Makhbul, M.Z.M. Prevalence, Extent and Severity of the Psychosocial Impact of Dental Aesthetics among Malaysian Adolescents. Sains. Malays. 2019, 48, 1729–1736. [Google Scholar] [CrossRef]
- Tajudin, Z.M.; Wan Hassan, W.N.; Yusof, Z.Y.M.; Makhbul, M.Z.M. Impacts of Self Perceived Malocclusion on the Oral Health Related Quality of Life of Young Adults. Healthcare 2021, 9, 248. [Google Scholar] [CrossRef]
- Walker-Harding, L.R.; Christie, D.; Joffe, A.; Lau, J.S.; Neinstein, L. Young Adult Health and Well-Being: A Position Statement of the Society for Adolescent Health and Medicine. J. Adolesc. Health 2017, 60, 758–759. [Google Scholar] [CrossRef] [Green Version]
- Wan Hassan, W.N.; Yusof, Z.Y.M.; Makhbul, M.Z.M.; Shahidan, S.S.; Mohd Ali, S.F.; Burhanudin, R.; Gere, M.J. Validation and Reliability of the Malaysian English Version of the Psychosocial Impact of Dental Aesthetics Questionnaire for Adolescents. Health Qual. Life Outcomes 2017, 15, 54. [Google Scholar] [CrossRef] [Green Version]
- Wan Hassan, W.N.; Yusof, Z.Y.M.; Shahidan, S.S.; Mohd Ali, S.F.; Makhbul, M.Z.M. Validation and Reliability of the Translated Malay Version of the Psychosocial Impact of Dental Aesthetics Questionnaire for Adolescents. Health Qual. Life Outcomes 2017, 15, 23. [Google Scholar] [CrossRef] [Green Version]
- Grzywacz, I. The Value of the Aesthetic Component of the Index of Orthodontic Treatment Need in the Assessment of Subjective Orthodontic Treatment Need. Eur. J. Orthod. 2003, 25, 57–63. [Google Scholar] [CrossRef]
- Schober, P.; Boer, C.; Schwarte, L.A. Correlation Coefficients: Appropriate Use and Interpretation. Anesth. Analg. 2018, 126, 1763–1768. [Google Scholar] [CrossRef]
- The Process Macro for Spss, Sas and R Version v4.0. Available online: http://www.processmacro.org/download.html (accessed on 20 December 2021).
- Alabdulrazaq, R.S.; Al-Haj Ali, S.N. Parental Reported Bullying among Saudi Schoolchildren: Its Forms, Effect on Academic Abilities, and Associated Sociodemographic, Physical, and Dentofacial Features. Int. J. Pediatr. 2020, 2020, 8899320. [Google Scholar] [CrossRef]
- Hajnal, A.; Vonk, J.; Hill, V.Z. Peer Influence on Conformity and Confidence in a Perceptual Judgment Task. Psihologija 2020, 53, 101–113. [Google Scholar] [CrossRef] [Green Version]
- Ahlin, E.M.; Lobo Antunes, M.J. Locus of Control Orientation: Parents, Peers, and Place. J. Youth Adolesc. 2015, 44, 1803–1818. [Google Scholar] [CrossRef]
- Vollmer, A.L.; Read, R.; Trippas, D.; Belpaeme, T. Children Conform, Adults Resist: A Robot Group Induced Peer Pressure on Normative Social Conformity. Sci. Robot 2018, 3, eaat7111. [Google Scholar] [CrossRef] [Green Version]
- Kawachi, I.; Berkman, L.F. Social Ties and Mental Health. J. Urban Health 2001, 78, 458–467. [Google Scholar] [CrossRef] [Green Version]
