1. Introduction
Selective mutism (SM) is a rare anxiety disorder characterized by the consistent inability to speak in settings where the expectation is to initiate speech or engage in reciprocal communication [
1]. The prevalence of SM is estimated to be less than 2%, with an onset age of before five. Children with SM may speak comfortably in certain situations, particularly at home, and persistently fail to speak in other social settings (e.g., school, community).
SM is classified in the Diagnostic and Statistical Manual for Mental Disorders as an anxiety disorder, which aligns with scholars’ consensus of close etiology links between SM and social anxiety disorder (SAD), specifically [
1]. Beyond etiology, behavior inhibition to escape stress inducing situations is a common coping strategy for individuals with anxiety [
2]. As with other anxiety disorders, SM often leads to dysfunction in a child’s life and warrants treatment [
3]. Children with SM engage in a pattern of avoidance to decrease feelings of anxiety in environments where speech is expected [
4]. The maladaptive cycle starts with a prompt for response, feelings of anxiety, avoidance of speech (e.g., parent speaks for child), and then decreased anxiety. Escaping aversive physiological and psychological effects of anxiety by withholding speech negatively reinforces the behavior and thus, the child is likely to avoid speaking in the future. Furthermore, parents/caregivers are reinforced for rescuing behaviors, and are therefore more likely to rescue via speaking for the child in the future. Lack of speech can result in social isolation and academic and social dysfunction, which means the behavioral avoidance cycle needs to be disrupted through exposure-based treatment.
Given the conceptualization that withholding speech fulfills a behavioral function for children with SM, behavioral therapy is a commonly recommended treatment for the disorder [
5]. Typical behavioral therapy for children with SM includes contingency management and shaping strategies, which include direct instruction and positive reinforcement for target behaviors. Stimulus fading, role-playing, and hierarchal exposure are common supplements to typical therapy as it builds on the child’s success with exposure to speaking in an increasing number of environments. The goal of behavioral treatment is for the child to experience decreased symptoms of SM (i.e., speech in several environments) as they increase skills and confidence with progressively more difficult exposure tasks.
In a recent analysis of peer-reviewed journal articles about SM treatment between 2005 and 2015, behavioral therapy appeared to be the most popular and effective therapy for SM [
6]. Behavioral therapy, in conjunction with another therapy (e.g., psychodynamic, systems), was implemented in 21 out of 23 articles reviewed and was the exclusive therapy used in seven of those articles. Six out of seven studies included only one or two participants. In the additional study, three participants were not included in the total sample size (
n = 9) because they dropped out after three sessions [
7]. Participants from the seven studies were between three and 13 years old and included 12 females and five males who were European American, African American, Asian American, Hispanic/Latina, and biracial. Therapy was implemented in a variety of settings, including school, clinic, and the community. All seven studies found improvements in SM symptoms, including increased responses, initiations of speech, verbalizations, and improved teacher and parent rating scale scores following a range of one to seven months of behavioral therapy.
While behavioral therapy appears to be a common and effective intervention for children with SM, there are limitations to its implementation in a traditional therapy format. Accessibility is a limitation to traditional behavioral therapy. Experts in treating SM are scarce, due in part to the rarity of the disorder [
4]. Second, families may encounter barriers seeking treatment due to costly 11 to 18 weekly sessions [
8]. Weekly treatment can cost between
$100–
$200 per hour, not including weekly travel costs (e.g., gas, bus, train, tolls). Third, scheduling challenges over the traditional therapy duration of three to six months may result in lost momentum with treatment effects. Fourth, even if a family can access treatment, the expectation of school personnel to implement the clinician-designed intervention may imply gaps in competency and execution of intervention plan [
7].
Disruptive innovations may circumvent these barriers (i.e., access, cost, scheduling, implementation competency) through novel forms of delivery of evidence- based interventions (EBIs) [
9]. Disruptive innovations synthesize common, robust EBI elements and aim to serve more people for lesser cost by meeting “the essential needs of the majority of consumers in more efficient and accessible ways” [
9], p. 467. As a disruptive innovation, brief interventions are a novel delivery format to reach more people through efficient treatment which includes less sessions than traditional therapy. The time and financial commitments associated with brief interventions may help to overcome scheduling and cost limitations associated with traditional behavioral therapy. Brief interventions as a screener to help guide individualized treatment aligns with previous treatment recommendations given the heterogeneity of symptoms and resulting dysfunction appearing across settings seen in children diagnosed with SM [
10].
