An Artificial Intelligence Approach to Support Detection of Neonatal Adverse Drug Reactions Based on Severity and Probability Scores: A New Risk Score as Web-Tool
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Data Acquisition
2.3. Causal Probability, Severity, and an ADR Risk Matrix
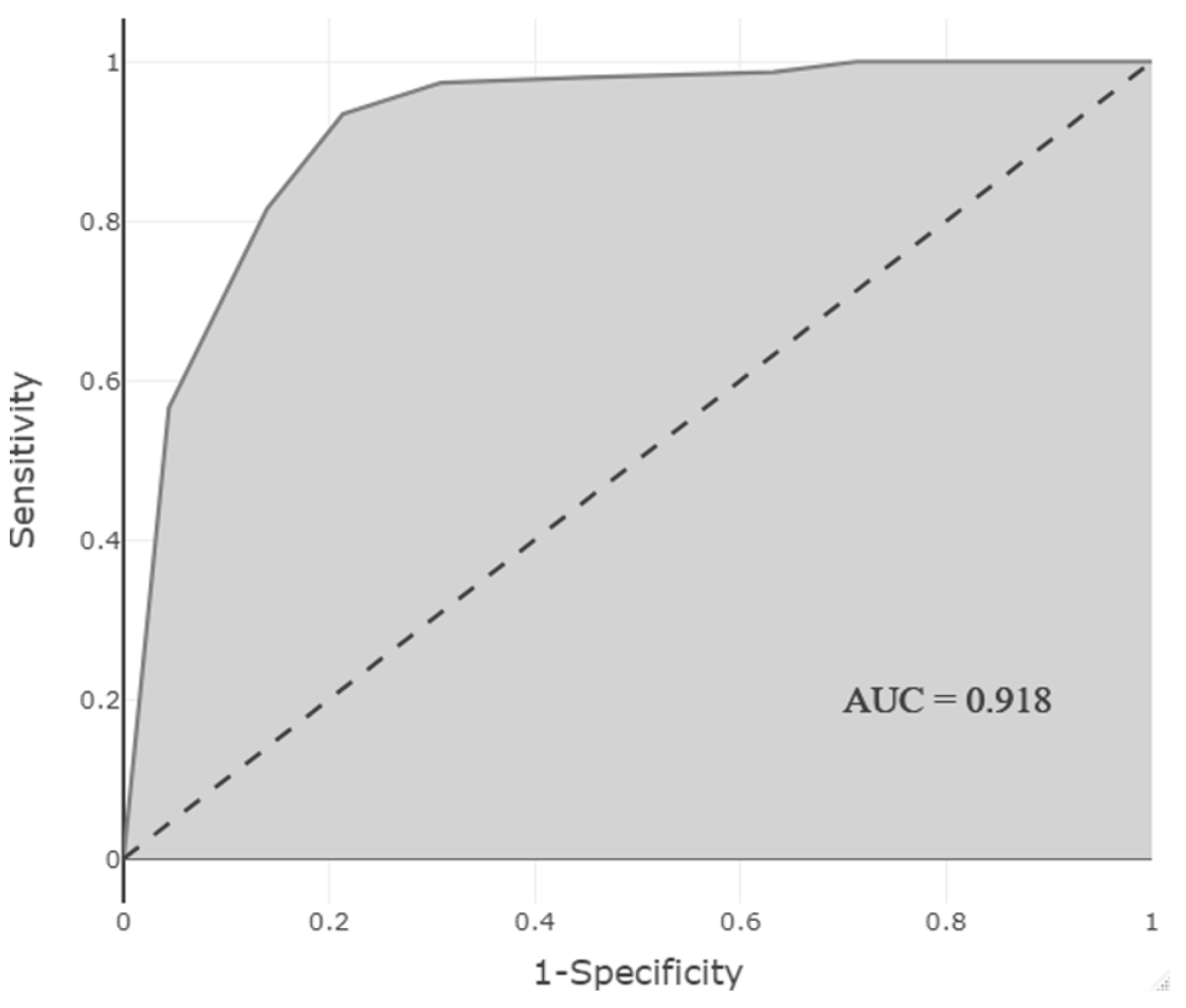
2.4. Random Forest Model Development, Optimization, and Validation
3. Results
3.1. Clinical Characteristics
3.2. Characteristics of Suspected ADRs: Probability and Severity Scores
3.3. Development and Optimization of a Model to Predict the Presence of ADRs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kaushal, R.; Bates, D.W.; Landrigan, C.; McKenna, K.J.; Clapp, M.D.; Federico, F.; Goldmann, D.A. Medication errors and adverse drug events in pediatric inpatients. JAMA 2001, 285, 2114–2120. [Google Scholar] [CrossRef] [PubMed]
- Sugioka, M.; Tachi, T.; Mizui, T.; Koyama, A.; Murayama, A.; Katsuno, H.; Matsuyama, T.; Aoyama, S.; Osawa, T.; Noguchi, Y.; et al. Effects of the number of drugs used on the prevalence of adverse drug reactions in children. Sci. Rep. 2020, 10, 21341. [Google Scholar] [CrossRef] [PubMed]
- Le, J.; Nguyen, T.; Law, A.V.; Hodding, J. Adverse drug reactions among children over a 10-year period. Pediatrics 2006, 118, 555–562. [Google Scholar] [CrossRef] [PubMed]
- Fabretti, S.C.; Brassica, S.C.; Cianciarullo, M.A.; Romano-Lieber, N.S. Triggers for active surveillance of adverse drug events in newborns. Cad. Saude Publica 2018, 34, e00069817. [Google Scholar] [CrossRef] [PubMed]
