Abstract
Monitoring of antibiotic prescription and consumption behavior is crucial. The Access, Watch, and Reserve (AWaRe) classification of antibiotics has been recently introduced in order to measure and improve patterns of antibiotic use. In this study, retrospective data about systemic antibiotic consumption (expressed in defined daily dose per 1000 inhabitants per day (DID)) in pediatric outpatients in a region in northern Spain (around 100,000 children up to 14 years old) from 2005 to 2018 were analyzed and compared with antibiotic consumption in general population in Spain. The pattern of use was analyzed by the percentage of the current AWaRe categories, the Access-to-Watch index, and the amoxicillin index. Data were calculated annually and compared into two periods. Mean antibiotic consumption in pediatric outpatients was 14.0 DID (CI 95% 13.38–14.62). It remained stable throughout the study and was lower than consumption in general population in Spain, particularly from 2016. Changes in the consumption of the main active principles have led to an improvement in the three metrics of the pattern of use. It is important to have a thorough knowledge of the methodology applied in studies about antibiotic consumption. There is a lack of an optimal standardized metric for the pediatric population.
1. Introduction
Reducing unnecessary and inappropriate use of antibiotics is a public health priority. Continuous monitoring of antibiotic prescription and consumption behavior is essential to control increasing antibiotic resistance worldwide [1].
The World Health Organization (WHO) launched the Global Antimicrobial Resistance and Use Surveillance System (GLASS) in 2015, which collects data on antibiotic consumption of 65 countries [2]. The European Centre for Disease Prevention and Control (ECDC), through the European Surveillance of Antimicrobial Consumption Network (ESAC-Net), has been monitoring antibiotic consumption in community and hospital sectors in 31 European countries since 1997, describing a high variability between countries. There is a north-to-south and west-to-east increasing gradient in terms of antibiotic consumption and bacterial resistance. Spain is one of the European countries with higher rates of antibiotic consumption and bacterial resistances [3].
The ECDC collects antibiotic consumption information according to the Defined Daily Dose (DDD) methodology developed by the WHO Collaborating Centre for Drug Statistics Methodology. In January 2019, this organism changed the DDDs for several antibiotics [4]. Moreover, the WHO introduced the Access, Watch, and Reserve (AWaRe) classification of antibiotics as part of the updated 2017 Model List of Essential Medicines. Access antibiotics are used as first- or second-line therapies and should be available at an affordable cost (mostly penicillins, sulfonamides, and first-generation cephalosporins), Watch antibiotics are recommended only for specific indications (mostly second and third cephalosporins, fluoroquinolones, and macrolides) and Reserve antibiotics include those of last resort (such as new carbapenems and glycopeptides, fifth-generation cephalosporins, and polymyxins). In 2019, the category of Not Recommended antibiotics was added to the framework, consisting of fixed-dose combinations of multiple broad-spectrum antibiotics that are not evidence based. This classification was developed to measure and drive improvement in antibiotic stewardship efforts on global, regional, and national levels and better understanding of national patterns of antibiotic use. There is a WHO global and national level target for Access antibiotics to account for at least 60% of overall antibiotic consumption by 2023 [5].
Antibiotics are among the most commonly prescribed drugs in pediatrics [6,7]. Nevertheless, units of measure used in most of these monitoring programs are not accurate to control the consumption in this population, as they do not take into account the particularity of children’s dosage regarding the weight [1,8].
This study aims to describe antibiotic consumption and to analyze the pattern of antibiotic use in pediatric outpatients in a region in northern Spain, pointing out difficulties when analyzing data of antibiotic consumption, particularly in children.
2. Materials and Methods
2.1. Study Setting and Population
Retrospective and descriptive study about consumption of antibacterials for systemic use (J01 group of the Anatomical Therapeutic Chemical Classification, ATC) in pediatric outpatients (up to 14 years old) from 2005 to 2018 in Principado de Asturias, a region in northern Spain, with 101,767 children protected by the National Health System in 2018. Data were collected from the billing data of the containers dispensed in the pharmacy offices run by the National Health System.
