In-Brace versus Out-of-Brace Protocol for Radiographic Follow-Up of Patients with Idiopathic Scoliosis: A Retrospective Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Patients
2.3. Method of Measurements
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
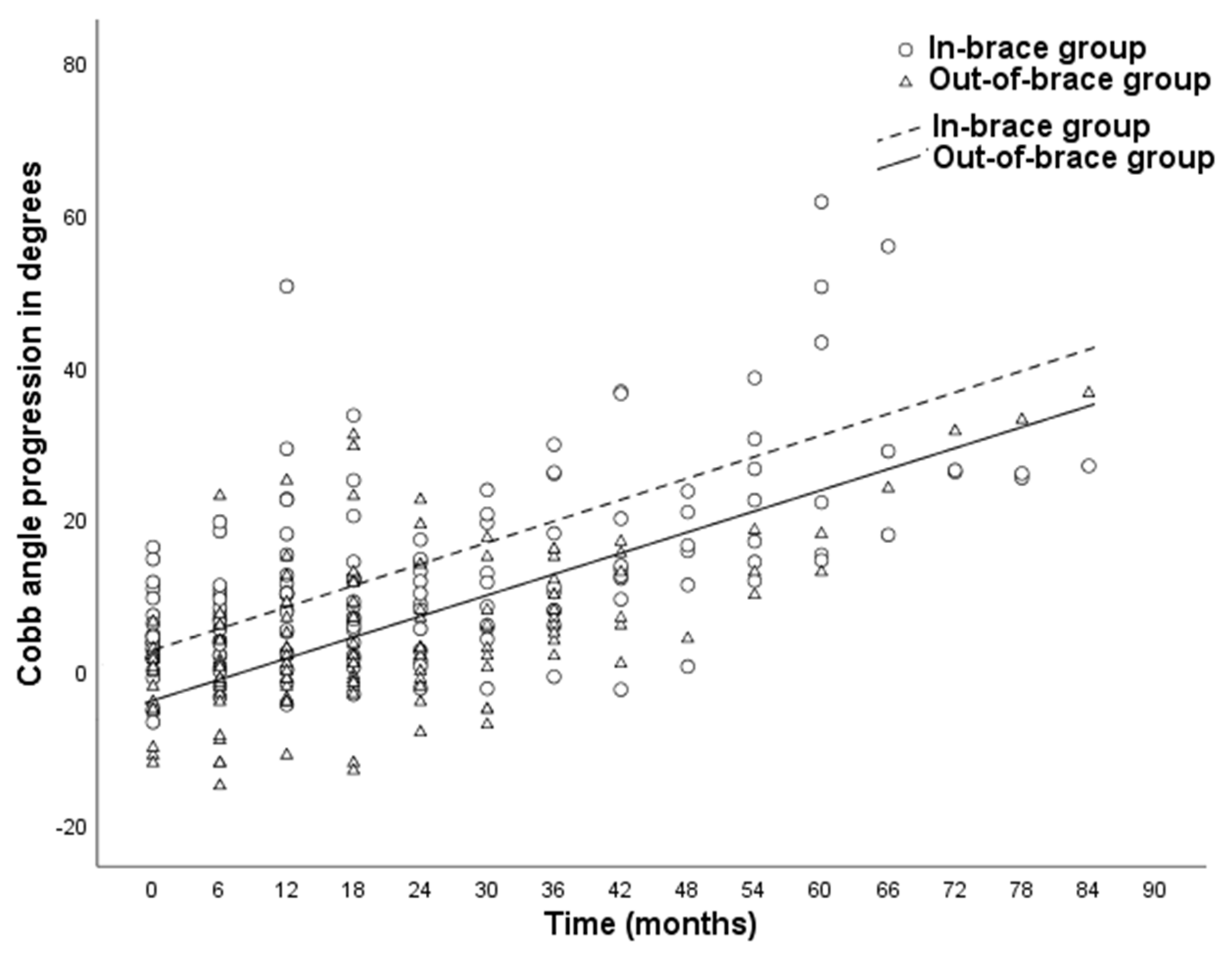
3.2. Curve Progression of Scoliosis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Di Maria, F.; Vescio, A.; Caldaci, A.; Vancheri, A.; Di Maria, C.; Sapienza, M.; Testa, G.; Pavone, V. Immediate Effects of Sforzesco((R)) Bracing on Respiratory Function in Adolescents with Idiopathic Scoliosis. Healthcare 2021, 9, 1372. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, S.L.; Dolan, L.; Wright, J.G.; Dobbs, M.B. Effects of bracing in adolescents with idiopathic scoliosis. N. Engl. J. Med. 2013, 369, 1512–1521. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Negrini, S.; Donzelli, S.; Aulisa, A.G.; Czaprowski, D.; Schreiber, S.; De Mauroy, J.C.; Diers, H.; Grivas, T.B.; Knott, P.; Kotwicki, T.; et al. 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 2018, 13, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Busscher, I.; Wapstra, F.H.; Veldhuizen, A.G. Predicting growth and curve progression in the individual patient with adolescent idiopathic scoliosis: Design of a prospective longitudinal cohort study. BMC Musculoskelet Disord. 2010, 11, 93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maruyama, T.; Takeshita, K. Surgical treatment of scoliosis: A review of techniques currently applied. Scoliosis 2008, 3, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Floman, Y.; Burnei, G.; Gavriliu, S.; Anekstein, Y.; Straticiuc, S.; Tunyogi-Csapó, M.; Mirovsky, Y.; Zarzycki, D.; Potaczek, T.; Arnin, U. Surgical management of moderate adolescent idiopathic scoliosis with ApiFix(R): A short peri- apical fixation followed by post-operative curve reduction with exercises. Scoliosis 2015, 10, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weinstein, S.L.; Dolan, L.; Cheng, J.; Danielsson, A.; Morcuende, A.J. Adolescent idiopathic scoliosis. Lancet 2008, 371, 1527–1537. [Google Scholar] [CrossRef] [Green Version]
- Katz, D.E.; Herring, J.A.; Browne, R.H.; Kelly, D.M.; Birch, J.G. Brace wear control of curve progression in adolescent idiopathic scoliosis. J. Bone Joint Surg. Am. 2010, 92, 1343–1352. [Google Scholar] [CrossRef] [PubMed]