- Coppini, R.; Simons, S.H.P.; Mugelli, A.; Allegaert, K. Clinical research in neonates and infants: Challenges and perspectives. Pharmacol. Res. 2016, 108, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Sridharan, K.; Al Jufairi, M.; Al Ansari, E. Off-label drug use and the risk of medication errors in critically ill neonates: A conceptual pilot study. Int. J. Risk Saf. Med. 2021, 32, 279–293. [Google Scholar] [CrossRef] [PubMed]
- Du, W.; Lehr, V.T.; Lieh-Lai, M.; Koo, W.; Ward, R.M.; Rieder, M.J.; Van Den Anker, J.N.; Reeves, J.H.; Mathew, M.; Lulic-Botica, M.; et al. An algorithm to detect adverse drug reactions in the neonatal intensive care unit. J. Clin. Pharmacol. 2013, 53, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Salaets, T.; Turner, M.A.; Short, M.; Ward, R.M.; Hokuto, I.; Ariagno, R.L.; Klein, A.; Beauman, S.; Wade, K.; Thomson, M.; et al. Development of a neonatal adverse event severity scale through a Delphi consensus approach. Arch. Dis. Child. 2019, 104, 1167–1173. [Google Scholar] [CrossRef] [PubMed]
- Naranjo, C.A.; Busto, U.; Sellers, E.M.; Sandor, P.; Ruiz, I.; Roberts, E.A.; Janecek, E.; Domecq, C.; Greenblatt, D.J. A method for estimating the probability of adverse drug reactions. Clin. Pharmacol. Ther. 1981, 30, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Allegaert, K.; van den Anker, J.N. Adverse drug reactions in neonates and infants: A population-tailored approach is needed. Br. J. Clin. Pharmacol. 2015, 80, 788–795. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, M. Variable Selection Using the Caret Package. 2012. Available online: http://cran.cermin.lipi.go.id/web/packages/caret/vignettes/caretSelection.pdf (accessed on 16 October 2022).
- Harrell, F.E., Jr.; rms: Regression Modeling Strategies. R Package Version 6.2-0. 2021. Available online: https://CRAN.R-project.org/package=rms (accessed on 10 October 2022).