2.2. Metrics of Antibiotic Consumption and Pattern of Antibiotic Use
Information about antibiotic consumption was expressed as DDD per 1000 inhabitants per day (DID) according to the latest and the previous available ATC/DDD index [9,10]. DIDs were calculated annually and aggregated by J01 group, therapeutic group, and active principle levels. Global data were contrasted to information about antibiotic consumption in Spanish general population by the ECDC [3,9,10].
To analyze the pattern of use, antibiotics were classified into the four current AWaRe categories: Access, Watch, Reserve, and Not Recommended. Antibiotics that could not be assigned to the AWaRe categories were left unclassified categories [5]. Three metrics of pattern of antibiotic use were calculated: first, the percentage of Access, Watch, Reserve, and Not Recommended antibiotic consumption (the DIDs of antibiotics in each group divided by the total DIDs); second, the Access-to-Watch index (the ratio of DIDs of Access antibiotics to Watch antibiotics); and third, the amoxicillin index (the DIDs of amoxicillin divided by the total DIDs) as the recommended first-line therapy for respiratory tract infections, which are the most common indication for antibiotic prescriptions in pediatrics [11,12].
2.3. Statistical Analyses
Antibiotic consumption and the pattern of use were calculated annually and compared into two periods (2005–2011 and 2012–2018). From the middle of 2018, an antibiotic stewardship program was implemented in our region, following the guidelines of the National Plan of Antimicrobial Resistance (PRAN) [13]. This program started in the hospital sector, and therefore, our results have not been affected by this strategy. Descriptive analyses were performed using means and confidence intervals of 95% (CI 95%), and variables were compared using the Student’s t-test. Statistical analyses were performed using IBM SPSS Statistics software (Statistical Package for the Social Sciences) version 23.0. The statistical significance level was defined as a two-tailed p-value < 0.05.
3. Results
3.1. Antibiotic Consumption
Mean antibiotic consumption in pediatric outpatients in Asturias, a region in northern Spain, between 2005 and 2018 was 14.0 DID (CI 95% 13.38–14.62), showing no statistically significant changes between periods. Figure 1 represents evolution of consumption of antibacterials for systemic use in the pediatric population in the community sector compared to consumption in Spanish general population published by the ECDC according to the previous and the latest ATC/DDD index [9,10].
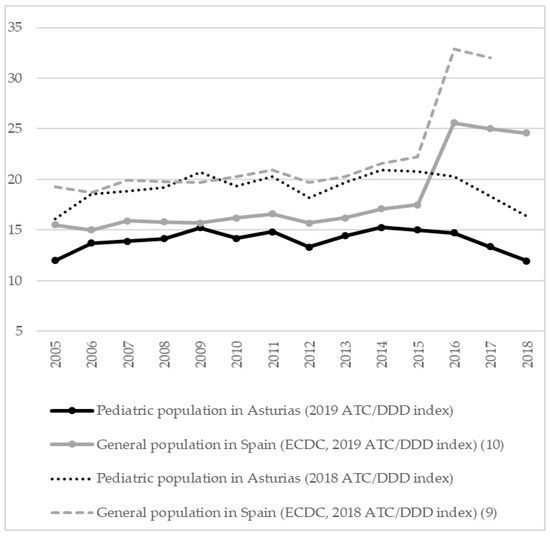
Figure 1.
Antibiotic consumption (DID) in the community sector in pediatric outpatients in Asturias and Spanish general population (2005–2018). DID, defined daily dose (DDD) per 1000 inhabitants per day.
The most consumed therapeutic groups were J01C (β-lactam penicillins, 10.7 DID; 76.7%), J01F (macrolides, lincosamides, and streptogramins, 1.8 DID; 12.8%), and J01D (other β-lactam antibacterials, referring to cephalosporins, 1.2 DID; 8.9%). The consumption of ten active principles represented 97.6% of the global use, and the consumption of amoxicillin and amoxicillin-clavulanate accounted for 72.8%. Consumption of amoxicillin, phenoxymethylpenicillin, azithromycin, and doxycycline significantly increased, whereas consumption of cefuroxime, cefixime, and clarithromycin decreased throughout the study (Table 1).

Table 1.
