POCUS Diagnosis of Sternal Fractures in Children without Direct Trauma—A Case Series
Abstract
1. Introduction
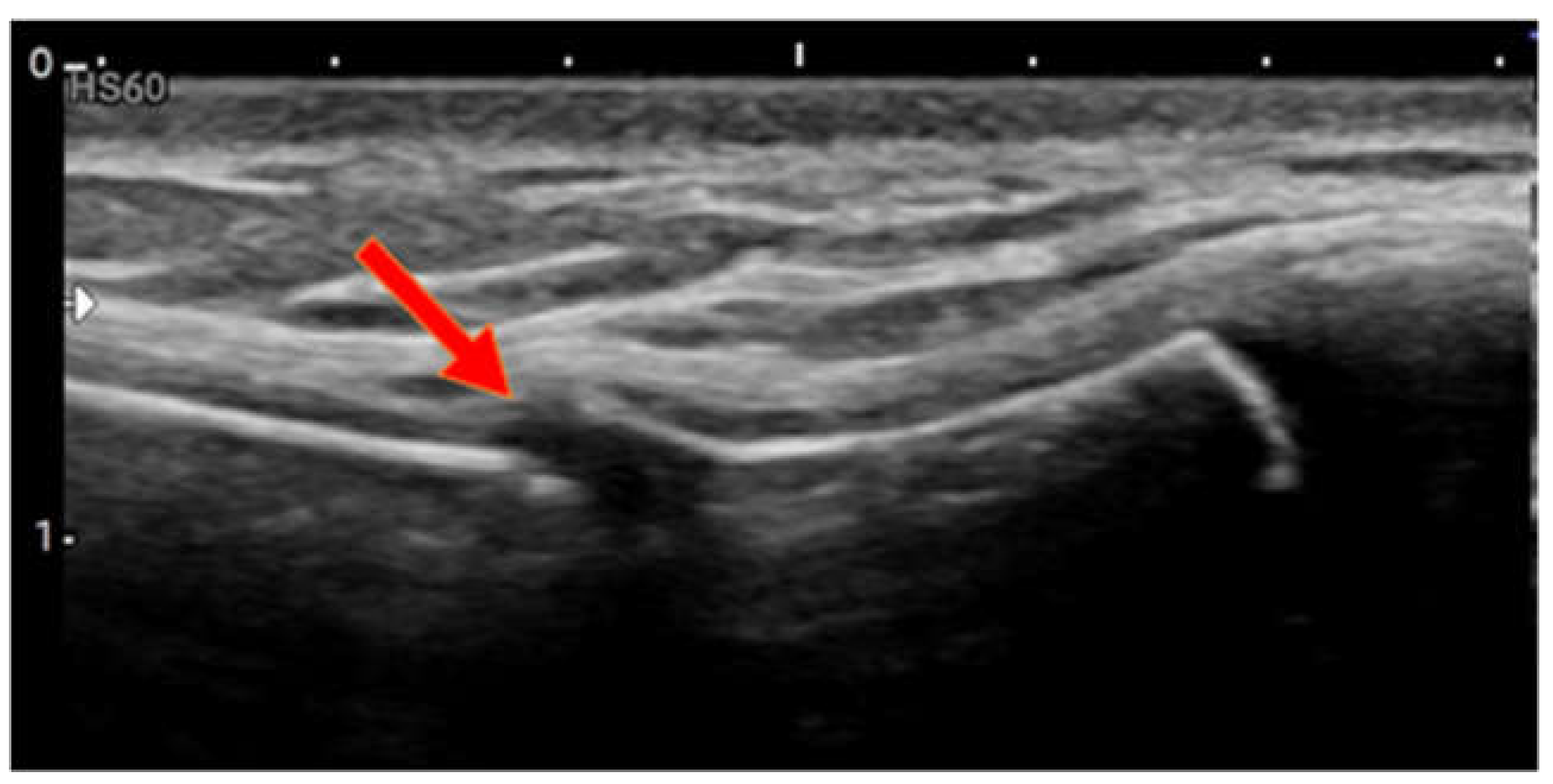
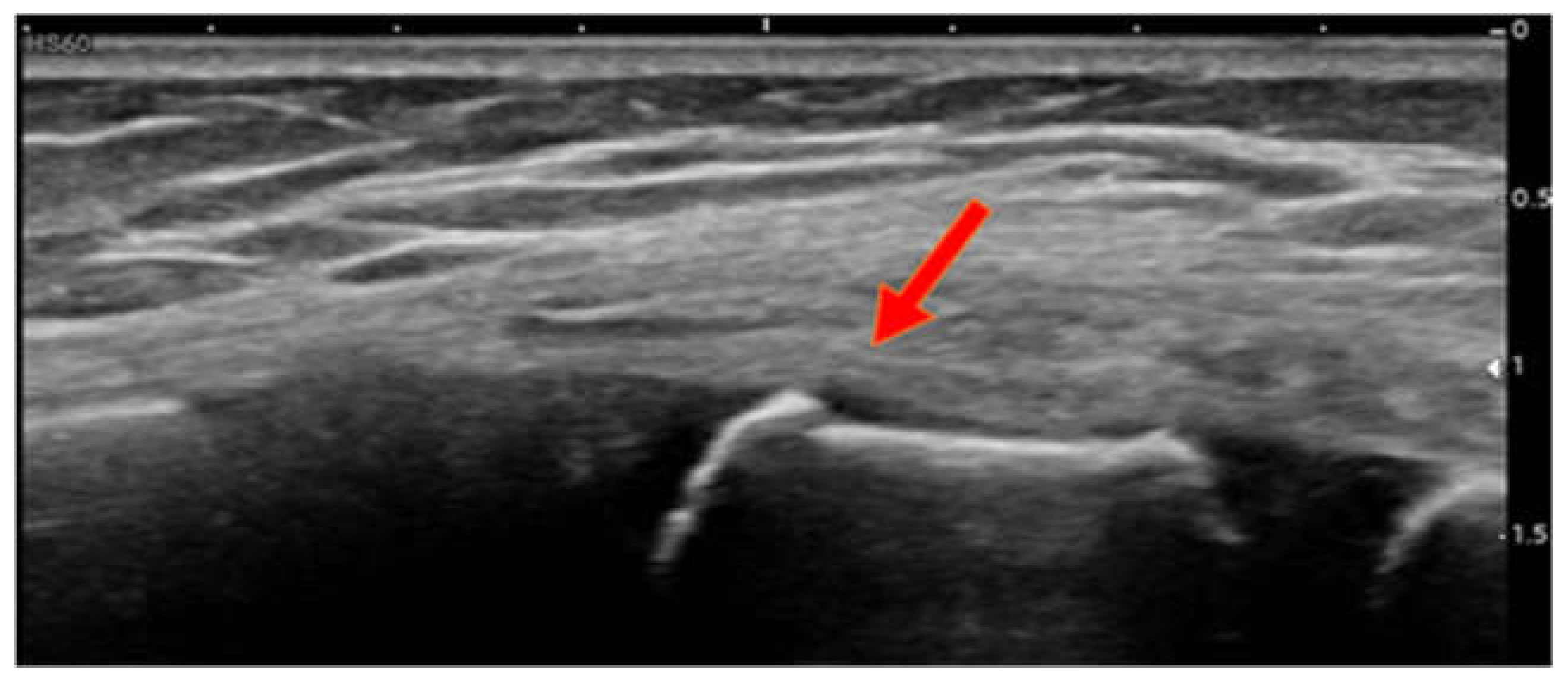
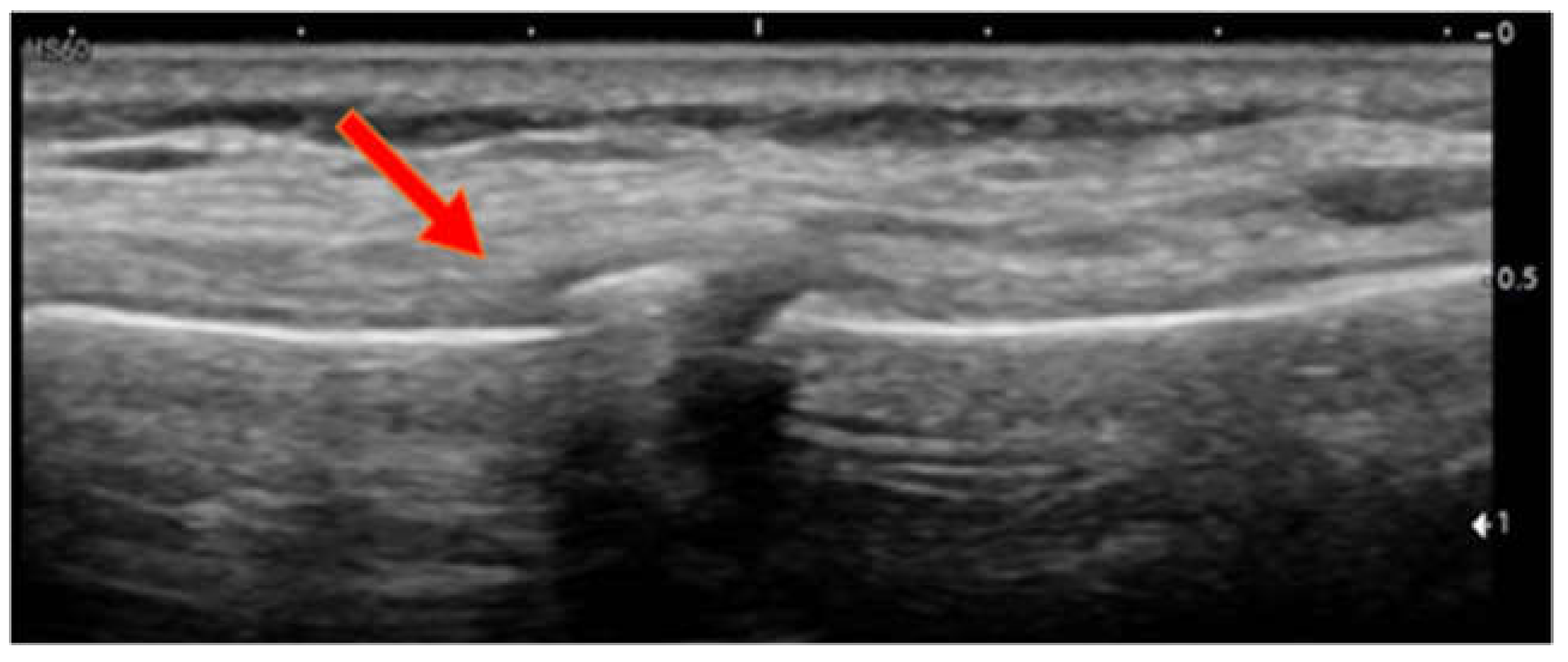
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Schmitt, S.; Krinner, S.; Langenbach, A.; Hennig, F.F.; Schulz-Drost, S. Analysis on the Age Distribution of Sternum Fractures. Thorac. Cardiovasc. Surg. 2018, 66, 670–677. [Google Scholar] [CrossRef]
- Özsoy, I.E.; Tezcan, M.A. A Rare Injury in Children: Sternum Fractures. J. Coll. Physicians Surg. Pak. 2019, 29, 993–995. [Google Scholar] [CrossRef] [PubMed]
- Perez, F.L.; Coddington, R.C. A Fracture of the Sternum in a Child. J. Pediatr. Orthop. 1983, 3, 513–515. [Google Scholar] [CrossRef] [PubMed]
- Fichtel, I.; Fernandez, F.; Wirth, T. Sternal fracture in growing children: A rare and often overlooked fracture? Documentation of four cases. Der Unf. 2016, 119, 570–574. [Google Scholar] [CrossRef]
- Khalil, P.A.; Benton, C.; Toney, A.G. Point-of-Care Ultrasound Used to Diagnose Sternal Fractures Missed by Conventional Imaging. Pediatr. Emerg. Care 2021, 37, 106–107. [Google Scholar] [CrossRef] [PubMed]