- Taylor, S.E.; Repetti, R.L.; Seeman, T. Health Psychology: What Is an Unhealthy Environment and How Does It Get under the Skin? Annu. Rev. Psychol. 1997, 48, 411–447. [Google Scholar] [CrossRef] [Green Version]
- Taghavi Bayat, J.; Hallberg, U.; Lindblad, F.; Huggare, J.; Mohlin, B. Daily Life Impact of Malocclusion in Swedish Adolescents: A Grounded Theory Study. Acta Odontol. Scand. 2013, 71, 792–798. [Google Scholar] [CrossRef] [PubMed]
- Paula, D.F., Jr.; Silva, É.T.; Campos, A.C.; Nuñez, M.O.; Leles, C.R. Effect of Anterior Teeth Display During Smiling on the Self-Perceived Impacts of Malocclusion in Adolescents. Angle Orthod. 2011, 81, 540–545. [Google Scholar] [PubMed]
- de Paula Junior, D.F.; Santos, N.C.; da Silva, E.T.; Nunes, M.F.; Leles, C.R. Psychosocial Impact of Dental Esthetics on Quality of Life in Adolescents. Angle Orthod. 2009, 79, 1188–1193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gleason, J.H.; Alexander, A.M.; Somers, C.L. Later Adolescents’ Reactions to Three Types of Childhood Teasing: Relations with Self-Esteem and Body Image. Soc. Behav. Pers. 2000, 28, 471–480. [Google Scholar] [CrossRef]
- Sides-Moore, L.; Tochkov, K. The Thinner the Better? Competitiveness, Depression and Body Image among College Student Women. Coll. Stud. J. 2011, 45, 439–449. [Google Scholar]
- Pickhardt, C.E. Adolescence and the Desire for Physical Beauty. Psychol. Today 2019. Available online: https://www.psychologytoday.com/us/blog/surviving-your-childs-adolescence/201902/adolescence-and-the-desire-physical-beauty (accessed on 29 January 2022).
- Bradbury, E. Self-Consciousness: What Is It and How Does It Relate to Cosmetic Procedures? J. Aesthet. Nurs. 2012, 1, 260–261. [Google Scholar] [CrossRef]
- Ruiz, C.; Conde, E.; Torres, E. Importance of Facial Physical Attractiveness of Audiovisual Models in Descriptions and Preferences of Children and Adolescents. Percept. Mot. Skills 2005, 101, 229–243. [Google Scholar] [CrossRef] [PubMed]
- Montero, J.; Gomez Polo, C.; Rosel, E.; Barrios, R.; Albaladejo, A.; Lopez-Valverde, A. The Role of Personality Traits in Self-Rated Oral Health and Preferences for Different Types of Flawed Smiles. J. Oral Rehabil. 2016, 43, 39–50. [Google Scholar] [CrossRef] [PubMed]
- Hoad-Reddick, G. How Relevant Is Counselling in Relation to Dentistry? Br. Dent. J. 2004, 197, 9–14. [Google Scholar]
- Widström, E.; Eaton, K.A. Oral Healthcare Systems in the Extended European Union. Oral Health Prev. Dent. 2004, 2, 155–194. [Google Scholar]
- Wan Hassan, W.N.; Makhbul, M.Z.M.; Yusof, Z.Y.M. Use of the Sociodental Approach in Estimating Orthodontic Treatment Needs in Adolescent Patients. J. Orofac. Orthop. 2021. [Google Scholar] [CrossRef]



| Variable | Groups | N (%) | DSC Score | Statistics | p | ||
|---|---|---|---|---|---|---|---|
| Mean | SD | t | F | ||||
| Gender | 3.289 | 0.001 * | |||||