Consumption (DID) of total and most commonly used antibiotics and pattern of use in pediatric outpatients in Asturias. Global data and comparison between periods.
3.2. Pattern of Antibiotic Use
The consumption of Access antibiotics was greater than 70% every year (minimum of 71.5% in 2005, maximum of 80.4% in 2015; Figure 2), and both Access-to-Watch index and amoxicillin index significantly increased overtime (Table 1).
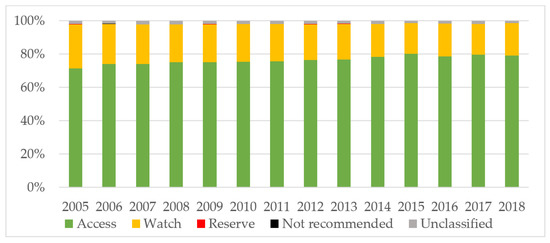
Figure 2.
Consumption of antibiotics (%) according to the AWaRe classification in pediatric outpatients in Asturias (2005–2018). AWaRe: Access, Watch, and Reserve antibiotics.
4. Discussion
The present study is the first carried out about antibiotic consumption and pattern of use in the entire pediatric population in our region, placed in northern Spain during a long time period. Furthermore, it shows the differences with antibiotic consumption in the Spanish general population and points out several difficulties when interpreting official data about this topic. The study shows that antibiotic consumption in the pediatric community sector in the study site was lower than consumption in general population in Spain, particularly from 2016, and that the pattern of antibiotic use improved throughout the study.
Readers must be aware of several aspects about interpreting data of antibiotic consumption. First, the ECDC collects antibiotic consumption information according to the DDD methodology developed by the WHO Collaborating Centre for Drug Statistics Methodology [4]. One DDD is the assumed average maintenance dose per day for a drug used in its main indication in a 70 kg adult. DDD is a technical unit of measurement and not a standard for appropriate use, but it makes possible to aggregate information about substances with different pack sizes, strengthening it into units of measurement of active substances. DID represents a standard in performing valid and reliable cross-national or longitudinal studies of antibiotic consumption, and thus, it allows to compare data between regions and countries. DID has been selected as the primary harmonized outcome indicator by the ECDC, the European Food Safety Authority (EFSA), and the European Medicines Agency (EMA) [14,15].
DDD values may be modified over time because of changes in the main indication or amendments for the recommended or prescribed daily dose. In January 2019, the WHO Collaborating Centre for Drug Statistics Methodology changed the DDDs for several antibiotics, including those with the highest consumption in the Spanish community sector: amoxicillin and amoxicillin-clavulanate (both from 1 g to 1.5 g) [4]. Historical ESAC-Net data on antibiotic consumption since 1997 were recalculated accordingly, following the normative to report all data from all years with the latest available ATC/DDD index. Thus, recent data displayed in the interactive database differ from those in historical annual epidemiological reports. Data may appear to be lower at present than previously, with the largest impact for the penicillins group [3,4,9,14]. Readers must be aware of these changes when comparing current data with that published in scientific papers until 2019. We observed a decline around 25% of antibiotic consumption rates in our pediatric population according to the latest ATC/DDD index, similar to the difference observed in the Spanish general population after the ATC/DDD update [9,14,15].
Second, there has been a noticeable increase of antibiotic consumption rates in Spain since 2016. Spain changed the source to report community consumption data from 2016 onwards from reimbursement data to National Health System to sales data, which resulted in a substantial technical increase of antibiotic consumption compared with previous years. The major limitation of reimbursement data is that antibiotics dispensed without a prescription and non-reimbursed prescribed antibiotics are not included. Spanish data are currently more reliable and comparable with those of other countries, as just a quarter of countries reporting information to ESAC-Net still provide reimbursement data [3]. Rates of Spanish antibiotic consumption are worrisome. In 2019, Spain was the fifth European country with the highest antibiotic consumption in the community sector, reaching 23.3 DID. This number is above the European mean (18 DID), while a significant decrease in the mean consumption of antibacterials in Europe was observed over the last ten years [14]. Although prohibited in Spain since 2002, dispensing antibiotics without a medical prescription is still a notorious problem. In simulated scenarios, an antibiotic is sold in 35% to 54% of times when it is requested without prescription [16,17]. Furthermore, there is a high prescription of antibiotics in the private sector in several regions in Spain [13].