- Goksuluk, D.; Korkmaz, S.; Zararsiz, G.; Karaagaoglu, A.E. easyROC: An interactive web-tool for roc curve analysis using r language environment. R J. 2016, 8, 213–230. [Google Scholar] [CrossRef]
- De Basagoiti, A.; Fernandez, A.; Mendiola, S.; De Miguel, M.; Guerra, E.; Loureiro, B.; Campino, A. Intravenous drug use in neonatal intensive care units. Eur. J. Hosp. Pharm. 2021, 28, 341–345. [Google Scholar] [CrossRef] [PubMed]
- Hornik, C.P.; Herring, A.H.; Benjamin, D.K., Jr.; Capparelli, E.V.; Kearns, G.L.; van den Anker, J.; Cohen-Wolkowiez, M.; Clark, R.H.; Smith, P.B.; Best Pharmaceuticals for Children Act-Pediatric Trials, N. Adverse events associated with meropenem versus imipenem/cilastatin therapy in a large retrospective cohort of hospitalized infants. Pediatr. Infect. Dis. J. 2013, 32, 748–753. [Google Scholar] [CrossRef] [PubMed]
- Alghamdi, A.A.; Keers, R.N.; Sutherland, A.; Ashcroft, D.M. Prevalence and Nature of Medication Errors and Preventable Adverse Drug Events in Paediatric and Neonatal Intensive Care Settings: A Systematic Review. Drug Saf. 2019, 42, 1423–1436. [Google Scholar] [CrossRef] [PubMed]
- Rhone, E.T.; Carmody, J.B.; Swanson, J.R.; Charlton, J.R. Nephrotoxic medication exposure in very low birth weight infants. J. Matern. Fetal. Neonatal. Med. 2014, 27, 1485–1490. [Google Scholar] [CrossRef] [PubMed]
- Rohr, S.B.; Sauer, H.; Gottschling, S.; Abdul-Khaliq, H.; Gortner, L.; Nunold, H.; Graber, S.; Meyer, S. Non-neurological, steroid-related adverse events in very low birth weight infants: A prospective audit. Swiss Med. Wkly. 2014, 144, w13954. [Google Scholar] [CrossRef] [PubMed]
- Malowany, J.I.; Knoppert, D.C.; Chan, A.K.; Pepelassis, D.; Lee, D.S. Enoxaparin use in the neonatal intensive care unit: Experience over 8 years. Pharmacotherapy 2007, 27, 1263–1271. [Google Scholar] [CrossRef] [PubMed]
- IBM Micromedex. Enoxaparin: Monitoring. 2021. Available online: http://www.micromedexsolutions.com/ (accessed on 18 December 2021).
- McMaster, C.; Liew, D.; Keith, C.; Aminian, P.; Frauman, A. A Machine-Learning Algorithm to Optimise Automated Adverse Drug Reaction Detection from Clinical Coding. Drug Saf. 2019, 42, 721–725. [Google Scholar] [CrossRef] [PubMed]
- Syrowatka, A.; Song, W.; Amato, M.G.; Foer, D.; Edrees, H.; Co, Z.; Kuznetsova, M.; Dulgarian, S.; Seger, D.L.; Simona, A.; et al. Key use cases for artificial intelligence to reduce the frequency of adverse drug events: A scoping review. Lancet Digit. Health 2022, 4, e137–e148. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Jung, K.; Winnenburg, R.; Shah, N.H. A method for systematic discovery of adverse drug events from clinical notes. J. Am. Med. Inform. Assoc. 2015, 22, 1196–1204. [Google Scholar] [CrossRef] [PubMed]