| Boys | 644 (45.2) | 13.3 | 5.2 | ||||
| Girls | 781 (54.8) | 12.3 | 5.4 | ||||
| Ethnicity | 7.088 | <0.001 * | |||||
| Malay | 978 (68.6) | 13.0 | 5.0 | ||||
| Chinese | 240 (16.8) | 11.5 | 6.0 | ||||
| Indian | 99 (6.9) | 14.1 | 5.9 | ||||
| Other | 108 (7.6) | 12.4 | 5.5 | ||||
| Age | 16.0 | 2.8 | 2.133 | 0.094 | |||
| 14 and below | 571 (40.1) | 12.4 | 5.2 | ||||
| 15 to 19 | 708 (49.7) | 13.1 | 5.3 | ||||
| 20 to 24 | 142 (10.0) | 12.7 | 5.7 | ||||
| 25 to 30 | 4 (0.3) | 12.5 | 5.4 | ||||
| Self-perceived malocclusion | 86.987 | <0.001 * | |||||
| None | 787 (55.2) | 14.5 | 5.1 | ||||
| Mild | 520 (36.5) | 11.2 | 4.7 | ||||
| Moderate | 78 (5.5) | 7.9 | 4.4 | ||||
| Severe | 40 (2.8) | 8.2 | 4.5 | ||||
| Variables | DSC | SI | PI | AC | Mean | S.D. | Min | Max |
|---|---|---|---|---|---|---|---|---|
| DSC: dental self-confidence | 1 | −0.487 *** | −0.527 *** | −0.582 *** | 12.8 | 5.3 | 0 | 24 |
| SI: social impact | 1 | 0.791 *** | 0.676 *** | 9.8 | 6.8 | 0 | 32 | |
| PI: psychological impact | 1 | 0.699 *** | 10.3 | 5.4 | 0 | 24 | ||
| AC: aesthetic concern | 1 | 2.6 | 1.9 | 0 | 8 | |||
| Age | 0.043 | 0.080 ** | 0.057 * | 0.089 ** | 16.0 | 2.8 | 12 | 30 |
| Gender ø | −0.087 ** | 0.071 ** | 0.109 *** | 0.102 *** |
| Direct Effects | |||||||
|---|---|---|---|---|---|---|---|
| Variables | B | SE | t | p | LLCI | ULCI | |
| SI → PI | 0.60 | 0.01 | 45.01 | <0.001 | 0.57 | 0.62 | * |
| SI → AC | 0.19 | 0.01 | 33.70 | <0.001 | 0.17 | 0.20 | * |
| SI → DSC | −0.04 | 0.03 | −1.37 | 0.171 | −0.09 | 0.02 | |
| PI → DSC | −0.20 | 0.04 | −5.45 | <0.001 | −0.27 | −0.13 | * |
| AC → DSC | −1.05 | 0.09 | −12.06 | <0.001 | −1.23 | −0.88 | * |
| R2 (PI): 0.656 (p < 0.001); R2 (AC): 0.513 (p < 0.001); R2 (DSC): 0.430 (p < 0.001) | |||||||
| Indirect Effects (SI → mediator → DSC) | |||||||
| Variables | Effect | BootSE | BootLLCI | BootULCI | |||
| PI | −0.12 | 0.02 | −0.16 | −0.07 | * | ||
| AC | −0.19 | 0.02 | −0.23 | −0.16 | * | ||
| Total | −0.31 | 0.03 | −0.36 | −0.26 | * | ||
| Direct Effects | |||||||
|---|---|---|---|---|---|---|---|
| Variables | B | SE | t | p | LLCI | ULCI | |
| SI → PI | 0.59 | 0.01 | 45.09 | <0.001 | 0.57 | 0.62 | * |
| SI → AC | 0.19 | 0.01 | 33.87 | <0.001 | 0.17 | 0.20 | * |
| SI → DSC | −0.03 | 0.03 | −0.96 | 0.339 | −0.08 | 0.03 | |
| PI → DSC | −0.21 | 0.04 | −5.88 | <0.001 | −0.28 | −0.14 | * |
| AC → DSC | −1.05 | 0.09 | −12.02 | <0.001 | −1.22 | −0.88 | * |
| SI*Age → DSC | 0.02 | 0.01 | 2.47 | 0.014 | 0.01 | 0.05 | * |
| PI*Age → DSC | −0.05 | 0.01 | −0.396 | <0.001 | −0.08 | −0.03 | * |
| AC*Age → DSC | −0.03 | 0.03 | −1.02 | 0.307 | −0.09 | 0.03 | |
| R2 (PI): 0.656 (p < 0.001); R2 (AC): 0.512 (p < 0.001); R2 (DSC): 0.442 (p < 0.001) | |||||||
| Conditional Direct Effects at Specific Levels of Age as Moderator | |||||||
| SI → DSC | B | SE | t | p | LLCI | ULCI | |