Third, prescriptions in children are commonly based on patient weight. Measuring antibiotic consumption by DDD can be found questionable in children, as it quantifies the volume of antibiotic administered but does not take into account body weight. Over 25 different measures can be found to describe antibiotic use in pediatric population, referring to the proportion of exposed patients and quantity and duration of antibiotic therapy [18]. The current recommendation metric in hospitalized patients for pediatric antibiotic stewardship programs is the number of days of therapy (DOT). Antibiotic DDD adjusted by weight has been recently developed for pediatric inpatients; this measure is highly correlated with DOT and names DDD in mg/kg, a standard not defined by the ATC/DDD system [1,8]. These measures have their application in the hospital sector and require patient-level data often inaccessible in studies in the community sector. DDD can still be used to follow antibiotic use density in populations where patients’ average weight is constant, as it could be in an entire pediatric population in a region such as ours [18].
In relation to the pattern of antibiotic use, the majority of non-Access antibiotic consumption in our study was from Watch Antibiotics, with Reserve and Not Recommended antibiotic consumption accounting for less than 0.15%. We observed an improvement in the pattern of antibiotic use in our population in the three mentioned metrics. Azithromycin was the main Watch antibiotic whose consumption increased over time in our study and the active principle with the highest increase in the study region [19]. Recent data on pediatric outpatient antibiotic stewardship suggest focusing on prescriptions of azithromycin in order to decrease antibiotic use [20,21]. Spain achieved the target in the WHO AWaRe framework of at least 60% of Access antibiotics in general population in 2004 and has increased since then up to 68.5% in 2015 [22]. Access antibiotics in our population were above 70% every year. However, our data are still inferior to that presented in the pediatric Spanish population, notifying 90% of Access antibiotics, Access-to-Watch index beyond 10, and amoxicillin index around 0.5 in 2015 [11].
The main current and global problem is the increasing consumption of both Access and Watch antibiotics, with the consumption of Watch antibiotics rising much faster than Access antibiotics, especially in low- and middle-income countries. This challenges the achievement of the AWaRe target for Access antibiotics to account for 60% of the global consumption by 2023 in these countries [11,22,23]. The use of the amoxicillin index can inform the development of initiatives to improve the use of amoxicillin and other Access antibiotics. Countries characterized by high consumption of amoxicillin have national guidelines for the treatment of respiratory tract infections supporting the use of this drug [12]. The AWaRe antibiotic classification provides a useful framework for exploring national antibiotic-consumption patterns [5,11,22,23].
Our study presents several limitations, mostly derived from the analysis and comparison of antibiotic consumption given the already-mentioned particularities of the different populations and measures and changes on the methodology. We did not include data about the hospital sector, below 1.5% of global consumption in our population [19], since the objective was to analyze the consumption and the pattern of antibiotic use in the pediatric community. We did not include data about antibiotic consumption without prescription, estimated at around 8% in the Spanish pediatric population in simulated scenarios [24], or about prescription of antibiotics in the private sector, but we do not expect to have a high rate in our population, as 98% of the pediatric population is covered by the National Health System [19].
5. Conclusions
Antibiotic consumption in pediatric outpatients between 2005 and 2018 in the study region, placed in northern Spain, remained stable and was lower than consumption in the general Spanish population. The pattern of antibiotic use improved throughout the study, but some points, such as increasing the amoxicillin index or controlling consumption of some Watch antibiotics, such as azithromycin, need to be improved. There is still a lack of an optimal standardized metric for the pediatric population. The reader must take into account the different methods of measurements and major changes on the data collection methodology used by the main international consumption surveillance systems when interpreting and comparing data about antibiotic consumption.