| Drugs | Number of ADRs (Incidence %) | Route | Onset Day (Mean) | Type of ADRs | Probability Median (Min–Max) | Severity Median (Min–Max) | Risk Score Median (Min–Max) | Risk Category Median (Min–Max) |
|---|---|---|---|---|---|---|---|---|
| Meropenem | 18 (16.07) | IV | 4.38 | Thrombocytopenia (12) Eosinophilia (4) Thrombocytosis (1) AST increase (1) | 2 (1–4) | 2 (1–3) | 4 (2–8) | 1 (1–2) |
| Dexamethasone | 16 (57.14) | IV | 2.68 | Hyperglycemia (13) Hypertension (2) AST, Cr, BUN increase (1) | 4 (1–4) | 2 (1–4) | 8 (2–12) | 2 (1–3) |
| Vancomycin | 15 (13.04) | IV | 7.46 | Neutropenia (11) Cr increase (4) | 3 (1–4) | 2 (1–4) | 6 (1–12) | 2 (1–3) |
| Furosemide | 10 (38.46) | IV | 2.62 | Hypochloremia (6) Hypomagnesemia (1) Hyponatremia (1) Hypokalemia (1) Alkalosis (1) | 4 (3–4) | 2 (1–3) | 8 (4–12) | 2 (1–3) |
| PN | 10 (6.32) | IV | 15.50 | Cholestasis (4) Hyperglycemia (2) TPNoma (1) Thrombus (1) Hyperkalemia (1) Hypernatremia (1) | 3 (2–4) | 2 (1–4) | 8 (2–16) | 2 (1–3) |
| Alprostadil | 9 (47.36) | IV | 5.22 | Pyloric stenosis (8) Hypotension (1) | 2 (2–3) | 3 (2–3) | 6 (6–9) | 2 (2–2) |
| Hydrocortisone | 7 (46.66) | IV | 2.57 | Hyperglycemia (7) | 3 (2–4) | 2 (2–3) | 6 (4–12) | 2 (1–3) |
| Hydrochlorothiazide | 5 (45.45) | Oral | 6.60 | Hypochloremia (2) Hyponatremia (1) Hypokalemia (1) Hyperglycemia (1) | 3 (3–3) | 2 (1–2) | 6 (3–6) | 2 (1–2) |
| Ibuprofen | 5 (55.55) | Oral | 2.80 | Thrombocytopenia (5) | 3 (2–4) | 2 (2–3) | 6 (6–8) | 2 (2–2) |
| Allopurinol | 4 (36.36) | Oral | 3.00 | Hypouricemia (2) INR increase (1) BUN increase (1) | 3 (2–4) | 1 (1–3) | 3 (2–12) | 1 (1–3) |
| Amikacin | 4 (3.36) | IV | 13.00 | Cr increase (3) ALP increase (1) | 3 (2–4) | 2 (2–3) | 6 (4–12) | 2 (1–3) |
| Amiodarone | 4 (100) | IV | 8.50 | TSH increase (2) Hemolytic anemia (1) Eosinophilia (1) | 3 (3–4) | 2 (1–3) | 6 (3–9) | 2 (1–2) |
| Fentanyl | 4 (8.69) | IV | 3.66 | Tachycardia (2) Hypoactivity (1) Hypotension (1) | 3 (2–4) | 2 (1–3) | 4 (3–12) | 1 (1–3) |
| Propranolol | 4 (44.44) | Oral | 5.00 | Hypoglycemia (3) Bradycardia (1) | 2 (2–4) | 2 (1–2) | 4 (2–8) | 1 (1–2) |
| Ciprofloxacin | 4 (33.33) | IV | 15.00 | AST increase (3) Hyperalgesia (1) | 2 (2–4) | 2 (2–2) | 4 (4–8) | 1 (1–2) |
| Biotin | 3 (100) | Oral | 4.00 | Pseudohyperthyroidism (2) Vomiting (1) | 4 (4–4) | 1 (1–2) | 4 (4–8) | 1 (1–2) |
