Stabilisation of Pathologic Proximal Femoral Fracture near the Growth Plate with Use of a Locking Plate and Transphyseal Screws
Abstract
:1. Introduction
2. Materials and Methods
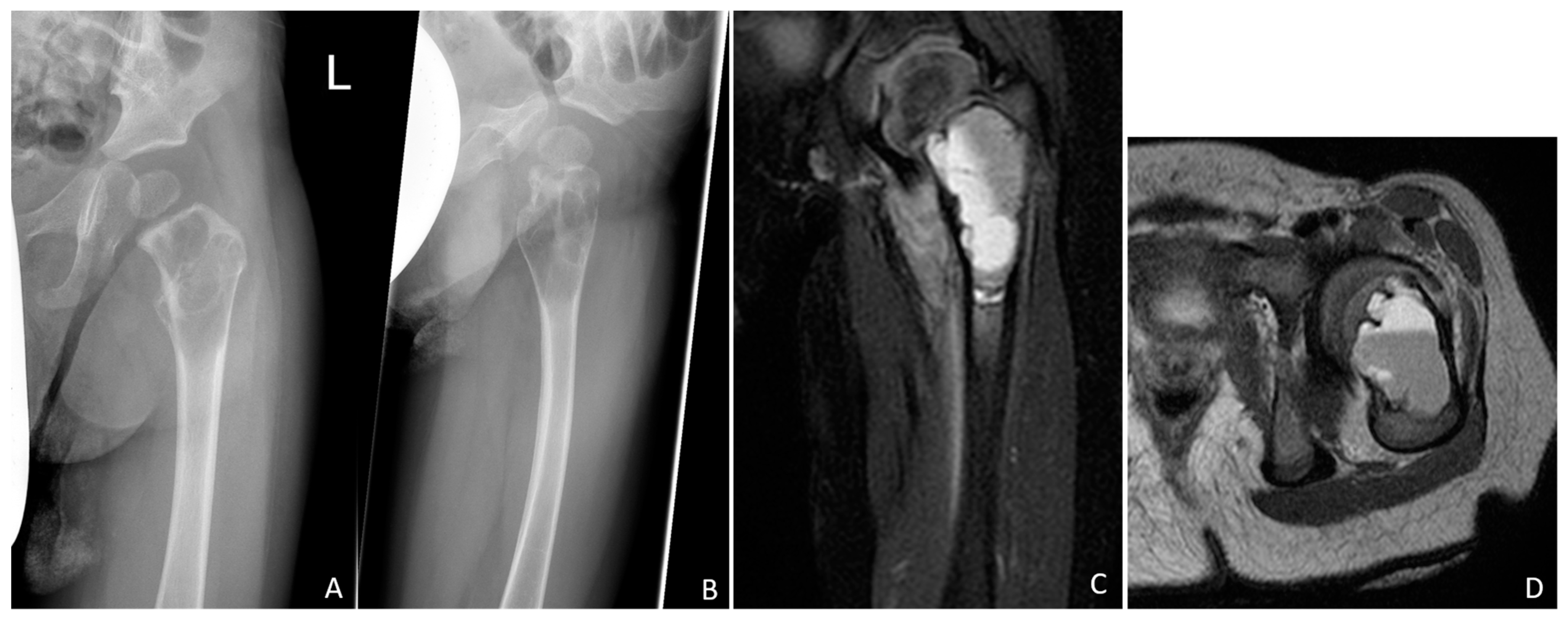
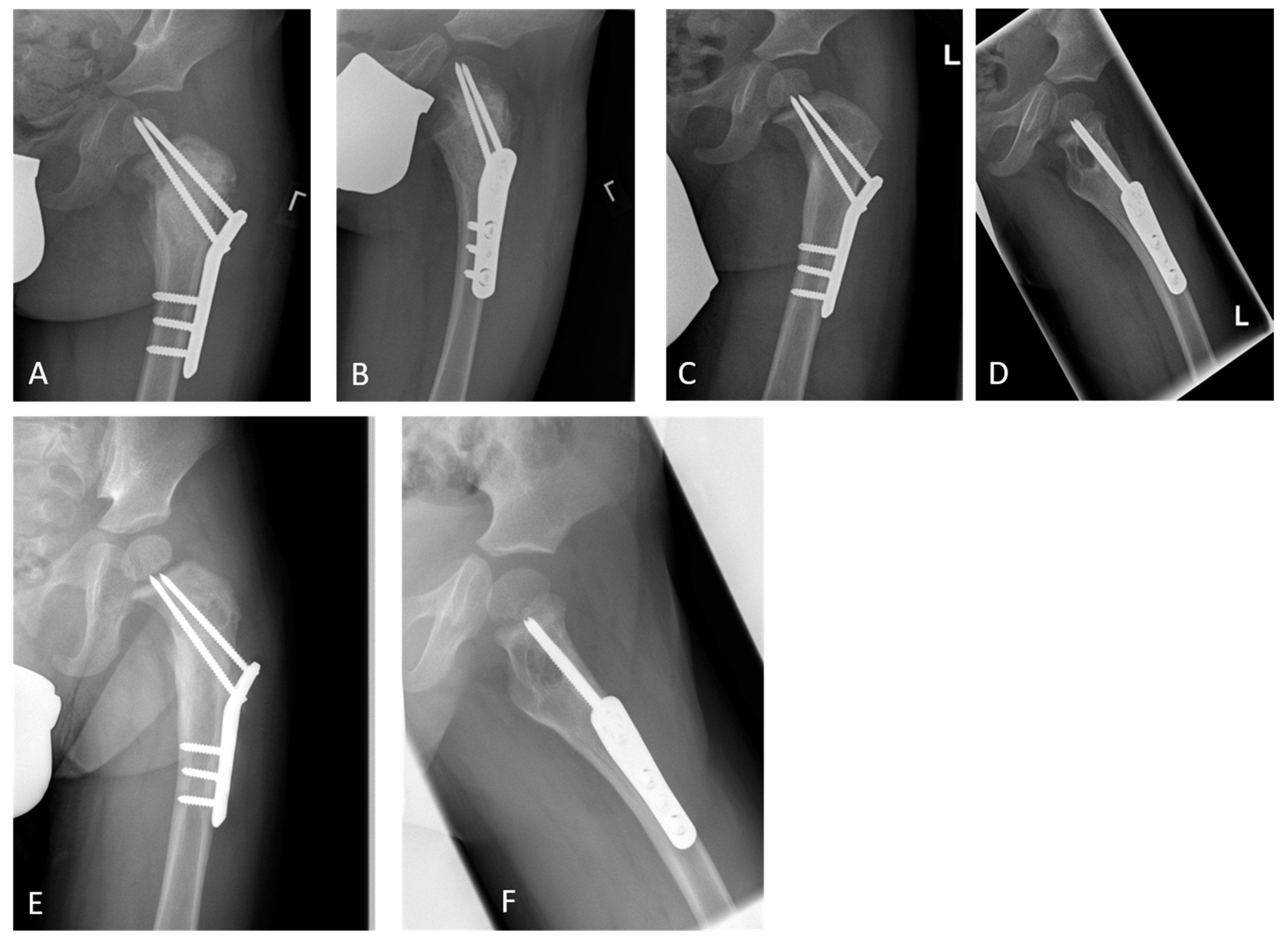
2.1. Case Report
2.2. Conducted Survey
3. Results
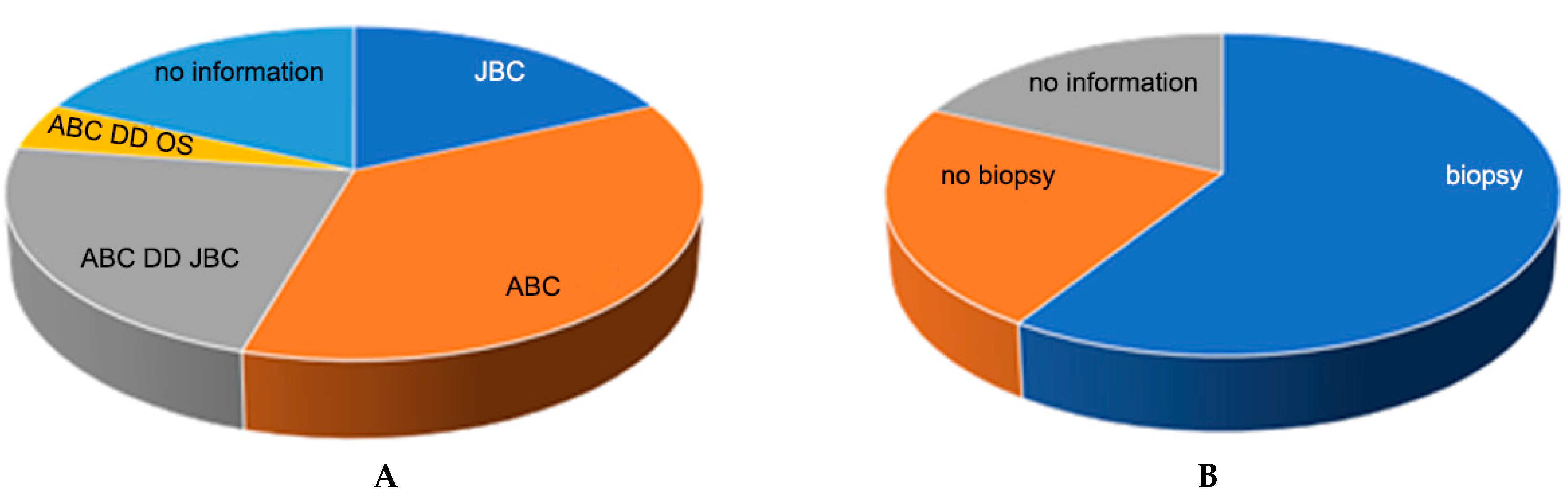
3.1. Survey Results
3.1.1. Entity Assessment
3.1.2. Assessment of the Need for Biopsy
3.1.3. Entity-Specific Local Therapy
3.1.4. Defect Filling
3.1.5. Stabilisation/Osteosynthesis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Freiberg, A.A.; Loder, R.T.; Heidelberger, K.P.; Hensinger, R.N. Aneurysmal bone cysts in young children. J. Pediatr. Orthop. 1994, 14, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Ozaki, T.; Hillmann, A.; Lindner, N.; Winkelmann, W. Aneurysmal bone cysts in children. J. Cancer Res. Clin. Oncol. 1996, 122, 767–769. [Google Scholar] [CrossRef]
- Dorfman, H.; Czerniak, B. Bone Tumors. Mosby: St. Louis, MI, USA, 1998; pp. 855–879. [Google Scholar]
- Campanacci, M.; Bertoni, F.; Bacchini, P. Bone and Soft Tissue Tumors; Springer: Berlin, Germany, 1990; pp. 725–751. [Google Scholar]
- Mankin, H.J.; Hornicek, F.J.; Ortiz-Cruz, E.; Villafuerte, J.; Gebhardt, M.C. Aneurysmal bone cyst: A review of 150 patients. J. Clin. Oncol. 2005, 23, 6756–6762. [Google Scholar] [CrossRef] [Green Version]
- Basarr, K.; Piskin, A.; Güçlü, B.; Yldz, Y.; Sagglk, Y. Aneurysmal bone cyst recurrence in children: A review of 56 patients. J. Pediatr. Orthop. 2007, 27, 938–943. [Google Scholar] [CrossRef]