- Nickson, C.; Rippey, J. Ultrasonography of sternal fractures. Australas. J. Ultrasound Med. 2011, 14, 6–11. [Google Scholar] [CrossRef][Green Version]
- You, J.S.; Chung, Y.E.; Kim, D.; Park, S.; Chung, S.P. Role of sonography in the emergency room to diagnose sternal fractures. J. Clin. Ultrasound 2010, 38, 135–137. [Google Scholar] [CrossRef]
- Sesia, S.B.; Prüfer, F.; Mayr, J. Sternal Fracture in Children: Diagnosis by Ultrasonography. Eur. J. Pediatr. Surg. Rep. 2017, 5, e39–e42. [Google Scholar] [CrossRef]
- Bühlmann, K.M.; Castiglioni, D.A.; Flores, X.O.; Sánchez, C.P.; Johnson, J.E.; Matta, M.P.; Lenz, J.G. Estudio clínico radiológico de las fracturas esternales en edad pediátrica. Radiologia 2019, 61, 234–238. [Google Scholar] [CrossRef]
- Perez-Martinez, A.; Marco-Macian, A.; Gonzalvez-Pinera, J.; Agustí-Buztke, B.; Goñi-Orayen, C.; Moya-Marchante, M. Cortical fracture of the sternum in a child: An infrequent case. Cir. Pediatrica 1996, 9, 130–131. [Google Scholar]
- Ferguson, L.P.; Wilkinson, A.G.; Beattie, T.F. Fracture of the sternum in children. Emerg. Med. J. 2003, 20, 518–520. [Google Scholar] [CrossRef]
- Davis, S.N.; Delaney, J.S.; Robichaud, L. An unusual cause of chest pain: Exercise induced sternal fracture in a young man. Am. J. Emerg. Med. 2020, 38, 2244-e1. [Google Scholar] [CrossRef] [PubMed]
