Preparedness for Life-Threatening Situations in a Pediatric Tertiary-Care University Children’s Hospital: A Survey †
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
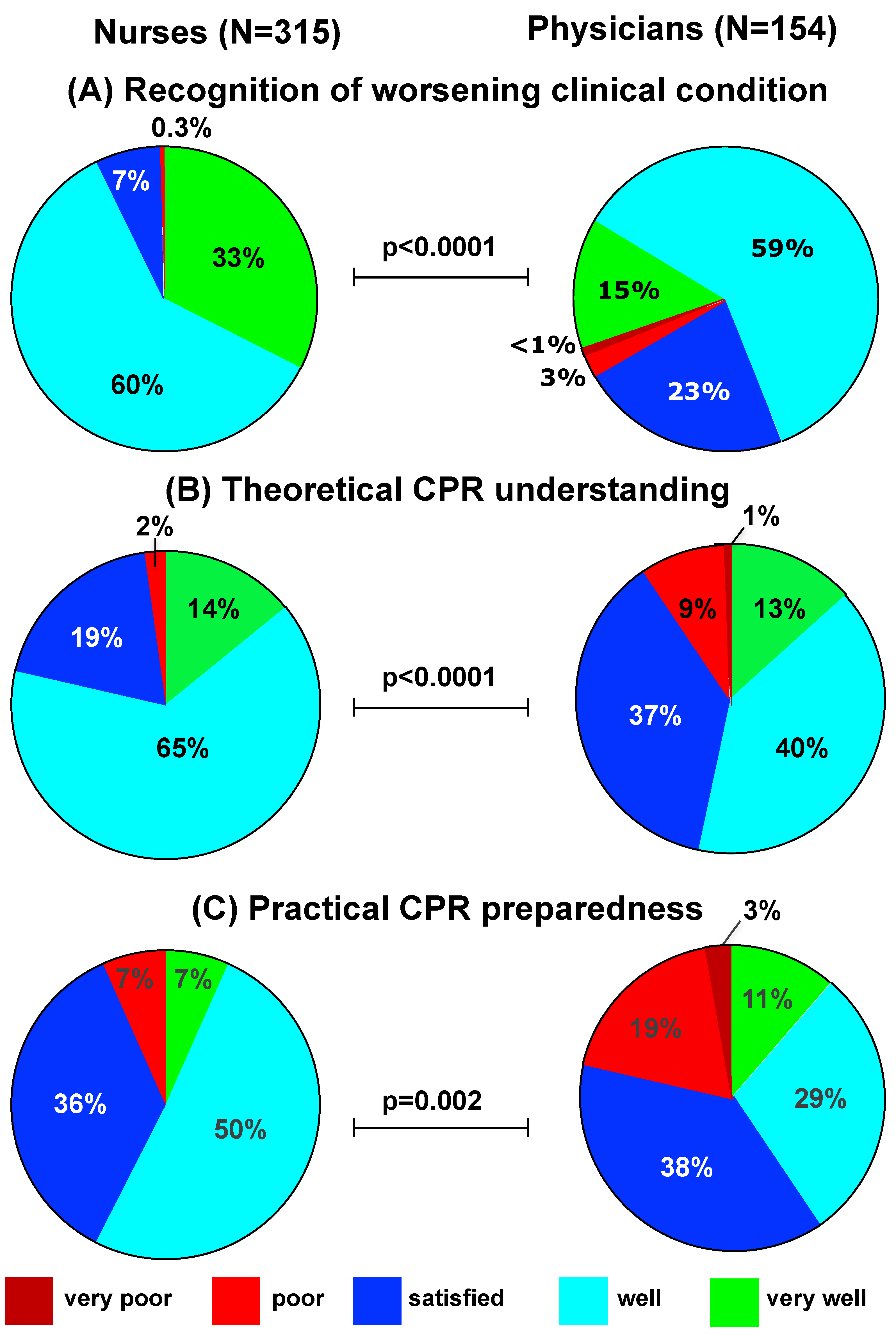
- (1)
- At first glance, the gap in training perception between nurses and physicians might be difficult to explain. However, importantly, the work experience of respondent nurses was significantly longer than that of participating physicians (Table 1). Furthermore, in Switzerland, nurses enjoy patient exposure at an earlier training stage compared to physicians, and the nurse–patient ratio is higher than the physician-patient ratio.
