Impact of the COVID-19 Pandemic on Emergency Care Utilization and Outcomes in Pediatric Patients with Intussusception
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Data Source
2.2. Study Period
2.3. Participant Selection
2.3.1. Inclusion Criteria
2.3.2. Exclusion Criteria
2.4. Measurements
2.5. Outcomes
2.6. Statistical Analysis
3. Results
3.1. Characteristics of the Patients
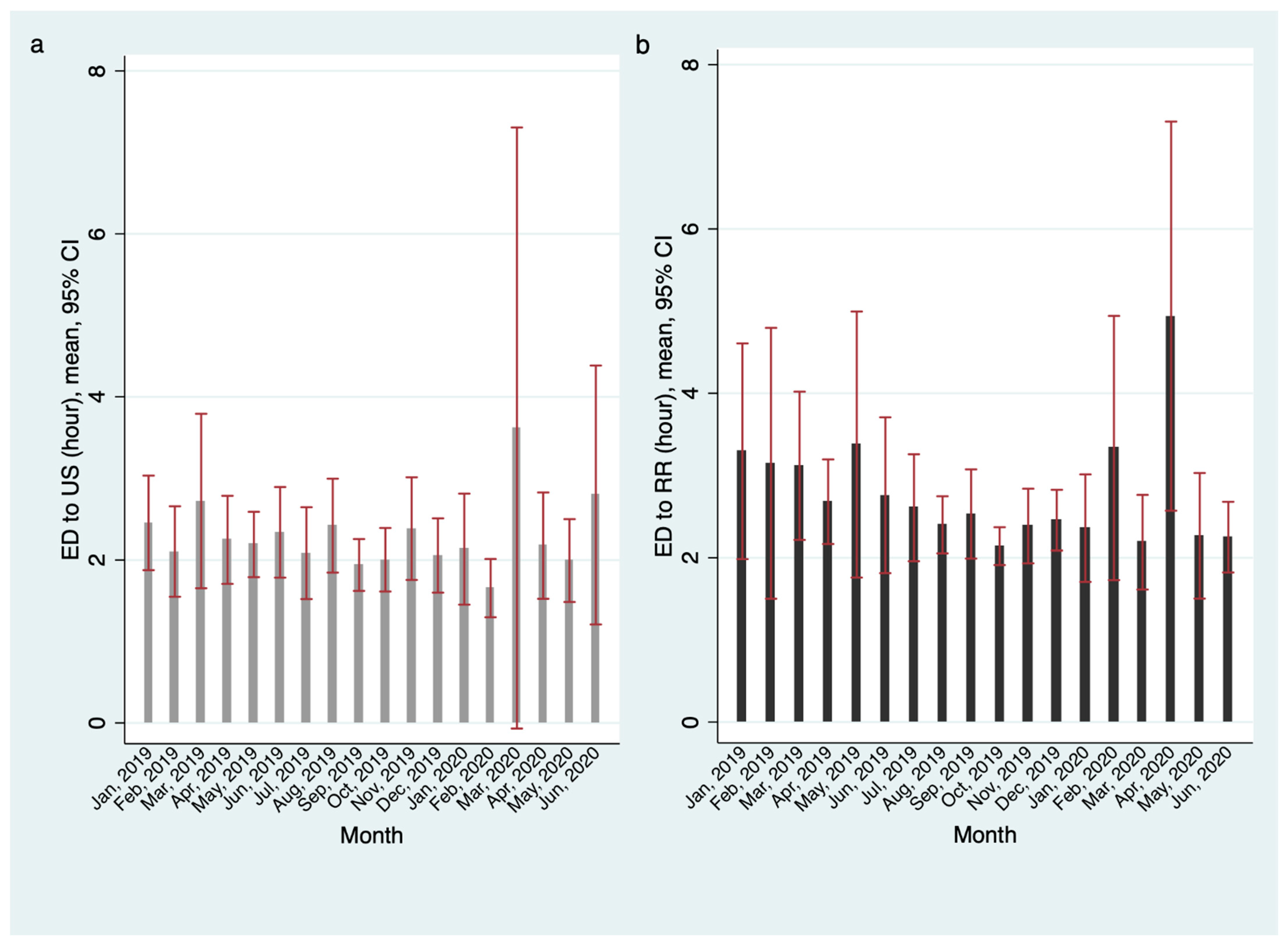
3.2. Primary Outcomes
3.3. Secondary Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lim, B.; Hong, E.K.; Mou, J.; Cheong, I. COVID-19 in Korea: Success Based on Past Failure. Asian Econ. Pap. 2021, 20, 41–62. [Google Scholar] [CrossRef]
- Dopfer, C.; Wetzke, M.; Scharff, A.Z.; Mueller, F.; Dressler, F.; Baumann, U.; Sasse, M.; Hansen, G.; Jablonka, A.; Happle, C. COVID-19 related reduction in pediatric emergency healthcare utilization—A concerning trend. BMC Pediatr. 2020, 20, 427. [Google Scholar] [CrossRef] [PubMed]
- Liguoro, I.; Pilotto, C.; Vergine, M.; Pusiol, A.; Vidal, E.; Cogo, P. The impact of COVID-19 on a tertiary care pediatric emergency department. Eur. J. Pediatr. 2021, 180, 1497–1504. [Google Scholar] [CrossRef]
- Choi, A.; Bae, W.; Kim, K.; Kim, S. Impact of COVID-19 on the Visit of Pediatric Patients with Injuries to the Emergency Department in Korea. Children 2021, 8, 568. [Google Scholar] [CrossRef]
- Choi, D.H.; Jung, J.Y.; Suh, D.; Choi, J.Y.; Lee, S.U.; Choi, Y.J.; Kwak, Y.H. Impact of the COVID-19 Outbreak on Trends in Emergency Department Utilization in Children: A Multicenter Retrospective Observational Study in Seoul Metropolitan Area, Korea. J. Korean Med. Sci. 2021, 36, e44. [Google Scholar] [CrossRef]
- Lee, D.E.; Ro, Y.S.; Ryoo, H.W.; Moon, S. Impact of temporary closures of emergency departments during the COVID-19 outbreak on clinical outcomes for emergency patients in a metropolitan area. Am. J. Emerg. Med. 2021, 47, 35–41. [Google Scholar] [CrossRef]
- Lock, J.F.; Wiegering, A. Changes in the management of acute appendicitis during the COVID-19 pandemic. Langenbeck’s Arch. Surg. 2021, 406, 503–504. [Google Scholar] [CrossRef]