Brief, Intensive, and Concentrated (BIC) interventions are an adaptation of brief interventions described above, as they share a foundational rationale to address the limitations of traditional therapy through short-term intervention but often have more than one or two sessions. A recent meta-analysis defined “brief” as interventions with notably less sessions than traditional therapy, “concentrated” as interventions with more than one session per week in short time period, and “intensive” as interventions that were both brief and concentrated [
11]. This meta-analysis provides initial support for BIC cognitive behavioral treatments (CBT) for anxiety disorders in children. A total of 23 randomized clinical controlled trials (RCTs) were reviewed, including 13 studies about specific phobias, three studies about obsessive- compulsive disorder (OCD), three studies about posttraumatic stress disorder (PTSD), and one study each about panic disorder, separation anxiety disorder, SAD, and mixed anxiety disorder. The format of therapy was individual for 20 studies and group for three studies. Results suggest strong acceptability of BICs, as evidenced by the 6% decline rate for family participation in the RCTs and 2% dropout rate once intervention had begun. Intervention integrity was not reported in this meta-analysis. Results showed a very large effect size (g = 1.47) when BICs were compared to waitlist controls, a large effect size (g = 0.97) when BICs were compared to placebo conditions, and no difference (g = 0.01) when BICs were compared to traditional (i.e., once per week for 11 to 18 weeks) CBT. This meta-analysis provides promising results to suggest BIC interventions have the same results of traditional CBT, while addressing its barriers, especially those related to access. Given the clarity and comprehensiveness of the definition of “intensive” intervention to include “brief” and “concentrated” approaches [
11], this current study’s intervention approach is referred to as “intensive” hereafter.
While there is well-developed evidence to support the implementation of RCTs for intensive interventions for anxiety disorders such as specific phobias, there is less information available about intensive interventions for SM and closely related disorders (e.g., SAD). Specifically, the seven behavioral therapy-exclusive articles included the SM intervention meta-analysis [
6] would not fit the criteria of BICs because treatment duration extended one to four months. Literature about SM treatment approaches are dominated by case studies [
6] and lacks exploration of intensive interventions as a treatment approach to SM or closely related disorders (e.g., SAD). Feasibility studies are warranted when “there are few previously published studies or existing data using a specific intervention technique” [
12], p. 453. Acceptability, implementation (i.e., integrity), and limited-efficacy testing (i.e., effectiveness) are essential areas of study when investigating BIC interventions for anxiety disorders [
12]. Acceptability is defined as satisfaction or the extent to which the intervention is suitable and satisfying to the consumer. Implementation is defined as integrity or the extent to which the intervention was executed as planned. Limited efficacy is defined as the exploration of whether the intended effects of the intervention occurred and the consideration of intervention effectiveness in a future study with more controlled conditions (e.g., RCT).
Acceptability, integrity, and effectiveness are fundamentally linked [
12]. An original factor analysis of the Treatment Evaluation Inventory TEI [
13] revealed acceptability and effectiveness load on the same factor for the TEI, which measures parent intervention acceptability. Meanwhile, previous literature shows a positive correlation link between acceptability and integrity, which suggests consumers are more likely to implement intervention with integrity when they consider it highly acceptable [
14]. The distinct connection between these variables make it essential to measure all three when assessing an intervention, like BIC.
Treatment acceptability is infrequently reported in the literature exploring intensive intervention approaches for individuals with anxiety disorders. Three studies of varying sample sizes (
n = 3,
n = 23,
n = 40), participant ages (7–18) and anxiety disorders (social phobia, SAD, OCD) are compared. One study included 40 children (ages 7–12) with social phobia, divided into treatment and control waitlist groups [
8]. Treatment participants received four 3-h sessions, including psychoeducation content and behavioral exposures, over the span of three weekends (15 days) in groups of four to six children. It was mentioned anecdotally that the intervention was highly acceptable to parents and children, as well as revealed through an average score of 3.83 (higher than “quite a bit satisfied”) on an eight-item 5-point Likert scale for acceptability. A second study involved three adolescents (ages 13–18) who received ten 1-h CBT sessions with the therapist and their parent over five days [
15]. All three participants agreed the treatment was rigorous but useful. Though parent and child anecdotes of acceptability are promising, information from more reliable measures is needed to understand which components of intensive intervention lend to its acceptability. The third study included 23 children (ages 8–11) with social phobia randomly divided into a treatment and waitlist control group [
16]. Treatment participants received three 3-h sessions, including psychoeducation content and behavioral exposures, over the span of three weeks in groups of five to seven children. No mention of treatment acceptability was made.