Author Contributions
Conceptualization, C.P.-M.; methodology, L.C.-M. and G.S.-S.; software, L.C.-M.; validation, G.S.-S. and C.P.-M.; formal analysis, G.S.-S.; investigation, E.G.-G.; resources, B.M.-P.; data curation, B.M.-P.; writing—original draft preparation, L.C.-M. and G.S.-S.; writing—review and editing, C.P.-M., E.G.-G. and B.M.-P.; visualization, C.P.-M. and B.M.-P.; supervision, E.G.-G.; project administration, L.C.-M.; funding acquisition, L.C.-M. All authors have read and agreed to the published version of the manuscript.
Funding
L.C.-M. was funded by Fundación Ernesto Sánchez Villares, grant number 2020/08 (from the Sociedad de Pediatría de Asturias, Cantabria y Castilla y León, SCCALP) with 500 euros for the development of this study. The remain authors received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Comité de Ética de Investigación del Principado de Asturias (protocol code 2020.191 and date of approval 4 May 2020).
Informed Consent Statement
Patient consent was waived due to the fact that all data used were population data, and no personal or identifiable information was collected.
Data Availability Statement
Restrictions apply to the availability of these data. Data were obtained by a permission from the Sub-Direction of the Organization of Health System of Principado de Asturias. All the authors have full access to the data, and L.C.-M. is the guarantor for the data.
Acknowledgments
Authors express their gratitude to Gracia Modroño Riaño and Maria Isabel Iglesias Carbajo (specialists in Hospital Pharmacy) and to Fundación Ernesto Sánchez Villares for the donation of a grant for the development of this study.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Ibrahim, O.M.; Polk, R.E. Antimicrobial use metrics and benchmarking to improve stewardship outcomes. Methodology, opportunities and challenges. Infect. Dis. Clin. N. Am. 2014, 28, 195–214. [Google Scholar] [CrossRef] [PubMed]
- Global Antimicrobial Resistance Surveillance System (GLASS) Report: Early Implementation 2020; World Health Organization: Geneva, Switzerland, 2020.
- European Center for Disease Prevention and Control. Antimicrobial Consumption Database (ESAC-Net). Available online: https://www.ecdc.europa.eu/en/antimicrobial-consumption/surveillance-and-disease-data/database (accessed on 1 February 2021).
- World Health Organization. ATC/DDD: WHO Collaborating Centre for Drug Statistics Methodology. Available online: https://www.whocc.no/atc_ddd_methodology/purpose_of_the_atc_ddd_system (accessed on 5 February 2021).
- World Health Organization Model list of Essential Medicines, 21st List; World Health Organization: Geneva, Switzerland, 2019.
- Chua, K.-P.; Volerman, A.; Conti, R.M. Prescription Drug Dispensing to US Children during the COVID-19 Pandemic. Pediatrics 2021, 148, e2021049972. [Google Scholar] [CrossRef] [PubMed]
- Youngster, I.; Avorn, J.; Belleudi, V.; Cantarutti, A.; Diez-Domingo, J.; Kirchmayer, U.; Park, B.-J.; Peiró, S.; Sanfélix-Gimeno, G.; Schröder, H.; et al. Antibiotic Use in Children—A Cross-National Analysis of 6 Countries. J. Pediatr. 2017, 182, 239–244. [Google Scholar] [CrossRef] [PubMed]
- Montecatine-Alonso, E.; Gil-Navarro, M.-V.; Fernández-Llamazares, C.M.; Fernández-Polo, A.; Soler-Palacín, P.; Llorente-Gutiérrez, J.; Calvo, M.-T.G.-T.; Esquivel-Mora, M.-D.; Pérez-Rodrigo, I.; Cisneros, J.M.; et al. Antimicrobial defined daily dose adjusted by weight: A proposal for antibiotic consumption measurement in children. Enferm. Infecc. Microbiol. Clin. 2019, 37, 301–306. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Antimicrobial consumption. In Annual Epidemiological Report for 2017; ECDC: Stockholm, Sweden, 2018. [Google Scholar]
- European Centre for Disease Prevention and Control. Antimicrobial consumption in the EU/EEA. In Annual Epidemiological Report for 2018; ECDC: Stockholm, Sweden, 2019. [Google Scholar]
- Hsia, Y.; Sharland, M.; Jackson, C.; Wong, I.C.K.; Magrini, N.; Bielicki, J.A. Consumption of oral antibiotic formulations for young children according to the WHO Access, Watch, Reserve (AWaRe) antibiotic groups: An analysis of sales data from 70 middle-income and high-income countries. Lancet Infect. Dis. 2019, 19, 67–75. [Google Scholar] [CrossRef]
- Huttner, A.; Bielicki, J.; Clements, M.; Frimodt-Møller, N.; Muller, A.; Paccaud, J.-P.; Mouton, J. Oral amoxicillin and amoxicillin-clavulanic acid: Properties, indications and usage. Clin. Microbiol. Infect. 2020, 26, 871–879. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Sanidad, Servicios Sociales e Igualdad. Plan Nacional de Resistencia Antibióticos (PRAN). Available online: http://www.resistenciaantibioticos.es/es (accessed on 12 March 2021).