- Delgado-Miguel, C.; Muñoz-Serrano, A.; Miguel-Ferrero, M.; Ceano-Vivas, M.D.; Calvo, C.; Martínez, L. Complicated Acute Appendicitis during COVID-19 Pandemic: The Hidden Epidemic in Children. Eur. J. Pediatr. Surg. 2021. [Google Scholar] [CrossRef]
- Ielpo, B.; Podda, M.; Pellino, G.; Pata, F.; Caruso, R.; Gravante, G.; Di Saverio, S.; ACIE Appy Study Collaborative. Global attitudes in the management of acute appendicitis during COVID-19 pandemic: ACIE Appy Study. Br. J. Surg. 2020, 108, 717–726. [Google Scholar] [CrossRef]
- Percul, C.; Cruz, M.; Curiel Meza, A.; González, G.; Lerendegui, L.; Malzone, M.C.; Liberto, D.; Lobos, P.; Imach, B.E.; Moldes, J.M.; et al. Impact of the COVID-19 pandemic on the pediatric population with acute appendicitis: Experience at a general, tertiary care hospital. Arch. Argent Pediatr. 2021, 119, 224–229. [Google Scholar]
- Saalabian, K.; Rolle, U.; Friedmacher, F. Impact of the Global COVID-19 Pandemic on the Incidence, Presentation, and Management of Pediatric Appendicitis: Lessons Learned from the First Wave. Eur. J. Pediatr. Surg. 2021, 31, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Melander, S.; Almström, J.; Enlund, G.; Frykholm, P. The COVID-19 pandemic first wave in Sweden: A national registry study of the effects on pediatric anesthesia and surgery. Pediatr. Anesth. J. 2021, 31, 846–853. [Google Scholar] [CrossRef] [PubMed]
- Park, J.S.; Byun, Y.-H.; Choi, S.J.; Lee, J.S.; Ryu, J.-M.; Lee, J.-Y. Decreased Incidence of Pediatric Intussusception during COVID-19. Children 2021, 8, 1072. [Google Scholar] [CrossRef] [PubMed]
- Blakelock, R.T.; Beasley, S.W. Infection and the gut. Semin. Pediatr. Surg. 2003, 12, 265–274. [Google Scholar] [CrossRef]
- Moazzam, Z.; Salim, A.; Ashraf, A.; Jehan, F.; Arshad, M. Intussusception in an infant as a manifesta- tion of COVID-19. J. Pediatr. Surg. Case Rep. 2020, 59, 101533. [Google Scholar] [CrossRef]
- Cai, X.; Ma, Y.; Li, S.; Chen, Y.; Rong, Z.; Li, W. Clinical Characteristics of 5 COVID-19 Cases with Non-respiratory Symptoms as the First Manifestation in Children. Front. Pediatr. 2020, 8, 258. [Google Scholar] [CrossRef]
- Martínez-Castaño, I.; Calabuig-Barbero, E.; Gonzálvez-Piñera, J.; López-Ayala, J.M. COVID-19 Infection Is a Diagnostic Challenge in Infants With Ileocecal Intussusception. Pediatr. Emerg. Care 2020, 36, e368. [Google Scholar] [CrossRef]