| 1 SD below mean | −0.10 | 0.04 | −2.55 | 0.011 | −0.17 | −0.02 | * |
| Mean | −0.03 | 0.03 | −0.96 | 0.339 | −0.08 | 0.03 | |
| 1 SD above mean | 0.04 | 0.04 | 1.07 | 0.284 | −0.04 | 0.13 | |
| Conditional Indirect Effects at Specific Levels of Age as Moderator | |||||||
| SI → PI → DSC | Effect | BootSE | BootLLCI | BootULCI | |||
| 1 SD below mean | −0.04 | 0.03 | −0.10 | 0.02 | |||
| Mean | −0.13 | 0.02 | −0.17 | −0.08 | * | ||
| 1 SD above mean | −0.21 | 0.03 | −0.28 | −0.15 | * | ||
| Direct Effects | |||||||
|---|---|---|---|---|---|---|---|
| Variables | B | SE | t | p | LLCI | ULCI | |
| SI → PI | 0.60 | 0.01 | 45.23 | < 0.001 | 0.57 | 0.63 | * |
| SI → AC | 0.19 | 0.01 | 33.94 | < 0.001 | 0.18 | 0.20 | * |
| SI → DSC | −0.34 | 0.09 | −3.63 | < 0.001 | −0.52 | −0.16 | * |
| PI → DSC | 0.12 | 0.12 | 0.99 | 0.321 | −0.12 | 0.35 | |
| AC → DSC | 0.95 | 0.28 | −3.35 | 0.001 | −1.50 | −0.39 | * |
| SI * Gender → DSC | 0.19 | 0.07 | 3.39 | 0.001 | 0.08 | 0.30 | * |
| PI * Gender → DSC | −0.20 | 0.07 | −2.76 | 0.006 | −0.34 | −0.06 | * |
| AC * Gender → DSC | −0.07 | 0.17 | −0.39 | 0.693 | −0.41 | 0.27 | |
| R2 (PI): 0.652 (p < 0.001); R2 (AC): 0.510 (p < 0.001); R2 (DSC): 0.435 (p < 0.001) | |||||||
| Conditional Direct Effects at Specific Levels of Gender as Moderator | |||||||
| SI → DSC | B | SE | t | p | LLCI | ULCI | |
| Male | −0.15 | 0.04 | −3.48 | 0.001 | −0.24 | −0.07 | * |
| Female | 0.04 | 0.04 | 1.10 | 0.272 | −0.03 | 0.11 | |
| Conditional Indirect Effects at Specific Levels of Gender as Moderator | |||||||
| SI → PI → DSC | Effect | BootSE | BootLLCI | BootULCI | |||
| Male | −0.05 | 0.04 | −0.12 | 0.02 | |||
| Female | −0.17 | 0.03 | −0.28 | −0.11 | * | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wan Hassan, W.N.; Makhbul, M.Z.M.; Othman, S.A. Age and Gender Are Associated with the Component of Psychosocial Impact of Dental Aesthetics Questionnaire in Young People: A Cross-Sectional Study. Children 2022, 9, 496. https://doi.org/10.3390/children9040496
Wan Hassan WN, Makhbul MZM, Othman SA. Age and Gender Are Associated with the Component of Psychosocial Impact of Dental Aesthetics Questionnaire in Young People: A Cross-Sectional Study. Children. 2022; 9(4):496. https://doi.org/10.3390/children9040496
Chicago/Turabian StyleWan Hassan, Wan Nurazreena, Mohd Zambri Mohamed Makhbul, and Siti Adibah Othman. 2022. "Age and Gender Are Associated with the Component of Psychosocial Impact of Dental Aesthetics Questionnaire in Young People: A Cross-Sectional Study" Children 9, no. 4: 496. https://doi.org/10.3390/children9040496
APA StyleWan Hassan, W. N., Makhbul, M. Z. M., & Othman, S. A. (2022). Age and Gender Are Associated with the Component of Psychosocial Impact of Dental Aesthetics Questionnaire in Young People: A Cross-Sectional Study. Children, 9(4), 496. https://doi.org/10.3390/children9040496