- European Centre for Disease Prevention and Control. Antimicrobial Consumption in the EU/EEA. In Annual Epidemiological Report 2019; ECDC: Stockholm, Sweden, 2020. [Google Scholar]
- European Centre for Disease Prevention and Control. Antimicrobial consumption (AMC) reporting protocol 2020. In European Surveillance of Antimicrobial Consumption Network (ESAC-Net) Surveillance Data for 2019; ECDC: Stockholm, Sweden, 2020. [Google Scholar]
- Scuri, S.; Petrelli, F.; Tanzi, E.; Thu, C.N.T.; Grappasonni, I. European university students of pharmacy: Survey on the use of pharmaceutical drugs. Acta Biomed. 2019, 90, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Guinovart, M.C.; Figueras, A.; Llop, J.C.; Llor, C. Obtaining antibiotics without prescription in Spain in 2014: Even easier now than 6 years ago. J. Antimicrob. Chemother. 2015, 70, 1270–1271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fortin, E.; Fontenla, P.S.; Manges, A.R.; Platt, R.W.; Buckeridge, D.L.; Quach, C. Measuring antimicrobial use in hospitalized patients: A systematic review of available measures applicable to paediatrics. J. Antimicrob. Chemother. 2014, 69, 1447–1456. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Calle-Miguel, L.; Carbajo, A.I.I.; Riaño, G.M.; Méndez, C.P.; García, E.G.; Nebreda, S.R.; Sánchez, G.S. Evolution of antibiotic consumption in pediatric outpatients of Asturias, Spain (2005–2018). An. Pediatr. 2021, 95, 438–447. [Google Scholar] [CrossRef] [PubMed]
- Watson, J.R.; Wang, L.; Klima, J.; Moore-Clingenpeel, M.; Gleeson, S.; Kelleher, K.; Jaggi, P. Healthcare Claims Data: An Underutilized Tool for Pediatric Outpatient Antimicrobial Stewardship. Clin. Infect. Dis. 2017, 64, 1479–1485. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.-N.; Huttner, B.; Magrini, N.; Cheng, Y.; Tong, J.; Li, S.; Wan, C.; Zhu, Q.; Zhao, S.; Zhuo, Z.; et al. Pediatric Antibiotic Prescribing in China According to the 2019 World Health Organization Access, Watch, and Reserve (AWaRe) Antibiotic Categories. J. Pediatr. 2020, 220, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Klein, E.Y.; Milkowska-Shibata, M.; Tseng, K.K.; Sharland, M.; Gandra, S.; Pulcini, C.; Laxminarayan, R. Assessment of WHO antibiotic consumption and access targets in 76 countries, 2000–2015: An analysis of pharmaceutical sales data. Lancet Infect. Dis. 2020, 21, 107–115. [Google Scholar] [CrossRef]
- Jackson, C.; Hsia, Y.; Bielicki, J.A.; Ellis, S.; Stephens, P.; Wong, I.C.K.; Sharland, M. Estimating global trends in total and childhood antibiotic consumption, 2011-2015. BMJ Glob. Health 2019, 27, e001241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simó, S.; Fraile, D.; Sánchez, A.; García-Algar, O. Dispensing of over-the-counter drugs in pharmacies. An. Pediatr. 2013, 79, 10–14. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).