- Bazuaye-Ekwuyasi, E.A.; Camacho, A.C.; Saenz Rios, F.; Torck, A.; Choi, W.J.; Aigbivbalu, E.E.; Mehdi, M.Q.; Shelton, K.J.; Radhakrishnan, G.L.; Radhakrishnan, R.S.; et al. Intussus- ception in a child with COVID-19 in the USA. Emerg. Radiol. 2020, 27, 761–764. [Google Scholar] [CrossRef]
- Sung, H.K.; Paik, J.H.; Lee, Y.J.; Kang, S. Impact of the COVID-19 Outbreak on Emergency Care Utilization in Patients with Acute Myocardial Infarction: A Nationwide Population-based Study. J. Korean Med. Sci. 2021, 36, e111. [Google Scholar] [CrossRef]
- Yoon, Y.-H.; Kim, J.-Y.; Choi, S.-H. Analysis of Patients with Acute Toxic Exposure between 2009 and 2013: Data from the Korea Health Insurance Review and Assessment Service and the National Emergency Department Information System. J. Korean Med. Sci. 2018, 33, e254. [Google Scholar] [CrossRef]
- Applegate, K.E. Intussusception in children: Evidence-based diagnosis and treatment. Pediatr. Radiol. 2009, 39, 140–143. [Google Scholar] [CrossRef] [PubMed]
- Pak, Y.S.; Ro, Y.S.; Kim, S.H.; Han, S.H.; Ko, S.K.; Kim, T.; Kwak, Y.H.; Heo, T.; Moon, S. Effects of Emergency Care-related Health Policies during the COVID-19 Pandemic in Korea: A Quasi-Experimental Study. J. Korean Med. Sci. 2021, 36, e121. [Google Scholar] [CrossRef] [PubMed]
- Ojetti, V.; Covino, M.; Brigida, M.; Petruzziello, C.; Saviano, A.; Migneco, A.; Candelli, M.; Franceschi, F. Non-COVID Diseases during the Pandemic: Where Have All Other Emergencies Gone? Medicina 2020, 56, 512. [Google Scholar] [CrossRef] [PubMed]
- Boeken, T.; Berre, A.L.; Mebazaa, A.; Boulay-Coletta, I.; Hodel, J.; Zins, M. Non-COVID-19 emergencies: Where have all the patients gone? Eur. Radiol. 2020, 30, 5220–5221. [Google Scholar] [CrossRef]
- Seo, S.; Suda, K.; Kato, H.; Abe, E.; Kosaka, S.; Fujiwara, K.; Ochi, T.; Koga, H.; Urao, M.; Okazaki, T. Decreased incidence of intussusception during the COVID-19 pandemic. Trends in pediatric surgical emergencies. Pediatr. Surg. Int. 2021, 37, 1761–1764. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare. Available online: http://ncov.mohw.go.kr/bdBoardList_Real.do?brdId=1&brdGubun=11&ncvContSeq=&contSeq=&board_id=&gubun= (accessed on 1 November 2021).