The integrity of intensive intervention implementation is also infrequently and not well documented in the literature when it is used as a novel delivery format for anxiety disorders. Two of the three studies previously reviewed [
5,
8]. The third study included videotapes of all sessions used to determine the adherence to the treatment protocol and noted adherence was reviewed and addressed after the first session to improve integrity [
16]. However, their review of treatment adherence was vague, and rate of adherence was not reported.
The outcomes of these studies provide initial support for intensive interventions as effective interventions for anxiety disorders like SM. For example, it was found that by posttreatment, 52.4% of treatment participants did not meet diagnostic criteria for social phobia, compared to 15.8% of controls [
8]. By 6-month follow-up, 76.9% of treatment participants did not meet diagnostic criteria for social phobia. At posttreatment and 6-month follow-up, treatment participants reported a greater improvement in anxiety symptoms, internalizing problems, depression, social skills, social competence, and parental social anxiety symptoms than control participants. In a different study, OCD symptoms decreased and functioning increased for all three participants, while two participants experienced a 40% decrease in symptoms [
15]. The additional study found that at posttreatment, diagnostic interviews, parent reports, and child reports indicated treatment group participants showed significantly improved social phobia related symptoms compared to controls [
16].
A ten-step intervention research trajectory for the development and testing of intervention approaches has been proposed [
17]. In this progress model, after identification of an issue (i.e., SM diagnosis) and strategies (i.e., behavioral therapy through intensive intervention) to address the issue, strategies should be tested for feasibility via a pilot study. The testing of behavioral therapy as an intervention for SM has been well documented in the SM literature with positive outcomes [
5,
6,
18]. However, none of the SM treatment studies examined the use of behavioral intervention in an intensive format. Thus, according to the research trajectory [
17], it is appropriate to implement a pilot study to assess the feasibility of an intensive intervention for children with SM. Specifically, piloting an intensive intervention in non-traditional settings like summer camps create “the potential for an intensive therapeutic experience, coupled with the innovation of a camp setting that includes fun, reinforcing activities…fit well within a day camp, short-term treatment model” [
19], p. 360.
One feasibility study to explore intensive summer camp intervention for children with separation anxiety disorder has been conducted [
20]. Specifically, the feasibility of intensive CBT for five girls (ages 8–11) with separation anxiety disorder during a seven-day summer camp was investigated. A case-series design including baseline, pretreatment, posttreatment, and three-month follow-up assessment measures indicated high rates of parental acceptability; parents were “very satisfied” with their daughters’ progress. Intervention integrity was not reported for this study. All participants experienced significant decreases in separation anxiety disorder symptoms at posttreatment, and none of the participants met diagnostic criteria at three-month follow-up.
Current Study
The present study aimed to parallel the prior separation anxiety disorder study [
20] by piloting an intensive summer day camp intervention for children with SM, called Confident Kids Camp (CKC). The current study utilized a non-randomized replicated AB single-case design to examine the acceptability, integrity, and effectiveness of intensive intervention implemented in a 5-consecutive day summer camp for 25 children with SM. It extends prior research on SM and it builds in additional methodological rigor by doing (a) family interviews to explore the acceptability of time, resources, and accessibility of this 5-day camp, (b) integrity checklists and integrity observations, (c) daily tracking of child-level anxiety levels and speaking behaviors including video recording, and (d) replication across participants. These study components increased the rigor of the prior intensive intervention studies previously described.
4. Discussion
4.1. Study Contributions to the Literature
The current study contributes to current literature by investigating the acceptability, integrity, and effectiveness of a 5-consecutive day intensive summer day camp for children with SM (i.e., CKC) through a replicated single-case AB design. This study extends on prior research about SM by exploring behavioral therapy implemented within an intensive format. While literature is well-established to suggest behavioral therapy is the most effective treatment for SM, it has not been evaluated in an intensive intervention format before. However, there is research available about intensive interventions for similar disorders (e.g., social phobia, OCD) to suggest initial effectiveness findings. This study builds in additional methodological rigor to previous studies about intensive intervention by thoroughly investigating the acceptability and integrity of intensive intervention. Given the rarity of the SM diagnoses, this sample size of 25 provides a robust beginning to research on intensive interventions for this anxiety disorder subtype. The examination of both individual change and replicated change further highlights the necessity of a combined approach when working with youth with SM who present unique symptom profiles.