- Puthoor, D.; Francis, L.; Ismail, R. Is sclerotherapy with polidocanol a better treatment option for aneurysmal bone cyst compared to conventional curettage and bone grafting? J. Orthop. 2021, 25, 265–270. [Google Scholar] [CrossRef]
- Campanacci, M.; Capanna, R.; Picci, P. Unicameral and aneurysmal bone cysts. Clin. Orthop. Relat. Res. 1986, 204, 25–36. [Google Scholar] [CrossRef]
- Dormans, J.P.; Hanna, B.G.; Johnston, D.R.; Khurana, J.S. Surgical treatment and recurrence rate of aneurysmal bone cysts in children. Clin. Orthop. Relat. Res. 2004, 421, 205–211. [Google Scholar] [CrossRef]
- Oliveira, A.M.; Perez-Atayde, A.R.; Inwards, C.Y.; Medeiros, F.; Derr, V.; Hsi, B.L.; Gebhardt, M.C.; Rosenberg, A.E.; Fletcher, J.A. USP6 and CDH11 oncogenes identify the neoplastic cell in primary aneurysmal bone cysts and are absent in so-called secondary aneurysmal bone cysts. Am. J. Pathol. 2004, 165, 1773–1780. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mahnken, A.; Nolte-Ernsting, C.; Wildberger, J.; Heussen, N.; Adam, G.; Wirtz, D.; Piroth, W.; Bücker, A.; Biesterfeld, S.; Haage, P. Aneurysmal bone cyst: Value of MR imaging and conventional radiography. Eur. Radiol. 2003, 13, 1118–1124. [Google Scholar] [CrossRef]
- Miwa, S.; Yamamoto, N.; Hayashi, K.; Takeuchi, A.; Igarashi, K.; Tada, K.; Higuchi, T.; Yonezawa, H.; Morinaga, S.; Araki, Y.; et al. Diagnostic accuracies of intraoperative frozen section and permanent section examinations for histological grades during open biopsy of bone tumors. Int. J. Clin. Oncol. 2021, 26, 613–619. [Google Scholar] [CrossRef]