| Control Group 1 (Jan~Jun, 2019) | Control Group 2 (Jul~Dec, 2019) | Study Group (Jan~Jun, 2020) | Total | p | |||||
|---|---|---|---|---|---|---|---|---|---|
| Intussusception suspected | 1223 | 1576 | 624 | 3423 | |||||
| True intussusception, n (%) | 679 | (55.52%) | 959 | (60.85%) | 347 | (53.80%) | 1985 | (57.99%) | 0.007 |
| True intussusception, n/100,000 (person-half-year) | 7.85 | 11.30 | 4.19 | 7.77 | <0.05 | ||||
| Age, mean ± SD | 1.79 | ±1.54 | 1.77 | ±1.41 | 1.95 | ±1.87 | 1.81 | ±1.55 | 0.034 |
| Patients younger than 6 years old, n (%) | 1205 | (98.53%) | 1559 | (98.92%) | 608 | (97.44%) | 3372 | (98.51%) | |
| Male, n (%) | 771 | (63.04%) | 998 | (63.32%) | 394 | (63.14%) | 2163 | (63.19%) | 0.988 |
| Symptom duration (hr), mean ± SD | 20.21 | ±31.28 | 20.17 | ±42.65 | 20.85 | ±43.83 | 20.31 | ±39.20 | 0.931 |
| Intervention | |||||||||
| US, n (%) | 1087 | (88.99%) | 1407 | (89.28%) | 555 | (86.05%) | 3049 | (88.53%) | 5 |
| RR, n (%) | 664 | (54.29%) | 934 | (59.26%) | 333 | (51.63%) | 1931 | (56.07%) | 0.001 |
| SR, n (%) | 26 | (2.13%) | 34 | (2.16%) | 20 | (3.10%) | 80 | (2.32%) | 0.347 |
| The time to intervention | |||||||||
| ED~US (hr), mean ± SD | 2.34 | ±4.39 | 2.16 | ±3.92 | 2.35 | ±7.13 | 2.26 | ±4.83 | 0.575 |
| ED~RR (hr), mean ± SD | 3.04 | ±6.38 | 2.41 | ±2.87 | 2.79 | ±4.39 | 2.69 | ±4.61 | <0.05 |
| ED~SR (hr), mean ± SD | 11.61 | ±23.45 | 9.23 | ±21.37 | 10.11 | ±13.17 | 10.22 | ±20.19 | 0.904 |
| ED LOS (hr), mean ± SD | 4.62 | ±4.15 | 4.67 | ±4.10 | 4.68 | ±4.13 | 4.65 | ±4.12 | 0.928 |
| ED to US | ED to RR | ED to SR | ||||
|---|---|---|---|---|---|---|
| Difference | 95% CI | Difference | 95% CI | Difference | 95% CI | |
| Control 1 vs. 2 | −0.1829 | −0.6468~0.2809 | −0.6296 | −1.1762~−0.0830 | −2.3823 | −15.0973~10.3327 |
| Control 1 vs. Study | 0.0114 | −0.5848~0.6077 | −0.2501 | −0.9703~0.4699 | −1.4978 | −16.0137~13.0181 |
| Control 2 vs. Study | 0.1944 | −0.3783~0.7670 | 0.3794 | −0.3038~1.0627 | 0.8846 | −12.8688~14.6379 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.H.; Ro, Y.S.; Kwon, H.; Suh, D.; Moon, S. Impact of the COVID-19 Pandemic on Emergency Care Utilization and Outcomes in Pediatric Patients with Intussusception. Children 2022, 9, 277. https://doi.org/10.3390/children9020277
Lee JH, Ro YS, Kwon H, Suh D, Moon S. Impact of the COVID-19 Pandemic on Emergency Care Utilization and Outcomes in Pediatric Patients with Intussusception. Children. 2022; 9(2):277. https://doi.org/10.3390/children9020277
Chicago/Turabian StyleLee, Jin Hee, Young Sun Ro, Hyuksool Kwon, Dongbum Suh, and Sungwoo Moon. 2022. "Impact of the COVID-19 Pandemic on Emergency Care Utilization and Outcomes in Pediatric Patients with Intussusception" Children 9, no. 2: 277. https://doi.org/10.3390/children9020277
APA StyleLee, J. H., Ro, Y. S., Kwon, H., Suh, D., & Moon, S. (2022). Impact of the COVID-19 Pandemic on Emergency Care Utilization and Outcomes in Pediatric Patients with Intussusception. Children, 9(2), 277. https://doi.org/10.3390/children9020277