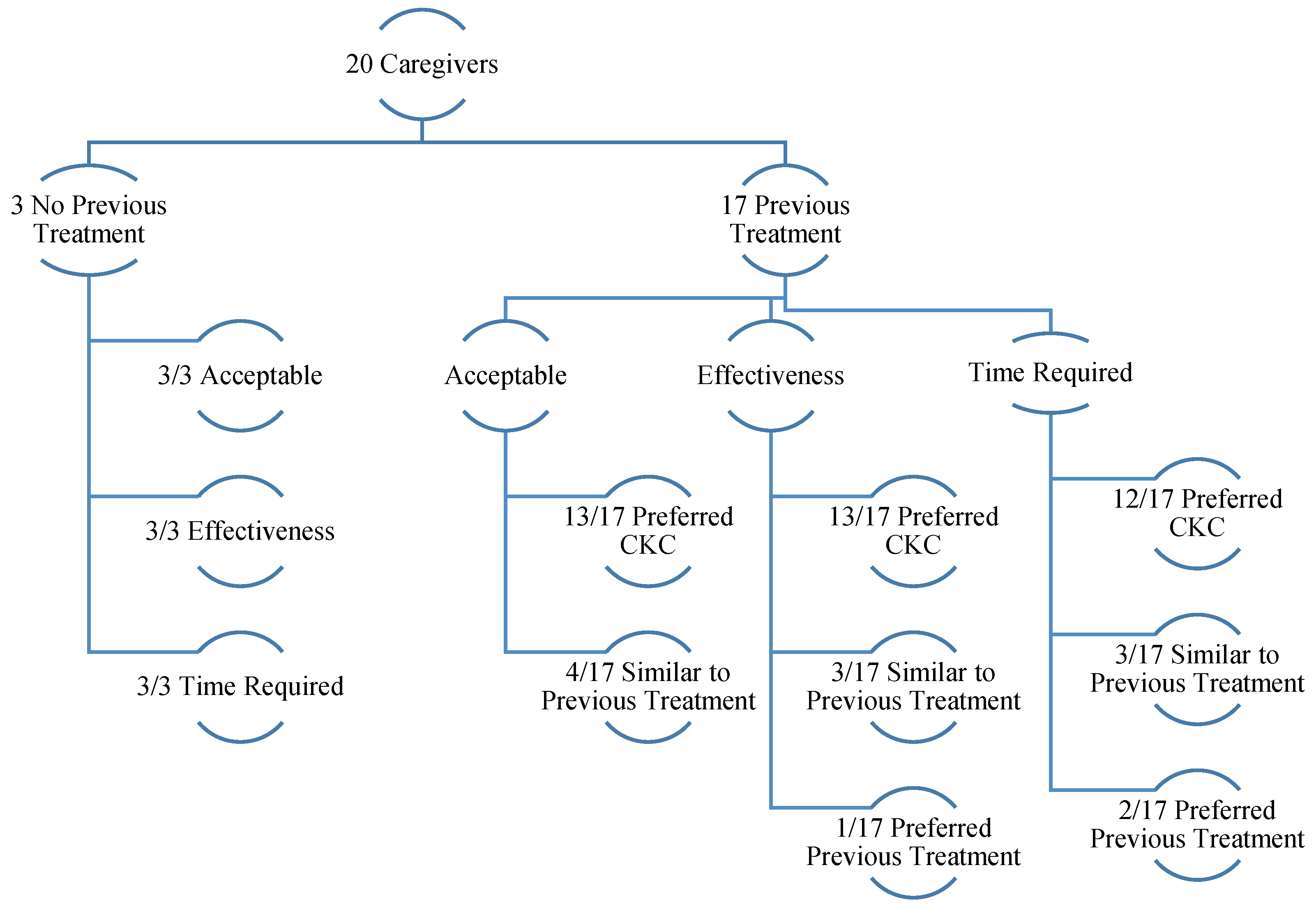
4.2. Treatment Acceptability
Caregivers inconsistently reported the intensive summer day camp as an acceptable treatment approach for SM. Specifically, only six caregivers endorsed satisfactory scores (110 or higher) [
34] for the intensive summer day camp’s overall acceptability on the TEQ-P. This overall score was impacted by inadequate scores of camp effectiveness on the TEQ-P, as only six caregivers endorsed acceptable scores (36 or higher) [
34]; however, the majority of caregivers endorsed satisfactory scores for the time required (
n = 16) and quality of treatment (
n = 17) of the intensive summer day camp on the TEQ-P. Conversely, family interviews revealed very high levels of caregiver-reported satisfaction with the intensive summer day camp, including for overall acceptability, effectiveness, time required, and quality of treatment.