- Mohaidat, Z.M.; Al-gharaibeh, S.R.; Aljararhih, O.N.; Nusairat, M.T.; Al-omari, A.A. Challenges in the diagnosis and treatment of aneurysmal bone cyst in patients with unusual features. Adv. Orthop. 2019, 2019, 2905671. [Google Scholar] [CrossRef] [Green Version]
- Deventer, N.; Schulze, M.; Gosheger, G.; de Vaal, M.; Deventer, N. Primary aneurysmal bone cyst and its recent treatment options: A comparative review of 74 cases. Cancers 2021, 13, 2362. [Google Scholar] [CrossRef]
- Kaiser, M.M. (Coordinator), S1-Leitlinie AWMF: Knochenzysten 006-029. Available online: https://register.awmf.org/de/leitlinien/detail/006-029 (accessed on 1 December 2022).
- Tomaszewski, R.; Rutz, E.; Mayr, J.; Dajka, J. Surgical treatment of benign lesions and pathologic fractures of the proximal femur in children. Arch. Orthop. Trauma Surg. 2022, 142, 615–624. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Rai, S.; Ze, R.; Tang, X.; Liu, R.; Hong, P. Injectable calcium sulfate vs mixed bone graft of autologous iliac bone and allogeneic bone: Which is the better bone graft material for unicameral bone cyst in humerus? Medicine 2020, 99, e20563. [Google Scholar] [CrossRef] [PubMed]
- Vergel De Dios, A.M.; Bond, J.R.; Shives, T.C.; McLeod, R.A.; Unni, K.K. Aneurysmal bone cyst. A clinicopathologic study of 238 cases. Cancer 1992, 69, 2921–2931. [Google Scholar] [CrossRef] [PubMed]
- van Geloven, T.P.G.; van der Heijden, L.; Laitinen, M.K.; Campanacci, D.A.; Döring, K.; Dammerer, D.; Badr, I.T.; Haara, M.; Beltrami, G.; Kraus, T.; et al. Do’s and don’ts in primary aneurysmal bone cysts of the proximal femur in children and adolescents: Retrospective multicenter EPOS study of 79 patients. J. Pediatr. Orthop. 2022, in press. [CrossRef] [PubMed]