| Enoxaparin | 3 (25.00) | SC | 17.00 | Thrombocytopenia (2) Microvascular hemorrhage (1) | 4 (4–4) | 3 (2–3) | 12 (8–12) | 3 (2–3) |
| Fluconazole | 3 (2.70) | IV | 7.00 | AST increase (3) | 2 (2–3) | 2 (2–2) | 4 (4–6) | 1 (1–2) |
| Methylprednisolone | 3 (75.00) | IV | 1.66 | Hyperglycemia (3) | 1 (1–2) | 1 (1–2) | 1 (1–4) | 1 (1–1) |
| Midazolam | 3 (10.00) | IV | 5.00 | AST increase (1) Hypotension (1) Methemoglobinemia (1) | 2 (2–4) | 2 (1–2) | 4 (2–8) | 1 (1–2) |
| Morphine | 3 (33.33) | IV | 2.00 | Seizure (1) Hypotension (1) Globe vesicle (1) | 3 (2–4) | 2 (2–3) | 6 (6–8) | 2 (2–2) |
| Octreotide | 3 (100) | IV | 8.33 | Hyperglycemia (3) | 3 (2–4) | 2 (1–2) | 6 (2–8) | 2 (1–2) |
| Dexmedetomidine | 2 (3.38) | IV | 4.00 | Hypotension (1) Seizure threshold descrease (1) | 4 (4–4) | 3 (3–3) | 12 (12–12) | 3 (3–3) |
| Phenobarbital | 2 (9.09) | Oral | 10.50 | GGT increase (1) ALT increase (1) | 3 (3–3) | 2 (2–2) | 6 (2–2) | 2 (2–2) |
| Levetiracetam | 2 (20.00) | Oral | 10.00 | Ocular deviation (1) GGT increase (1) | 3 | 3 | 9 | 2 |
| Milrinone | 2 (13.33) | IV | 13.50 | Hypotension (2) | 4 | 2 | 8 | 2 |
| Vinblastine | 2 (100) | IV | 3.00 | Leukopenia (1) Erythrocyte reduction (1) | 4 | 3 | 12 | 3 |
| Vitamin A | 2 (8.69) | Oral | 12.50 | Thrombocytosis (1) | 4 | 2 | 8 | 2 |
| Diazoxide | 1 (12.50) | Oral | 7 | Hyperbilirubinemia (1) | 3 | 3 | 9 | 2 |
| Dornaz alpha | 1 (20.00) | İnhaler | 4 | Thrombocytopenia (1) | 4 | 4 | 16 | 3 |
| Etoposide/Carboplatin | 1 (100) | IV | 3 | Airway obstruction (1) | 4 | 4 | 16 | 3 |
| Phenytoin | 1 (25.00) | IV | 2 | Neutropenia (1) | 3 | 1 | 3 | 1 |
| Flecainide | 1 (50.00) | Oral | 1 | AST increase (1) | 3 | 3 | 9 | 2 |
| Gentamicin | 1 (0.54) | IV | 3 | Tachycardia (1) | 2 | 2 | 4 | 1 |
| Captopril | 1 (14.28) | Oral | 25 | Cr increase (1) | 3 | 2 | 6 | 2 |
| Levosimendan | 1 (33.33) | IV | 2 | Hypotension (1) | 4 | 2 | 8 | 2 |
| Maflor | 1 (3.33) | Oral | 8 | Hypotension (1) | 3 | 2 | 6 | 2 |
| Metronidazole | 1 (7.69) | IV | 4 | ALP increase (1) | 2 | 2 | 4 | 1 |
| Paracetamol | 1 (25.00) | IV | 1 | AST increase (1) | 3 | 1 | 3 | 1 |
| Prednisolone | 1 (100) | Oral | 5 | AST increase (1) | 3 | 4 | 12 | 3 |
| Salbutamol | 1 (3.84) | İnhaler | 8 | INR increase (1) | 3 | 2 | 6 | 2 |
| Ampicillin + Sulbactam | 1 (25.00) | IV | 17 | Hypokalemia (1) | 3 | 2 | 6 | 2 |
| Ceftriaxone | 1 (100) | IV | 2 | ALP increase (1) | 2 | 2 | 4 | 1 |
| Sholl Solution | 1 (50.00) | Oral | 12 | Hyperbilirubinemia (1) | 4 | 2 | 8 | 2 |
| Sotalol | 1 (100) | Oral | 5 | Vomiting (1) | 4 | 2 | 8 | 2 |
| Spirinolactone | 1 (16.66) | Oral | 30 | Hypoglycemia (1) | 3 | 2 | 6 | 2 |