- (2)
- (3)
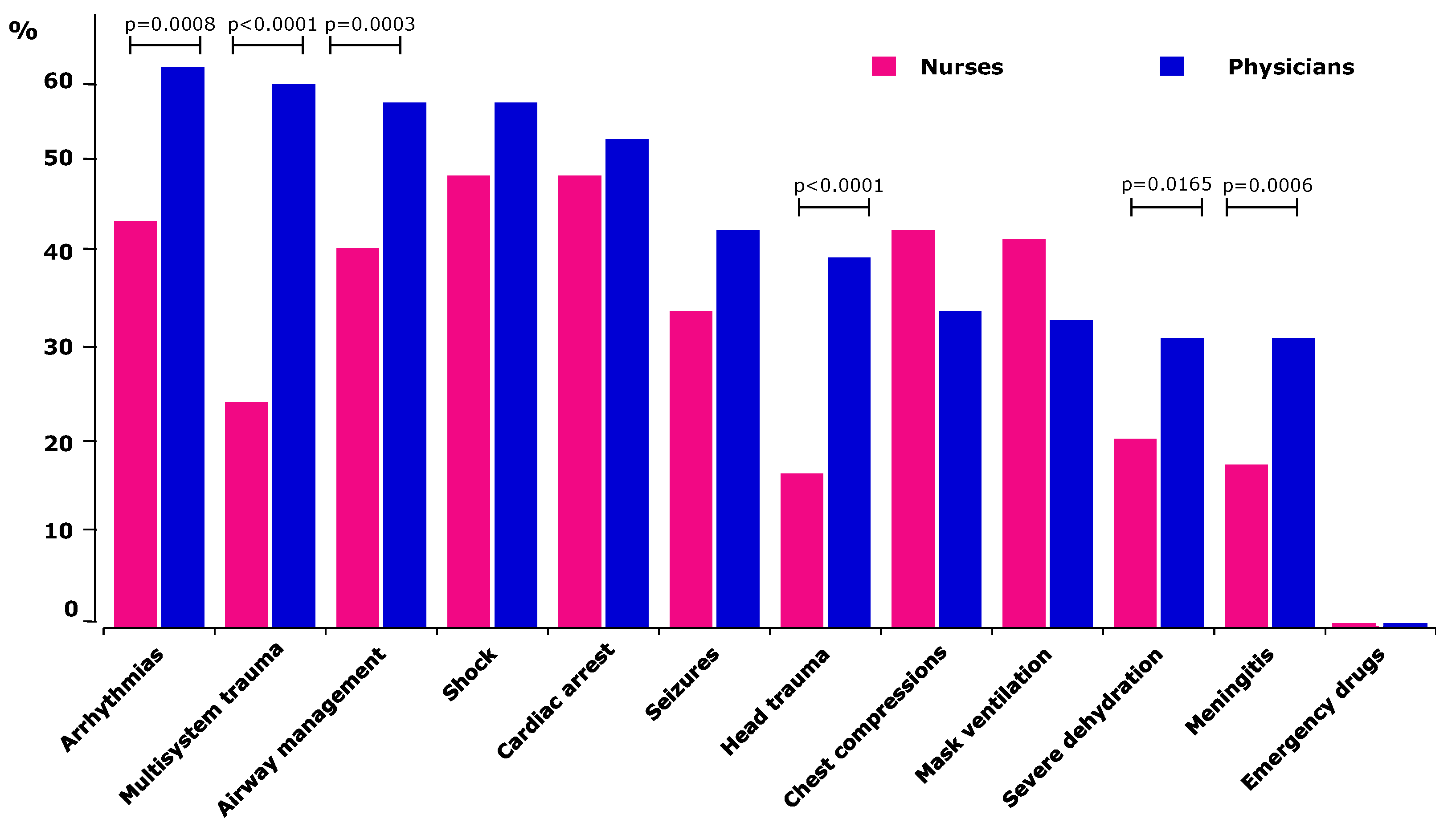
- Finally, the need for training appeared to favor certain clinical scenarios. On one side, it is remarkable that three out of the four most commonly cited areas of need (arrhythmias, cardiac arrest and shock) pertain to the domain of pediatric cardiology and intensive care. This might relate to the fact that these are rare but potentially life-threatening conditions. On the other side, emergency drugs were never cited as a training need. This is surprising, considering that medication errors are among the most potent contributors to iatrogenic morbidity and mortality [20]. An explanation might be that this is a global medical skill rather than a specific clinical scenario.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Topjian, A.A.; Berg, R.A.; Nadkarni, V.M. Pediatric cardiopulmonary resuscitation: Advances in science, techniques, and outcomes. Pediatrics 2008, 122, 1086–1098. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hunt, E.A.; Patel, S.; Vera, K.; Shaffner, D.H.; Pronovost, P.J. Survey of pediatric resident experiences with resuscitation training and attendance at actual cardiopulmonary arrests. Pediatr. Crit. Care Med. 2009, 10, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Jung, P.; Brenner, S.; Bachmann, I.; Both, C.; Cardona, F.; Dohna-Schwake, C.; Eich, C.; Eifinger, F.; Huth, R.; Heimberg, E.; et al. More Than 500 Kids Could Be Saved Each Year! Ten Consensus Actions to Improve Quality of Pediatric Resuscitation in DACH-Countries (Austria, Germany, and Switzerland). Front. Pediatr. 2020, 8, 549710. [Google Scholar] [CrossRef] [PubMed]
- Ames, S.G.; Davis, B.S.; Marin, J.R.; Fink, E.L.; Olson, L.M.; Gausche-Hill, M.; Kahn, J.M. Emergency Department Pediatric Readiness and Mortality in Critically Ill Children. Pediatrics 2019, 144, e20190568. [Google Scholar] [CrossRef] [PubMed]
- Ciurzynski, S.M.; Gottfried, J.A.; Pietraszewski, J.; Zalewski, M. Impact of Training Frequency on Nurses’ Pediatric Resuscitation Skills. J. Nurses Prof. Dev. 2017, 33, E1–E7. [Google Scholar] [CrossRef]
- Ralston, M.E.; Zaritsky, A.L. New opportunity to improve pediatric emergency preparedness: Pediatric emergency assessment, recognition, and stabilization course. Pediatrics 2009, 123, 578–580. [Google Scholar] [CrossRef]
- Boynton, P.M.; Greenhalgh, T. Selecting, designing, and developing your questionnaire. BMJ 2004, 328, 1312–1315. [Google Scholar] [CrossRef] [Green Version]
- Boynton, P.M. Administering, analysing, and reporting your questionnaire. BMJ 2004, 328, 1372–1375. [Google Scholar] [CrossRef] [Green Version]
- Stone, D.H. Design a questionnaire. BMJ 1993, 307, 1264–1266. [Google Scholar] [CrossRef] [Green Version]