Acceptability results from this study differ from previous intensive intervention literature for similar disorders, in which high levels of caregiver satisfaction were endorsed consistently [
8,
15,
18]. There are important potential explanations for why differences in acceptability exist between this study and past intensive intervention literature for similar disorders. First, it is possible caregivers from this study were less likely to endorse acceptable rates of effectiveness on the TEQ-P at posttreatment because they had not yet observed change in their child’s speech at school, which is both a naturalistic exposure and the primary environment where SM is reinforced [
4]. This is an explanation unique to SM that may influence why differences in acceptability existed between this study and previous intensive intervention literature. This explanation is supported by evidence from this study that counselors were more likely than caregivers to recognize the breakdown in the SM avoidance cycle (i.e., effectiveness changes) by the last day of camp, as they endorsed significant improvements in anxiety throughout camp for majority of campers (
n = 18). Caregivers from this study endorsed significant improvements in speaking behaviors (i.e., effectiveness) for majority of campers (
n = 17), but not until three-month follow-up. Second, this study differed from previous intensive intervention literature because it was the first to use a reliable survey to assess satisfaction with intensive intervention effectiveness. There are nine items on the TEQ-P that measure effectiveness, which is more than the overall acceptability measure used in the most comparable study [
8]. It is possible acceptability surveys and interviews from other studies assessed more for time required and quality of treatment than effectiveness, and that their results reflect this.
Despite differences in acceptability scores between this study and previous literature, there were many overlaps that add to the intensive intervention literature. Parent scaffolding of behavioral strategies (e.g., community-based exposure) and parent training, were the two distinct themes positively contributing to caregiver acceptability in this study’s family interviews consistent with prior literature [
18]. These identical reports align with the use of BICs as disruptive innovations, as their purpose is to treat the disorder, while relaying all necessary behavioral skills to caregivers, during a condensed treatment approach [
11]. The majority of caregivers in this study reported cost acceptability compared to cost of previous treatments, despite an average per camper out-of-pocket cost over
$2700 and inadequate effectiveness scores on the TEQ-P. Consistent with findings from two prior studies [
8,
18], it is possible intensive interventions are most accessible to higher income families, given travel and therapy costs to access experts for less prevalent disorders (e.g., SM). These data provoke critical discussion about whether intensive interventions are a disruptive innovation to behavioral therapy in its traditional format. While the intensive format is disruptive, these cost data suggest intensive intervention may not address cost barriers to treatment as originally hypothesized. Third, as expected, almost all caregivers reported satisfaction with this study’s scheduling and counselor implementation competency. This is consistent with prior report [
11] of BICs as disruptive innovations to circumvent traditional behavior therapy barriers, such as scheduling conflict for weekly therapy and lack of access to expert clinicians.
4.3. Treatment Integrity
As anticipated, all camp counselors self-reported excellent daily implementation integrity ratings (
M = 97%), exceeding the 80% adherence threshold recommended [
23]. This finding aligns with previous IBTSM research that behavioral therapy for SM can be implemented with high rates of integrity [
34],
M = 99% and supports findings from prior intensive intervention literature for similar disorders, e.g., [
16]. As hypothesized, counselor integrity was protected by consistency in counselor-camper match throughout treatment, brevity of treatment, counselor competency, and detailed treatment protocols [
22]. Interrater agreement between counselor self-ratings and a licensed clinician was 93% across daily one-hour observations of 14 counselors, which exceeded the average 81% agreement rate recommended [
24]. This is promising data for intensive interventions as disruptive innovations aim to address the barrier of implementation competency associated with low-prevalence disorders. Specifically, novice counselors in related professional fields (e.g., psychology graduate students, social workers) displayed superb treatment adherence to behavioral therapy following a one-day training from a SM expert clinician.