| Terlipressin | 1 (33.33) | IV | 4 | Gynecomastia (1) | 4 | 2 | 8 | 2 |
| Total Fluid | 1 (0.36) | IV | 1 | Hyponatremia (1) | 3 | 1 | 3 | 1 |
| Ursodiol | 1 (50.00) | Oral | 8 | Hyperglycemia (1) | 2 | 2 | 4 | 1 |
| SEVERITY | ||||||
|---|---|---|---|---|---|---|
| Mild (1) n = 28 (14.97%) | Moderate (2) n = 102 (54.55%) | Severe (3) n = 47 (25.13%) | Life Threatening (4) n = 10 (5.35%) | Death (5) - | ||
| PROBABILITY | Definite (4) n = 62 (33.16%) | 4 | 8 | 12 | 16 | 20 |
| Probable (3) n = 68 (36.37%) | 3 | 6 | 9 | 12 | 15 | |
| Possible (2) n = 52 (27.80%) | 2 | 4 | 6 | 8 | 10 | |
| Unlikely (1) n = 5 (2.67%) | 1 | 2 | 3 | 4 | 5 | |
| Variables | β | SE(β) | p * | OR | 95% CI for OR | Risk Score |
|---|---|---|---|---|---|---|
| Endocrine system drugs | 2.443 | 0.522 | <0.001 | 11.508 | 4.134–32.039 | 2 points |
| Cardiovascular system drugs | 2.702 | 0.501 | <0.001 | 14.902 | 5.583–39.774 | 3 points |
| Diseases of the circulatory system | 1.354 | 0.596 | 0.023 | 3.872 | 1.203–12.460 | 1 point |
| Nervous system drugs | 1.026 | 0.394 | 0.009 | 2.790 | 1.288–6.042 | 1 point |
| Parenteral nutrition treatment | 1.344 | 0.402 | 0.001 | 3.835 | 1.745–8.431 | 1 point |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yalçın, N.; Kaşıkcı, M.; Çelik, H.T.; Allegaert, K.; Demirkan, K.; Yiğit, Ş.; Yurdakök, M. An Artificial Intelligence Approach to Support Detection of Neonatal Adverse Drug Reactions Based on Severity and Probability Scores: A New Risk Score as Web-Tool. Children 2022, 9, 1826. https://doi.org/10.3390/children9121826
Yalçın N, Kaşıkcı M, Çelik HT, Allegaert K, Demirkan K, Yiğit Ş, Yurdakök M. An Artificial Intelligence Approach to Support Detection of Neonatal Adverse Drug Reactions Based on Severity and Probability Scores: A New Risk Score as Web-Tool. Children. 2022; 9(12):1826. https://doi.org/10.3390/children9121826
Chicago/Turabian StyleYalçın, Nadir, Merve Kaşıkcı, Hasan Tolga Çelik, Karel Allegaert, Kutay Demirkan, Şule Yiğit, and Murat Yurdakök. 2022. "An Artificial Intelligence Approach to Support Detection of Neonatal Adverse Drug Reactions Based on Severity and Probability Scores: A New Risk Score as Web-Tool" Children 9, no. 12: 1826. https://doi.org/10.3390/children9121826
APA StyleYalçın, N., Kaşıkcı, M., Çelik, H. T., Allegaert, K., Demirkan, K., Yiğit, Ş., & Yurdakök, M. (2022). An Artificial Intelligence Approach to Support Detection of Neonatal Adverse Drug Reactions Based on Severity and Probability Scores: A New Risk Score as Web-Tool. Children, 9(12), 1826. https://doi.org/10.3390/children9121826