- Kelley, K.; Clark, B.; Brown, V.; Sitzia, J. Good practice in the conduct and reporting of survey research. Int. J. Qual. Health Care 2003, 15, 261–266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rattray, J.; Jones, M.C. Essential elements of questionnaire design and development. J. Clin. Nurs. 2007, 16, 234–243. [Google Scholar] [CrossRef] [PubMed]
- Lava, S.A.; Simonetti, G.D.; Ferrarini, A.; Ramelli, G.P.; Bianchetti, M.G. Regional differences in symptomatic fever management among pediatricians in Switzerland: The results of a cross-sectional Web-based survey. Br. J. Clin. Pharm. 2013, 75, 236–243. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santi, M.; Janner, M.; Simonetti, G.D.; Lava, S.A. Prescription of vitamin D among Swiss pediatricians. Eur. J. Pediatr. 2019, 178, 1119–1123. [Google Scholar] [CrossRef] [PubMed]
- Kusuoka, H.; Hoffman, J.I. Advice on statistical analysis for Circulation Research. Circ. Res. 2002, 91, 662–671. [Google Scholar] [CrossRef] [Green Version]
- Lava, S.A.; Simonetti, G.D.; Ramelli, G.P.; Tschumi, S.; Bianchetti, M.G. Symptomatic management of fever among Swiss board-certified pediatricians: The results of a cross-sectional Web-based survey. Clin. Ther. 2012, 34, 250–256. [Google Scholar] [CrossRef]
- Binkhorst, M.; van der Aar, I.M.; Linders, M.; van Heijst, A.F.J.; de Boode, W.P.; Draaisma, J.M.T.; Hogeveen, M. Training practices in neonatal and paediatric life support: A survey among healthcare professionals working in paediatrics. Resusc. Plus 2021, 5, 100063. [Google Scholar] [CrossRef]
- Temsah, M.H.; Alrabiaah, A.; Al-Eyadhy, A.; Al-Sohime, F.; Al Huzaimi, A.; Alamro, N.; Alhasan, K.; Upadhye, V.; Jamal, A.; Aljamaan, F.; et al. COVID-19 Critical Care Simulations: An International Cross-Sectional Survey. Front. Public Health 2021, 9, 700769. [Google Scholar] [CrossRef]
- Welp, A.; Manser, T. Integrating teamwork, clinician occupational well-being and patient safety-development of a conceptual framework based on a systematic review. BMC Health Serv. Res. 2016, 16, 281. [Google Scholar] [CrossRef] [Green Version]
- Manser, T.; Brösterhaus, M.; Hammer, A. You can’t improve what you don’t measure: Safety climate measures available in the German-speaking countries to support safety culture development in healthcare. Z. Evid. Qual. Gesundhwes. 2016, 114, 58–71. [Google Scholar] [CrossRef]
- Thomas, A.N.; Pilkington, C.E.; Greer, R. Critical incident reporting in UK intensive care units: A postal survey. J. Eval. Clin. Pract. 2003, 9, 59–68. [Google Scholar] [CrossRef]
- Lehmann, R.; Seitz, A.; Meyburg, J.; Hoppe, B.; Hoffmann, G.F.; Tönshoff, B.; Huwendiek, S. Pediatric in-hospital emergencies: Real life experiences, previous training and the need for training among physicians and nurses. BMC Res. Notes 2019, 12, 19. [Google Scholar] [CrossRef] [PubMed]