Similarly, caregivers’ average self-rated implementation integrity during the intensive summer day camp, during which they led a community-based exposure activity for their child, was 96%, which exceeded the 80% standard [
23]. No previous study has reported caregiver implementation integrity for intensive interventions. All counselors scored their camper’s caregiver’s implementation at or above 80% integrity during the community-based exposure, and the rate of interrater agreement (91%) was higher than the recommended threshold of 81% [
24]. As hypothesized, it is likely caregiver integrity was protected by similar factors described above for counselors. High levels of caregiver treatment adherence is important for the intensive intervention literature for SM. Ultimately, these adherence rates imply caregivers obtained excellent behavioral therapy skills for SM as a result of daily two-hour parent trainings from a SM expert clinician. High rates of caregiver adherence suggest caregivers perceived the behavioral treatment approach as highly acceptable [
14], which is impressive given the heterogeneous sample for this study, which included caregivers whose children had no previous treatment for SM, previous behavioral treatment, and previous play therapy.
These acceptability and integrity data provide initial support for intensive interventions as disruptive innovations to address the barrier of access to expert clinicians for a low-prevalence disorder like SM. Specifically, they provide initial support for the component of BIC interventions to access an expert briefly and then generalize skills learned to home, school, and public [
11]. It was surprising, then, that only two caregivers showed evidence of tracking implementation integrity between intensive summer day camp and three-month follow-up, especially in light of the ability to receive effectiveness data from the majority of families at three-month follow-up (reported below). It is likely the integrity rating sheets were burdensome to track and subsequently turn in via email scanning/mail. Though there is information to be desired about caregiver implementation between posttreatment and three-month follow-up, it can be hypothesized caregivers continued to implement behavioral therapy strategies successfully. This hypothesis is supported by the link between implementation integrity and intervention effectiveness discussed further below.
4.4. Anxiety Symptoms
This was the first intensive intervention study for an anxiety disorder to assess within-intervention subtype anxiety changes, and the results are promising. Counselors indicated that 18 of 25 campers experienced a significant decrease in their highest subtype of anxiety during camp. The younger, middle, and older camp classes experienced anxiety change on counselor-rated DBRs with large effect sizes. In contrast to significant counselor-rated changes in anxiety for those participating in the intensive summer camp, only three campers’ caregivers endorsed significant decreases in anxious symptoms from pretreatment to posttreatment. These data differ from a previous intensive intervention study that found all five participants experienced a significant decrease in separation anxiety disorder symptoms at posttreatment [
20].
These outcome data pertaining to anxiety symptoms are important, as they align with the behavioral conceptualization of the communication hierarchy associated with SM. Specifically, counselors increase exposure to speech (e.g., forced-choice questions vs. open-ended questions) at an appropriate pace to promote speech, and the pace of this treatment hierarchy was individualized to each camper. Counselor DBR data suggest some change was occurring for most children’s highest rated anxiety during camp, which aligns with the behavioral mechanism of change theory that lower rates of anxiety promote success with exposure to speech in incrementally challenging situations. This process is identical to the goal of behavioral treatment for SM, which is to decrease symptoms of SM as children become more confident with increasingly challenging exposures. Results from this study suggest counselors, or providers of the intensive intervention, are in a better position to identify those symptoms changes during treatment than caregivers who were not present throughout the day.
4.5. Speaking Behaviors
Nine of the 25 campers experienced significant improvements in caregiver-rated speaking behaviors from pretreatment to posttreatment, as reported on the SMQ. This increased within other campers at follow-up (9 out of 14), suggesting a lag effect of speech behavior. These data are consistent with the behavioral mechanism of change theory that anxiety was reduced prior to seeing changes in speech. Specifically, speech was established in a safe environment (i.e., camp) with repetitive exposures before it was generalized to school/community with improvements noticeable to caregivers.
Study results also support the importance of looking at treatment outcomes, developmentally. For example, aggregated class effect size calculations revealed that the older class experienced significant improvements in caregiver-rated speaking behaviors from pretreatment to posttreatment (
RCI = 3.11). Yet, those changes appeared to max out for the older group, as speaking behavior was maintained at three-month follow-up. Aggregated class effect size calculations revealed significant improvements in caregiver-rated camper speaking behaviors for the younger (
RCI = 8.10) and middle (
RCI = 7.17) class from posttreatment to three-month follow-up, and for total campers (
RCI = 4.50). Similar developmental differences in treatment gains at one-year follow-up after six months of behavioral treatment for SM (
n = 24) were found compared to prior studies [
18] which found that 78% of three to five-year-olds did not meet diagnostic criteria for SM, compared to 33% of six to nine-year-olds. While the present study did not assess for diagnostic criteria, speaking behaviors are the most related SM diagnostic symptom, and this study provides more evidence to support that breaking the speech avoidance cycle [
4] can result in better outcomes [
18].