- Bagatur, A.E.; Zorer, G. Complications associated with surgically treated hip fractures in children. J. Pediatr. Orthop. B 2002, 11, 219–228. [Google Scholar] [CrossRef] [PubMed]
- Togrul, E.; Bayram, H.; Gulsen, M.; Kalaci, A.; Ozbarlas, S. Fractures of the femoral neck in children: Long-term follow-up in 62 hip fractures. Injury 2005, 36, 123–130. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Michalik, R.; Hildebrand, F.; Delbrück, H. Stabilisation of Pathologic Proximal Femoral Fracture near the Growth Plate with Use of a Locking Plate and Transphyseal Screws. Children 2022, 9, 1932. https://doi.org/10.3390/children9121932
Michalik R, Hildebrand F, Delbrück H. Stabilisation of Pathologic Proximal Femoral Fracture near the Growth Plate with Use of a Locking Plate and Transphyseal Screws. Children. 2022; 9(12):1932. https://doi.org/10.3390/children9121932
Chicago/Turabian StyleMichalik, Roman, Frank Hildebrand, and Heide Delbrück. 2022. "Stabilisation of Pathologic Proximal Femoral Fracture near the Growth Plate with Use of a Locking Plate and Transphyseal Screws" Children 9, no. 12: 1932. https://doi.org/10.3390/children9121932
APA StyleMichalik, R., Hildebrand, F., & Delbrück, H. (2022). Stabilisation of Pathologic Proximal Femoral Fracture near the Growth Plate with Use of a Locking Plate and Transphyseal Screws. Children, 9(12), 1932. https://doi.org/10.3390/children9121932