- Posfay-Barbe, K.M.; Heininger, U.; Aebi, C.; Desgrandchamps, D.; Vaudaux, B.; Siegrist, C.A. How do physicians immunize their own children? Differences among pediatricians and nonpediatricians. Pediatrics 2005, 116, e623–e633. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| All | Nurses | Physicians | p-Value | |
|---|---|---|---|---|
| Department | 469 | 315 | 154 | p < 0.0001 |
| Pediatrics | 288 (61%) | 218 (69%) | 70 (45%) | |
| Pediatric surgery | 82 (18%) | 58 (18%) | 24 (16%) | |
| Pediatric emergency | 43 (9%) | 28 (8.9%) | 15 (9.7%) | |
| Other (e.g., across several departments) | 56 (12%) | 11 (3.5%) | 45 (29%) | |
| Work experience as a healthcare professional | 469 | 315 | 154 | p = 0.0002 |
| <1 year | 3 (0.6%) | 2 (0.6%) | 1 (0.6%) | |
| 1–5 years | 99 (21%) | 58 (18%) | 41 (27%) | |
| 6–10 years | 95 (20%) | 52 (17%) | 43 (28%) | |
| >10 years | 272 (58%) | 203 (64%) | 69 (45%) | |
| Duration of employment at current hospital | 468 | 314 | 154 | p < 0.0001 |
| <1 year | 57 (12%) | 17 (5.4%) | 40 (26%) | |
| 1–5 years | 152 (33%) | 94 (30%) | 58 (38%) | |
| 6–10 years | 72 (15%) | 46 (15%) | 26 (17%) | |
| >10 years | 187 (40%) | 157 (50%) | 30 (19%) | |
| Hours spent working on a weekly basis | 469 | 315 | 154 | p < 0.0001 |
| <20 h/week | 100 (21%) | 70 (22%) | 30 (19%) | |
| 20–40 h/week | 145 (31%) | 123 (39%) | 22 (14%) | |
| >40 h/week | 224 (48%) | 122 (39%) | 102 (66%) | |
| Exposure frequency to life-threatening situations | 459 | 309 | 150 | p = 0.0005 |
| daily | 81 (18%) | 53 (17%) | 28 (19%) | |
| weekly | 79 (17%) | 41 (13%) | 38 (25%) | |
| monthly | 87 (19%) | 53 (17%) | 34 (23%) | |
| once every 2–6 months | 104 (23%) | 77 (25%) | 27 (18%) | |
| yearly | 62 (14%) | 46 (15%) | 16 (11%) | |
| <1 time/year | 46 (10%) | 39 (13%) | 7 (4.7%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ulmer, F.; Pallivathukal, S.; Bartenstein, A.; Bieri, R.; Studer, D.; Lava, S.A.G. Preparedness for Life-Threatening Situations in a Pediatric Tertiary-Care University Children’s Hospital: A Survey. Children 2022, 9, 271. https://doi.org/10.3390/children9020271
Ulmer F, Pallivathukal S, Bartenstein A, Bieri R, Studer D, Lava SAG. Preparedness for Life-Threatening Situations in a Pediatric Tertiary-Care University Children’s Hospital: A Survey. Children. 2022; 9(2):271. https://doi.org/10.3390/children9020271
Chicago/Turabian StyleUlmer, Francis, Sabine Pallivathukal, Andreas Bartenstein, Ruth Bieri, Daniela Studer, and Sebastiano A. G. Lava. 2022. "Preparedness for Life-Threatening Situations in a Pediatric Tertiary-Care University Children’s Hospital: A Survey" Children 9, no. 2: 271. https://doi.org/10.3390/children9020271
APA StyleUlmer, F., Pallivathukal, S., Bartenstein, A., Bieri, R., Studer, D., & Lava, S. A. G. (2022). Preparedness for Life-Threatening Situations in a Pediatric Tertiary-Care University Children’s Hospital: A Survey. Children, 9(2), 271. https://doi.org/10.3390/children9020271