This was the first study to track daily child speaking behaviors and code words per minute during a 5-consecutive day intensive summer day camp for SM. This study found that three campers improved responsive speech throughout camp and that four campers improved spontaneous speech over camp. This methodology of measuring speech raises the bar from previous SM literature [
35,
36]. Both articles reported increases in response rate to over 50% of prompted opportunities by halfway through treatment. Campers do not escape responses during camp (i.e., response rate of ~100%), and are thus inundated with learning opportunities that speaking cannot be avoided. It makes sense, then, that campers were likely to generalize this learning to different contexts (i.e., school and public) after camp was over via parent SMQ ratings at three-month follow-up. As a result, evidence from this study demonstrated caregiver-rated camper speaking behaviors improved more between posttreatment and three-month follow-up than pretreatment to posttreatment. Verifying those changes within the school context will be essential in future research.
4.6. Limitations
The present study is limited by reliability and validity of baseline measures. First, consistency in baseline anxiety levels could not be established due to significant differences in caregiver-rated SCARED scores from intake to pretreatment. Second, due to intensive summer day camp structure, there was not ample time/opportunity to establish a baseline of speech behavior before intervention; however, ITSSIM software was chosen specifically for analysis because it addresses this clinical practice limitation. Third, the DBR was a truncated scale from zero to two, which could have affected how changes were detected, most notably resulting in large effect sizes. Additionally, the lack of a comparison group is a limitation of this study. Without a comparison group, it is impossible to know if camper changes over time were due to intervention or not. Maturation is a possible explanation for changes over time and is a threat to the internal validity of this study without a comparison group. Missing data from the three-month follow-up is a limitation of the study. It is also possible a biased subsample responded to study recruitment materials.
4.7. Implications for Research
This pilot feasibility study sets a foundation for the investigation of intensive summer day camps as a treatment for SM, as to date, intensives have only been reported in the literature for other anxiety-related conditions [
8,
20]. Replications of this study, with refinements, are warranted to address its limitations. First, more research is needed to better understand family acceptability of intensive summer day camp intervention as a treatment for SM to clarify inconsistencies in this study’s results of effectiveness acceptability. Future research should consider using the TEQ-P to assess family acceptability, but place it at a follow-up data collection time point for more accurate perceptions about intervention effectiveness. Additionally, a future study could explore the psychometric properties of the semi-structured interview used in this study, as it could be an important tool for quality improvement efforts. Continued research efforts to evaluate the acceptability of intensive summer day camps as a treatment for SM are critical to establishing its feasibility.
More research is needed to better understand factors contributing to implementation integrity of behavioral therapy during and after the intensive summer day camp for children with SM. Given the high rates of integrity by counselors and caregivers during camp after only a brief training from the lead CKC clinician, it would be interesting to assess which parts of the parent and counselor training promote integrity. Most notably, more research is needed to understand parent implementation integrity of SM behavioral therapy after intensive summer day camp is over. Specifically, understanding which components of acceptability optimize the likelihood parents will practice SM behavioral therapy and track their implementation integrity would be useful for practice.
Future research may address limitations from this study’s evaluation of the effectiveness of intensive summer day camp intervention. Researching the possible treatment effects of the lead-in session is warranted. As such, ensuring a baseline for speaking behaviors and anxiety levels is established before intervention will result in more valid data. Additionally, implementation with more severe SM campers and with a control group will make for exciting progress in the literature. Next, a better understanding of responsive speech changes to spontaneous speech will be warranted for the intensive summer day camp intervention research. Additionally, controlling for a clinic effect is essential in future research. While this study’s intensive intervention simulated a school-like environment, it is essential to transition treatment to the child’s unique environment, especially school.
4.8. Implications for Practice
This study informs initial implications for practice. First, this study suggests SM behavioral therapy can be implemented with integrity by novice clinicians and parents after training from a SM expert clinician. Given training was brief and there is a need for SM-competent clinicians, SM expert clinicians may be motivated to provide training to clinicians, schools, and parents. Second, a lack of replicated change across campers at posttreatment and inadequate follow-up response rate may reveal a need for more frequent booster sessions. This implication for practice would be interesting to investigate alongside increasing access to teletherapy, as it is also perceived as a cost-effective and accessible treatment for anxiety disorders [
37].