- Brigham, E.M.; Armstrong, D.G. Motivations for Compliance with Bracing in Adolescent Idiopathic Scoliosis. Spine Deform. 2017, 5, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Yang, Y.; Dang, X.; Zhao, L.; Ren, J.; Zhang, L.; Sun, J. Factors relating to curve progression in female patients with adolescent idiopathic scoliosis treated with a brace. Eur. Spine J. 2015, 24, 244–248. [Google Scholar] [CrossRef] [PubMed]
- Emans, J.B.; Kaelin, A.; Bancel, P.; Hall, J.E.; Miller, E.M. The Boston bracing system for idiopathic scoliosis. Follow-up results in 295 patients. Spine 1986, 11, 792–801. [Google Scholar] [CrossRef] [PubMed]
- Lenke, L.G.; Betz, R.R.; Harms, J.; Bridwell, K.H.; Clements, D.H.; Lowe, T.G.; Blanke, K. Adolescent idiopathic scoliosis: A new classification to determine extent of spinal arthrodesis. J. Bone Jt. Surg Am. 2001, 83, 1169–1181. [Google Scholar] [CrossRef]
- Rahman, T.; Bowen, J.R.; Takemitsu, M.; Scott, C. The association between brace compliance and outcome for patients with idiopathic scoliosis. J. Pediatr. Orthop. 2005, 25, 420–422. [Google Scholar] [CrossRef] [PubMed]
- Bogaart, M.V.D.; Van Royen, B.J.; Haanstra, T.M.; De Kleuver, M.; Faraj, S.S.A. Predictive factors for brace treatment outcome in adolescent idiopathic scoliosis: A best-evidence synthesis. Eur. Spine J. 2019, 28, 511–525. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Qin, X.; Qiu, Y.; Zhu, Z. Initial Correction Rate Can be Predictive of the Outcome of Brace Treatment in Patients With Adolescent Idiopathic Scoliosis. Clin. Spine Surg. 2017, 30, E475–E479. [Google Scholar] [CrossRef] [PubMed]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Diagnosed with idiopathic scoliosis | Diagnosed with non-idiopathic scoliosis |
| Major curve Cobb angle was <50 degrees at study inclusion | Patients with non-progressive scoliosis 1 |
| Patients underwent surgical correction after failed brace treatment | Previous spinal surgery during bracing period |
| Follow-up of the bracing period was with radiographs | Radiographs in braces other than the Boston brace |
| Follow-up of the bracing period was at least 18 months | |
| Radiographs and patients data were available |
| Criterion | n | In-Brace Group (n = 25) | n | Out-of-Brace Group (n = 26) | p-Value |
|---|---|---|---|---|---|