- Jones, G.L. Upper Extremity Stress Fractures. Clin. Sports Med. 2006, 25, 159–174. [Google Scholar] [CrossRef]
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Age (years) | 14 | 9 | 6 |
| Sex | Male | Male | Female |
| Trauma impact | Feet | Feet | Head |
| Fracture site | Manubrium sterni caudal | 1st sternebra cranial | 1st sternebra caudal |
| Displacement | None | None | None |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Troxler, D.; Mayr, J. POCUS Diagnosis of Sternal Fractures in Children without Direct Trauma—A Case Series. Children 2022, 9, 1691. https://doi.org/10.3390/children9111691
Troxler D, Mayr J. POCUS Diagnosis of Sternal Fractures in Children without Direct Trauma—A Case Series. Children. 2022; 9(11):1691. https://doi.org/10.3390/children9111691
Chicago/Turabian StyleTroxler, David, and Johannes Mayr. 2022. "POCUS Diagnosis of Sternal Fractures in Children without Direct Trauma—A Case Series" Children 9, no. 11: 1691. https://doi.org/10.3390/children9111691
APA StyleTroxler, D., & Mayr, J. (2022). POCUS Diagnosis of Sternal Fractures in Children without Direct Trauma—A Case Series. Children, 9(11), 1691. https://doi.org/10.3390/children9111691