| Gender, female (%) | 25 | 22 (88.0%) | 26 | 24 (92.3%) | 0.61 |
| Age at start of Boston brace treatment | 25 | 11.0 ± 2.7 | 26 | 11.7 ± 2.0 | 0.26 |
| Pre-brace Cobb angle | 18 | 40.0 ± 7.4 | 26 | 37.7 ± 7.8 | 0.32 |
| Pre-brace Lenke classification, curve type 1 (%) | 25 | 20 (80%) | 26 | 24 (92%) | 0.20 |
| Brace initiation before menarche (%) | 21 | 15 (71.4%) | 24 | 19 (79.2%) | 0.55 |
| Initial in-brace correction | 18 | 19.5% ± 16.4 | 21 | 37.3% ± 18.1 | <0.01 * |
| Study follow-up duration (years) | 25 | 3.4± 2.0 | 26 | 3.3 ± 1.3 | 0.78 |
| Duration of brace treatment (years) | 25 | 4.1 ± 2.1 | 25 | 3.6 ± 1.6 | 0.37 |
| Age at surgery | 25 | 15.0 ± 1.6 | 25 | 15.3 ± 1.8 | 0.57 |
| Preoperative Cobb angle out-of-brace † | 11 | 57.9 ± 8.0 | 26 | 52.5 ± 9.7 | 0.11 |
| Measurement | Estimate in CA In-Brace Group | Estimate in CA Out-of-Brace Group | Mean Difference | SE∆ | p-Value | 95% CI∆ |
|---|---|---|---|---|---|---|
| Mean curve progression 1 | 22.9 (SD = 15.3) | 15.2 (SD = 7.9) | 7.6 | 3.4 | 0.03 * | 0.80–14.45 |
| Monthly curve progression 2 | 0.5 | 0.5 | 0.0 | 0.1 | 0.80 | −0.09–0.11 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peeters, C.M.M.; van Hasselt, A.J.; Wapstra, F.-H.; Jutte, P.C.; Kempen, D.H.R.; Faber, C. In-Brace versus Out-of-Brace Protocol for Radiographic Follow-Up of Patients with Idiopathic Scoliosis: A Retrospective Study. Children 2022, 9, 465. https://doi.org/10.3390/children9040465
Peeters CMM, van Hasselt AJ, Wapstra F-H, Jutte PC, Kempen DHR, Faber C. In-Brace versus Out-of-Brace Protocol for Radiographic Follow-Up of Patients with Idiopathic Scoliosis: A Retrospective Study. Children. 2022; 9(4):465. https://doi.org/10.3390/children9040465
Chicago/Turabian StylePeeters, Charles M. M., Arthur J. van Hasselt, Frits-Hein Wapstra, Paulus C. Jutte, Diederik H. R. Kempen, and Christopher Faber. 2022. "In-Brace versus Out-of-Brace Protocol for Radiographic Follow-Up of Patients with Idiopathic Scoliosis: A Retrospective Study" Children 9, no. 4: 465. https://doi.org/10.3390/children9040465
APA StylePeeters, C. M. M., van Hasselt, A. J., Wapstra, F.-H., Jutte, P. C., Kempen, D. H. R., & Faber, C. (2022). In-Brace versus Out-of-Brace Protocol for Radiographic Follow-Up of Patients with Idiopathic Scoliosis: A Retrospective Study. Children, 9(4), 465. https://doi.org/10.3390/children9040465







